Abstract
Background
Bone bruises are frequently associated with anterior cruciate ligament (ACL) tears as a result of trauma or direct shear stress of the bone.
Purpose
To review the evidence regarding the characteristics of the bone bruise associated with ACL tears, its relevance on clinical outcomes, and its progression over time. In particular, the long-term effects of the bone bruise on the knee osteochondral architecture and joint function were evaluated.
Study design
Review; level of evidence: 4.
Methods
An electronic search was performed on PubMed. Combinations of keywords included: “bone bruise AND knee”; “bone bruise AND anterior cruciate ligament”; “bone bruise AND osteo-chondral defects”. Any level of evidence studies concerning bone bruises in patients with partial or complete ACL tears were retrieved.
Results
A total of 25 studies were included; three of them investigated biomechanical parameters, seven were concerned with clinical outcomes, and 15 were radiological studies. Evaluation of the bone bruise is best performed using a fat-saturated T2-weighted fast spin echo exam or a short tau inversion recovery sequence where fat saturation is challenging. The location of the injury has been demonstrated to be more frequent in the lateral compartment of the joint (lateral femoral condyle and lateral tibial plateau). It is associated with ACL tears in approximately 70% of cases, often with collateral ligament or meniscal tears. Mid- and long-term outcomes demonstrated a complete healing of the marrow lesions at magnetic resonance imaging, but chondral defects detected with T1ρ sequences are still present 1 year after the ACL injury. Functional examination of the knee, through clinical International Knee Documentation Committee scores, did not show any correlation with the bone bruise.
Conclusion
Although bone bruise presence yields to higher pain levels, no correlation with functional outcomes was reported. Most studies have a short-term follow-up (<2 years) compared to the length of time it takes to develop post-traumatic osteoarthritis, so it still remains unclear whether the initial joint injury and bone bruise have a direct relationship to long-term function.
Keywords: bone bruise, anterior cruciate ligament, magnetic resonance imaging, knee
Introduction
Anterior cruciate ligament (ACL) tears are commonly caused during sport participation1 and are often associated with meniscal and cartilage lesions. The global incidence of ACL injuries is about 100,000–250,000 cases per year.2 A high rate (from 10%–90%) of osteoarthritis development after ACL injury has been reported, despite optimizing treatment,3–6 in mid- and long-term follow-up studies (up to 14 years). Magnetic resonance imaging (MRI) is currently the best imaging tool for radiological examination of these types of lesions,7 corroborating the clinical examination of the patient, and it is ideal for assessing associated lesions. A sensitivity of 78% and a specificity of 100% are reported for ACL tear radiologic diagnosis by a 1.5 Tesla MRI.8 Several ancillary findings are frequently associated with ligamentous injuries of the knee, such as osteochondral defects, occult cortical fractures, and bone bruises (BBs) or contusions.9 New sequences are currently developing in order to evaluate cartilage changes as well, such as T1ρ sequences.10,11 BBs are usually defined as an alteration of the signal intensity of the bone marrow, seen at MRI using T1-weighted and T2-weighted images, but they are best seen with fat suppression and short tau inversion recovery (STIR) sequences.12,13 Bruises of the bone have been also defined as bone marrow edema-like lesions,11 so that a differentiation can be made with the bone marrow lesions.14 The latter occur in osteoarthritis-affected knees because of the bone-on-bone stress concentration. The main cause of an articular BB appears to be the direct impact loading of the joint surfaces in conjunction with shear stress applied at the bone during a ligament rupture.15 Multiligamentous injuries have been reported in association with the ACL rupture, and BBs have been documented in different locations of the knee joint following acute injury or trauma.7,13,16 With respect to ACL lesions, BB(s) has been found in approximately 70% of knees with tears.11
Histologically, the BB has been rarely evaluated, but some evidence in the literature has reported that it is characterized by hemorrhage, edema, necrosis, and fibrosis.13,14 These features have been considered to result from microtrabecular fractures, which often occur during knee injury.11 In addition to these findings, chondrocyte death has been reported, also implying chondral defects of the overlying cartilage.11,16 Concerning this topic, the literature lacks strong evidence regarding the long-term changes in an ACL injured knee in relation to bone marrow changes. The location of the bone marrow lesions has been largely investigated; reporting a common location within the lateral compartment.17,18 In addition, the lesions feature a typical appearance, and the pattern of the lesion is strongly connected to the mechanism of injury.15 The natural history of a BB is not completely understood because follow-up studies,19,20 showing long- and short-term outcomes, reported variable healing patterns of these lesions over time, in terms of both their function and their anatomic sequelae.
In this review of the literature, evidence regarding MRI evaluation, localization and appearance of the bone injury, mechanism-related features, and clinical issues have been summarized. The aim of this review is to report the characteristics of the BB associated with ACL tears, its definition and classification, diagnostic tools used for assessment, its relevance on clinical outcomes, and its progression over time. In particular, we were interested in evidence regarding the long-term effects of the BB on the knee’s osteochondral architecture and function.
Methods
For article research, the PubMed online database was used (http://www.ncbi.nlm.nih.gov/pubmed). The search was performed between July–August 2014. Combinations of keywords were: “bone bruise AND knee”; “bone bruise AND anterior cruciate ligament”; and “bone bruise AND osteo-chondral defects”. We searched for any level of evidence studies concerning BB detection, clinically-associated features, and related injury mechanisms in patients with partial or complete ACL tears. We excluded studies in which knee BB was reported that was not associated with ACL lesions, studies on cadavers, or in vitro studies. No time interval for year of publication was set. Of each of the articles retrieved, the entire bibliography was screened in order to find studies that could be relevant for the review. Studies were retrieved in full text, analyzed, and tabulated. The studies included were classified into one of three categories: radiological; clinical; or mechanism-related studies. The study selection process was carried out as shown in Figure 1. A summary of the studies is reported in Table 1.
Figure 1.
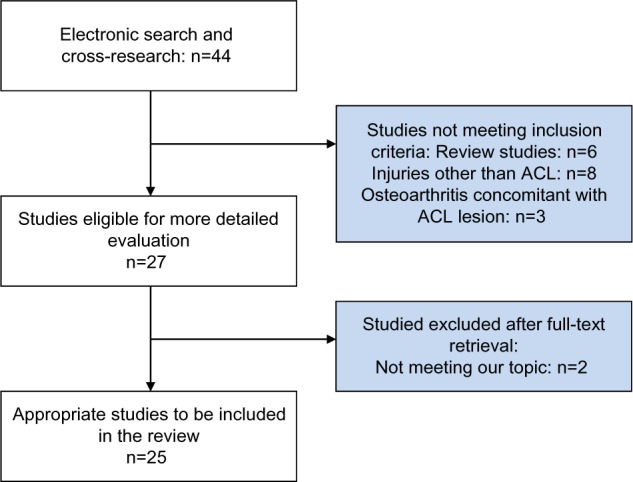
Study selection process.
Abbreviations: n, number; ACL, anterior cruciate ligament.
Table 1.
Radiological studies
| Study | Year | Aim | MRI sequence | BB definition | Materials and subjects | Results | Conclusion | Clinical relevance |
|---|---|---|---|---|---|---|---|---|
| Tung et al26 | 1993 | Assess utility of ancillary MRI findings in ACL injured knee | PD, T2, | Abnormal bone marrow intensity area | 99 patients underwent arthroscopy (50 ACL tears) | BB observed in 26.2% of cases (44% of ACL tears group versus 9.4% of normal ACL group; P=0.0003) | Specific lateral compartment BB pattern occurs in 73% of ACL tears | One of the first studies reporting BB as a secondary finding for ACL rupture |
| McCauley et al23 | 1994 | Assess utility of ancillary MRI findings in ACL injured knee | T1 | Nonlinear low signal in the bone marrow | 68 patients underwent diagnostic arthroscopy (39 had ACL tear) | Presence of BB in PLTP had a sensitivity of 46%–50% and a specificity of 97%. Posterior displacement of the posterior horn of lateral meniscus had sensitivity of 56% and specificity of 97%–100%. PCL angle <105º had a sensitivity of 72%–74% and a specificity of 79%–86% | Ancillary findings at MRI are helpful in diagnosing ACL tears | Sensitivity and specificity are reported for many ancillary findings in ACL injured knee |
| Munshi et al25 | 2000 | Evaluate MRI efficacy in acutely injured knee | PD, T2 | 23 patients with acute injury of the knee | ACL lesions occurred in 20 patients. Of these, 14 had BB in the LFC or PLTP, or both | MRI can be a clear support to clinical examination in knee trauma | ||
| Vellet et al17 | 1991 | Assessing of prevalence, classification, and follow-up of post-traumatic osteochondral lesions in traumatic injury of the knee | T1, T2 | Altered signal intensity in images (reticular, geographic, linear, impaction, osteochondral occult fractures) | 120 patients with acute post-traumatic hemarthrosis (ACL tear in 79% of occult fracture- positive subjects) | Occult subcortical fractures were assessed in 72%: reticular (70%); geographic (22%); impaction (5%); linear (0.6%); and osteochondral (0.6%). ACL rupture was seen in 79% of the occult fracture subjects versus 56% of the subjects without. Lateral joint compartment fractures were in the lateral compartment in 81% of cases, 41% in the LFC, and 40% in the LTP. The medial joint compartment was involved in 19% of cases, 4.4% in the MFC, and 14.5% in the MTP. Relative rotation of the femur and tibia was responsible for 57% of the injuries | Occult subcortical fractures are associated with osteochondral sequelae | A description of several patterns of occult subcortical fractures, which can be associated with traumatic knee injuries |
| Yoon et al18 | 2011 | Evaluate the prevalence of bone contusion in ACL injured knee with or without associated lesions | T1, T2 | Altered signal intensity area | 81 patients with arthroscopic diagnosis of ACL rupture undergoing ACLR | BB was detected in 84% of the subjects. The locations of BB were: LFC (1% posterior, 51% central, 16% anterior); LTP (posterior 73%); MFC (anterior 5%, central 19%); and MTP (central 2%, posterior 23%). Meniscal lesion was associated with 54% (lateral) and 51% (medial) of the cases. MCL injury was associated with 22% of cases | Bone contusion of the medial side occurs more often than previously assessed, due to a pivot shift mechanism (high-energy injuries) | The medial compartment BB should not be neglected and can be considered a mechanism-related finding |
| Costa-Paz et al19 | 2001 | Assessing the natural history and healing of BB with a 2-year MRI follow-up | Type I: diffuse signal alteration with marrow changes. Type II: subchondral signal alteration. Type III: disruption or depression of cortical bone | 21 patients underwent ACLR without any cartilage defect | Twenty-nine BBs were observed on preoperative MRI: 13 type I (mainly LTP); eleven type II; and five type III (mainly LFC). In 15 patients (71%), BB resolved without any sequelae; six osteochondral defects were still present at MRI follow-up. The IKDC score revealed nine normal knees, ten nearly-normal knees, and two abnormal knees | No correlation was found between functional and radiological outcomes | This study provides classification of the lesions and a medium-term follow-up | |
| Bretlau et al12 | 2002 | Evaluate the location and pattern of BB in an acutely injured knee | T1, T2, three-dimensional gradient echo, STIR | Geographic, reticular, nonlinear, low-signal intensity (T1) regions. Three types: type I, loss of signal intensity in short TE sequences in the marrow, no cortical interruption; type II, loss of signal intensity in short TE sequences in the marrow, with interruption of the black cortical line; type III, loss of signal intensity in short TE sequences in the region of bone adjacent to the cortex, without a definite cortical interruption | 63 patients with acute injury of the knee (35 BB-positive) | ACL partial or complete tears were found in 24 patients. BB was observed in 56% of the subjects (67% of those with ACL rupture): 63% in LTP; 51% in LFC; 35% in MTP; and 26% in MFC. At late follow-up (11–16 months; 25 patients), 88% of BB lesions were healed (P=0.013) | BB is frequent in acute knee injuries and resolves in most cases between 4 months and 12 months | Location and follow-up data reported |
| Chin et al24 | 2013 | Assess incidence and patterns on BB | T1, T2 | Altered signal intensity area | 88 MRI images of the injured knee (58 with ACL injury) | BB in the femur was assessed in 71 (80.7%) patients, in the tibia in 62 (70.5%) patients, and in the patella in nine (10.2%) patients. ACL tears were observed in patients with tibial bruising were twice the ACL tears in those without (prevalence ratio: 2.01) A similar ACL prevalence was observed for subjects with lateral tibial bruising (prevalence ratio: 1.93) | Different patterns of BB are found in injured knees with or without ACL rupture | The prevalence of tibia bruising reported is double in confront of the prevalence of FC bruise |
| Mink and Deutsh9 | 1989 | Evaluate cartilage and bone injuries at MRI in the injured knee | T1 | Traumatically involved geographic and nonlinear area of subcortical bone, with a low-intensity signal | 66 patients with knee injury | BB was detected in 27 knees (30 lesions). BB locations were: 17 in the femur; six in the tibia; three in both bones. A clear history of direct trauma of the bone was assessed for seven of the 30 lesions; the others were associated with twisting. ACL tears were detected in 25 patients, of them 23 had lateral compartment BB | Bone marrow lesions are common in acute knee injury, but the specific pathologic substrate should be clarified | First attempt at definition and localization of BB in the ACL injured knee |
| Gentili et al22 | 1994 | Establish sensitivity and specificity of ancillary findings at MRI | T2 | Geographic, reticular, nonlinear, high-signal intensity regions | 89 patients (54 torn ACL, 35 normal ACL) | BB in LFC (above femoral sulcus): sensitivity, 51%; specificity, 100%; BB in the tibial plateau or femoral condyle: sensitivity, 58%; specificity, 100% | Secondary ACL tear findings increase accuracy of the diagnosis through MRI | Sensitivity and specificity of some secondary findings in the ACL injured knee are reported |
| Davies et al32 | 2004 | Evaluate short-term MRI outcomes in an acutely injured knee | STIR | Higher intensity region | 30 patients with acute injury | BB was an inclusion criteria (detected in 30 patients). Of these, 67% had ACL rupture, 23% had collateral ligament or menisci lesions. The majority had PLTP and LFC BB. At follow-up (12–14 weeks), a reduction of 50% of the BB volume was observed in 24 patients; five had a reduction of less than 50%, one showed 33% increased volume. Larger volume at baseline was associated with osteochondral injuries (P=0.02) | Most of the BB reduced in volume in about 3 months. No correlation was found between volume and lesion patterns | BB healing can be observed at short-term follow-up |
| Theologis et al11 | 2011 | Quantify BMEL and cartilage properties in ACL injured knees | T2 FS, T1ρ | Signal intensity algorithm relative to the surrounding marrow | Nine patients undergoing ACLR | BMEL common in LTP and LFC. Resolution at 1 year: 50% of cases. Overlying cartilage T1ρ intensity higher than in surrounding areas (P<0.05) | Overlying cartilagechanges persits at 1-year follow-up. BMEL volume correlates to the severity of cartilage alteration | Bone marrow lesions correlate significantly with cartilage defects |
| Jelić and Masulović13 | 2011 | Determine BB frequency | T1, T2 FS, STIR | Altered signal intensity area | 120 patients with acutely injured knee | BB was detected in 32.5% of subjects. Eleven patients had BB at the tibial plateau, seven (28%) had BB at both the tibia and femur, which more frequently occurred in the lateral compartment. Three patients had occult cortex fracture and were excluded. ACL tears were present in 69% of BB-positive patients; meniscal lesion was present in 72% of patients. Two patients had BB without lesions. Of the BB-negative patients, 43% had ACL injury and 63% had meniscal lesions | BB is best seen in STIR sequences. It is often associated with menisci and ACL lesions | A comparison of the MRI sequences has been evaluated |
| Halinen et al7 | 2009 | Evaluation at MRI of soft-tissue injuries in knee trauma | T1, T2, T2 FS, STIR | 44 patients with complete ACL and MCL rupture | Associated lesions: eleven medial and 14 lateral meniscal tears. BB was detected in 88.6% of patients. Anterior LFC and PLTP were the most common locations (56.8%). PLTP (18.2%) and anterior LFC (6.8%) | Medial meniscal tears, ligamentous injuries, and BB are precisely seen at MRI | All MRI sequence types were obtained | |
| Faber et al4 | 2014 | MRI follow-up study for the detection of subchondral bone marrow changes | T1, T2 | 23 patients with ACL injury | At baseline, all patients had LTP subchondral bone alterations. Altered marrow signal became normal at the 6.5-year follow-up in 15 of the 23 patients. Persistent subchondral lesions were observed in eight patients. Of these, there were five with low signals in T1 and T2, two with increased T1 and intermediate T1, and one with decreased T1 and increased T2 (consistent with BB). Thinned cartilage was detected in two patients at baseline (LFC), but it was present in 13 patients at follow-up (eight of them with subchondral alterations) | Osteochondral sequelae have been demonstrated in 65% of the patients, despite ACL reconstruction | Long-term evaluation of chondral defects |
Abbreviations: MRI, magnetic resonance imaging; BB, bone bruise; PD, proton density; ACL, anterior cruciate ligament; PLTP, posterolateral tibial plateau; LFC, lateral femoral condyle; LTP, lateral tibial plateau; MFC, medial femoral condyle; MTP, medial tibial plateau; ACLR, anterior cruciate ligament reconstruction; MCL, medial collateral ligament; IKDC, International Knee Documentation Committee; STIR, short tau inversion recovery; FC, femoral condyle; BMEL, bone marrow edema-like lesions; FS, fat suppression; TE, time of echo.
Results
Definition and classification
Lesions of bone marrow seen by MRI are usually described as an altered signal intensity of the area that involves the contusion. In 1989 Mink and Deutsch9 first defined a BB as a “traumatically involved, geographic and nonlinear area of signal loss involving the subcortical bone”, and Lynch et al21 proposed the first categorization. According to Lynch et al,21 three types of lesions can be observed by MRI of the knee, based on their morphology, and with all exhibiting a signal loss in short-echo time sequences (T1-weighted). Type I lesions were located in the medullary space, mainly within the epiphyseal and metaphyseal portion of the bone, without any cortical involvement; type II lesions were characterized by interruption of the black subchondral line; and type III were restricted to the subcortical area, without a definite interruption of the cortex. Occult fracture classification was later proposed by Vellet et al17 in 1991 and utilized by several successive studies for BB classification.12,22 According to this classification, three types of lesion are distinguished based on morphology and localization. Reticular fractures were reticular and serpiginous occult subcortical fractures localized in the epiphyseal and metaphyseal marrow, distant from the chondral surface.17 Geographic fractures were mainly localized near the cortex; these fractures were also divided in two subcategories: geographic I, with a coalescence pattern (not peripheral); and geographic II, coalescent, crescentic, circumscribing a central marrow fat zone close to the cortical bone.17 Lastly, the linear fractures were defined as linear, 2 mm width subcortical lesions.17 The appearance and location of BB have also been considered by Costa-Paz et al19 in 2001, who described a further classification. Type I lesions were defined as diffuse and were associated with medullar changes, often with a reticular pattern and distant from the articular surface. Type II lesions included the focal alteration of the signal, contiguous to the articular surface. Finally, type III involved the surface, with depression or disruption of the articular contour.19
Magnetic resonance imaging evaluation
The reported MRI sensitivity and specificity are, respectively, 58%–61% and 86%–93% for BB in any bone compartment, though the specificity increases to 97% for BB in the posterior lateral tibial plateau (LTP) and 100% for the lateral femoral condyle (LFC).22,23 Radiological studies (Table 1) reported several sequences for the detection of BB; most of them evaluated BB through T1-w and T2-w sequences,9,12,17,22,24 with a shared detection of increased signal intensity in T2-w and decreased detection in T1-w. Proton density sequences were utilized in two studies.25,26 Other sequences, such as STIR and fat saturation, are not performed for patient examination in day-to-day clinical practice, but they have been used in some studies for the experimental examination of the knee.7,12,13 According to Jelić and Masulović,13 STIR sequences are best for detecting BB because it is able to suppress the fat bone marrow signal. Theologis et al11 utilized the T1ρ sequences for the detection of lesions in the cartilage overlying the BB-involved area in the lateral tibia. According to these findings, an altered signal was found in the cartilage overlying the BB lesion when compared to the surrounding cartilage areas, at times remaining also after the BB had resolved. In the same study, a volume computation algorithm27 was utilized and the volume of the bruised bone can be extrapolated by setting a relative intensity threshold, which allows for the differentiation between the bruised and the normal marrow. Another method28 has been utilized by Szkopek et al29 and was based on the calculation of the diameters of the lesion (one coronal diameter and its perpendicular one) and the number of slices in which the bruise was seen.
Localization
In conjunction with ACL tears, the BB is seen in the lateral compartment of the joint – ie, the LFC and the LTP. Vellet et al17 reported 81% of BB in the lateral compartment (41% LFC; 40% LTP), while the medial compartment was involved in 19% of cases (4.4% in the medial femoral condyle; 14.5% in the medial tibial plateau [MTP]). Similar findings were reported by Yoon et al,18 showing an overall incidence of 84%: LFC (1% posterior, 51% central, 16% anterior); LTP (posterior 73%); medial femoral condyle (anterior 5%, central 19%); and MTP (central 2%, posterior 23%). A lower incidence was reported by Bretlau et al12 (56%) and Jelić and Masulović13 (32.5%).
Mechanism of injury
Localization of the BB is strongly connected to the mechanism of injury,15,30 and many feel that the BB localization is a footprint of the mechanism itself.15 Sanders et al15 reported a detailed analysis about the injury mechanism and BB localization. Pivot shift injuries are mainly characterized by bone contusion in the LTP and the midportion of the LFC, with a more anterior or posterior LFC localization depending on the knee flexion at the moment of the injury.15 Injury caused by hyperextension of the knee and resulting in ACL and/or posterior cruciate ligament tears is usually associated with a “kissing lesion” BB pattern, with BB localization observed in the anterior aspect of the femoral condyles and the anterior aspect of the tibial plateau, which collide against one another during hyperextension.15 It can be located medially if a varus force occurs concomitantly with the extension.15 Returning to pivot shift injuries, Westermann et al31 reported that the tibial plateau geometry affects the mechanism of injury and thus the BB pattern. In this study, the results showed that a knee with a highly convex plateau (a more unstable knee) requires less energy to dislocate; thus, bone contusion is less likely to be severe. On the other hand, a more stable knee, with a lower plateau curvature ray, needs much more energy to result in an ACL rupture, so in the event of a tear, more vigorous impact has occurred, resulting in a more severe BB. In addition to these results, it has been also reported30 that noncontact (NC) injuries result in higher bruise incidence rates when compared with the contact (C) injuries. Significantly more LTP and lateral posterior LTP BB was shown in the NC group (P<0.019 and P=0.045, respectively), and similarly in MTP (P=0.045). A higher intensity of bruises was found in the NC group (81% versus 36%; P<0.001).
Associated lesions
The lesions, which are associated with ACL rupture in conjunction with a BB, are meniscal tears and medial collateral ligament sprains. Nishimori et al16 reported an overall BB incidence of 89.7% of patients with acute ACL injuries. At the arthroscopic examination of these BB-positive patients, 91.4% had lateral meniscal tears (P=0.008), 94.3% had cartilage defects in the LFC (P=0.004), and 80% had cartilage defects in the posterior LTP (P=0.04). Davies et al32 reported that 67% of ACL ruptures occurred in BB-positive patients, with 23% exhibiting associated menisci or collateral ligament injuries, while Jelić and Masulović13 reported a higher incidence of meniscal tears (72% of the BB-positive subjects). Halinen et al7 reported eleven medial and 14 lateral meniscal tears in a cohort of 44 patients (BB prevalence: 88.6%). Faber et al4 evaluated joint cartilage changes above marrow lesions. At baseline, all patients had LTP subchondral bone alterations at MRI, and eight had LFC marrow defects. Altered LTP marrow signal became normal at the 6.5-year follow-up in 15 of 23 patients. Persistent subchondral lesions were observed in eight patients. Of these, there were five with low signals in T1 and T2, two with increased T1 and intermediate T1, and one with decreased T1 and increased T2 (consistent with BB). Thinned cartilage was detected in only two patients at baseline (LFC), and it was present in 13 patients at follow-up (eight of them with subchondral bone alteration).
Risk factors
Preinjury risk factors have been not extensively investigated. According to Bisson et al,33 age >18 years predicted less LFC BB (odds ratio [OR] =0.27 for ages 18–28 years; and OR =0.18 for ages >29 years); male sex predicted mild, moderate, and severe LFC BB (OR =6.16; OR =8.98; and OR =15.66, respectively), and mild LTP BB (OR =0.19). Injury features were also analyzed, showing that C injuries predicted severe LTP BB (OR =5.1). Dunn et al34 shared the hypothesis that younger age was a risk factor (P=0.034), and the authors also reported that the nonjumping mechanism of injury is mainly associated with BB (P=0.006).
Clinical outcomes
Two studies19,20 evaluated patients with BB associated with ACL rupture, utilizing the International Knee Documentation Committee (IKDC) score. Costa-Paz et al19 reported nine normal knees, ten nearly-normal knees, and two abnormal knees at a mean follow-up of 2 years among 21 patients with an original MRI that was positive for BB and ACL injury. The same study reported BB healing in 71% of patients, with cartilage defects still present in six patients. According to Hanypsiak et al,20 the mean IKDC score was 70 in 36 patients with BB, and 70.6 in eight patients without BB (P>0.05). At an average follow-up of 12.7 years, all the lesions were healed at MRI examination. A similar conclusion was made by Bretlau et al,12 who conducted a follow-up between 4 months and 16 months among 64 subjects (35 were BB-positive). A clinical comparison between patients with (number [n] =20) and without (n=20) BB was carried out by Johnson et al,35 indicating that patients with geographic lateral BB showed larger effusion (4.6 cm versus 3.9 cm), longer time for effusion dissipation (4 weeks versus 2.4 weeks), longer time to achieve nonantalgic gait without aids (4 weeks versus 2.8 weeks), longer time to achieve symmetric and equal range of motion (ROM) (3.8 weeks versus 2.7 weeks) (P<0.001), and higher pain scores (6.1 versus 2.9) when compared to subjects without BB, respectively. ROM has also been investigated by Quelard et al,36 who assessed recovery time length in BB-positive patients. Delayed recovery correlated with limited preoperative ROM (P<0.001), operative delay <45 days (P=0.003), and female sex (P=0.049). BB was observed more frequently in patients with limited preoperative ROM (P<0.001). Szkopek et al29 assessed pain reduction (using a numeric rating scale and the K2 essay of the Knee Injury and Osteoarthritis Outcome Score [KOOS]) of about 50% in an observational follow-up of 2 weeks among patients with acute ACL rupture associated with BB. Furthermore, this study correlated the BB with the KOOS score; BB volume was correlated with K2 (pain) in the medial tibial compartment, and K5 (psychological and social aspects) was correlated with pain in the LFC. BB intensity was related with K1 (swelling and mechanical symptoms) and K5.
Discussion
BB is associated with approximately 70% of ACL tears and can be detected with different patterns of localization and severity, consistent with the mechanism of injury.15 The BB was first described and classified by Mink and Deutsch9 in 1989 as an ancillary finding on an MRI of the injured knee. BB consists of bone marrow signal intensity alteration, which can be seen as a lower intensity in T1-weighted sequences, and it exhibits increased intensity in T2-weighted images. The explanation for these findings is related to the histological alterations that the bone contusion leads to. Hemorrhage and edema increase the water concentration in the involved area, which is responsible for the signal increase or decrease. STIR sequences were used in the study by Jelić and Masulović,13 who stated that these sequences are the best imaging tool for BB evaluation. From a radiological perspective, bone marrow signal is usually as intense as the signal from subcutaneous fat; therefore, when this signal is abolished, the BB is enhanced. The clinical issue regarding this topic is that STIR sequences are not routinely obtained for patients with knee injuries. Since BB is also easily seen using a fat-saturated T2-weighted fast spin echo exam,17 we can state that a T2-weighted STIR sequence can be used in instances where fat saturation is challenging, such as when metal is present. In addition, it may be helpful to detect and assess associated injuries at the time an ACL injury is suspected, so as to confirm the complete injury pattern. As previously reported, the mechanism of injury is directly correlated with BB location.15 NC injuries seem more likely to lead to the consistent location of BBs,30 and knee geometry may also affect BB severity.31 In the literature, it is also reported that the medial side BB should raise concerns for a possible multiligamentous injury.37
From an overall perspective, the BB pattern can be evaluated as a result of the specific bone contusion mechanism that was in place during the injury; this can lead to a better clinical examination of the patients in order to retrieve lesions that are specifically associated with that injury type. Clinically, higher pain scores were observed in patients with BBs when compared with the scores of those without,35 but functionally, the BB in ACL injured knees does not correlate with IKDC scores.19,20 Based on this review of the literature, at medium- and long-term follow-up, there does not appear to be any relationship between BB pattern and clinical knee function. However, Theologis et al11 reported that defects of the overlying joint cartilage can still be seen at a 12-month follow-up, despite healing of the bruise. In addition to this, Faber et al4 reported a further development of cartilage lesions following subchondral marrow changes. Therefore, longer-term follow-up is necessary to clearly outline the natural history of the BB and the overlying cartilage. There appears to be some interest in assessing BB volume and size,11,27,29 and this may be associated with chondral defects and long-term functional knee scores. At this point, volume analysis is not of any routine clinical relevance, but it may be related to overall joint injury and eventual long-term impact on joint function. Simple algorithm-based software28 could be used for the follow-up of these lesions in order to monitor their reduction over time, as well as to clear the patient to return to full activity levels. An experimental algorithm was also developed,11,27 but its complexity limits its use to scientific research only.
With respect to chondral defects, Theologis et al11 reported that microscopic lesions of the overlying joint cartilage can be still seen after BB healing. Clinical studies concerning this topic should be carried out, in order to correlate morphological changes in the knee architecture (osseous and cartilage structures) and the patient’s long-term functional outcomes. At this point, there appears to be a lack of evidence as to whether the BB should be regarded as a lesion that needs treatment or not, especially in terms of the possible effects of microtrabecular fractures on the biomechanics of knee joint homeostasis. Regrettably, the reviewed studies were really different in terms of the sequences used to assess the BB, the cohort size, and the outcomes evaluated; therefore, we were not able to compare results. Furthermore, most of the studies were of a low level of evidence, and this affected the quality of the findings. In addition to these limitations, the unsystematic character of this review may have led to some relevant papers being missed.
Conclusion
In conclusion, although there seems to be quite a few studies on various aspects of BBs, many questions remain, especially in terms of the effect of the BB on long-term joint function, its relationship to outcomes following ACL injury, and the development of post-traumatic osteoarthritis. We can state that currently, BB of the knee is an ancillary radiographic finding of the ACL and other knee multiligamentous injuries. It is often associated with other joint injuries, in addition to the ACL, as a conglomeration of injury severity. Therefore, the impact of the BB on global joint injury (rather than in isolation) may be of greater significance. Although its presence yields higher pain levels, no correlations have been solidly made with functional outcomes. Most follow-up studies of BBs are short term when compared to the length of time it takes to develop post-traumatic osteoarthritis, so it still remains unclear if the initial joint injury and BB have a direct relationship to long-term function. Post-traumatic osteoarthritis of the knee is a common sequelae of ACL injury, and identifying predisposing factors early in the course of the disease is essential as a means of developing and instituting preventative measures.
Table 2.
Clinical studies
| Study | Year | Aim | Materials and subjects | Intervention | Results | Conclusion | Clinical relevance |
|---|---|---|---|---|---|---|---|
| Nishimori et al16 | 2008 | Correlate cartilage defects of the PLTP with BB | 39 patients underwent ACLR (35 BB-positive; four BB-negative) | MRI evaluation of the presence of BB in the lateral compartment; arthroscopic evaluation of cartilage defect | BB was observed in 89.7% of patients; at overall arthroscopic examination, 84.6% had lateral meniscal tears, 87.2% had cartilage defects in LFC, and 74.3% had cartilage defects in PLTP. Of the BB-positive group, 91.4% had lateral meniscal tears (P=0.008), 94.3% had cartilage defects in LFC (P=0.004), and 80% had cartilage defects in PLTP (P=0.04) | BB correlates with articular cartilage defects in ACL injuries | Arthroscopic examination of the associated lesions |
| Johnson et al35 | 2000 | Assessing the effect of geographic BB lesions on clinical outcomes | 40 patients with ACL tears (20 BB-positive and 20 BB-negative) | One week to 4 weeks assessment of: pain; ROM; effusion; and days to nonantalgic gait | BB-positive patients showed: larger effusion (4.6 cm versus 3.9 cm); longer time for effusion dissipation (4 weeks versus 2.4 weeks); longer time to achieve nonantalgic gait without aids (4 weeks versus 2.8 weeks); longer time to achieve symmetric and equal ROM (3.8 weeks versus 2.7 weeks) (P<0.001); and higher pain scores (6.1 versus 2.9) | Statistically significant association between BB and increased disability | Patients with BB geographic lesions postoperative recovery and pain evaluation |
| Hanypsiak et al20 | 2008 | Assessing the natural history and healing of BB and cartilage defects at a 12-year follow-up | 44 subjects underwent ACLR | Patients called for at least a 10-year follow-up; MRI, radiographic assessment, clinical features, and IKDC score were evaluated | IKDC was 70.6 in BB-negative patients (n=36) and 70.0 in BB-positive patients (n=8) (P>0.05). No correlation found between cartilage lesions before surgery and at follow-up. IKDC was 72.8 in patients with cartilage defects and 69.0 in those without (P>0.05). At an average of 12.7 years of follow-up, 100% of lesions were absent at MRI | BB resolves over a long time period; its evaluation and presence at baseline did not affect IKDC score after surgery | Functional knee examination and correlation with the BB |
| Bisson et al33 | 2013 | To determine a possible association between bone bruises and demographic factors and articular injuries in ACL injured patients | 171 patients with ACL injury | MRI BB detection and localization, multivariate analysis for the correlation of BB and its predisposing factors | BB was detected in: 85% of LTP; 77% of LFC; 26% of MTP; and 6% of MFC. Age >18 years predicted less LFC BB (OR =0.27, for ages 18–28; and OR =0.18, for ages >29 years); male sex predicted mild, moderate, and severe LFC BB (OR =6.16; OR =8.98; and OR =15.66, respectively) and mild LTP BB (OR =0.19); contact injuries predicted severe LTP BB (OR =5.1). LFC and LTP BB were associated with meniscal tears (OR =2.57 and OR =3.13, respectively) | BB is most common in young males and is associated with meniscal tears | Several risk factors for the prediction of BB development in the lateral compartment are evaluated |
| Dunn et al34 | 2010 | Evaluate the correlation between BB and other preoperative features with prolonged knee pain and dysfunction | 525 patients underwent ACLR | The administration of the KOOS symptom and pain scales and SF-36 bodily pain scale. BB assessment (presence [yes/no] and location) at MRI | BB presence was 80% among subjects. Higher pain was associated with high BMI (P<0.0001), female sex (P=0.001), lateral collateral ligament injury (P=0.012), and older age (P=0.038). More symptoms were associated with lateral collateral ligament injury (P=0.014), higher BMI (P<0.0001), and female sex (P<0.0001). BB was not associated with either pain or symptoms, while younger age and nonjumping mechanism were associated with BB (P=0.034 and P=0.006, respectively) | Younger age and not jumping at the time of injury are risk factors for BB development | Clinical and social factors are correlated with the BB |
| Szkopek et al29 | 2012 | Evaluate the association between BB, pain, and dysfunction with a 2-month follow-up | 17 patients with ACL tears | MRI evaluation and KOOS after injury and at 2 weeks, 1 month, and 2 months. Subjective pain evaluated daily | Pain reduction was about 50% in 2 weeks. BB volume was larger in the lateral compartment than in the medial compartment. Volume increased in 2 weeks and began to decrease at 1 month. BB volume was correlated with K2 in the medial tibial compartment, and with K5 in the LFC. BB intensity was related with K1 and K5 | No strong correlation between disability and lateral BB | Functional assessment of the knee correlated with the BB natural history |
| Westermann et al31 | 2013 | Assess the correlation between lateral compartment geometry and BB patterns | Two cases of ACL injury | MRI evaluation 7 days and 10 days after injury; radiological measurement of tibial plateau curvature | Case 1: LTP curvature radius was 53.5 mm; BB was severe/extended. Case 2: LTP curvature radius was 32.1 mm; BB was mild/superficial | Highly convex joint surface (unstable knee) is associated with milder BB because of the lower amount of force needed for dislocation | In BB, evaluation of the knee geometry can also help to determine the cause and mechanism |
Abbreviations: PLTP, posterolateral tibial plateau; BB, bone bruise; ACLR, anterior cruciate ligament reconstruction; MRI, magnetic resonance imaging; LFC, lateral femoral condyle; ROM, range of motion; IKDC, International Knee Documentation Committee; n, number; OR, odds ratio; LTP, lateral tibial plateau; MTP, medial tibial plateau; MFC, medial femoral condyle; KOOS, Knee Injury and Osteoarthritis Outcome Score; SF-36, Short Form-36; BMI, body mass index; ACL, anterior cruciate ligament; K1, module I of the KOOS score; K2, module II of the KOOS score; K3, module III of the KOOS score.
Table 3.
Biomechanical studies
| Study | Year | Aim | Materials and subjects | Intervention | Results | Conclusion | Clinical relevance |
|---|---|---|---|---|---|---|---|
| Sanders et al15 | 2000 | Show bone contusion patterns associated with different ligament injuries | Description | Pivot shift injury: ACL rupture with BB in PLTP and LFC (exact location in LFC depends on the flexion of the knee). Dashboard injury: PCL rupture with BB in the anterior tibial plateau. Hyperextension injury: PCL and ACL tears with BB in the anterior tibial plateau and the anterior part of the femoral condyles | BB pattern could be considered a footprint of the mechanism of injury | First study to collect all of the mechanism of injury and their relationship with the BB pattern | |
| Quelard et al36 | 2010 | Assess preoperative factors that correlate with prolonged ROM deficits after ACLR | 217 patients undergoing ACLR | ROM goniometric measurement at 6 weeks and 3 months. MRI evaluation of bone contusion | Delayed recovery correlated with limited preoperative ROM (P<0.001), BB of the lateral compartment (P<0.001), operative delay <45 days (P=0.003), and female sex (P=0.049). BB and limited preoperative ROM were correlated (P<0.001) | BB and reduced ROM are risk factors for delayed recovery from ACLR | Clinical postoperative management and rehabilitation protocols must consider BB lesions |
| Viskontas et al30 | 2008 | Correlate BB location patterns with mechanism of injury | 100 patients with ACL rupture (86 NC; 14 C) | BB assessment: frequency; location; depth; and intensity | Associated lesions were MCL (70% in the NC group and 71% in the C group); medial meniscal tear (38% NC; 36% C); and lateral meniscal tear (34% NC; 29% C). Statistically relevant prevalence of lateral compartment BB when compared to the medial compartment (both groups, P<0.001). Significantly more LTP BB in the NC group (P<0.019). More PLTP (posterior third) BB (P=0.045) and MTP (P=0.045). Greater intensity (grade 3) was found in the NC group (81% versus 36%; P<0.001). Higher intensity at the LTP in the NC group (P<0.001) | Significantly different BB patterns are shown for C and NC groups of lesions | Correlates BB incidence with the type of injury |
Abbreviations: ACL, anterior cruciate ligament; BB, bone bruise; PLTP, posterolateral tibial plateau; LFC, lateral femoral condyle; PCL, posterior cruciate ligament; ROM, range of motion; ACLR, anterior cruciate ligament reconstruction; MRI, magnetic resonance imaging; NC, noncontact; C, contact; MCL, medial collateral ligament; LTP, lateral tibial; MTP, medial tibial plateau.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Nicolini AP, de Carvalho RT, Matsuda MM, Sayum J, Cohen M. Common injuries in athletes’ knee: experience of a specialized center. Acta Ortop Bras. 2014;22(3):127–131. doi: 10.1590/1413-78522014220300475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sutton KM, Bullock JM. Anterior cruciate ligament rupture: differences between males and females. J Am Acad Orthop Surg. 2013;21(1):41–50. doi: 10.5435/JAAOS-21-01-41. [DOI] [PubMed] [Google Scholar]
- 3.Barenius B, Ponzer S, Shalabi A, Bujak R, Norlén L, Eriksson K. Increased risk of osteoarthritis after anterior cruciate ligament reconstruction: a 14-year follow-up study of a randomized controlled trial. Am J Sports Med. 2014;42(5):1049–1057. doi: 10.1177/0363546514526139. [DOI] [PubMed] [Google Scholar]
- 4.Faber KJ, Dill JR, Amendola A, Thain L, Spouge A, Fowler PJ. Occult osteochondral lesions after anterior cruciate ligament rupture. Six-year magnetic resonance imaging follow-up study. Am J Sports Med. 2014;27(4):489–494. doi: 10.1177/03635465990270041301. [DOI] [PubMed] [Google Scholar]
- 5.Lohmander LS, Englund PM, Dahl LL, Roos EM. The long-term consequence of anterior cruciate ligament and meniscus injuries: osteoarthritis. Am J Sports Med. 2007;35(10):1756–1769. doi: 10.1177/0363546507307396. [DOI] [PubMed] [Google Scholar]
- 6.Wen C, Lohmander LS. Osteoarthritis: Does post-injury ACL reconstruction prevent future OA? Nat Rev Rheumatol. 2014;10(10):577–578. doi: 10.1038/nrrheum.2014.120. [DOI] [PubMed] [Google Scholar]
- 7.Halinen J, Koivikko M, Lindahl J, Hirvensalo E. The efficacy of magnetic resonance imaging in acute multi-ligament injuries. Int Orthop. 2009;33(6):1733–1738. doi: 10.1007/s00264-008-0689-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Van Dyck P, Vanhoenacker FM, Lambrecht V, et al. Prospective comparison of 1.5 and 3.0-T MRI for evaluating the knee menisci and ACL. J Bone Joint Surg Am. 2013;95(10):916–924. doi: 10.2106/JBJS.L.01195. [DOI] [PubMed] [Google Scholar]
- 9.Mink JH, Deutsch AL. Occult cartilage and bone injuries of the knee: detection, classification, and assessment with MR imaging. Radiology. 1989;170(3 Pt 1):823–829. doi: 10.1148/radiology.170.3.2916038. [DOI] [PubMed] [Google Scholar]
- 10.Gupta R, Virayavanich W, Kuo D, et al. MR T1ρ quantification of cartilage focal lesions in acutely injured knees: correlation with arthroscopic evaluation. Magn Reson Imaging. 2014 Aug 8; doi: 10.1016/j.mri.2014.07.015. Epub. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Theologis AA, Kuo D, Cheng J, et al. Evaluation of bone bruises and associated cartilage in anterior cruciate ligament-injured and - reconstructed knees using quantitative t(1ρ) magnetic resonance imaging: 1-year cohort study. Arthroscopy. 2011;27(1):65–76. doi: 10.1016/j.arthro.2010.06.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bretlau T, Tuxøe J, Larsen L, Jørgensen U, Thomsen HS, Lausten GS. Bone bruise in the acutely injured knee. Knee Surg Sports Traumatol Arthrosc. 2002;10(2):96–101. doi: 10.1007/s00167-001-0272-9. [DOI] [PubMed] [Google Scholar]
- 13.Jelić D, Masulović D. Bone bruise of the knee associated with the lesions of anterior cruciate ligament and menisci on magnetic resonance imaging. Vojnosanit Pregl. 2011;68(9):762–766. doi: 10.2298/vsp1109762j. [DOI] [PubMed] [Google Scholar]
- 14.Hernández-Molina G, Guermazi A, Niu J, et al. Central bone marrow lesions in symptomatic knee osteoarthritis and their relationship to anterior cruciate ligament tears and cartilage loss. Arthritis Rheum. 2008;58(1):130–136. doi: 10.1002/art.23173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sanders TG, Medynski MA, Feller JF, Lawhorn KW. Bone contusion patterns of the knee at MR imaging: footprint of the mechanism of injury. Radiographics. 2000;20(Spec No):S135–S151. doi: 10.1148/radiographics.20.suppl_1.g00oc19s135. [DOI] [PubMed] [Google Scholar]
- 16.Nishimori M, Deie M, Adachi N, et al. Articular cartilage injury of the posterior lateral tibial plateau associated with acute anterior cruciate ligament injury. Knee Surg Sports Traumatol Arthrosc. 2008;16(3):270–274. doi: 10.1007/s00167-007-0458-x. [DOI] [PubMed] [Google Scholar]
- 17.Vellet AD, Marks PH, Fowler PJ, Munro TG. Occult posttraumatic osteochondral lesions of the knee: prevalence, classification, and short-term sequelae evaluated with MR imaging. Radiology. 1991;178(1):271–276. doi: 10.1148/radiology.178.1.1984319. [DOI] [PubMed] [Google Scholar]
- 18.Yoon KH, Yoo JH, Kim KI. Bone contusion and associated meniscal and medial collateral ligament injury in patients with anterior cruciate ligament rupture. J Bone Joint Surg Am. 2011;93(16):1510–1518. doi: 10.2106/JBJS.J.01320. [DOI] [PubMed] [Google Scholar]
- 19.Costa-Paz M, Muscolo DL, Ayerza M, Makino A, Aponte-Tinao L. Magnetic resonance imaging follow-up study of bone bruises associated with anterior cruciate ligament ruptures. Arthroscopy. 2001;17(5):445–449. doi: 10.1053/jars.2001.23581. [DOI] [PubMed] [Google Scholar]
- 20.Hanypsiak BT, Spindler KP, Rothrock CR, et al. Twelve-year follow-up on anterior cruciate ligament reconstruction: long-term outcomes of prospectively studied osseous and articular injuries. Am J Sports Med. 2008;36(4):671–677. doi: 10.1177/0363546508315468. [DOI] [PubMed] [Google Scholar]
- 21.Lynch TC, Crues JV, 3rd, Morgan FW, We Sheehan, Harter LP, Ryu R. Bone abnormalities of the knee: prevalence and significance at MR imaging. Radiology. 1989;171(3):761–766. doi: 10.1148/radiology.171.3.2717748. [DOI] [PubMed] [Google Scholar]
- 22.Gentili A, Seeger LL, Yao L, Do HM. Anterior cruciate ligament tear: indirect signs at MR imaging. Radiology. 1994;193(3):835–840. doi: 10.1148/radiology.193.3.7972834. [DOI] [PubMed] [Google Scholar]
- 23.McCauley TR, Moses M, Kier R, Lynch JK, Barton JW, Jokl P. MR diagnosis of tears of anterior cruciate ligament of the knee: importance of ancillary findings. AJR Am J Roentgenol. 1994;162(1):115–119. doi: 10.2214/ajr.162.1.8273648. [DOI] [PubMed] [Google Scholar]
- 24.Chin YC, Wijaya R, Chong LR, Chang HC, Lee YH. Bone bruise patterns in knee injuries: where are they found? Eur J Orthop Surg Traumatol. 2013 Sep 22; doi: 10.1007/s00590-013-1319-6. Epub. [DOI] [PubMed] [Google Scholar]
- 25.Munshi M, Davidson M, MacDonald PB, Froese W, Sutherland K. The efficacy of magnetic resonance imaging in acute knee injuries. Clin J Sport Med. 2000;10(1):34–39. doi: 10.1097/00042752-200001000-00007. [DOI] [PubMed] [Google Scholar]
- 26.Tung GA, Davis LM, Wiggins ME, Fadale PD. Tears of the anterior cruciate ligament: primary and secondary signs at MR imaging. Radiology. 1993;188(3):661–667. doi: 10.1148/radiology.188.3.8351329. [DOI] [PubMed] [Google Scholar]
- 27.Li X, Ma BC, Bolbos RI, et al. Quantitative assessment of bone marrow edema-like lesion and overlying cartilage in knees with osteoarthritis and anterior cruciate ligament tear using MR imaging and spectroscopic imaging at 3 Tesla. J Magn Reson Imaging. 2008;28(2):453–461. doi: 10.1002/jmri.21437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Huttner HB, Steiner T, Hartmann M, et al. Comparison of ABC/2 estimation technique to computer-assisted planimetric analysis in warfarin-related intracerebral parenchymal hemorrhage. Stroke. 2006;37(2):404–408. doi: 10.1161/01.STR.0000198806.67472.5c. [DOI] [PubMed] [Google Scholar]
- 29.Szkopek K, Warming T, Neergaard K, Jørgensen HL, Christensen HE, Krogsgaard M. Pain and knee function in relation to degree of bone bruise after acute anterior cruciate ligament rupture. Scand J Med Sci Sports. 2012;22(5):635–642. doi: 10.1111/j.1600-0838.2011.01297.x. [DOI] [PubMed] [Google Scholar]
- 30.Viskontas DG, Giuffre BM, Duggal N, Graham D, Parker D, Coolican M. Bone bruises associated with ACL rupture: correlation with injury mechanism. Am J Sports Med. 2008;36(5):927–933. doi: 10.1177/0363546508314791. [DOI] [PubMed] [Google Scholar]
- 31.Westermann RW, Wolf BR, Wahl CJ. Does lateral knee geometry influence bone bruise patterns after anterior cruciate ligament injury? A report of two cases. Iowa Orthop J. 2013;33:217–220. [PMC free article] [PubMed] [Google Scholar]
- 32.Davies NH, Niall D, King LJ, Lavelle J, Healy JC. Magnetic resonance imaging of bone bruising in the acutely injured knee – short-term outcome. Clin Radiol. 2004;59(5):439–445. doi: 10.1016/j.crad.2003.11.012. [DOI] [PubMed] [Google Scholar]
- 33.Bisson LJ, Kluczynski MA, Hagstrom LS, Marzo JM. A prospective study of the association between bone contusion and intra-articular injuries associated with acute anterior cruciate ligament tear. Am J Sports Med. 2013;41(8):1801–1807. doi: 10.1177/0363546513490649. [DOI] [PubMed] [Google Scholar]
- 34.Dunn WR, Spindler KP, Amendola A, et al. MOON ACL Investigation Which preoperative factors, including bone bruise, are associated with knee pain/symptoms at index anterior cruciate ligament reconstruction (ACLR)? A Multicenter Orthopaedic Outcomes Network (MOON) ACLR Cohort Study. Am J Sports Med. 2010;38(9):1778–1787. doi: 10.1177/0363546510370279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Johnson DL, Bealle DP, Brand JC, Jr, Nyland J, Caborn DN. The effect of a geographic lateral bone bruise on knee inflammation after acute anterior cruciate ligament rupture. Am J Sports Med. 2000;28(2):152–155. doi: 10.1177/03635465000280020301. [DOI] [PubMed] [Google Scholar]
- 36.Quelard B, Sonnery-Cottet B, Zayni R, Ogassawara R, Prost T, Chambat P. Preoperative factors correlating with prolonged range of motion deficit after anterior cruciate ligament reconstruction. Am J Sports Med. 2010;38(10):2034–2039. doi: 10.1177/0363546510370198. [DOI] [PubMed] [Google Scholar]
- 37.Geeslin AG, LaPrade RF. Location of bone bruises and other osseous injuries associated with acute grade III isolated and combined posterolateral knee injuries. Am J Sports Med. 2010;38(12):2502–2508. doi: 10.1177/0363546510376232. [DOI] [PubMed] [Google Scholar]