Abstract
OBJECTIVE
To describe a case of bilateral superior (SSCD) and posterior semicircular canal dehiscences (PSCD) and the use of a transmastoid approach unilaterally to address both defects simultaneously.
PATIENT PRESENTATION
In a patient with right-sided hyperacusis, bilateral SSCD and PSCD, located adjacent to the common crus, were found with a right-sided anterosuperiorly positioned sigmoid sinus and a high-riding jugular bulb. Audiogram and cervical vestibular evoked myogenic potentials testing was consistent with right-sided semicircular canal dehiscence. A right-sided transmastoid approach provided access to plug both defects simultaneously after posterior mobilization of the sigmoid sinus. The hyperacusis was completely resolved with a 10-30dB improvement in his right ear’s air conduction without decrement in bone conduction.
CONCLUSION
In properly selected patients, a transmastoid approach can be used to effectively manage SSCD and PSCD simultaneously. Preoperative CT is recommended to evaluate the sites of dehiscences and the presence of complicating vascular anatomy.
Keywords: mastoid, semicircular canals, vestibular evoked myogenic potential, hearing loss
INTRODUCTION
First described by Minor et al(1), superior semicircular canal dehiscence syndrome (SSCD) is characterized by absence of the bone overlying superior semicircular canal (SSC), which creates a so-called “third-window effect” and causes abnormal transmission of acoustic energy within the inner ear. With this defect, patients typically present with sound- and/or pressure-induced vertigo (Tullio phenomenon) and nystagmus in a vertical-torsional plane (1-3). Patients with SSCD may have other manifestations like low-frequency hearing loss (typically conductive), hyperacusis, autophony, and other unusual auditory phenomena. A spectrum of symptoms and signs associated with a defect involving the posterior canal (posterior semicircular canal dehiscence syndrome - PSCD) has been recently described (4-6). While unilateral SSC and posterior semicircular canal (PSC) dehiscences have been well-described in the literature, there are few reports of bilateral dehiscences of both SSC and PSC. Moreover, surgical management of dehiscences of multiple semicircular canals has never been reported. We present an unusual case of bilateral SSCD and PSCD and a transmastoid approach to simultaneously address both bony defects on one side where they had caused hearing loss and problematic hyperacusis.
CASE DESCRIPTION
A 52-year-old man presented with progressive right-sided hyperacusis, which interfered with his recreational and choir activities. He also described pain induced by high frequency sounds, right aural fullness, and autophony. He denied pressure- or sound-induced vertigo. However, he had experienced occasional but progressive imbalance. The patient had had significant environmental noise exposure and had a history of a significant head trauma while working in construction many years preceding the development of any of the troublesome symptoms mentioned above. His head and neck examination, including otoscopy, was normal. His fistula test was negative subjectively and objectively bilaterally. His remaining physical examination was normal except for a broad-based gait.
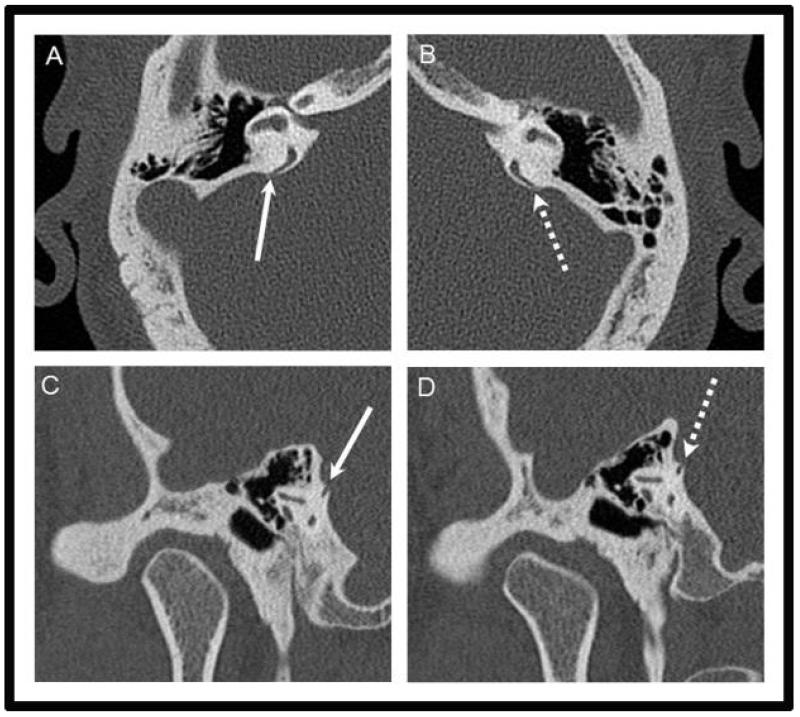
Audiometry revealed bilateral down-sloping sensorineural hearing loss (SNHL) in a noise-induced configuration (Figure 1). Additionally, there was a 10–20dB low frequency SNHL in the right ear. His word recognition testing scores were 84% and 92% on the right and left sides at 65dB respectively. Tympanometry was normal. A click-induced cervical vestibular evoked myogenic potential (VEMP) test demonstrated responses at 70dB normal hearing level (nHL) bilaterally (normal thresholds are around 95 nHL(2)), and an insignificant interaural amplitude difference. He complained of right ear discomfort and nystagmus subjectively at 95dB. With videonystagmography, no vertical or horizontal nystagmus was seen with sound or pressure stimuli. He had a spontaneous right-beating nystagmus and abnormal optokinetic and saccade testing suggesting a central aetiology. His caloric testing was normal. Magnetic resonance imaging performed five years prior to clinical presentation was normal. Temporal bone computed tomography (CT) in the axial and oblique planes revealed dehiscences of both superior (Figures 2A & 2C) and posterior (Figures 2B & 2D) canals on the right side of 2-3 mm. Interestingly, the superior dehiscence was not at the usual area at the dome of SCC but located more posteriorly and adjacent to the common crus. The posterior defect was also adjacent to the common crus. A similar pattern was detected on the contralateral side (Figure 3) but with smaller dehiscences (approximately 1mm each). While the lateral tegmen was not low-lying, CT delineated an anterosuperiorly positioned sigmoid sinus and a high-riding jugular bulb on the right side.
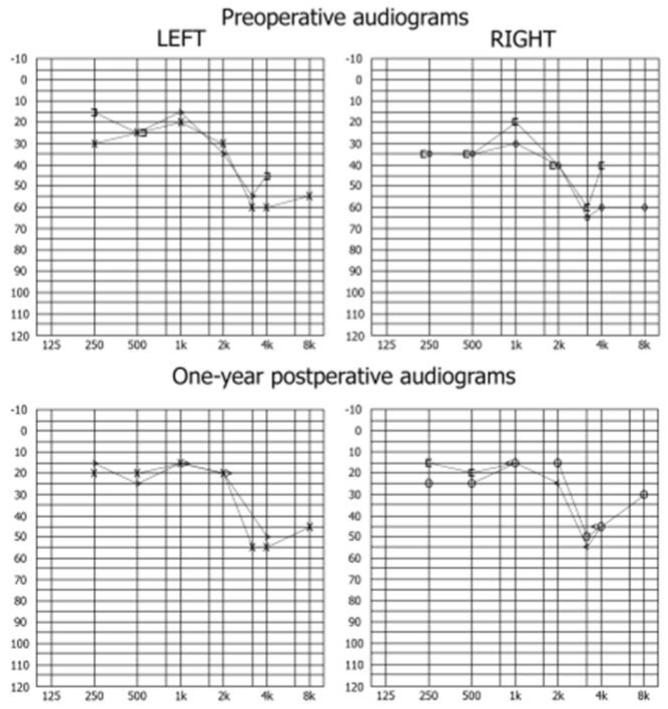
Figure 1.
Preoperative and 1-year postoperative audiograms. Of note, bone conduction thresholds from the 6 month postoperative were used in 1-year postoperative audiogram as these thresholds were not recorded at the one year time point.
Figure 2.
Axial (A and B) and oblique Poschl (C and D) images of the right (A and C) and left (B and D) temporal bone demonstrate bilateral dehiscence of the superior semicircular canal (arrowheads, A and C; arrows B and D) in close proximity to the common crus. Also note the anterior positioning of the groove for the right sigmoid sinus (A, asterisk) compared to the normal left side.
Figure 3.
Axial (A and B) and oblique Poschl (C and D) images of the right (A and C) and left (B and D) temporal bone demonstrate bilateral dehiscence of the posterior semicircular canal (arrows, A and C; dashed arrows B and D) also in close proximity to the common crus.
Motivated by his autophony and right-sided hyperacusis, the patient elected to undergo surgery. A transmastoid approach to address the right-sided PSCD and SCCD with intraoperative auditory brainstem response and electrocochleography monitoring was selected. To access the otic capsular structures, the aberrant sigmoid sinus required significant decompression and posterior mobilization. After skeletonization and blue-lining of SSC and PSC, small dehiscences (2-3mm each) of both canals were noted where the posterior fossa dura rested on exposed canal lumina. The lumina of the canals on either side of the dehiscences were exposed using micropicks, and temporalis fascia plugs were then gently advanced toward the ampullated and the common crus ends of each canal. Small bone chips were advanced behind the fascia plugs within the lumen of each canal, and bone pate was then placed over the area. Intraoperative ABR and electrocochleography waveforms were preserved throughout the procedure.
One month postoperatively, the patient experienced significant improvement in his right-sided hyperacusis although he described persistent right ear fullness. He developed symptoms of right benign positional vertigo (BPPV) and had a positive right-sided Dix-Hallpike manoeuvre. An Epley manoeuvre on the right effectively treated his symptoms. Of note, his hyperacusis was completely resolved at 3 months postoperatively, and he resumed all choir-related activities. He experienced some residual imbalance worsened by moving his head up or down. It resolved by one year postoperatively after a course of vestibular rehabilitation. His right-sided ear fullness was also improving at that time.
Audiograms demonstrated mild improvement in some of the patient’s bone conduction thresholds on the right side at 1 month and 3 month intervals. His one year postoperative audiogram demonstrated a 10-30dB improvement in the patient’s low frequency air conduction thresholds in the operative ear (Figure 1) and a speech discrimination score of greater than 92% with normal tympanometry. His contralateral thresholds were unchanged as was the high frequency, noise-induced configuration of hearing loss bilaterally.
DISCUSSION
We present a rare case of bilateral dehiscences of both SSC and PSC, in which the right-sided dehiscences were symptomatic. The aetiology of SCCD was proposed as a combination of a developmental abnormality resulting in thin bone overlying the SCC and disruption of this thin bony layer by head trauma or gradual degeneration (2). Zhou et al (7) expanded upon this idea and proposed a congenital defect of the entire middle fossa floor as the likely aetiology for semicircular canal dehiscence syndrome (SCD). While our patient’s head trauma could have contributed to his abnormal optokinetic and saccade testing and broad-based gait, the long interval between this event and the occurrence of his fistulous symptoms made it less likely to be a contributory factor in the development of his symptomatic dehiscences.
Our patient had an unusual presentation of SCD with troublesome hyperacusis as his primary complaint. Patients with SSCD often present with pressure- or sound-induced vertigo and nystagmus. These phenomena are due to the creation of a mobile third window into the inner ear as the result of the dehiscence, causing abnormal ampullofugal and ampullopetal endolymphic flow, which results in atypical activation or inhibition of the affected canals (1,3). PSCD has been shown to cause sound- and pressure-induced vertigo, disequilibrium, or no vestibular symptoms in some patients (4-8). Our patient was not affected by any significant vestibular symptoms. However, his hyperacusis had significantly interfered with his involvement in choir and his social interactions with his young children leading him to seek definitive management. Despite his somewhat unusual symptomatic presentation, he had low frequency hearing loss and abnormal VEMP thresholds, which are known to be associated with SSCD (8).
The anatomy of dehiscences described in our case is unusual. In their original and subsequent reports, Minor et al (1,9) described SSCD occurring at the roof of the SSC. However, there appeared to be some variability in the location of the bony dehiscences in SSCD (9,10). The location of PSCD also appeared to be more variable. Brantberg et al(6) reported a case of PSCD close to the ampulla. In another radiologic report, defects could be seen along either the caudal portion or the cephalic portion of the PSC (4). In our report, the defects were found to be very close to the common crus. Interestingly, high-riding jugular bulbs were seen in the majority of patients with PSCD (4), as we observed in our patient.
The unusual anatomy dictated our choice of operative approach as a middle fossa approach would not have provided adequate exposure to address both of the canal dehiscences simultaneously. While the transmastoid approach was complicated by the anteriorly positioned sigmoid sinus, we were able to effectively mobilize this vessel posteriorly to provide adequate access for successful plugging of the involved canals. Doing so resulted in a marked improvement in the patient’s primary symptom of hyperacusis as well as a 10-30dB improvement in his air conduction thresholds without affecting his cochlear function.
The postoperative development of BPPV-like symptoms/findings in our patient was very surprising, given that plugging of PSC was shown to effectively treat intractable BPPV (11). Possible explanations include cupulolithiasis or incomplete occlusion of the posterior canal. Regardless, a repositioning manoeuvre eliminated the observed nystagmus and resulted in resolution of the patient’s associated positional symptoms.
SUMMARY.
Dehiscence of both superior and posterior canals, which can occur bilaterally, may present with a spectrum of symptoms atypical from the more common superior semicircular canal dehiscence syndrome.
Dehiscences of the superior semicircular canal dehiscence syndrome and posterior semicircular canal dehiscence syndrome may occur close to the common crus.
Computed topographic imaging and vestibular evoked myogenic potential should be used as complimentary studies to clearly define the location and size of the canal dehiscences and identify preoperatively any aberrant vascular or dural anatomy that may complicate surgical management.
A transmastoid approach can enable effective and simultaneous management of dehiscences of the posterior semicircular canal and superior semicircular canal.
ACKNOWLEGDEMENT
This project was supported by the Clinical and Translational Science Award (CTSA) program, previously through the National Centre for Research Resources (NCRR) grant 1UL1RR025011, and now by the National Centre for Advancing Translational Sciences (NCATS), grants 9U54TR000021. Gubbels SP (senior author) receives support from NM 1 R03 DC012432-01 and P30 HD003352.
REFERENCES
- 1.Minor LB, Solomon D, Zinreich JS, Zee DS. Sound- and/or pressure-induced vertigo due to bone dehiscence of the superior semicircular canal. Arch Otolaryngol Head Neck Surg. 1998;124:249–58. doi: 10.1001/archotol.124.3.249. [DOI] [PubMed] [Google Scholar]
- 2.Minor LB, Cremer PD, Carey JP, Della Santina CC, Streubel SO, Weg N. Symptoms and signs in superior canal dehiscence syndrome. Ann N Y Acad Sci. 2001;942:259–73. doi: 10.1111/j.1749-6632.2001.tb03751.x. [DOI] [PubMed] [Google Scholar]
- 3.Banerjee A, Whyte A, Atlas MD. Superior canal dehiscence: review of a new condition. Clin Otolaryngol. 2005;30:9–15. doi: 10.1111/j.1365-2273.2004.00940.x. [DOI] [PubMed] [Google Scholar]
- 4.Gopen Q, Zhou G, Poe D, Kenna M, Jones D. Posterior semicircular canal dehiscence: first reported case series. Otol Neurotol. 2010;31:339–44. doi: 10.1097/MAO.0b013e3181be65a4. [DOI] [PubMed] [Google Scholar]
- 5.Krombach GA, DiMartino E, Schmitz-Rode T, Prescher A, Haage P, Kinzel S, et al. Posterior semicircular canal dehiscence: a morphologic cause of vertigo similar to superior semicircular canal dehiscence. Eur Radiol. 2003;13:1444–50. doi: 10.1007/s00330-003-1828-5. [DOI] [PubMed] [Google Scholar]
- 6.Brantberg K, Bagger-Sjoback D, Mathiesen T, Witt H, Pansell T. Posterior canal dehiscence syndrome caused by an apex cholesteatoma. Otol Neurotol. 2006;27:531–4. doi: 10.1097/01.mao.0000201433.50122.62. [DOI] [PubMed] [Google Scholar]
- 7.Zhou G, Gopen Q, Poe DS. Clinical and diagnostic characterization of canal dehiscence syndrome: a great otologic mimicker. Otol Neurotol. 2007;28:920–926. [PubMed] [Google Scholar]
- 8.Chien WW, Carey JP, Minor LB. Canal dehiscence. Curr Opin Neurol. 2011;24:25–31. doi: 10.1097/WCO.0b013e328341ef88. [DOI] [PubMed] [Google Scholar]
- 9.Minor LB. Superior canal dehiscence syndrome. Am J Oto. 2000;21:9–19. [PubMed] [Google Scholar]
- 10.Rajenderkumar D, Farrell KL, Alles RM, Savy L. Multiple dehiscence of semicircular canals. J Laryngol Otol. 2007;121:80–2. doi: 10.1017/S0022215106003537. [DOI] [PubMed] [Google Scholar]
- 11.Beyea JA, Agrawal SK, Parnes LS. Transmastoid semicircular canal occlusion: a safe and highly effective treatment for benign paroxysmal positional vertigo and superior canal dehiscence. Laryngoscope. 2012;122:1862–6. doi: 10.1002/lary.23390. [DOI] [PubMed] [Google Scholar]