Abstract
Intracranial brain parenchymal tuberculomas may form paradoxically, days to months after starting antituberculous drug therapy. They may develop in and around optic chiasm and optic nerves after antituberculous treatment as a quite rare occurrence in tuberculous meningitis (TBM) this may lead to severe visual loss if not treated properly. We describe a 5 year-old child with documented TBM being treated with first line antituberculous drugs which developed visual impairment 3 months after starting the treatment. MRI after gadolinium administration revealed multiple perichiasmatic ring enhancing lesions due to tuberculomas. Visual impairment developing in a patient on treatment with antituberculous drugs should give rise to a suspicion of rare optochiasmatic tuberculomas; this necessitates urgent contrast-enhanced MRI of the brain and prompt treatment with steroids.
Keywords: optochiasmatic tuberculoma, paradoxical response, MRI
Introduction
Tuberculosis (TB) is the 7th leading cause of death and disability worldwide and has reached epidemic proportions in both developed and undeveloped nations. Approximately 5 to 10% of tuberculosis cases involve the brain and central nervous system. Tuberculomas account for 10 to 30% of intracranial (IC) masses in TB-endemic areas.
The clinical and neuroimaging features of tuberculoma are variable and may pose a diagnostic challenge in the absence of systemic TB or tuberculous meningitis. [1].
Central nervous system (CNS) involvement is seen in about 10% of patients with tuberculosis, and this is more common in developing countries [1, 2]. CNS tuberculosis may manifest in diffuse form with meningitis or in focal form as intracranial tuberculomas [2]. Neuro-ophthalmologic complications of tuberculous meningitis include oculomotor nerve palsy, pupillary abnormalities and optic disc changes of papillitis, papilledema, or optic atrophy [3]. These complications are seen in the late stage of tuberculous meningitis, usually manifesting in the elderly [4]. Intracranial tuberculomas may enlarge or develop afresh as a paradoxical response to ongoing antituberculous chemotherapy for tuberculous meningitis. Tuberculomas may rarely develop during treatment of TBM around the anterior optic pathway including the optic nerve and optic chiasm, threatening vision [5]. We describe paradoxical development of tuberculomas in the anterior optic pathway demonstrated by MRI in a case of TBM who complained of progressive loss of vision during the 2nd month of antituberculous therapy (ATT).
Case Report
A 5-year-old child, taking ATT since 3 months for tuberculous meningitis, presented with progressive diminution in both eyes and headache for the last 10 days. He started taking ATT as a combination of rifampicin, isoniazid, pyrazinamide and ethambutol, as well as corticosteroids for two weeks. After he had been diagnosed with imaging examination and also in laboratory, tuberculous meningitis has been confirmed in the infective clinic of the Kosovo University Clinical Center. At the time of hospitalization, the child did not have any problems with his sight; while in the neurological aspect, positive meningeal syndrome was present. The patient reported full compliance with the antituberculous drug regime and his clinical condition improved gradually. After the initial improvement with ATT, he started to suffer vision diminution. The examination revealed vision diminution, and fundoscopy showed bilateral papilledema. His serology was negative for human immunodeficiency virus (HIV). On 27.01. 2014, a brain MRI was performed on a 1.5 tesla MRI system in the Prima Imaging Centre in Prishtina, using T1-weighted (T1W) and T2-weighted (T2W) sequences in axial, coronal and sagittal plans; this was followed by intravenous administration of gadolinium containing contrast agent and subsequent T1W imaging in all the plans. MRI showed multiple rounded lesions with hyperintense signal intensity wall on T1W sequence in the suprasellar cistern. T2W images showed round lesions filling suprasellar cistern (Fig. 1).
Fig.1.
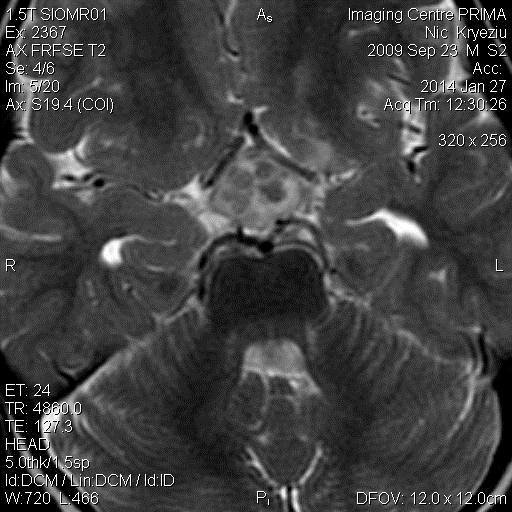
T2W images showed round lesions filling suprasellar cistern
Post-gadolinium enhanced T1W images depicted multiple ring enhancing lesions clustered around optic chiasma in the suprasellar cistern (Fig. 2), 3)).
Fig.2.
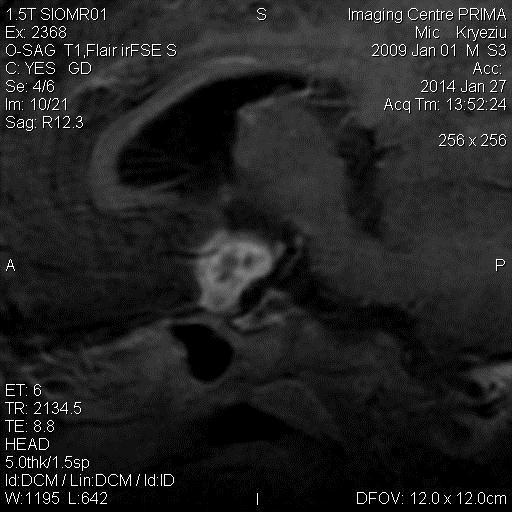
Post-gadolinium enhanced T1W images in sagital section depicted multiple ring enhancing lesions clustered around optic chiasma in the suprasellar cistern
Fig.3.
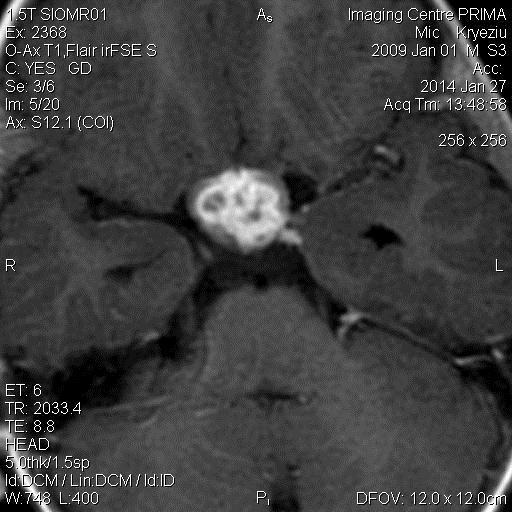
Post-gadolinium enhanced T1W images in axial section showing multiple ring enhancing lesions clustered around optic chiasma in the suprasellar cistern
Clinical features and imaging findings were compatible with a diagnosis of TBM with optochiasmatic tuberculomas resulting in neuro-opthalmologic manifestations, possibly due to paradoxical response to treatment. We have recommended a continuation of treatment with ATT along with corticosteroids. We are still waiting for a successful finalization of this therapy.
Discussion
Visual loss in TBM resulting from involvement and inflammation of the optic chiasm and optic nerves is a rare occurrence [6, 7]. Visual loss developing during treatment of TBM may be related to drug toxicity and arachnoiditis besides tuberculomas involving the anterior optic pathway. The optochiasmatic region may be a rare location involved by paradoxical development of intracranial tuberculomas during ATT for CNS or pulmonary tuberculosis [6, 7, 8].
Pathogenesis of this paradoxical development and/or expansion of tuberculomas have been attributed to exaggerated host reaction to tuberculous protein in a patient being successfully treated with ATT [2, 5]. Role of corticosteroids in controlling tuberculomas in this situation is more likely due to an effect on this host response rather than reduction of associated edema. The paradoxical response resulting in optochiasmatic tuberculomas has important diagnostic and therapeutic implications [2, 6, 7].
Early recognition of this condition and continued ATT and corticosteroid therapy or surgical decompression of optic pathway may help in preserving the visual function of the patient [2, 7, 8]. The treating neurologist and ophthalmologist need to be aware of such a rare occurrence of paradoxical optochiasmatic tuberculomas as a cause of visual impairment in the spectrum of tuberculosis and its treatment. This awareness and proper clinical judgment helps in timely recognition of this phenomenon in a patient on ATT who needs to be closely followed [8]. Satisfactory initial response to ATT, no associated systemic features and persistent sensitivity of isolated Mycobacterium tuberculosis to the instituted first line antituberculous drugs favoured a diagnosis of paradoxical response against progressive drug resistant infection in our case. MRI helps in early detection of intracranial tuberculomas which are seen as ring enhancing lesions after contrast administration. Intracranial tuberculomas are usually parenchymal and extra-axial location in CSF spaces is exceedingly rare. Optochiasmatic tuberculomas may be intrachiasmatic or perichiasmatic in location; this differentiation is difficult even with MRI [2]. Multiple ring enhancing lesions due to tuberculomas on MRI need to be differentiated from neurocysticercosis, pyogenic abscesses, metastasis and toxoplasmosis. Clinical features, serology and CSF findings are helpful besides imaging to arrive at proper diagnosis. Optochiasmatic tuberculomas also need to be considered in the differential diagnosis of optic nerve and perichiasmatic tumors in view of prevalent TB [9, 10, 11].
Using MRI, the exact location and relationship of tuberculomas with respect to the optic nerve and chiasm can be determined. This helps in planning surgical decompression of optochiasmatic tuberculomas threatening vision. For the treatment of paradoxical development of tuberculomas, antituberculous drugs are continued as usual and systemic corticosteroids are added [2, 5]. Steroids overcome the inflammatory response of the host body to the breakdown products of killed Mycobacterium tuberculosis [10]. ATT is continued up to 24-30 months, though a shorter course has been reported to be effective as well [2]. Corticosteroid therapy is continued for 6-8 weeks and withdrawn after gradual tapering. Failure of medical therapy is an indication for urgent surgical decompression [8]. Timely decompression of optochiasmatic region is important for a favorable visual recovery. Prompt surgical intervention for tuberculomas of the anterior optic pathway is facilitated by MRI by providing a roadmap.
Conclusions
Paradoxical development of optochiasmatic tuberculomas may present as visual impairment in a patient on ATT for TBM. MRI demonstrates ring enhancing lesions around the optic chiasm and aids in the management by helping in timely diagnosis and follow-up. Corticosteroid therapy may achieve satisfactory decompression and preserve vision.
References
- 1.Wasay M, Kheleani BA, Moolani MK, et al. Brain CT and MRI findings in 100 consecutive patients with intracranial tuberculoma. J Neuroimaging. 2003;13:240–247. [PubMed] [Google Scholar]
- 2.Monga PK, Dhaliwal U. Paradoxical reaction in tubercular meningitis resulting in involvement of optic radiation. Indian J Ophthalm. 2009;57:139–141. doi: 10.4103/0301-4738.45504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Amitava AK, Alarm S, Hussain R. Neuro-ophthalmic features in pediatric tubercular meningoencephalitis. J Pediatr Ophthalmol Strabismus. 2001;38:229–234. doi: 10.3928/0191-3913-20010701-10. [DOI] [PubMed] [Google Scholar]
- 4.Poon WS, Ahuja A, Li AK. Optochiasmatic tuberculoma causing progressive visual failure: When has medical treatment failed? Postgrad Med J. 1993;69(808):147–149. doi: 10.1136/pgmj.69.808.147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tsai MH, Huang YC, Lin TY. Development of tuberculoma during therapy presenting as hemianopsia. Pediatr Neurol. 2004;31(5):360–363. doi: 10.1016/j.pediatrneurol.2004.05.008. [DOI] [PubMed] [Google Scholar]
- 6.Silverman IE, Liu GT, Bilaniuk LT, Volpe NJ, Galetta SL. Tuberculous meningitis with blindness and perichiasmal involvement on MRI. Pediatr Neurol. 1995;12:65–67. doi: 10.1016/0887-8994(94)00107-d. [DOI] [PubMed] [Google Scholar]
- 7.Yeh S, Cunningham MA, Patronas N, Foroozan R. Optic neuropathy and perichiasmal tuberculomas associated with Mycobacterium tuberculosis meningitis in pregnancy. Can J Ophthalmol. 2009;44(6):713–715. doi: 10.3129/i09-167. [DOI] [PubMed] [Google Scholar]
- 8.Sharma K, Pradhan S, Varma A, Rathi B. Irreversible blindness due to multiple tuberculomas in the suprasellar cistern. J Neuroophthalmol. 2003;23(3):211–212. doi: 10.1097/00041327-200309000-00006. [DOI] [PubMed] [Google Scholar]
- 9.Aversa do Souto A, Fonseca AL, Gadelha M, Donangelo I, Chimelli L, Domingues FS. Optic pathways tuberculoma mimicking glioma: Case report. Surg Neurol. 2003;60(4):349–353. doi: 10.1016/s0090-3019(03)00133-2. [DOI] [PubMed] [Google Scholar]
- 10.Kalkan A, Serhatlioglu S, Ozden M, et al. Paradoxically developed optochiasmatic tuberculoma and tuberculous lymphadenitis: a case report with 18-month follow-up by MRI. South Med J. 2006;99:388–392. doi: 10.1097/01.smj.0000209091.57281.23. [DOI] [PubMed] [Google Scholar]
- 11.Moon S, Son J, Chang W. A case of oculomotor nerve palsy and choroidal tuberculous granuloma associated with tuberculous meningoencephalitis. Korean J Ophthalmol. 2008;22(3):201–204. doi: 10.3341/kjo.2008.22.3.201. [DOI] [PMC free article] [PubMed] [Google Scholar]


