Abstract
Aim
Prior evidence observed no predictive utility of coronary CT angiography (CCTA) over the coronary artery calcium score (CACS) and the Framingham risk score (FRS), among asymptomatic individuals. Whether the prognostic value of CCTA differs for asymptomatic patients, when stratified by CACS severity, remains unknown.
Methods and results
From a 12-centre, 6-country observational registry, 3217 asymptomatic individuals without known coronary artery disease (CAD) underwent CACS and CCTA. Individuals were categorized by CACS as: 0–10, 11–100, 101–400, 401–1000, >1000. For CCTA analysis, the number of obstructive vessels—as defined by the per-patient presence of a ≥50% luminal stenosis—was used to grade the extent and severity of CAD. The incremental prognostic value of CCTA over and above FRS was measured by the likelihood ratio (LR) χ2, C-statistic, and continuous net reclassification improvement (NRI) for prediction, discrimination, and reclassification of all-cause mortality and non-fatal myocardial infarction. During a median follow-up of 24 months (25th–75th percentile, 17–30 months), there were 58 composite end-points. The incremental value of CCTA over FRS was demonstrated in individuals with CACS >100 (LRχ2, 25.34; increment in C-statistic, 0.24; NRI, 0.62, all P < 0.001), but not among those with CACS ≤100 (all P > 0.05). For subgroups with CACS >100, the utility of CCTA for predicting the study end-point was evident among individuals whose CACS ranged from 101 to 400; the observed predictive benefit attenuated with increasing CACS.
Conclusion
Coronary CT angiography provides incremental prognostic utility for prediction of mortality and non-fatal myocardial infarction for asymptomatic individuals with moderately high CACS, but not for lower or higher CACS.
Keywords: Coronary computed tomographic angiography, Coronary artery calcium scoring, Framingham risk score, Asymptomatic, Prognostic
Introduction
Office-based cardiovascular event prediction algorithms have been utilized for future risk stratification in asymptomatic populations, and are useful for identifying individuals who will benefit from preventive therapies.1 Yet, these clinical prediction methods are less effective for identifying specific individuals who are at risk for adverse clinical events.2–4 Recently, non-invasive imaging modalities for the identification of subclinical atherosclerosis have emerged as robust methods that augment identification of individuals at risk, incremental to office-based risk assessments.5 Among these modalities, the coronary artery calcium score (CACS) has been widely used, and multiple population-based studies demonstrated that CACS provided powerful prognostic information across different age categories, gender, and ethnicities.6–8
Recently, coronary computed tomographic angiography (CCTA) has emerged as an non-invasive cardiovascular imaging modality that enables visualization of both calcified and non-calcified atherosclerotic plaques, with high diagnostic performance for identification and exclusion of coronary luminal stenoses.9,10 Prior investigations have examined the utility of CCTA for assessing future cardiovascular risk among asymptomatic individuals.11–15 Recently, our investigative group observed no added benefit of CCTA for risk stratification beyond clinical risk factor scoring and CACS.16 Nevertheless, given the heterogeneity of this population, it remains to be clarified whether the prognostic value of CCTA differs according to varying CACS severity. Consequently, in a large multinational prospective study, we sought to determine the prognostic value of CCTA according to varying CACS categories in a population of asymptomatic patients.
Methods
Design overview, setting, and participants
The study design and rationale of the CONFIRM (COronary CT Angiography EvaluatioN For Clinical Outcomes: An InteRnational Multicenter) registry has been described elsewhere.17 In brief, the CONFIRM registry was designed to evaluate the ability of CCTA findings to predict mortality and major adverse cardiac events. Overall, 27 125 patients who underwent CCTA at 12 centres in 6 countries (Canada, Germany, Italy, South Korea, Switzerland, and USA) were initially enrolled between February 2003 and December 2009. Inclusion criteria were age 18 years or older, availability of CCTA by scanner with 64-detector rows or greater, and the presence of interpretable CCTA. For the purpose of this study, at baseline, persons were deemed ineligible for inclusion if they had previously experienced chest pain (n = 14 063), unknown symptom status (n = 4685), a prior history of myocardial infarction (MI), coronary revascularization, and cardiac transplantation (n = 752), or the absence of concurrent CACS or follow-up data for all-cause mortality or non-fatal MI (n = 4373). Clinical indications for CCTA in individuals without chest pain in the CONFIRM registry were for the assessment of coronary artery disease (CAD) in individuals with a history of peripheral arterial disease, cerebrovascular disease, or multiple CAD risk factors, individuals with pre-operative evaluation or pre-electrophysiological procedure evaluation (e.g. left atrial appendage evaluation, pulmonary vein mapping), or individuals with non-major congenital heart disease including atrial septal defect or ventricular septal defect.
Hence, the analytic sample consisted of 3217 asymptomatic individuals from seven centres in five countries (Canada, Italy, Germany, South Korea, and USA) for the current study. Each of the study centres' institutional review boards approved the study protocol, and all of the participants provided informed consent.
Data acquisition and image analysis
Multi-detector row CT scanners consisting of 64-rows or greater acquired CACS and CCTA. Data acquisition and image post-processing, and data interpretation, were performed according to the guideline of the Society of Cardiovascular Computed Tomography (SCCT).18,19 The coronary artery calcium score was measured using the scoring system (in units) described by Agatston et al.20 The mean dose length product derived from CCTA and coronary artery calcium scan was 726 ± 316 mGy × cm.
The definition of coronary atherosclerosis by CCTA analysis was any tissue structures >1 mm2, which were either within the lumen of the coronary artery or adjacent to the coronary artery lumen that could be distinguished from neighbouring epicardial fat, pericardial tissue, or the artery lumen itself. All identified lesions were examined by maximum-intensity-projection and multi-planar reconstruction techniques along multiple longitudinal axes and in the transverse plane. Identified plaques were assigned according to a modified 16-segment American Heart Association coronary tree model:21 left main; proximal, mid, and distal left anterior descending (LAD) artery; first and second diagonal branches of the LAD; proximal and distal left circumflex artery; first and second obtuse marginal branches of the left circumflex artery; proximal, mid, and distal right coronary artery; posterior descending artery; and posterolateral branches (left or right). We defined obstructive CAD as coronary artery segments exhibiting plaque with a luminal diameter stenosis ≥50%, and non-obstructive CAD as coronary artery segments displaying plaque with a luminal diameter stenosis <50%. We additionally categorized obstructive CAD as 1-vessel disease (VD), 2-VD, and 3-VD or left main disease.
Patient follow-up
Patients were followed prospectively for 2.5 years. During this study, the primary outcome measure was a composite of all-cause mortality and non-fatal MI. Trained personnel adjudicated all deaths by direct interview with physicians, next-of-kin, and/or witnesses, by review of hospital records, or by querying of national medical databases. Non-fatal MI was defined by the Universal Definition of Myocardial Infarction.22 All the patients were questioned using a scripted interview, and all procedures were confirmed by review of the patients' medical record.
Statistical analysis
Continuous variables are expressed as means ± standard deviation (SD), and categorical variables are presented as counts with proportions. Differences between continuous variables were analysed by Student's t-test and those between categorical variables by the χ2 test or Fisher's exact test, as appropriate. A 2.5-year horizon period was employed for the analyses. Cumulative event rates were calculated using the Kaplan–Meier estimator and compared using the log-rank test.
On the background of CACS, subjects were classified according to the following categories: 0–10, 11–100, and >100. Furthermore, subjects with CACS >100 were categorized as 101–400, 401–1000, and >1000.23 For each CACS category, the incremental prognostic value of CCTA, above and beyond an office-based risk stratification algorithm, was evaluated. Specifically, for the office-based risk stratification algorithm, we categorized individuals as low (<10%), low-intermediate (10–15%), high-intermediate (16–20%), and high (>20%) risk according to published Framingham 10-year coronary heart disease risk scores.24
Statistical significance for the added prognostic value of each CCTA category was evaluated using the likelihood ratio (LR) χ2 test,25 the difference in C-statistic (ΔC-statistic),26,27 and continuous net reclassification improvement (cNRI).28,29 A standard bootstrap method was employed to generate the corresponding confidence intervals (CIs) for estimates. A two-tailed P-value <0.05 was considered statistically significant. All analyses were performed using SAS (version 9.2, SAS Institute, Inc., Cary, NC, USA).
Results
Baseline characteristics
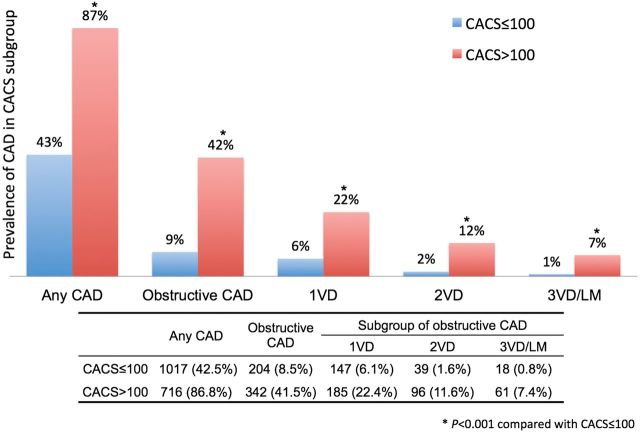
During a median follow-up of 24 months (25th–75th percentile: 17–30 months), there were 58 composite end-points among 3217 individuals (1.8% during 2.5 years). Table 1 reports the baseline cardiovascular risk factors, stratified by CACS categories above and below 100. Subjects with CACS >100 tended to be older, male, and had a higher prevalence of hypertension, diabetes, current smoking, and dyslipidaemia (all P < 0.05). Figure 1 illustrates the prevalence of CAD as well as extent and severity among patients with CACS above and below 100. As expected, prevalent any CAD including both non-obstructive and obstructive was higher in those with a CACS >100 (87 vs. 43%, P < 0.001). The proportion of individuals with obstructive CAD was also higher on the background of CACS >100 (42 vs. 9%, P < 0.001). Likewise, the percentage in the number of increasing stenosed vessels was higher in patients with a CACS >100 when compared with those whose CACS was ≤100 (all, P < 0.001).
Table 1.
Baseline characteristics of study population according to coronary artery calcium score categories
| Variables | Total (n = 3217) | CACS |
P-value | |
|---|---|---|---|---|
| ≤100 (n = 2392) | >100 (n = 825) | |||
| Age (years) | 57 ± 12 | 55 ± 11 | 62 ± 11 | <0.001 |
| Gender (male) | 2031 (63%) | 1430 (60%) | 601 (73%) | <0.001 |
| Hypertension | 1458 (46%) | 994 (42%) | 464 (57%) | <0.001 |
| Diabetes | 431 (13%) | 253 (11%) | 178 (22%) | <0.001 |
| Current smoking | 432 (13%) | 295 (12%) | 137 (17%) | 0.001 |
| BMI (kg/m2) | 27 ± 5 | 27 ± 5 | 28 ± 5 | 0.001 |
| Dyslipidaemia | 1715 (54%) | 1206 (51%) | 509 (62%) | <0.001 |
| Total cholesterol | 195 ± 45 | 197 ± 45 | 183 ± 42 | <0.001 |
| HDL cholesterol | 54 ± 16 | 54 ± 16 | 49 ± 15 | <0.001 |
| LDL cholesterol | 119 ± 37 | 121 ± 37 | 110 ± 35 | <0.001 |
Continuous values are mean ± SD and categorical values are number and percentage (%).
BMI, indicates body mass index; CACS, coronary artery calcium score; HDL, high-density lipoprotein; LDL, low-density lipoprotein; n, number.
Figure 1.
Prevalence of coronary artery disease evaluated by coronary computed tomographic angiography according to coronary artery calcium score categories. Number and percentage (%). Any CAD indicates obstructive and non-obstructive coronary artery disease; CACS, coronary artery calcium score; CCTA, coronary CT angiography; LM, left main disease; VD, vessel disease.
Clinical outcomes
Over the course of the study period, the overall Kaplan–Meier 2.5-year cumulative event estimate was 2.3% (95% CI, 1.9–2.8%) (Table 2). Specifically, the Kaplan–Meier 2.5-year cumulative event estimate was 1.3% among individuals with CACS ≤100, increasing to 5.1% (95% CI, 3.7–6.9%) among individuals with CACS >100 (log-rank, P < 0.001). Among the subgroups with CACS >100, the composite event estimates increased proportionally with increasing CACS categories.
Table 2.
Composite outcomes of all-cause mortality and non-fatal myocardial infarction according to coronary artery calcium score categories during 2.5-year follow-up period
| Number of subjects | Number of composite outcomes (number of MIs) | Kaplan–Meier 2.5-year cumulative event estimates (95% CI) | |
|---|---|---|---|
| Total | 3217 | 58 (12) | 2.3% (1.9–2.8) |
| 0≤ CACS ≤10 | 1818 | 19 (2) | 1.3% (0.9–2.0) |
| 10< CACS ≤100 | 574 | 6 (1) | 1.3% (0.6–2.7) |
| CACS >100 | 825 | 33 (9) | 5.1% (3.7–6.9) |
| 100< CACS ≤400 | 472 | 14 (4) | 3.6% (2.1–5.8) |
| 400< CACS ≤1000 | 217 | 12 (2) | 6.8% (4.0–11.2) |
| CACS >1000 | 136 | 7 (3) | 7.8% (4.1–14.0) |
CACS, indicates coronary artery calcium score; CI, confidence interval; No, number; MIs, non-fatal myocardial infarctions.
Incremental value of coronary CT angiography in addition to the Framingham risk score
In Table 3, adding CCTA to a model including the FRS significantly improved the prediction of the composite end-point for those with CACS >100: LRχ2 = 25.34, cNRI = 0.62 (95% CI, 0.24–1.02), and ΔC-statistic = 0.24 (95% CI, 0.11–0.37), all P < 0.001. Conversely, the incremental value of CCTA over and above FRS was non-significant in patients with CACS ≤100: LRχ2 = 6.30 and 2.84 among individuals with a CACS of 0–10, and 11–100, both P > 0.05. Continuous NRI and the ΔC-statistic also demonstrated negligible added benefit of CCTA over FRS in these subgroups.
Table 3.
Incremental prognostic benefit of coronary computed tomographic angiography over Framingham risk scoring in predicting 2.5-Year Risk of composite outcome of all-cause mortality and non-fatal myocardial infarction according to coronary artery calcium score categories
| CACS categories | 0–10 | 11–100 | >100 | Subgroup of CACS >100 |
||
|---|---|---|---|---|---|---|
| 101–400 | 401–1000 | >1000 | ||||
| Number of subjects (number of events) | 1818 (19) | 574 (6) | 825 (33) | 472 (14) | 217 (12) | 136 (7) |
| Likelihood ratio tests | ||||||
| Likelihood ratio χ2 | 6.30 | 2.84 | 25.34 | 14.68 | 9.22 | 5.36 |
| P-value | 0.178 | 0.584 | <0.001 | 0.005 | 0.056 | 0.252 |
| cNRIs | ||||||
| Proportion of event correctly reclassified | −0.16 | 0.31 | 0.07 | 0.05 | 0.70 | 0.59 |
| Proportion of non-event correctly reclassified | 0.56 | −0.23 | 0.55 | 0.70 | 0.04 | −0.02 |
| cNRI (95% CI) | 0.39 (−0.04–0.94) | 0.08 (−1.24–0.77) | 0.62 (0.24–1.02) | 0.74 (0.23–1.38) | 0.74 (0.12–1.17) | 0.57 (−0.23–1.18) |
| P-value | 0.092 | 0.300 | <0.001 | 0.008 | 0.010 | 0.160 |
| C-statistics | ||||||
| C of FRS (95% CI) | 0.64 (0.53–0.75) | 0.68 (0.40–0.97) | 0.53 (0.42–0.64) | 0.64 (0.49–0.78) | 0.58 (0.39–0.77) | 0.56 (0.34–0.78 |
| C of FRS + CCTA (95% CI) | 0.71 (0.59–0.83) | 0.73 (0.50–0.96) | 0.77 (0.69–0.85) | 0.77 (0.61–0.92) | 0.75 (0.63–0.87) | 0.78 (0.67–0.90) |
| ΔC (95% CI) | 0.07(−0.02–0.17) | 0.05 (−0.05–0.14) | 0.24 (0.11–0.37) | 0.13 (0.03–0.23) | 0.17 (−0.03–0.37) | 0.23 (0.05–0.40) |
| P-value | 0.145 | 0.312 | <0.001 | 0.011 | 0.088 | 0.013 |
C, indicates C-statistics; CACS, coronary artery calcium score; CCTA, coronary computed tomographic angiography; ΔC, difference in C-statistic; FRS, Framingham Risk Score; cNRI, continuous net reclassification improvement; CI, confidence interval.
Among patients with CACS >100, the incremental benefit of CCTA over FRS was particularly evident for those with a CACS between 101 and 400. The LRχ2 was 14.68 (P = 0.005) and the ability of CCTA to correctly reclassify and discriminate individuals from FRS was significant: cNRI = 0.74 (95% CI, 0.23–1.38, P = 0.008) and ΔC-statistic = 0.13 (95% CI, 0.03–0.23, P = 0.011). However, the incremental value of CCTA for predicting the composite end-point was attenuated among patients when CACS increased >400 (Table 3). The LRχ2 gradually declined becoming marginally non-significant for individuals with a CACS between 401 and 1000 (9.22, P = 0.06), and in those with CACS >1000 (5.36, P = 0.25). Likewise, cNRI was mitigated in patients whose CACS was >1000 (0.57, 95% CI, −0.23–1.18, P = 0.16), albeit with improved discrimination (ΔC-statistic = 0.23, P = 0.01).
Discussion
In this global multicentre study, we set out to determine whether CCTA improved risk prediction for future fatal and non-fatal events over FRS when stratified by CACS severity, in an asymptomatic population. The major finding was that CCTA improved risk prediction for future fatal and non-fatal events by adding further prognostic information to the FRS in patients whose CACS was >100.
The added prognostic value of CCTA over the FRS was particularly proven in subjects with a CACS between 101 and 400. Most reclassification of this subgroup occurred in the non-event proportion (0.70 of 0.74), suggesting most individuals were correctly reclassified to a lower-risk category by CCTA. The incremental benefit of CCTA over FRS may, in large, be attributable to the diagnostic accuracy within this CACS category.30 In addition, individuals with a CACS between 101 and 400 were accompanied by intermediate event risk (3.6%), allowing CCTA to discriminate future risk. Therefore, CCTA may be considered for reclassification especially in this subset of individuals. Forthcoming studies are needed to test this notion.
Although the added benefit of CCTA over FRS was statistically significant in patients with CACS >100, it was limited among individuals whose CAC exceeded 400. Modest improvements in reclassification occurred in individuals with CACS between 401 and 1000, and discrimination for individuals with CACS >1000. Notably, the lack of a beneficial impact of CCTA among individuals with a very high calcium score may likely be afforded to a decreased diagnostic accuracy of CCTA due to beam hardening and blooming artefacts.31 In a meta-analysis, Abdulla et al.30 documented that the overall diagnostic accuracy of CCTA was markedly reduced in patients with CACS >400. In one other study,32 the diagnostic precision of CCTA for detecting obstructive CAD diminished in patients with severe calcification (i.e. CACS >600). Consequently, other functional tests, for instance, myocardial perfusion imaging or exercise stress testing, may need to be considered instead of CCTA in this population.
Likewise, the incremental benefit of CCTA over and above FRS was negligible in patients with CACS ≤100. Most (74%) of the study population consisted of patients with a CACS ≤100, which is fitting with past large-scale epidemiological studies.6,33 This finding may be explained by the inability of CCTA to reclassify individuals to a lower-risk category in this population with low event rates. Indeed, the Kaplan–Meier 2.5-year event estimate for individuals with CACS ≤100 was only 1.3% and which was significantly lower than those with CACS >100. Large-scale epidemiological studies have also reported a very low risk for persons in this category.6,33,34 Even in a symptomatic population, patients with CACS ≤100 have a very low probability (<2%) of myocardial ischaemia on the nuclear stress test.35,36 Based on Bayes theorem, it may be challenging for CCTA to provide any further incremental value in this very-low-risk population compared with, for example, intermediate risk patients with CACS 101–400.37 Therefore, it is questionable whether CCTA should also be performed in populations whose CACS ≤100 for further risk stratification. Rather, lifestyle modification and non-pharmacological interventions should be recommended for this population. Reassessment of coronary plaque burden using only CACS could further be considered in 3–5 years.38,39
Nevertheless, the current study observations may have important clinical ramifications. Early studies with CCTA employed non-negligible doses of radiation that were similar, or even higher, than current generation nuclear stress testing; doses that contrasted unfavourably to the low-dose CACS.40 However, recent technological advances in CCTA now enable performance of CCTA at doses even lower than CACS, and can now often be performed in ranges <1 mSv.41,42 Furthermore, CCTA can directly and accurately identify location and severity of coronary plaque, while a relationship between CACS and severity of luminal stenosis is weak, especially in patients with acute coronary syndrome.43,44 Recent publications also showed clinical importance of vulnerable plaque features including non-calcified plaque, which was identified by CCTA.45,46 Therefore, future studies evaluating plaque characteristics by CCTA using very low radiation dose image acquisition techniques may identify improved prognostic utility beyond CACS and FRS in asymptomatic populations.
This study had some limitations that bear mentioning. Given the observational nature of the study, the potential biases—including population heterogeneity, inter-observer variability in CCTA diagnosis, as well as other unobserved confounders, cannot be dismissed. To minimize selection bias, we prospectively employed standardized data definitions and only included experienced CCTA centres whereby persons with expert proficiency led acquisition and interpretation of all CCTAs in the current registry.17 While this cohort is the largest global multicentre CCTA study to date, lack of added prognostic value in patients with CACS <100 and >400 may be secondary to a reduced study sample size and limited follow-up duration in these subgroups. Also, considering FRS reflects 10-year risk estimate, a 2.5-year follow-up duration of the current study limits long-term prognostic utility of CCTA when added to FRS predictors. Future studies will be needed to fully address these questions, and further follow-up this study cohort along with an expansion of the current registry size is already underway.
Conclusions
For asymptomatic individuals with moderately elevated CACS, CCTA improves prediction, discrimination and reclassification for risk of future fatal and non-fatal events above and beyond clinical risk assessment. Coronary CT angiography does not reliably improve risk stratification for individuals with lower or higher CACS.
Funding
Research reported in this publication was supported by the Heart Lung and Blood Institute of the National institutes of Health (Bethesda, MD, USA) under award number R01 HL115150. This work was supported by the IT R&D program of MSIP/KEIT. [10044910, Development of Multi-modality Imaging and 3D Simulation-Based Integrative Diagnosis-Treatment Support Software System for Cardiovascular Diseases. This study was also funded, in part, by a generous gift from the Dalio Institute of Cardiovascular Imaging (New York, NY, USA) and the Michael Wolk Foundation (New York, NY, USA). NRF/MSIP (This research was supported by Leading Foreign Research Institute Recruitment Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Science, ICT & Future Planning (MSIP) (2012027176).
Conflict of interest: none declared.
References
- 1.Stone NJ, Robinson JG, Lichtenstein AH, Bairey Merz CN, Blum CB, Eckel RH, Goldberg AC, Gordon D, Levy D, Lloyd-Jones DM, McBride P, Schwartz JS, Shero ST, Smith SC, Watson K, Wilson PWF. 2013 ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults. J Am Coll Cardiol. 2014;63:2889–2934. doi: 10.1016/j.jacc.2013.11.002. [DOI] [PubMed] [Google Scholar]
- 2.Akosah KO, Schaper A, Cogbill C, Schoenfeld P. Preventing myocardial infarction in the young adult in the first place: how do the national cholesterol education panel iii guidelines perform? J Am Coll Cardiol. 2003;41:1475–1479. doi: 10.1016/s0735-1097(03)00187-6. [DOI] [PubMed] [Google Scholar]
- 3.Hecht HS, Superko HR. Electron beam tomography and national cholesterol education program guidelines in asymptomatic women. J Am Coll Cardiol. 2001;37:1506–1511. doi: 10.1016/s0735-1097(01)01211-6. [DOI] [PubMed] [Google Scholar]
- 4.Nasir K, Michos ED, Blumenthal RS, Raggi P. Detection of High-Risk Young Adults and Women by Coronary Calcium and National Cholesterol Education Program Panel III Guidelines. J Am Coll Cardiol. 2005;46:1931–1936. doi: 10.1016/j.jacc.2005.07.052. [DOI] [PubMed] [Google Scholar]
- 5.Greenland P, Alpert JS, Beller GA, Benjamin EJ, Budoff MJ, Fayad ZA, Foster E, Hlatky MA, Hodgson JM, Kushner FG, Lauer MS, Shaw LJ, Smith SC, Jr, Taylor AJ, Weintraub WS, Wenger NK American College of Cardiology Foundation, American Heart Association Task Force on Practice Guidelines, American Society of Echocardiography, American Society of Nuclear Cardiology, Imaging SoA, Prevention, Angiography SfC, Interventions, Society of Cardiovascular Computed Tomography, Society for Cardiovascular Magnetic Resonance. 2010 ACCF/AHA Guideline for Assessment of Cardiovascular Risk in Asymptomatic Adults. J Am Coll Cardiol. 2010 doi: 10.1016/j.jacc.2010.09.001. j.jacc.2010.2009.2001. [DOI] [PubMed] [Google Scholar]
- 6.Detrano R, Guerci AD, Carr JJ, Bild DE, Burke G, Folsom AR, Liu K, Shea S, Szklo M, Bluemke DA, O'Leary DH, Tracy R, Watson K, Wong ND, Kronmal RA. Coronary calcium as a predictor of coronary events in four racial or ethnic groups. N Engl J Med. 2008;358:1336–1345. doi: 10.1056/NEJMoa072100. [DOI] [PubMed] [Google Scholar]
- 7.Budoff MJ, Shaw LJ, Liu ST, Weinstein SR, Mosler TP, Tseng PH, Flores FR, Callister TQ, Raggi P, Berman DS. Long-Term Prognosis associated with coronary calcification: observations from a registry of 25,253 patients. J Am Coll Cardiol. 2007;49:1860–1870. doi: 10.1016/j.jacc.2006.10.079. [DOI] [PubMed] [Google Scholar]
- 8.Yeboah J, McClelland RL, Polonsky TS, Burke GL, Sibley CT, O'Leary D, Carr JJ, Goff DC, Greenland P, Herrington DM. Comparison of novel risk markers for improvement in cardiovascular risk assessment in intermediate-risk individuals. JAMA. 2012;308:788–795. doi: 10.1001/jama.2012.9624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Meijboom WB, van Mieghem CA, Mollet NR, Pugliese F, Weustink AC, van Pelt N, Cademartiri F, Nieman K, Boersma E, de Jaegere P, Krestin GP, de Feyter PJ. 64-slice computed tomography coronary angiography in patients with high, intermediate, or low pretest probability of significant coronary artery disease. J Am Coll Cardiol. 2007;50:1469–1475. doi: 10.1016/j.jacc.2007.07.007. [DOI] [PubMed] [Google Scholar]
- 10.Min JK, Shaw LJ, Berman DS. The present state of coronary computed tomography angiography a process in evolution. J Am Coll Cardiol. 2010;55:957–965. doi: 10.1016/j.jacc.2009.08.087. [DOI] [PubMed] [Google Scholar]
- 11.Choi E-K, Choi SI, Rivera JJ, Nasir K, Chang S-A, Chun EJ, Kim H-K, Choi D-J, Blumenthal RS, Chang H-J. Coronary computed tomography angiography as a screening tool for the detection of occult coronary artery disease in asymptomatic individuals. J Am Coll Cardiol. 2008;52:357–365. doi: 10.1016/j.jacc.2008.02.086. [DOI] [PubMed] [Google Scholar]
- 12.Kornowski R, Bachar GN, Dvir D, Fuchs S, Atar E. Angiographic findings and clinical outcomes in asymptomatic patients with severe obstructive atherosclerosis on computed tomography angiography. Isr Med Assoc J. 2008;10:627–633. [PubMed] [Google Scholar]
- 13.Cho I, Suh JW, Chang HJ, Kim KI, Jeon EJ, Choi SI, Cho YS, Youn TJ, Chae IH, Kim CH, Choi DJ. Prevalence and prognostic implication of non-calcified plaque in asymptomatic population with coronary artery calcium score of zero. Korean Circ J. 2013;43:154–160. doi: 10.4070/kcj.2013.43.3.154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Djaberi R, Schuijf JD, Boersma E, Kroft LJM, Pereira AM, Romijn JA, Scholte AJ, Jukema JW, Bax JJ. Differences in atherosclerotic plaque burden and morphology between type 1 and 2 diabetes as assessed by multislice computed tomography. Diabetes Care. 2009;32:1507–1512. doi: 10.2337/dc09-0320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zeina A, Odeh M, Rosenschein U, Zaid G, Barmeir E. Coronary artery disease among asymptomatic diabetic and nondiabetic patients undergoing coronary computed tomography angiography. Coron Artery Dis. 2008;19:37. doi: 10.1097/MCA.0b013e3282f2f19e. [DOI] [PubMed] [Google Scholar]
- 16.Cho I, Chang HJ, Sung JM, Pencina MJ, Lin FY, Dunning AM, Achenbach S, Al-Mallah M, Berman DS, Budoff MJ, Callister TQ, Chow BJ, Delago A, Hadamitzky M, Hausleiter J, Maffei E, Cademartiri F, Kaufmann P, Shaw LJ, Raff GL, Chinnaiyan KM, Villines TC, Cheng V, Nasir K, Gomez M, Min JK, Investigators C. Coronary computed tomographic angiography and risk of all-cause mortality and nonfatal myocardial infarction in subjects without chest pain syndrome from the CONFIRM Registry (coronary CT angiography evaluation for clinical outcomes: an international multicenter registry) Circulation. 2012;126:304–313. doi: 10.1161/CIRCULATIONAHA.111.081380. [DOI] [PubMed] [Google Scholar]
- 17.Min JK, Dunning A, Lin FY, Achenbach S, Al-Mallah MH, Berman DS, Budoff MJ, Cademartiri F, Callister TQ, Chang HJ, Cheng V, Chinnaiyan KM, Chow B, Delago A, Hadamitzky M, Hausleiter J, Karlsberg RP, Kaufmann P, Maffei E, Nasir K, Pencina MJ, Raff GL, Shaw LJ, Villines TC. Rationale and design of the CONFIRM (COronary CT Angiography EvaluatioN For Clinical Outcomes: An InteRnational Multicenter) Registry. J Cardiovasc Comput Tomogr. 2011;5:84–92. doi: 10.1016/j.jcct.2011.01.007. [DOI] [PubMed] [Google Scholar]
- 18.Hendel RC, Patel MR, Kramer CM, Poon M, Carr JC, Gerstad NA, Gillam LD, Hodgson JM, Kim RJ, Lesser JR, Martin ET, Messer JV, Redberg RF, Rubin GD, Rumsfeld JS, Taylor AJ, Weigold WG, Woodard PK, Brindis RG, Douglas PS, Peterson ED, Wolk MJ, Allen JM. ACCF/ACR/SCCT/SCMR/ASNC/NASCI/SCAI/SIR 2006 appropriateness criteria for cardiac computed tomography and cardiac magnetic resonance imaging: a report of the American College of Cardiology Foundation Quality Strategic Directions Committee Appropriateness Criteria Working Group, American College of Radiology, Society of Cardiovascular Computed Tomography, Society for Cardiovascular Magnetic Resonance, American Society of Nuclear Cardiology, North American Society for Cardiac Imaging, Society for Cardiovascular Angiography and Interventions, and Society of Interventional Radiology. J Am Coll Cardiol. 2006;48:1475–1497. doi: 10.1016/j.jacc.2006.07.003. [DOI] [PubMed] [Google Scholar]
- 19.Mark DB, Berman DS, Budoff MJ, Carr JJ, Gerber TC, Hecht HS, Hlatky MA, Hodgson JM, Lauer MS, Miller JM, Morin RL, Mukherjee D, Poon M, Rubin GD, Schwartz RS. ACCF/ACR/AHA/NASCI/SAIP/SCAI/SCCT 2010 expert consensus document on coronary computed tomographic angiography: a report of the American College of Cardiology Foundation Task Force on Expert Consensus Documents. Circulation. 2010;121:2509–2543. doi: 10.1161/CIR.0b013e3181d4b618. [DOI] [PubMed] [Google Scholar]
- 20.Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M, Jr, Detrano R. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol. 1990;15:827–832. doi: 10.1016/0735-1097(90)90282-t. [DOI] [PubMed] [Google Scholar]
- 21.Austen WG, Edwards JE, Frye RL, Gensini GG, Gott VL, Griffith LS, McGoon DC, Murphy ML, Roe BB. A reporting system on patients evaluated for coronary artery disease. Report of the Ad Hoc Committee for Grading of Coronary Artery Disease, Council on Cardiovascular Surgery, American Heart Association. Circulation. 1975;51:5–40. doi: 10.1161/01.cir.51.4.5. [DOI] [PubMed] [Google Scholar]
- 22.Thygesen K, Alpert JS, White HD Joint ESCAAHAWHFTFftRoMI. Universal definition of myocardial infarction. Eur Heart J. 2007;28:2525–2538. doi: 10.1093/eurheartj/ehm355. [DOI] [PubMed] [Google Scholar]
- 23.Greenland P, Bonow RO, Brundage BH, Budoff MJ, Eisenberg MJ, Grundy SM, Lauer MS, Post WS, Raggi P, Redberg RF, Rodgers GP, Shaw LJ, Taylor AJ, Weintraub WS. American College of Cardiology Foundation Clinical Expert Consensus Task F, Society of Atherosclerosis I, Prevention, Society of Cardiovascular Computed T. ACCF/AHA 2007 clinical expert consensus document on coronary artery calcium scoring by computed tomography in global cardiovascular risk assessment and in evaluation of patients with chest pain: a report of the American College of Cardiology Foundation Clinical Expert Consensus Task Force (ACCF/AHA Writing Committee to Update the 2000 Expert Consensus Document on Electron Beam Computed Tomography) developed in collaboration with the Society of Atherosclerosis Imaging and Prevention and the Society of Cardiovascular Computed Tomography. J Am Coll Cardiol. 2007;49:378–402. doi: 10.1016/j.jacc.2006.10.001. [DOI] [PubMed] [Google Scholar]
- 24.Wilson PWF, D'Agostino RB, Levy D, Belanger AM, Silbershatz H, Kannel WB. Prediction of coronary heart disease using risk factor categories. Circulation. 1998;97:1837–1847. doi: 10.1161/01.cir.97.18.1837. [DOI] [PubMed] [Google Scholar]
- 25.Vickers A, Cronin A, Begg C. One statistical test is sufficient for assessing new predictive markers. BMC Med Res Methodol. 2011;11:13. doi: 10.1186/1471-2288-11-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pencina MJ, D'Agostino RB. Overall C as a measure of discrimination in survival analysis: model specific population value and confidence interval estimation. Stat Med. 2004;23:2109–2123. doi: 10.1002/sim.1802. [DOI] [PubMed] [Google Scholar]
- 27.Harrell FE, Jr, Lee KL, Mark DB. Multivariable prognostic models: issues in developing models, evaluating assumptions and adequacy, and measuring and reducing errors. Stat Med. 1996;15:361–387. doi: 10.1002/(SICI)1097-0258(19960229)15:4<361::AID-SIM168>3.0.CO;2-4. [DOI] [PubMed] [Google Scholar]
- 28.Steyerberg EW, Pencina MJ. Reclassification calculations for persons with incomplete follow-up. Ann Intern Med. 2010;152:195–196. doi: 10.7326/0003-4819-152-3-201002020-00019. author reply 196–197) [DOI] [PubMed] [Google Scholar]
- 29.Pencina MJ, D'Agostino RB, Sr, Steyerberg EW. Extensions of net reclassification improvement calculations to measure usefulness of new biomarkers. Stat Med. 2011;30:11–21. doi: 10.1002/sim.4085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Abdulla J, Pedersen KS, Budoff M, Kofoed KF. Influence of coronary calcification on the diagnostic accuracy of 64-slice computed tomography coronary angiography: a systematic review and meta-analysis. Int J Cardiovasc Imaging. 2012;28:943–953. doi: 10.1007/s10554-011-9902-6. [DOI] [PubMed] [Google Scholar]
- 31.Zhang S, Levin DC, Halpern EJ, Fischman D, Savage M, Walinsky P. Accuracy of MDCT in assessing the degree of stenosis caused by calcified coronary artery plaques. AJR Am J Roentgenol. 2008;191:1676–1683. doi: 10.2214/AJR.07.4026. [DOI] [PubMed] [Google Scholar]
- 32.Arbab-Zadeh A, Miller JM, Rochitte CE, Dewey M, Niinuma H, Gottlieb I, Paul N, Clouse ME, Shapiro EP, Hoe J, Lardo AC, Bush DE, de Roos A, Cox C, Brinker J, Lima JA. Diagnostic accuracy of computed tomography coronary angiography according to pre-test probability of coronary artery disease and severity of coronary arterial calcification. The CORE-64 (Coronary Artery Evaluation Using 64-Row Multidetector Computed Tomography Angiography) International Multicenter Study. J Am Coll Cardiol. 2012;59:379–387. doi: 10.1016/j.jacc.2011.06.079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Erbel R, Mohlenkamp S, Moebus S, Schmermund A, Lehmann N, Stang A, Dragano N, Gronemeyer D, Seibel R, Kalsch H, Brocker-Preuss M, Mann K, Siegrist J, Jockel KH Heinz Nixdorf Recall Study Investigative G. Coronary risk stratification, discrimination, and reclassification improvement based on quantification of subclinical coronary atherosclerosis: the Heinz Nixdorf Recall study. J Am Coll Cardiol. 2010;56:1397–1406. doi: 10.1016/j.jacc.2010.06.030. [DOI] [PubMed] [Google Scholar]
- 34.Elias-Smale SE, Proenca RV, Koller MT, Kavousi M, van Rooij FJ, Hunink MG, Steyerberg EW, Hofman A, Oudkerk M, Witteman JC. Coronary calcium score improves classification of coronary heart disease risk in the elderly: the Rotterdam study. J Am Coll Cardiol. 2010;56:1407–1414. doi: 10.1016/j.jacc.2010.06.029. [DOI] [PubMed] [Google Scholar]
- 35.Berman DS, Wong ND, Gransar H, Miranda-Peats R, Dahlbeck J, Hayes SW, Friedman JD, Kang X, Polk D, Hachamovitch R, Shaw L, Rozanski A. Relationship between stress-induced myocardial ischemia and atherosclerosis measured by coronary calcium tomography. J Am Coll Cardiol. 2004;44:923–930. doi: 10.1016/j.jacc.2004.06.042. [DOI] [PubMed] [Google Scholar]
- 36.He ZX, Hedrick TD, Pratt CM, Verani MS, Aquino V, Roberts R, Mahmarian JJ. Severity of coronary artery calcification by electron beam computed tomography predicts silent myocardial ischemia. Circulation. 2000;101:244–251. doi: 10.1161/01.cir.101.3.244. [DOI] [PubMed] [Google Scholar]
- 37.Fagan TJ. Letter: Nomogram for Bayes theorem. N Engl J Med. 1975;293:257. doi: 10.1056/NEJM197507312930513. [DOI] [PubMed] [Google Scholar]
- 38.Erbel R, Budoff M. Improvement of cardiovascular risk prediction using coronary imaging: subclinical atherosclerosis: the memory of lifetime risk factor exposure. Eur Heart J. 2012;33:1201. doi: 10.1093/eurheartj/ehs076. [DOI] [PubMed] [Google Scholar]
- 39.Min JK, Lin FY, Gidseg DS, Weinsaft JW, Berman DS, Shaw LJ, Rozanski A, Callister TQ. Determinants of coronary calcium conversion among patients with a normal coronary calcium scan: what is the ‘warranty period’ for remaining normal? J Am Coll Cardiol. 2010;55:1110–1117. doi: 10.1016/j.jacc.2009.08.088. [DOI] [PubMed] [Google Scholar]
- 40.Raff GL, Chinnaiyan KM, Share DA, Goraya TY, Kazerooni EA, Moscucci M, Gentry RE, Abidov A Advanced Cardiovascular Imaging Consortium C-I. Radiation dose from cardiac computed tomography before and after implementation of radiation dose-reduction techniques. JAMA. 2009;301:2340–2348. doi: 10.1001/jama.2009.814. [DOI] [PubMed] [Google Scholar]
- 41.Menke J, Unterberg-Buchwald C, Staab W, Sohns JM, Seif Amir Hosseini A, Schwarz A. Head-to-head comparison of prospectively triggered vs. retrospectively gated coronary computed tomography angiography: meta-analysis of diagnostic accuracy, image quality, and radiation dose. Am Heart J. 2013;165:154–163 e153. doi: 10.1016/j.ahj.2012.10.026. [DOI] [PubMed] [Google Scholar]
- 42.Achenbach S, Marwan M, Ropers D, Schepis T, Pflederer T, Anders K, Kuettner A, Daniel WG, Uder M, Lell MM. Coronary computed tomography angiography with a consistent dose below 1 mSv using prospectively electrocardiogram-triggered high-pitch spiral acquisition. Eur Heart J. 2010;31:340–346. doi: 10.1093/eurheartj/ehp470. [DOI] [PubMed] [Google Scholar]
- 43.Henneman MM, Schuijf JD, Pundziute G, van Werkhoven JM, van der Wall EE, Jukema JW, Bax JJ. Noninvasive evaluation with multislice computed tomography in suspected acute coronary syndrome: plaque morphology on multislice computed tomography versus coronary calcium score. J Am Coll Cardiol. 2008;52:216–222. doi: 10.1016/j.jacc.2008.04.012. [DOI] [PubMed] [Google Scholar]
- 44.Gottlieb I, Miller JM, Arbab-Zadeh A, Dewey M, Clouse ME, Sara L, Niinuma H, Bush DE, Paul N, Vavere AL, Texter J, Brinker J, Lima JAC, Rochitte CE. The absence of coronary calcification does not exclude obstructive coronary artery disease or the need for revascularization in patients referred for conventional coronary angiography. J Am Coll Cardiol. 2010;55:627–634. doi: 10.1016/j.jacc.2009.07.072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Motoyama S, Sarai M, Harigaya H, Anno H, Inoue K, Hara T, Naruse H, Ishii J, Hishida H, Wong ND, Virmani R, Kondo T, Ozaki Y, Narula J. Computed tomographic angiography characteristics of atherosclerotic plaques subsequently resulting in acute coronary syndrome. J Am Coll Cardiol. 2009;54:49–57. doi: 10.1016/j.jacc.2009.02.068. [DOI] [PubMed] [Google Scholar]
- 46.Kristensen TS, Kofoed KF, Kuhl JT, Nielsen WB, Nielsen MB, Kelbaek H. Prognostic implications of nonobstructive coronary plaques in patients with non-ST-segment elevation myocardial infarction: a multidetector computed tomography study. J Am Coll Cardiol. 2011;58:502–509. doi: 10.1016/j.jacc.2011.01.058. [DOI] [PubMed] [Google Scholar]