Summary
Artifacts in magnetic resonance imaging and foreign bodies within the patient’s body may be confused with a pathology or may reduce the quality of examinations. Radiologists are frequently not informed about the medical history of patients and face postoperative/other images they are not familiar with. A gallery of such images was presented in this manuscript. A truncation artifact in the spinal cord could be misinterpreted as a syrinx. Motion artifacts caused by breathing, cardiac movement, CSF pulsation/blood flow create a ghost artifact which can be reduced by patient immobilization, or cardiac/respiratory gating. Aliasing artifacts can be eliminated by increasing the field of view. An artificially hyperintense signal on FLAIR images can result from magnetic susceptibility artifacts, CSF/vascular pulsation, motion, but can also be found in patients undergoing MRI examinations while receiving supplemental oxygen. Metallic and other foreign bodies which may be found on and in patients’ bodies are the main group of artifacts and these are the focus of this study: e.g. make-up, tattoos, hairbands, clothes, endovascular embolization, prostheses, surgical clips, intraorbital and other medical implants, etc. Knowledge of different types of artifacts and their origin, and of possible foreign bodies is necessary to eliminate them or to reduce their negative influence on MR images by adjusting acquisition parameters. It is also necessary to take them into consideration when interpreting the images. Some proposals of reducing artifacts have been mentioned. Describing in detail the procedures to avoid or limit the artifacts would go beyond the scope of this paper but technical ways to reduce them can be found in the cited literature.
MeSH Keywords: Artifacts; Image Interpretation, Computer-Assisted; Magnetic Resonance Imaging
Background
Artifacts in magnetic resonance imaging (MRI) may be caused by the MR scanner hardware itself or by the interaction of the patient with the hardware [1]. Artifacts and foreign bodies within the patient’s body may be confused with a pathology or just reduce the quality of examinations. The knowledge of the artifacts and their sources is extremely important in order to avoid false diagnoses and to learn how to eliminate them [2]. Radiologists are frequently not informed about the medical history of patients. When performing the examinations, they face postoperative images (without knowing the patient’s history) or other images they are not familiar with – caused by foreign bodies.
Almost every MRI exam includes some kind of artifacts. Depending on their origin, one can classify them into the following groups:
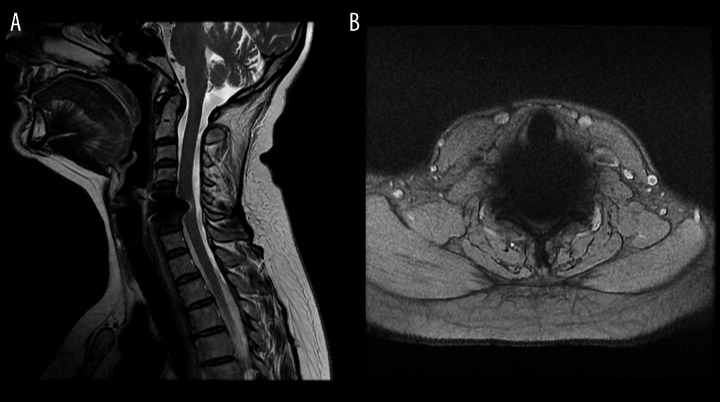
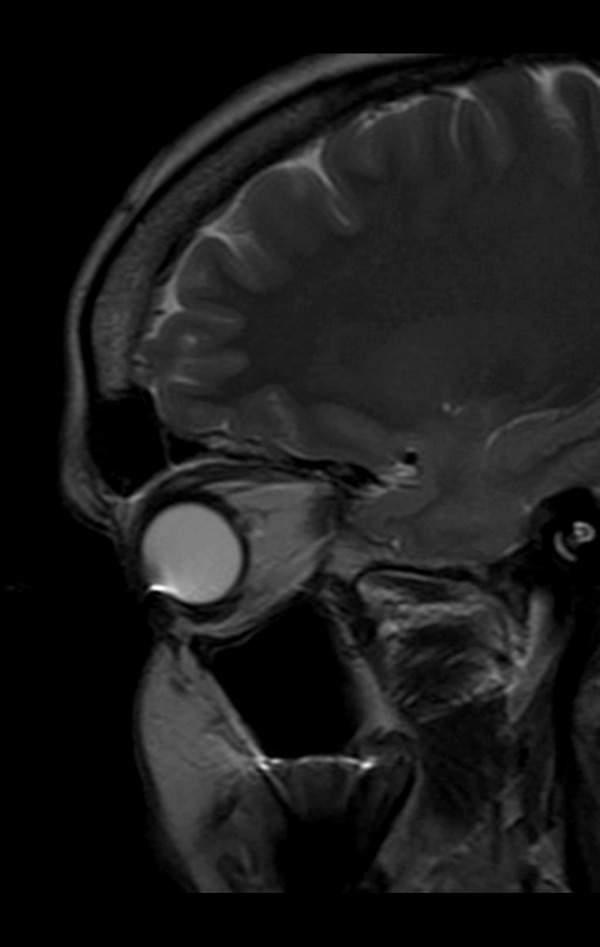
Truncation artifacts which occur near sharp high-contrast boundaries and are also known as the Gibbs phenomenon. They appear as multiple, alternating bright and dark lines – “ringing”. They can be misinterpreted as a syrinx in the spinal cord (Figure 1) [3] or a meniscal tear in the knee.
Motion artifacts caused by breathing, cardiac movement, CSF pulsation/blood flow, patient’s movement, which create ghost artifacts (Figures 2–6). They can be reduced by patient immobilization, cardiac/respiratory gating, saturation bands, or drugs that slow down the intestinal peristalsis. One can also reduce motion artifacts by using echo-planar imaging (EPI), a very fast MR imaging technique [4].
Aliasing artifacts occur when the anatomical structures located outside the field of view are mapped at the opposite end of the image. One can eliminate them by increasing the field of view (FOV) [3] (Figure 7A, 7B).
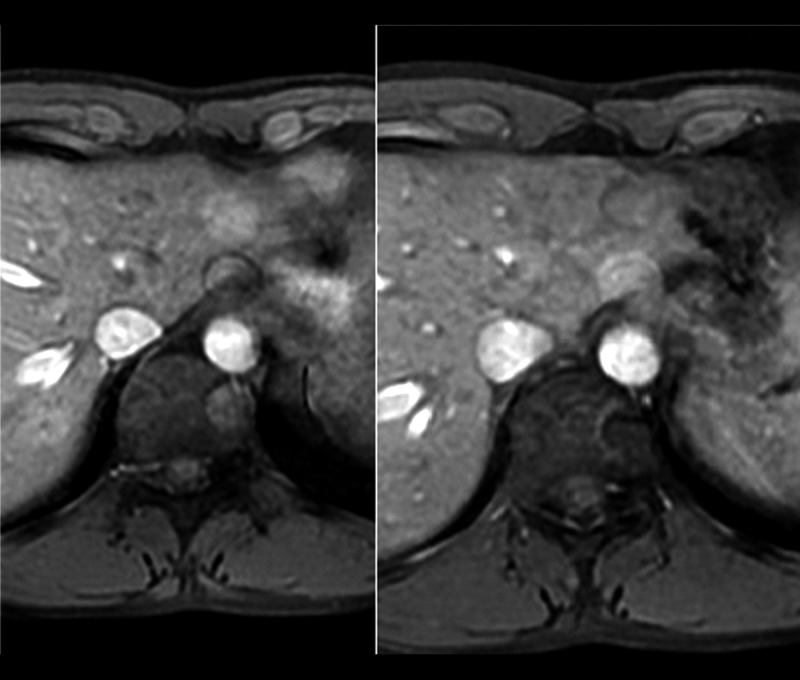
Chemical shift artifacts appear as dark or bright bands at the lipid-water interface and are seen especially in case of fluid-filled structures surrounded by fat (e.g. eye balls in the orbits, bladder). They tend to by less prominent on T1-weighted images than on T2-weighted images. Interestingly, these artifacts have been used as a diagnostic aid [3], to confirm the presence of fat within lesions, e.g. in adrenal adenomas (Dual echo sequences/out-of-phase images – Figure 8A) or to accentuate the fat-water interfaces at visceral margins Figure 8B), thus helping in the evaluation of peripheral tumors for possible extravisceral extension [5].
Others – technical literature uses many different names for artifacts, e.g. banding artifact, pile-up artifact, peripheral signal artifact, spike noise artifact, blurring artifact, suppression artifact etc. [1].
Figure 1.

Typical syrinx-like manifestation of truncation artifact in the spinal cord.
Figure 2.

CSF pulsation imitates intradural spinal hemangioma.
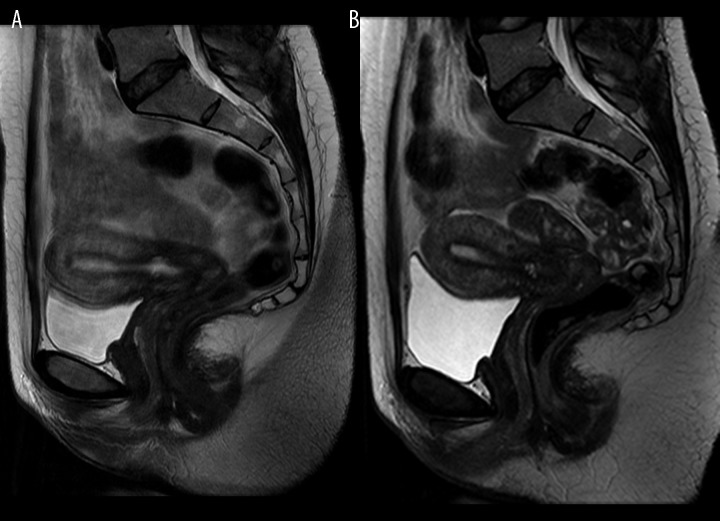
Figure 6.
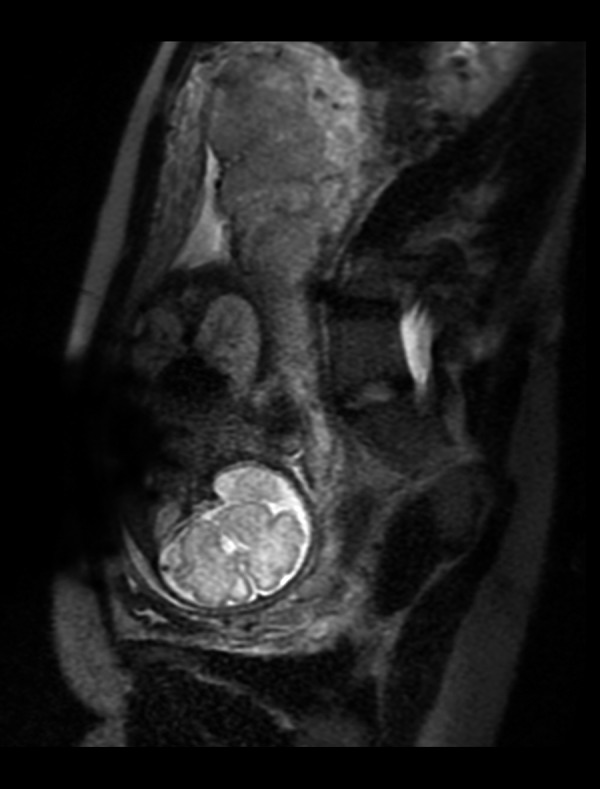
Motion artifacts caused by the peristalsis produce a blurry image of the uterus in pelvic MRI (A). Reduction of the artifacts after intramuscular or intravenous administration of buscolysin (B).
Figure 7.
Aliasing artifact (“wrap around”) on brain MRI with FOV=24×18 cm (A). The same patient, examination with FOV=24×24 cm (B).
Figure 8.

Examples of chemical shift artifacts in the out-of-phase image (A) and in FIESTA/2D sequence (B).
Examples
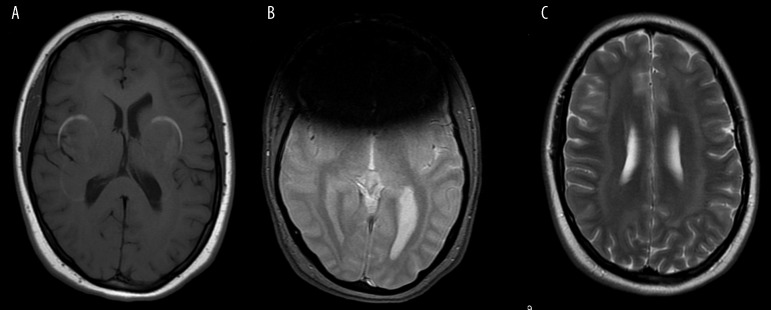
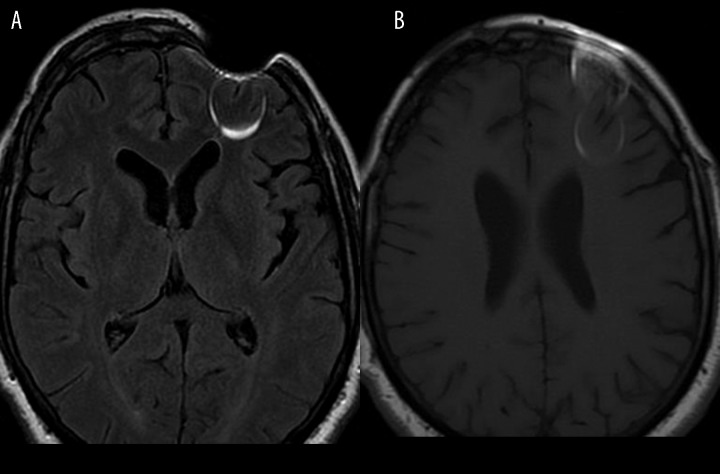
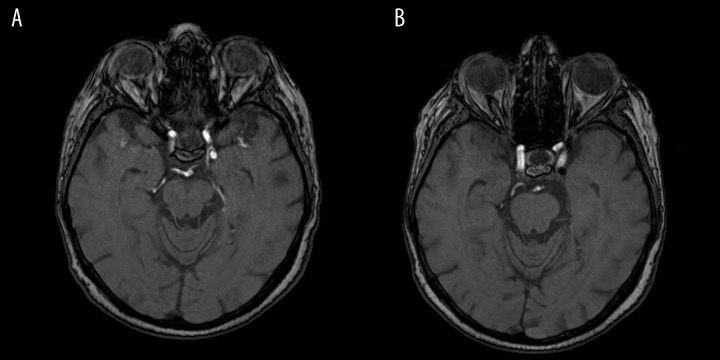
An abnormally hyperintense signal on FLAIR images can result from CSF/vascular pulsation (Figure 9), magnetic susceptibility artifact (Figure 10), motion, but also in patients undergoing MRI examinations while receiving supplemental oxygen [6].
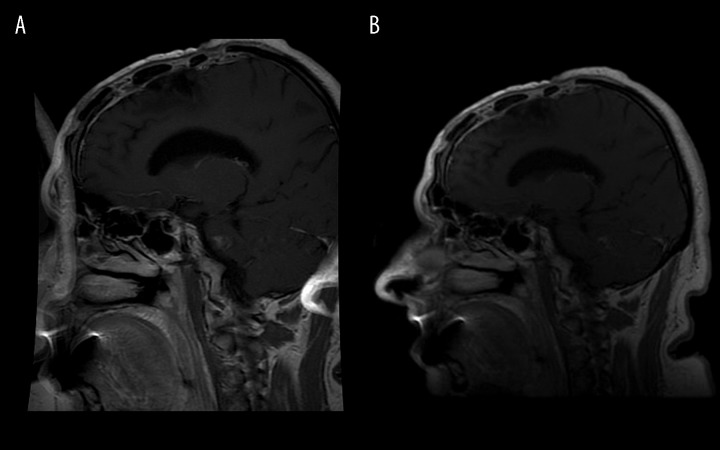
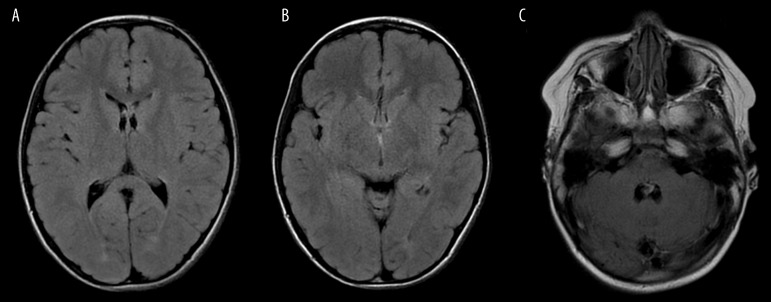
Figure 9.
FLAIR-hyperintense signal in the frontal horns of the lateral ventricles (A), third ventricle (B) and in the fourth ventricle (C).
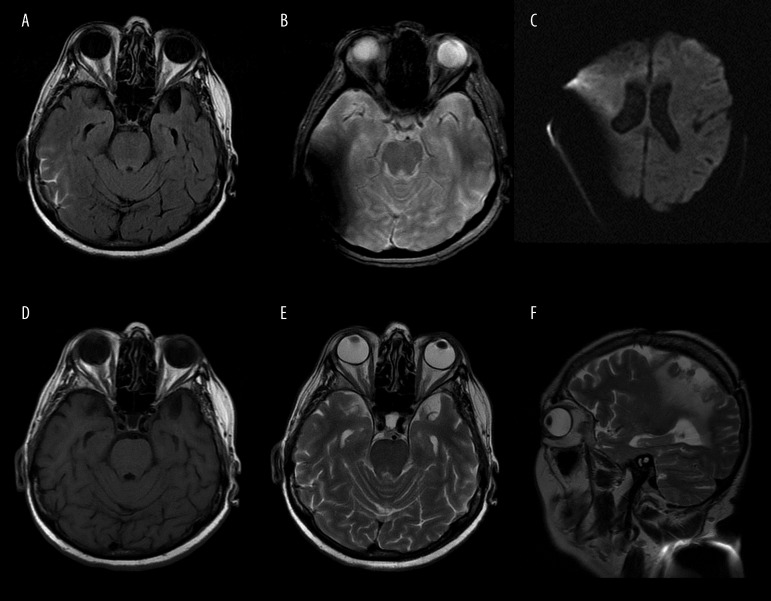
Figure 10.
This artifact from clothing ornament – hyperintense signal on FLAIR sequence – may raise the suspicion of subarachnoid hemorrhage. (A). Gradient echo sequences (B) and DWI (C) are very sensitive to artifacts, especially those produced by metallic objects. The artifacts are almost invisible in SE/T1-weighted sequence (D) and in FSE/T2 (E – note that only the lens in the right eye ball shows abnormal signal intensity). Sagittal projection shows directly the source of the artifact located on the arm (F – FSE/T2, sag).
Metallic objects, not only within the patient’s body but also on the patient, e.g. in the clothes, may result in FLAIR-hyperintensity due to a magnetic susceptibility artifact. In brain MRI such artificial FLAIR-hyperintensity in the subarachnoid space may lead to a false diagnosis of subarachnoid hemorrhage (Figure 10A). Sometimes it is not necessarily a visible metallic element like in the case presented in Figure 10. We had a case of a patient who wore only a white singlet during the examination which seemed to be made of cotton (!) and the artifact disappeared after she had taken it off.
Spike noise artifacts, resembling checkered pattern on the clothes, are caused by static electricity from clothing or blankets and are not necessarily related to metal – they may be caused by acrylic materials [1].
The aim of this article was to present different types of artifacts and appearances of various foreign bodies within the patient’s body in magnetic resonance imaging in order not to confuse them with pathological conditions. The authors presented a gallery of such images. All examinations were performed with use of GE Signa HDxt scanners with a magnetic field strength of 1.5 T.
The Gallery of Images of Foreign Bodies with and without Artifacts
As stated in the introduction, artifacts are frequently caused by metallic and other foreign bodies which may be found on and in patients’ bodies and these are the focus of this paper.
One can divide them into the following groups:
– group A – foreign bodies we know and can eliminate: the most popular and easy to recognize and eliminate, usually connected with outfit or ornament of the body, make-up, hair accessories – hair ties, clothes, labels on clothes, but also with medical equipment, e.g. hearing aid;
– group B – foreign bodies that are known but impossible to eliminate, e.g. surgical/neurosurgical clip or staplers, endoprostheses;
– group C – foreign bodies that are not known to the MRI unit personnel because the patients forget about them, do not know about them or do not report them in the questionnaire they fill in before the examination.
Different sequences are sensitive to these objects to various degrees (Figure 10).
The best way to reduce the severity of susceptibility artifacts caused by metallic foreign bodies is to use spin echo sequences (SE) with a short echo time (TE) [7]. The artifacts are less prominent in fast SE (FSE) than in conventional SE sequences [8]. However, it is not always possible and not always improves the image quality in a significant way. Iterative decomposition of water and fat with echo asymmetry and the least-squares estimation (IDEAL) is a recently developed sequence which separates fat and water with a very high signal-to-noise-ratio (SNR), is insensitive to magnetic field inhomogeneity and reduces metallic artifacts, e.g. in postoperative patients with metallic hardware [9]. It also improves fat suppression [1]. Gradient echo (GRE) and echo-planar sequences should be avoided because they accentuate susceptibility artifacts [10,11]. However this is also not always possible and in such cases reducing TE in GRE sequence is helpful [1].
Group A
The newborns, especially before the era of MR-compatible incubators, were usually examined dressed up from toes to head to keep them warm during their stay in the scanner room. Probably, the metallic thread in the labels in the newborns’ caps was the reason why the brain images were completely illegible when the cap had remained on the baby’s head. Similarly, an elastic left in the patient’s hair or a hearing aid forgotten in the ear (Figure 11) can produce the same effect of signal loss and “black hole” in the head.
Figure 11.
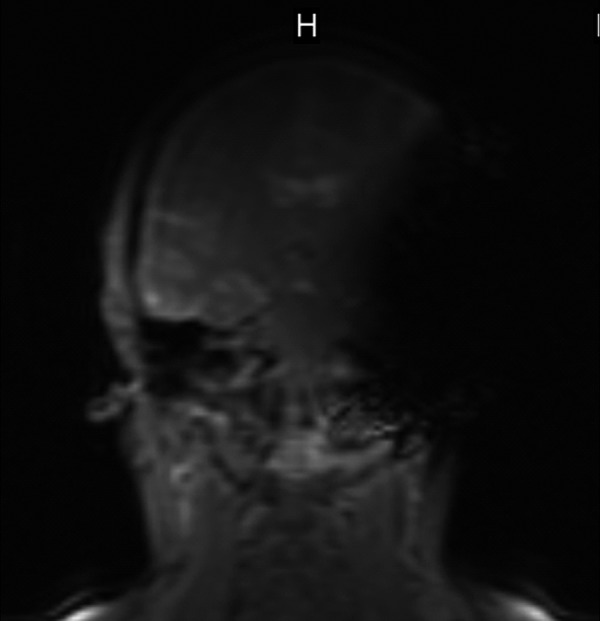
Hearing aid forgotten by the patient – pilot sequence.
Cosmetics can produce severe distortion of the magnetic field and make the contents of the orbits difficult to assess. The distortion results from the presence of iron oxide in the pigments used to produce dark shades of the make-up [12] (Figure 12). Tattoo pigments contain metallic elements which also distort the magnetic field and sometimes make MR imaging impossible (Figure 13), not to mention possible heating up and burning the patient during the study, or the carcinogenic ingredients.
Figure 12.
Artifacts in the eye ball region caused by the make-up. Artifacts caused by a dental implant in the maxillary sinus region are also seen.
Figure 13.
Tattoo-induced artifacts making it impossible to visualize the whole fetal head.
Group B
The type and size of an artifact produced by dental materials correlates with their shape, size, number of objects and most significantly – type of metal [13,14]. The same applies to other metallic implants, not only to dental ones [15]. Orthodontic appliances (ferromagnetic material) generally cause large magnetic field distortion and signal loss in frontal and/or temporal lobes and upper and lower jaw regions. Dental implants usually are made of titanium (non-ferromagnetic material) which should not have an influence on MR images. However, due to traces of ferromagnetic iron, they may decrease the quality of MR images [16].
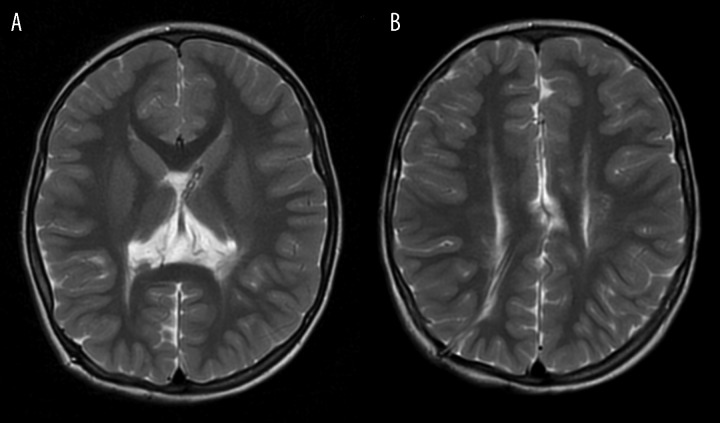
Excessive artifacts make it very difficult, and sometimes impossible, to recognize an important intracerebral pathology (Figure 14). Such excessive artifacts are caused by orthodontic braces, more and more frequently encountered not only in children and adolescents. Dental materials interfere not only with brain MRI but also with orofacial and neck imaging [14].
Figure 14A, B.
Orthodontic braces. Typical T1-hyperintense artifacts (A). Loss of signal in GRE/T2*-weighted images (B) makes it impossible to see the anterior part of the brain in this patient with seizures but band heterotopia can be appreciated if the radiologist is familiar with this kind of neuronal migration defect.
Figure 14C. Orthodontic braces. FSE/T2-sequence is less sensitive and band heterotopia can be diagnosed more easily.
The knowledge of the influence of dental implants on various sequences and of different kinds of signal alterations they cause is extremely important in order not to mistake them for brain lesions (Figure 15).
Figure 15.
Artifact caused by a dental implant in the right temporal lobe can be easily misinterpreted as a focal lesion on FLAIR images (A) but its typical rounded hyperintense appearance on T1-weighted images (B) enables proper interpretation of this finding.
Neurosurgical clips produce similar artifacts (Figure 16).
Figure 16.
Artifacts produced by neurosurgical clips. FLAIR, ax (A), SE/T1, ax (B).
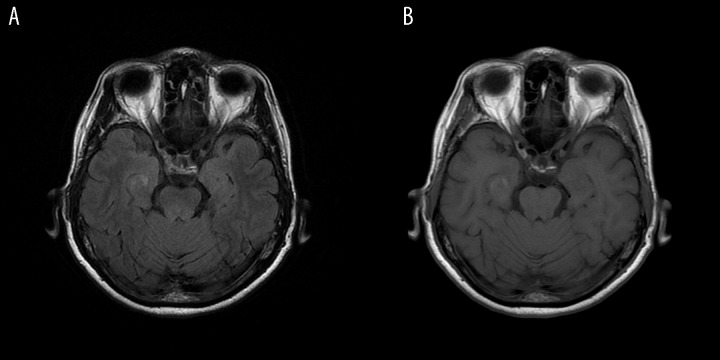
Ventricular shunt valves can also generate considerable artifacts due to distortion of the MR image, especially in GRE sequences [17]. However, nowadays they are most often visible as low signal intensity lines only and do not disturb MR images (Figure 17).
Figure 17.
(A, B) Ventricular shunt in the frontal horn of the left lateral ventricle – without artifacts.
Disc prostheses and other elements used for spinal surgery (e.g. interspinous process spacers) also induce significant artifacts in MRI which may complicate radiological follow-up after surgery [18]. Stainless steel is known to produce large amounts of artifacts, whereas titanium is known to produce significantly less of them [19]. These artifacts make interpretation of the spinal cord difficult and visualization of the root canals impossible at the operated levels (Figure 18). Magnesium and carbon-fiber-reinforced polymers produce fewer artifacts than titanium [20].
Figure 18.
Artifacts caused by an intervertebral implant are less pronounced in FSE/T2-sequence (A) than in GRE sequence (MERGE/2D, T2, ax – B) at the operated level of C5/C6.
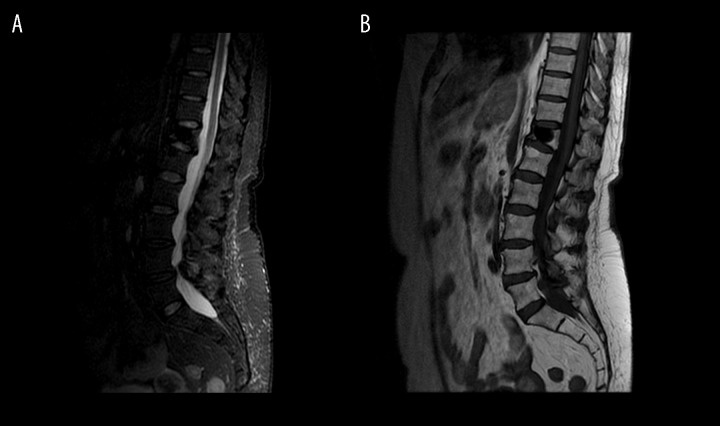
Image-guided application of cement for kyphoplasty or vertebroplasty results in the presence of low signal intensity material in the treated vertebral body in all sequences and does not produce artifacts (Figure 19).
Figure 19.
Vertebroplasty after Th12 fracture. STIR, sag (A), FSE/T1, sag (B).
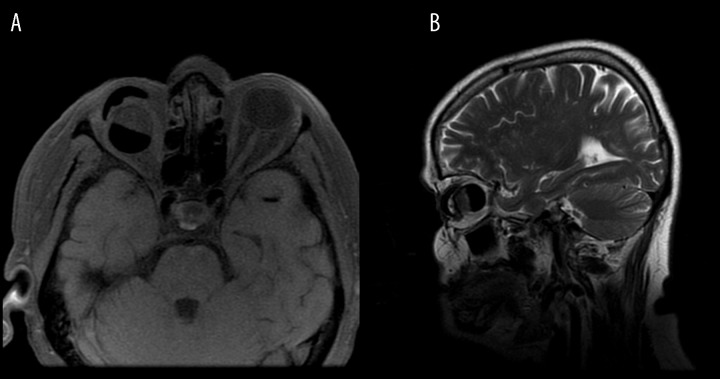
Intracranial aneurysms treated by coiling may be difficult to assess after the procedure because of MR imaging artifacts. On the other hand, intracranial aneurysms occluded with the liquid polymer Onyx are hypointense, probably because of its tantalum content, and do not create artifacts [21] (Figure 20).
Figure 20.
MR-angiography, raw data. Aneurysm at the bifurcation of the left ICA (A). “Black hole” in the treated aneurysm after embolization (B).
Medical implants can make it impossible to examine the abdomen and pelvis - like a stent graft in the aorta and both common iliac arteries in our patient who forgot to mention in the questionnaire that he had undergone stent graft implantation in the past. A pilot sequence clearly showed that pelvic MRI cannot be performed due to a large “black hole” mentioned above. The joint that was operated on with the use of screws can pose a similar problem due to signal loss in some sequences and to the artifacts caused by screws (the so called pile-up artifacts and imperfect fat suppression) which may be so extensive that the interpretation of the images may turn out to be impossible [15] (Figure 21). On the other hand, like in case of materials used in spine surgery, orthopedic materials may produce no artifacts if they are made of polymers blend, e.g. biodegradable interference screws which are not visible on plain films and degrade completely after 2–4 years and only the bone tunnel is visible on MRI (Figure 22).
Figure 21.
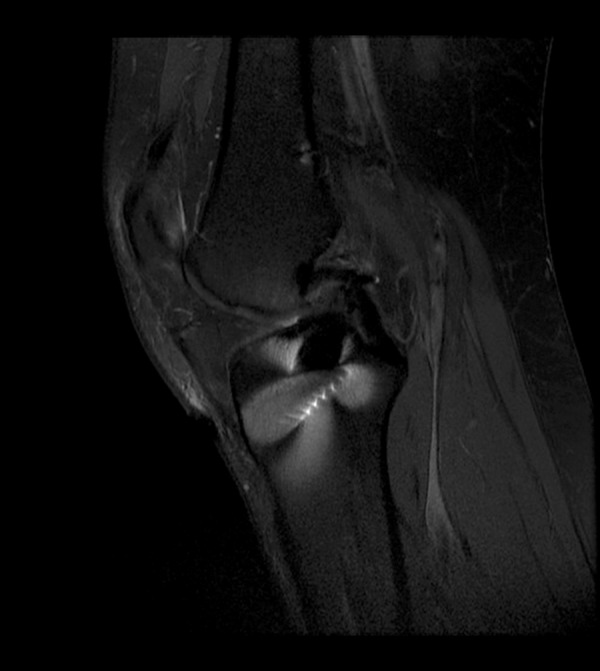
Excessive artifacts in the MRI (FSE, PD + fatsat) of the knee after the reconstruction of the anterior cruciate ligament with the use of stainless steel screws.
Figure 22.

No artifacts in case of polymer biodegradable interference screws.
Sternal wires after thoracic procedures are of less concern as they distort the magnetic field but usually allow to image the thorax. Their MR appearance is similar to that produced by neurosurgical clips presented in Figure 16.
Metallic surgical clips can be almost harmless for imaging in some sequences and projections (Figure 23A) but can distort the examination severely making it impossible to read the most affected slices in the same patient depending on the kind of sequence (Figure 23B, 23C).
Figure 23.
Metallic surgical clip in the abdominal wall, almost harmful in FSE/T2-weighted image in the sagittal plane (A) but disturbing the assessment of the uterus in that 44-year-old woman with cervical cancer (LAVA, post Gad, ax – B, FSE/T1+fatsat, ax – C).
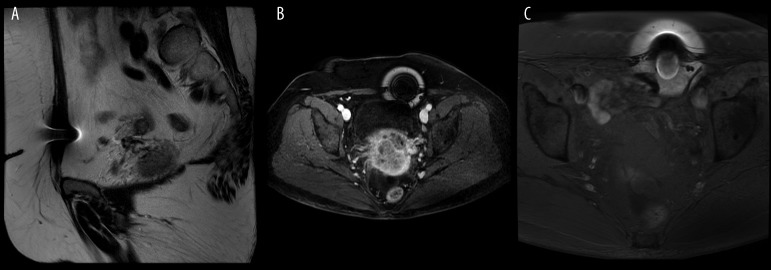
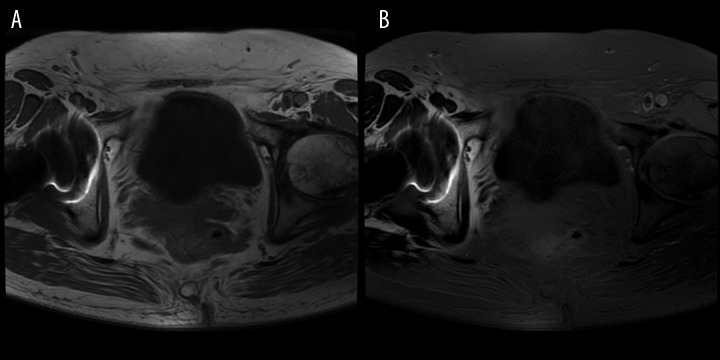
Pelvic MRI can also be disturbed by hip prostheses (Figure 24).
Figure 24.
Right hip prosthesis. FSE/T1, ax (A), FSE/T1+fatsat, ax (B).
Group C
The radiologist is not always informed about the therapies that the examined patients underwent in the past and some of these therapies have an impact on MR imaging with a possibility of revealing unusual findings. The sustained-release intra-vaginal estradiol ring is one of them. It is a contraceptive method as well as a useful therapeutic option in the treatment of vaginal atrophy in postmenopausal women and it appears as a low signal intensity round element in the vagina.
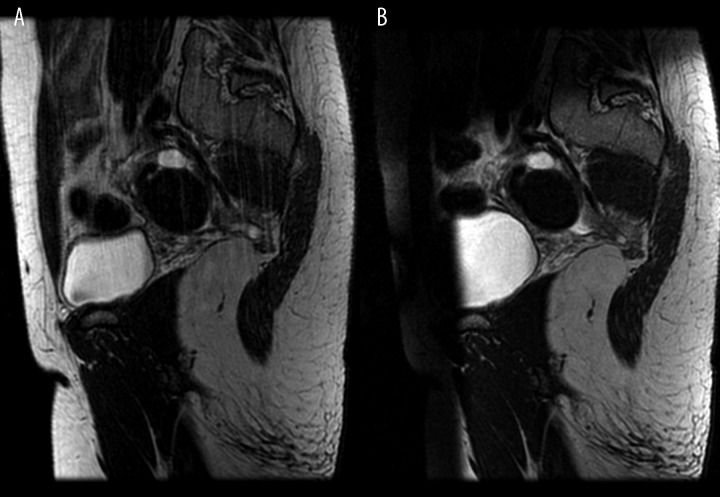
Sometimes the patient does not know what exactly is placed in his orbit after enucleation like in one of our cases in which the patient removed the removable eye ball prosthesis before MRI but there was still some part of it in the orbit (Figure 25).
Figure 25.
Patient with a history of enucleation due to melanoma. FSE/T1 + fatsat, ax (A), FSE/T2, sag (B).
Others
Apart from these three groups of artifacts mentioned above, we may also be forced to deal with artifacts, the occurrence of which indicates a failure of the MRI system [3], e.g. many a time we dealt with artifacts that indicated the failure of coils or the ones that occurred during GRE/T2* sequence and informed us about the failure of the magnet cooling system.
And finally, radiologists should be aware of normal conditions which sometimes may be misleading, mistaken for artifacts, and interfere with establishing diagnosis, like menstrual bleeding in female patients or uterine contractions that occur in everyday life and not only during labor.
Conclusions
Knowledge of different types of artifacts, of their origin and of possible foreign bodies is necessary to eliminate them or to reduce their negative influence on MR images by adjusting acquisition parameters. It is also necessary to take them into consideration when interpreting the images. Some proposals of reducing artifacts were mentioned but describing in detail the procedures to avoid or limit artifacts would go beyond the scope of this paper. However, technical ways to reduce them can be found in the cited literature [1,3,8,15].
Figure 3.
Multiple images of the aorta – ghosting artifact caused by aortal pulsation.
Figure 4.

SE/T1-weighted images after intravenous administration of the contrast material – hyperintense signal caused by arterial pulsation imitates a cerebellar, contrast-enhanced lesion (A – axial plane, B – sagittal plane, C – coronal plane).
Figure 5.
Motion artifacts caused by breathing (A). Saturation band (B) reduces the artifacts and improves image quality.
References
- 1.Graves MJ, Mitchell DG. Body MRI artifacts in clinical practice: a physicist’s and radiologist’s perspective. J Magn Reson Imaging. 2013;38:269–87. doi: 10.1002/jmri.24288. [DOI] [PubMed] [Google Scholar]
- 2.Kathiravan S, Kanakaraj J. A review on potential issues and challenges in MR imaging. Scientific World Journal. 2013;2013:783715. doi: 10.1155/2013/783715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hakky M, Pandey S, Kwak E, Jara H, Erbay SH. Application of basic physics principles to clinical neuroradiology: differentiating artifacts from true pathology on MRI. Am J Roentgenol. 2013;201:369–77. doi: 10.2214/AJR.12.10394. [DOI] [PubMed] [Google Scholar]
- 4.Poustchi-Amin M, Mirowitz SA, Brown JJ, et al. Principles and applications of echo-planar imaging: a review for the general radiologist. Radiographics. 2001;21:767–79. doi: 10.1148/radiographics.21.3.g01ma23767. [DOI] [PubMed] [Google Scholar]
- 5.Hood MN, Ho VB, Smirniotopoulos JG, Szumowski J. Chemical Shift: The Artifact and Clinical Tool Revisited. Radiographics. 1999;19:357–71. doi: 10.1148/radiographics.19.2.g99mr07357. [DOI] [PubMed] [Google Scholar]
- 6.Stuckey SL, Goh TD, Heffernan T, Rowan D. Hyperintensity In the Subarachnoid Space on FLAIR MRI. Am J Roentgenol. 2007;189:913–21. doi: 10.2214/AJR.07.2424. [DOI] [PubMed] [Google Scholar]
- 7.Tartaglino LM, Flanders AE, Vinitski S, Friedman DP. Metallic artifacts on MR images of the postoperative spine: reduction with fast spin-echo techniques. Radiology. 1994;190:565–69. doi: 10.1148/radiology.190.2.8284417. [DOI] [PubMed] [Google Scholar]
- 8.Pierre-Jerome C, Arslan A, Bekkelund SI. MRI of the spine and spinal cord: imaging techniques, normal anatomy, artifacts, and pitfalls. J Manipulative Physiol Ther. 2000;23:470–75. doi: 10.1067/mmt.2000.108819. [DOI] [PubMed] [Google Scholar]
- 9.Cha JG, Hong HS, Park JS, et al. Practical application of iterative decomposition of water and fat with echo asymmetry and least-squares estimation (IDEAL) imaging in minimizing metallic artifacts. Korean J Radiol. 2012;13:332–41. doi: 10.3348/kjr.2012.13.3.332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ruan C. MR artifacts: Mechanism and control. http://ric.uthscsa.edu/personalpages/lancaste/DI2_Projects_2003/MRI_Artifacts.pdf.
- 11.Shapiro L, Harish M, Hargreaves B, et al. Advances in musculoskeletal MRI: technical considerations. J Magn Reson Imaging. 2012;36:775–87. doi: 10.1002/jmri.23629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sacco DC, Steiger DA, Bellon EM, et al. Artifacts caused by cosmetics in MR imaging of the head. Am J Roentgenol. 1987;148:1001–4. doi: 10.2214/ajr.148.5.1001. [DOI] [PubMed] [Google Scholar]
- 13.Fache JS, Price C, Hawbolt EB, Li DK. MR imaging artifacts produced by dental materials. Am J Neuroradiol. 1987;8:837–40. [PMC free article] [PubMed] [Google Scholar]
- 14.Mathew CA, Maller S, Maheshwaran Interactions between magnetic resonance imaging and dental material. J Pharm Bioallied Sci. 2013;5(Suppl 1):S113–16. doi: 10.4103/0975-7406.113309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hargreaves BA, Worters PW, Pauly KB, et al. Metal-induced artifacts in MRI. Am J Roentgenol. 2011;197:547–55. doi: 10.2214/AJR.11.7364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Costa ALF, Appenzeller S, Yasuda CL, et al. Artifacts in brain magnetic resonance imaging due to metallic dental objects. Med Oral Patol Oral Cir Bucal. 2009;14:E278–82. [PubMed] [Google Scholar]
- 17.Lavinio A, Harding S, Van Der Boogaard F, et al. Magnetic field interactions in adjustable hydrocephalus shunts. J Neurosurg Pediatr. 2008;2:222–28. doi: 10.3171/PED/2008/2/9/222. [DOI] [PubMed] [Google Scholar]
- 18.Sundseth J, Jacobsen EA, Kolstad F, et al. Magnetic resonance imaging evaluation after implantation of a titanium cervical disc prosthesis: a comparison of 1.5 and 3 Tesla magnet strength. Eur Spine J. 2013;22:2296–302. doi: 10.1007/s00586-013-2994-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Knott PT, Mardjetko SM, Kim RH, et al. A comparison of magnetic and radiographic imaging artifact after using three types of metal rods: stainless steel, titanium, and vitallium. Spine J. 2010;10:789–94. doi: 10.1016/j.spinee.2010.06.006. [DOI] [PubMed] [Google Scholar]
- 20.Ernstberger T, Buchhorn G, Heidrich G. Artifacts in spine magnetic resonance imaging due to different intervertebral test spacers: an in vitro evaluation of magnesium versus titanium and carbon-fiber-reinforced polymers as biomaterials. Neuroradiology. 2009;51:525–29. doi: 10.1007/s00234-009-0537-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Saatci I, Cekirge HS, Ciceri EF, et al. CT and MR imaging findings and their implications in the follow-up of patients with intracranial aneurysms treated with endosaccular occlusion with onyx. Am J Neuroradiol. 2003;24:567–78. [PMC free article] [PubMed] [Google Scholar]