Abstract
Study Design
Retrospective matched–cohort analysis.
Objective
To evaluate the change in radiographic parameters in patients undergoing interbody fusion and posterior instrumentation compared to posterior spine fusion alone (PSF) for degenerative scoliosis.
Summary of Background Data
Little is known about the effect of lateral interbody fusion (LIF) on sagittal plane correction in the setting of degenerative scoliosis. We performed a retrospective study to investigate these changes compared to PSF.
Methods
Between 1997 and 2011, 33 patients had LIF at 181 levels between T8 and L5 vertebrae for the treatment of degenerative scoliosis (mean; 5±2 levels). Of those, 23 patients had additional anterior lumbar interbody fusion (ALIF) at 37 levels between L4 and S1 vertebrae (mean; 1.6±0.5 levels). A 1:1 matched control of patients who underwent PSF was performed. Patients were matched by age, gender, and diagnosis. Clinical and radiographic data were collected and compared between the matched cohorts.
Results
Lumbar lordosis was significantly restored in LIF±ALIF compared to PSF cohort (44°±14° versus 36°±15°, p=0.02). The segmental lumbar lordosis over the 102 LIF levels significantly improved from 12°±10° to 21°±13° postoperatively (p<0.0001). However, the change over the 37 ALIF levels was not significant (from 30°±15° to 29°±9°, p=0.8). Sagittal plane alignment was improved in LIF±ALIF compared to PSF cohort and trended toward but did not reach significance (3.8±3.2 cm versus 6.2±5.7 cm, p=0.09). Sacral slope was significantly higher in LIF±ALIF compared to PSF cohort (33°±11° versus 28°±10°, p=0.03). Pelvic tilt was lower in LIF±ALIF compared to PSF cohort and trended toward but did not reach significance (22°±10° versus 26°±10°, p=0.08).
Conclusion
Lumbar lordosis and sacral slope were mildly but statistically improved in the interbody fusion cohort compared to PSF cohort. Sagittal alignment and pelvic tilt trended toward but did not reach statistical significance. Segmental lumbar lordosis was improved at LIF levels more than at ALIF levels.
Keywords: lateral interbody fusion, anterior lumbar interbody fusion, posterior spine fusion, sagittal alignment, coronal plane, spinopelvic parameters, degenerative scoliosis
Introduction
Several surgical techniques have been utilized for the treatment of degenerative scoliosis. Traditionally, this has involved posterior instrumented spine fusion alone (PSF). This approach allows decompression of neural elements and simultaneous instrumented fusion with reasonably high fusion rates1. Recent advances in minimally invasive techniques have popularized fusion techniques utilizing interbody fusion grafts to obtain deformity correction, indirect decompression and arthrodesis followed by posterior instrumentation through either open or percutaneous techniques. These interbody fusion techniques are associated with high fusion rates however need to be balanced against the increased level of invasiveness and complications that can be encountered with these techniques. The anterior retroperitoneal approach for anterior lumbar interbody fusion (ALIF) carries an increased risk of vascular and visceral injures1–6. The minimally invasive lateral transpsoas interbody fusion (LIF) has a lower incidence of vascular injuries but maybe associated with a higher neuropraxia rate related to retraction of the lumbar plexus.1,7–10. The circumferential surgery has a very high arthrodesis rate and can allow extension to the pelvis which may limit the degeneration of distal unfused segments6,11. Clinical studies have demonstrated that interbody fusion grafts are associated with high fusion rates and improvement in sagittal balance3–6,8–10. This improvement was also reported in cadaveric studies12. Sagittal balance has been correlated with health–related quality of life measures13–15. Thus, restoring the sagittal alignment should be one of the primary goals in the treatment of degenerative scoliosis. Further, there is limited data in literature regarding the effect of the interbody fusion, and specifically LIF on spinopelvic parameters (pelvic incidence, pelvic tilt, and sacral slope)16,17. The pelvic incidence (PI) determines the lumbar lordosis (LL). Boulay et.18 established the predictive equation for lumbar lordosis while Schwab et al.19 expressed it simply as “LL = PI + 9° (± 9)” based on healthy asymptomatic adults. The pelvic incidence (PI) is an anatomical, constant parameter in each skeletally mature individual and independent of the position of pelvis20,21. The pelvic tilt (PT) could compensate for the spinal deformity through pelvic retroversion (increasing of PT)19,22. Lastly, the sacral slope (SS) completes the geometric relationship between these spinopelvic parameters in which the pelvic incidence is the total of the pelvic tilt and the sacral slope (PI = PT + SS)19–23.
In this study, we evaluate the change in sagittal and coronal plane alignment, lumbar lordosis, and spinopelvic parameters on patients who had interbody fusion utilizing LIF ± ALIF compared to PSF alone for degenerative scoliosis. We hypothesized that patients treated with the interbody fusion techniques would have improved radiographic parameters compared with those treated with PSF alone.
Materials and Methods
A diagnostic and surgical database was queried for patients who underwent spine fusion at Mayo Clinic. Between 1997 and 2011, 33 patients underwent lateral interbody fusion (LIF) with or without a simultaneous anterior lumbar interbody fusion for the treatment of degenerative scoliosis (LIF ± ALIF cohort). A 1:1 matched control group was created from patients who underwent posterior spine fusion alone using instrumentation and bone graft during the same time frame for the same diagnosis of degenerative scoliosis (PSF cohort). The control cohort was matched for gender, age, and diagnosis. Patients were followed for 1.8 years (1.7 month– 3.3 years) in LIF ± ALIF cohort, and 2.7 years (1.5 month–7.8 years) in PSF cohort. Ten patients did not reach a minimum of one year follow–up (nine patients missed their evaluation and one died) (Table 1).
Table 1.
Patients’ characteristics
| Parameters | LIF ± ALIF Cohort | PSF cohort | p–value |
|---|---|---|---|
| Male patients | 7 | 7 | |
| Female patients | 26 | 26 | |
| Age* (years) | 66 ± 8 | 67 ± 9 | |
| Posterior fusion level* | 10 ± 3 | 7 ± 5 | 0.02 |
| Posterior fusion to sacrum/pelvis (patients) | 28 (85%) | 10 (30%) | 0.0001 |
| Time to follow–up† (range) | 1.8 years (1.7 month– 3.3 years) | 2.7 years (1.5 month–7.8 years) |
Values are expressed as mean ± standard deviation,
Values are expressed as mean with the range in parentheses.
LIF ± ALIF cohort: Patients underwent, in addition to posterior fusion constructs, LIF with or without a simultaneous ALIF. PSF cohort: Patients underwent posterior spine fusion alone (PSF) using instrumentation and bone graft.
P value in boldface indicates a statistical significance.
LIF indicates lateral interbody fusion; ALIF, anterior lumbar interbody fusion; PSF, posterior spine fusion.
Medical records were retrospectively reviewed until the most recent clinical evaluation. Patients’ demographics, operative details, and complications requiring additional operations were collected. The numberical visual analogue scale (VAS) for back and lower extremity pain (total 10 points) were recorded before the index procedure and at follow-up. A radiographic analysis was also conducted before the index procedure and at follow–up. The analysis was performed on an in–house computerized radiographic tool and all measurements were made by one author AP and lateral standing radiographs were analyzed for the following parameters (Figure 1).
Coronal Cobb angle: It is measured from the angle formed between the superior end plate of the upper tilted vertebra and the inferior end plate of the lower tilted vertebra24.
Sagittal vertical alignment (SVA): The horizontal distance from the posterosuperior aspect of the S1 to the vertical line drawn through the midbody of C7 vertebra (C7 plumbline)21,25.
Global lumbar lordosis (LL): It is measured from the angle formed between the superior end plate of the L1 to the superior endplate of the S121,25.
Segmental lordosis: It is measured from the angle formed between the end plates of upper and lower vertebras at the segment of interest.
Pelvic incidence (PI): The angle between the line through the midpoint of the superior sacral end plate to the center of femoral head, and the line perpendicular to the midpoint of the superior sacral end plate21,25.
Pelvic tilt (PT): The angle between the line through the midpoint of the superior sacral end plate to the center of femoral head, and the vertical reference line21,25.
Sacral slope (SS): The angle between the superior sacral end plate, and the horizontal reference line21,25.
Figure 1.
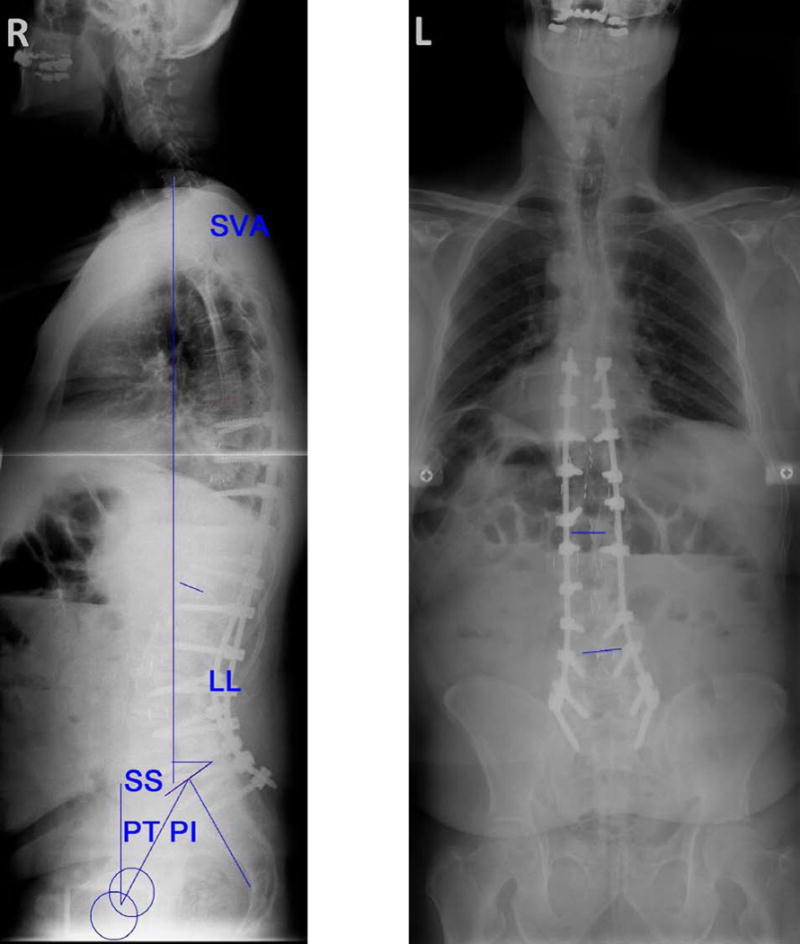
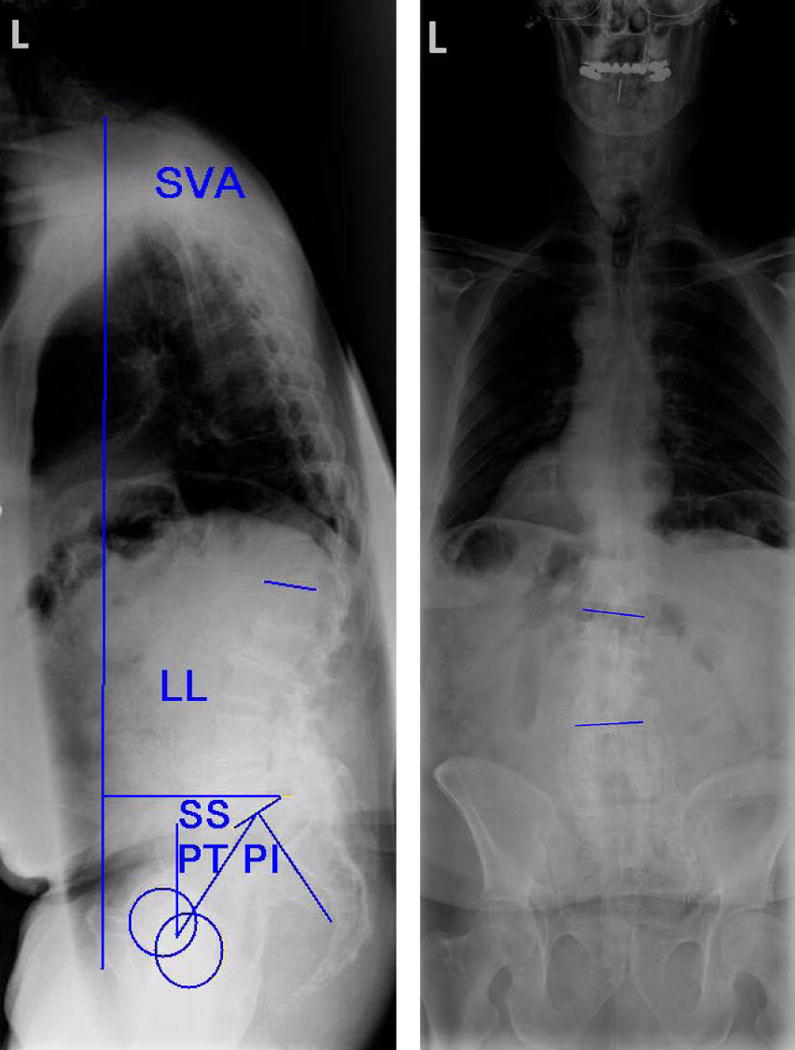
|
| ||||||
| Coronal Cobb angle (°) | SVA | LL | PT | SS | PI | |
|
| ||||||
| Preoperative | 15° | 13 cm | 43° | 33° | 34° | 67° |
|
| ||||||
| Postoperative | 6° | 4.1 cm | 57° | 29° | 35° | 64° |
|
| ||||||
| Sagittal Vertical Alignment (SVA), Lumbar Lordosis (LL), Pelvic Tilt (PT), Sacral Slope (SS), and Pelvic Incidence (PI).
| ||||||
Since full–length AP and Lateral radiographs were not available for all patients, changes in sagittal vertical alignment are reported for 32 patients in the LIF ± ALIF cohort and 23 patients in the PSF cohort. Changes in coronal Cobb angle are reported for 30 patients in the PSF cohort. The remaining parameters are reported for all patients.
PSF was performed with a traditional midline open muscle stripping technique with pedicle screw and hook fixation of the spine. ALIF was performed utilizing a midline retroperitoneal approach to the spine with diskectomy and implant placement. LIF was performed utilizing a lateral transpsoas approach with the neural monitoring for the treatment of lumbar spine and a lateral transthoracic or thoracoabdominal approach with or without rib resection for the treatment of thoracic and upper lumbar levels. Diskectomy was performed followed by implant placement. Posterior instrumentation after interbody fusion consisted either traditional midline muscle stripping approach in the minority of cases or percutaneous spinal fixation in the majority of cases.
LIF technique was performed for 181 levels (102 lumbar, and 79 thoracic) using Clydesdale® spinal system interbody device (Medtronic Sofamor Danek, Memphis, TN, USA). This was performed between T8 and L5 with a mean of 5 ± 2 levels per patient (Table 2). One patient underwent one–level, four patients underwent two–level, four patients underwent four–level, three patients underwent five–level, nine patients underwent six–level, nine patients underwent seven–level and three patients underwent eight–level procedures. Of the 33 patients, 23 also underwent an ALIF at L5–S1 or L4–S1at the index procedure using Sovereign® spinal system interbody device (Medtronic Sofamor Danek, Memphis, TN, USA) (Table 2). ALIF was performed when fusion to the pelvis was indicated in order to increase the arthrodesis rate and improve the lumbar lordosis at lumbosacral junction. Fourteen ALIFs were impacted at L4–L5, and twenty–three at L5–S1. Nine patients underwent one–level, and 14 patients underwent two–level procedures. All patients had posterior instrumentation through either traditional midline muscle stripping approach (five patients) or percutaneous spinal fixation (28 patients). The fluoroscopy was used for instrumentation placement in 24 patients and O–arm with stealth navigation for instrumentation in nine patients. Twenty–eight patients had posterior–based facetectomies utilizing a minimally invasive technique through tubular retractors combined with percutaneous instrumentation, and the remainder five patients had open facetectomies. The mean number of posterior fusion levels were higher in LIF ± ALIF cohort compared to PSF cohort (10 ± 3 versus 7 ± 5, p = 0.02).
Table 2.
Levels of LIF and ALIF techniques.
| Thoracic | Lumbar | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Technique | T8–T9 | T9–T10 | T10–T11 | T11–T12 | T12–L1 | L1–L2 | L2–L3 | L3–L4 | L4–L5 | L5–S1 | Total |
| LIF | 1 | 8 | 20 | 24 | 26 | 29 | 30 | 30 | 13 | 0 | 181 |
| ALIF | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 14 | 23 | 37 |
LIF: lateral interbody fusion. ALIF: anterior lumbar interbody fusion.
Unless otherwise specified, data is expressed as mean ± standard deviation and n indicates number of patients. The preoperative radiographic parameters (baseline) were compared to their corresponding values measured postoperatively using paired t–tests. Binary variables were compared between the matched sets using McNemar’s test. Continuous variables (radiographic parameters or VAS pain scores) were compared between the matched sets using paired t–tests. All statistical tests were two–sided and p–values less than 0.05 were considered to be statistically significant. JMP® version 9.0.1 was used for statistical analysis (SAS Institute Inc, SAS Campus Drive, Cary, NC, USA 27513).
Institutional review board approval was obtained for all aspects of this study.
Results
There was no observed difference in preoperative radiographic parameters between the matched case–control sets, with the exception of preoperative coronal Cobb angle which was higher in LIF ± ALIF cohort compared to the PSF cohort (39° ± 18° versus 25° ± 15°, p=0.004) (Table 3). Additionally, postoperative fusion levels were higher in LIF ± ALIF cohort compared to PSF cohort (10 ± 3 versus 7 ± 5, p = 0.02).
Table 3.
Mean Values and Matching Comparison Results for the Radiographical Parameters of the LIF ± ALIF Cohort and PSF Cohort
| Parameters | n | LIF ± ALIF cohort | PSF cohort | p–value |
|---|---|---|---|---|
| Preoperative parameters | ||||
| Sagital vertical aligment† | 22 | 4.9 ± 4.7 | 5.9 ± 4.3 | 0.4 |
| Coronal Cobb angle* | 30 | 39° ± 18° | 25° ± 15° | 0.004 |
| Lumbar lordosis* | 33 | 38° ± 14° | 38° ± 16° | 1 |
| Pelvic incidence* | 33 | 59° ± 16° | 56° ± 15° | 0.4 |
| Pelvic tilt* | 33 | 28° ± 11° | 27° ± 11° | 0.8 |
| Sacral slope* | 33 | 32° ± 12° | 29° ± 12° | 0.5 |
| Postoperative parameters | ||||
| Sagital vertical aligment† | 22 | 3.8 ± 3.2 | 6.2 ± 5.7 | 0.09 |
| Coronal Cobb angle* | 30 | 16° ± 11° | 18° ± 15° | 0.6 |
| Lumbar lordosis* | 33 | 44° ± 14° | 36° ± 15° | 0.02 |
| Pelvic incidence* | 33 | 55° ± 13° | 54° ± 11° | 0.5 |
| Pelvic tilt* | 33 | 22° ± 10° | 26° ± 10° | 0.08 |
| Sacral slope* | 33 | 33° ± 11° | 28° ± 10° | 0.03 |
| Change between postoperative and preoperative parameters | ||||
| Sagital vertical aligment† | 22 | – 1.1 ± 4 | 0.3 ± 5 | 0.3 |
| Coronal Cobb angle* | 30 | – 24° ± 13° | – 7° ± 14° | <0.0001 |
| Lumbar lordosis* | 33 | 6° ± 16° | – 2° ± 12° | 0.04 |
| Pelvic incidence* | 33 | – 4° ± 10° | – 2° ± 14° | 0.6 |
| Pelvic tilt* | 33 | – 5° ± 13° | – 0.5° ± 9° | 0.06 |
| Sacral slope* | 33 | 2° ± 13° | – 2° ± 11° | 0.3 |
Values were measured in centimeters and presented as mean ± standard deviation.
Values were measured in degrees and presented as mean ± standard deviation.
n value indicates number of matched case–control sets.
LIF ± ALIF cohort: Patients underwent, in addition to posterior fusion constructs, LIF with or without a simultaneous ALIF.
PSF cohort: Patients underwent posterior spine fusion alone (PSF) using instrumentation and bone graft.
P value in boldface indicates a statistical significance.
LIF ± ALIF Cohort
Radiographic evaluation
Within the LIF ± ALIF cohort, the mean preoperative and postoperative radiographic parameters showed a significant change in coronal Cobb angle, lumbar lordosis, and pelvic tilt (Figure 2). Changes in sagittal vertical alignment trended towards but did not reach significance (p=0.08). There was no detected difference in sacral slope following surgery (Figure 2). In detail, mean coronal Cobb angle significantly corrected from 39° ± 19° preoperatively to 15° ± 11° postoperatively (change; −24° ± 14°, p<0.0001, n=33). Mean lumber lordosis significantly improved from 38° ± 14° preoperatively to 44° ± 14° postoperatively (change; 6° ± 16°, p=0.047, n=33). Mean positive sagittal balance improved from 5.6 ± 5 cm preoperatively to 4.3 ± 3 cm postoperatively that trended towards but did not reach statistical significance (change; −1.3 ± 4 cm, p=0.08, n=32). There were five patients (15%) where positive sagittal balance shifted from >4 cm to ≤4 cm. Evaluating the spinopelvic parameters, mean pelvic tilt significantly changed from 28° ± 11° preoperatively to 22° ± 10° postoperatively (change; −5° ± 13°, p=0.03, n=33). There was no significant change in mean sacral slope (32° ± 12° preoperatively to 33° ± 11° postoperatively, p=0.5, n=33).
Figure 2.
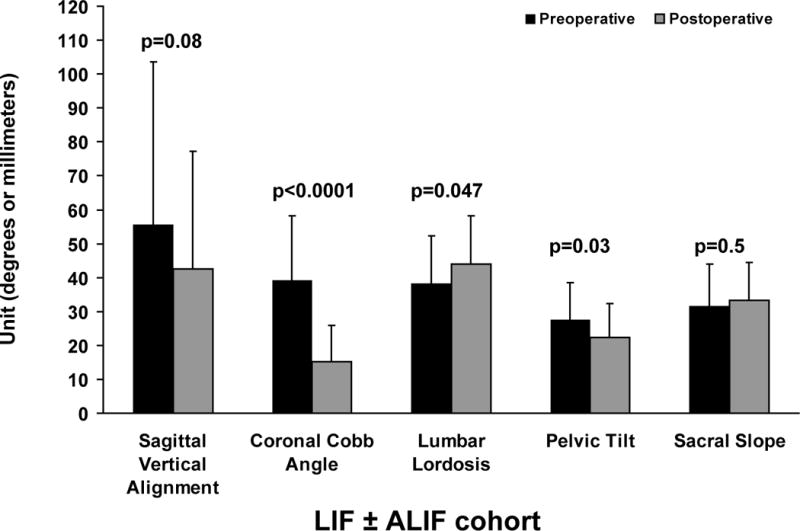
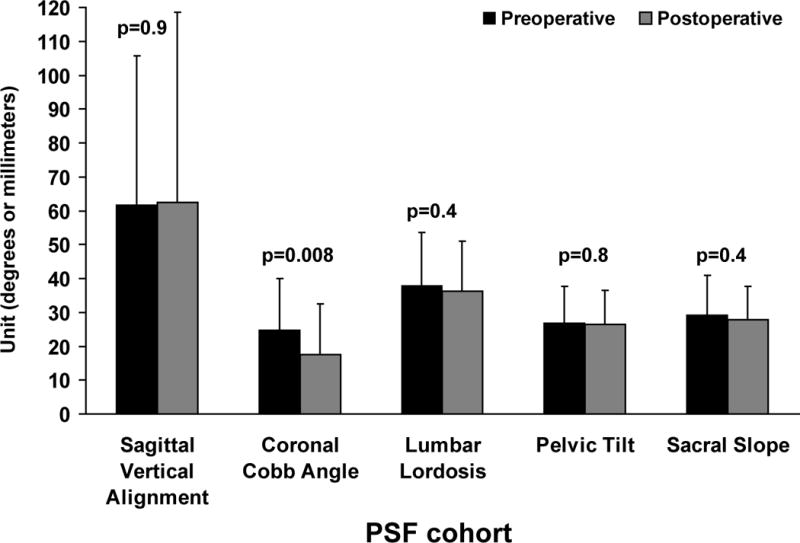
The mean and upper standard deviation for preoperative and postoperative radiographical parameters of the LIF ± ALIF cohort and PSF cohort were shown. P values of paired t tests were also presented. LIF indicates lateral interbody fusion; ALIF, anterior lumbar interbody fusion; PSF, posterior spine fusion.
Additional operations and VAS for pain
Within the LIF ± ALIF cohort, mean VAS for back pain score (total 10 points) significantly lessened from 8 ± 2 preoperatively to 2 ± 3 postoperatively (p<0.0001). Mean VAS for lower extremity pain score significantly lessened from 4 ± 4 preoperatively to 1.5 ± 3 postoperatively (p=0.002). Complications requiring additional operations were performed for 11 patients (33%) including revision or removal of posterior fusion constructs in four patients (12%) (Table 4).
Table 4.
Complications requiring additional operations
| LIF ± ALIF cohort | Patients |
|---|---|
| Surgical wound complication | 4 |
| Extension of fusion for PJK | 2 |
| Hardware removal | 1 (dislodged) 1 (symptomatic) |
| Decompression for neurological deterioration | 3 |
| PSF cohort | |
| Surgical wound complication | 4 |
| Extension of fusion for PJK and/or distal adjacent segment disease. | 1 (proximal) 2 (distal) 1 (both) |
| Hardware removal | 1 (symptomatic) |
| Pseudoarthrosis repair | 3 |
| Pseudomeningocele repair | 1 |
PJK: proximal junctional kyphosis
LIF ± ALIF cohort: Patients underwent, in addition to posterior fusion constructs, LIF with or without a simultaneous ALIF.
PSF cohort: Patients underwent posterior spine fusion alone (PSF) using instrumentation and bone graft.
PSF cohort
Radiographic evaluation
Within the PSF cohort, there was only a significant change in coronal Cobb angle but not any of their sagittal plane radiographic parameters following surgery (Figure 2). In detail, mean coronal Cobb angle significantly corrected from 25° ± 15° preoperatively to 18° ± 15° postoperatively (change; −7° ± 14°, p=0.008, n=30). Mean lumbar lordosis was 38° ± 16° preoperatively and 36° ± 15° postoperatively (change; −2° ± 12°, p=0.4, n=33). Mean positive sagittal vertical alignment changed from 6.2 ± 4 cm preoperatively to 6.2 ± 6 cm postoperatively (change; 0.1 ± 5 cm, p=0.9, n=23). Evaluating the spinopelvic parameters, there was no significant change in mean pelvic tilt (27 ± 11 preoperatively to 26 ± 10 postoperatively, p=0.8, n=33), or sacral slope (29 ± 12 preoperatively to 28 ± 10 postoperatively, p=0.4, n=33).
Additional operations and VAS for pain
Within the PSF cohort, mean VAS for back pain score significantly lessened from 7 ± 3 preoperatively to 3 ± 3 postoperatively (p<0.0001). Mean VAS for lower extremity pain score significantly lessened from 5 ± 4 preoperatively to 2 ± 3 postoperatively (p<0.0001). Complications requiring additional operations were performed for 13 patients (39%) including revision or removal of posterior fusion constructs in eight patients (24%) (Table 4).
Comparison of Matched Cohorts
Radiographic evaluation
When comparing postoperative values between the matched cohorts, lumbar lordosis and sacral slope were statistically improved in LIF ± ALIF cohort compared to PSF cohort. There was a trend towards improvement in sagittal alignment and pelvic tilt favoring the LIF ± ALIF cohort compared to PSF cohort but this did not reach statistical significance (Table 3).
When comparing the change between postoperative and preoperative values between the matched cohorts, coronal Cobb angle and lumbar lordosis were statistically improved to a greater degree in the interbody fusion cohort (Table 3). In detail, lumbar lordosis changed by 6° ± 16° in LIF ± ALIF cohort compared to −2° ± 12° in PSF cohort (p=0.04). Coronal Cobb angle changed by −24° ± 13° in LIF ± ALIF cohort compared to −7° ± 14° in PSF cohort (p<0.0001). Pelvic tilt change by −5° ± 13° in LIF ± ALIF cohort compared to −0.5° ± 9° in PSF cohort, which trended toward but did not reach statistical significance (p=0.06) (Table 3).
VAS for pain
When comparing postoperative VAS pain scores between the matched cohorts, mean VAS for back pain score was 2 ± 3 and 3 ± 3 points in LIF ± ALIF cohort and PSF cohort respectively (p=0.2), and mean VAS for lower extremity pain score was 1.5 ± 3 and 2 ± 3 points in LIF ± ALIF cohort and PSF cohort respectively (p=0.6).
Segmental Changes in Lumbar Lordosis
We also compared the segmental lumbar lordosis correction achieved with LIF technique versus ALIF technique. The preoperative and postoperative segmental lumbar lordosis was compared between 102 levels treated with the LIF technique, and 37 levels treated with the ALIF technique (Table 5). Over the LIF levels, the segmental lumbar lordosis was significantly improved by a mean of 9° ± 10° (p<0.0001). No significant improvement in the segmental lumbar lordosis was found over the ALIF levels, with a mean change of −1° ± 13° (p=0.8). This demonstrates in our cohort that greater lordosis correction was achieved at LIF levels compared to ALIF levels, although this is not a direct comparison of the two techniques as they were rarely performed at the same levels. ALIF was frequently performed at L4–L5 and L5–S1 whereas LIF was never performed at L5–S1 and rarely performed at L4–L5.
Table 5.
Lumbar lordosis at LIF levels and ALIF levels
| Technique | Levels (patients) | Levels/patient* | Preoperative lordosis* | Postoperative lordosis* | Change* | p–value† |
|---|---|---|---|---|---|---|
| LIF | 102 (33) | 3 ± 1 | 12° ± 10° | 21° ± 13° | 9° ± 10° | <0.0001 |
| ALIF | 37 (23) | 1.6 ± 0.5 | 30° ± 15° | 29° ± 9° | – 1° ± 13° | 0.8 |
Values are expressed as mean ± standard deviation.
p–value for the comparison between the mean preoperative and postoperative lordosis values.
LIF: lateral interbody fusion. ALIF: anterior lumbar interbody fusion.
P value in boldface indicates a statistical significance.
Discussion
Primary degenerative scoliosis or “de novo” scoliosis develops in a previously straight spine secondary to degenerative changes of the facet joints, disk space, and other structural elements of the vertebral column1,26. Degenerative scoliosis is common with prevalence up to 68% in asymptomatic elderly population1,27. While many surgical spine fusion techniques exist for the treatment of degenerative scoliosis, the most common involve posterior instrumented fusion1,26. With these approaches, surgeons often corrected the deformity with focus on coronal rather than sagittal plane. Restoration of sagittal balance has been shown to correlate with better patient–reported health outcomes. Surgical management should ideally restore normal sagittal alignment by correcting the deformity13–15. For that purpose, the interbody fusion has been gaining popularity as this technique enhances spine arthrodesis rates and has been theorized to improve sagittal balance2–10.
We demonstrate that global lumbar lordosis and sacral slope were significantly improved in the LIF ± ALIF cohort compared to PSF cohort. There was a trend for improvement in sagittal vertical alignment and pelvic tilt favoring LIF ± ALIF cohort compared to PSF cohort but this did not reach statistical significance. The significant difference in postoperative lumbar lordosis between the matched cohorts was due to the gain in segmental lordosis over LIF levels, not ALIF levels. Because of risks associated with the ALIF technique, it might be indicated at lower fusion segments (L4 to S1) to enhance arthrodesis, rather than correcting deformity in all cases. This may be related to the unique anatomy of the lower lumbar segments. These segments are often significantly lordotic and the addition of an interbody fusion may not result in additional segmental lordosis at these segments. There are probably exceptions to this finding when these segments have significant disk degeneration and collapse, however this was not specifically investigated in our study due to the small number of patients in our cohorts.
Several studies have reported on the effect of lateral lumbar interbody fusion in the treatment of lumbar scoliosis8,28,29. Yson et al.29 reported significant gain in the segmental lumbar lordosis following lateral lumbar interbody fusion in 56 patients (88 levels). Kotwal et al.8 found that the segmental disc height, the segmental coronal angle, the segmental lordotic angle, excluding the T12–L1 lordotic angle, and the coronal Cobb angle were significantly restored following lateral lumbar interbody fusion in 118 patients (237 levels). Acosta et al.9 reported significant correction in the segmental, the regional, and the global coronal plane alignment, but not the regional lumbar lordosis or the global sagittal alignment following lateral lumbar interbody fusion in 36 patients (66 levels). Johnson et al.16 found significant correction of the coronal Cobb angle and the segmental lumbar lordosis, but not the global lumbar lordosis or the spinopelvic indices (pelvic incidence, pelvic tilt, and sacral slope) following extreme lateral interbody fusion.
Several limitations are present in this study primarily related the retrospective nature of the query. First and foremost is the limited number of patients available for review, the lack of full length radiographs in a small group of patients, and the lack of more detailed patient reported outcomes for satisfaction and function in all patients. In addition, given the nature of the study design, patient selection might introduce a bias, and the matching criteria were limited to age, gender and diagnosis.
Although the case and control cohorts had no detected difference in their preoperative sagittal plane measurements, there were other significant differences between the two cohorts. Patients undergoing PSF alone had shorter fusion segments compared to patients treated with interbody fusions. This may reflect a change in practice and surgical techniques in the treatment of degenerative scoliosis. There are also limitations in the comparisons between the segmental lumbar lordosis at levels treated with the LIF technique versus ALIF technique. Since that only L4–L5 and L5–S1 were treated with ALIF techniques, and all lumbar levels excluding L5–S1 were treated with LIF techniques it is difficult to compare these techniques directly as the regional anatomy of the lower lumbar segments differs greatly from the upper lumbar segments. Since the majority of lumbar lordosis arises from L4–S1, it might be technically difficult to improve lumbar lordosis at these segments if they are already lordotic compared to higher lumbar levels. The lack of change in lumbar lordosis at the ALIF treated levels may be related to the L4–S1 segments being hyperlordotic prior to surgery. The interbody grafts at these levels results in a high fusion rate, but may not affect the focal geometry of these segments.
Conclusion
We found improved restoration of lumbar lordosis in patients undergoing LIF with or without ALIF compared to PSF alone. Further, we noted improved postoperative segmental lumbar lordosis in levels treated with LIF technique compared to ALIF technique. Although our study did not collect detailed patient–reported outcomes, there is growing evidence that restoration of sagittal plane alignment contributes to a successful long–term outcome. LIF may be one tool in the armamentarium of the surgeon in tackling spinal deformity although the technique and its indications are still evolving.
Acknowledgments
The device(s)/drug(s) is/are FDA-approved or approved by corresponding national agency for this indication.
CTSA Grant Number UL1 TR000135 from the National Center for Advancing Translational Sciences (NCATS), a component of the National Institutes of Health (NIH), funds were received to support this work. The contents of this work are solely the responsibility of the authors and do not necessarily represent the official view of NIH.
Relevant financial activities outside the submitted work: grant, board membership, patents, royalties, grants/grants pending, and fees for participation in review activities.
References
- 1.Kotwal S, Pumberger M, Hughes A, et al. Degenerative scoliosis: a review. HSS J. 2011;7:257–64. doi: 10.1007/s11420-011-9204-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sasso RC, Best NM, Mummaneni PV, et al. Analysis of operative complications in a series of 471 anterior lumbar interbody fusion procedures. Spine (Phila Pa 1976) 2005;30:670–4. doi: 10.1097/01.brs.0000155423.18218.75. [DOI] [PubMed] [Google Scholar]
- 3.Crandall DG, Revella J. Transforaminal lumbar interbody fusion versus anterior lumbar interbody fusion as an adjunct to posterior instrumented correction of degenerative lumbar scoliosis: three year clinical and radiographic outcomes. Spine (Phila Pa 1976) 2009;34:2126–33. doi: 10.1097/BRS.0b013e3181b612db. [DOI] [PubMed] [Google Scholar]
- 4.Hsieh PC, Koski TR, O’Shaughnessy BA, et al. Anterior lumbar interbody fusion in comparison with transforaminal lumbar interbody fusion: implications for the restoration of foraminal height, local disc angle, lumbar lordosis, and sagittal balance. J Neurosurg Spine. 2007;7:379–86. doi: 10.3171/SPI-07/10/379. [DOI] [PubMed] [Google Scholar]
- 5.Pavlov PW, Meijers H, van Limbeek J, et al. Good outcome and restoration of lordosis after anterior lumbar interbody fusion with additional posterior fixation. Spine (Phila Pa 1976) 2004;29:1893–9. doi: 10.1097/01.brs.0000137067.68630.70. discussion 900. [DOI] [PubMed] [Google Scholar]
- 6.Dorward IG, Lenke LG, Bridwell KH, et al. Transforaminal versus Anterior Lumbar Interbody Fusion in Long Deformity Constructs: a matched cohort analysis. Spine (Phila Pa 1976) 2013 doi: 10.1097/BRS.0b013e31828d6ca3. [DOI] [PubMed] [Google Scholar]
- 7.Knight RQ, Schwaegler P, Hanscom D, et al. Direct lateral lumbar interbody fusion for degenerative conditions: early complication profile. J Spinal Disord Tech. 2009;22:34–7. doi: 10.1097/BSD.0b013e3181679b8a. [DOI] [PubMed] [Google Scholar]
- 8.Kotwal S, Kawaguchi S, Lebl D, et al. Minimally Invasive Lateral Lumbar Interbody Fusion: Clinical and Radiographic Outcome at a Minimum 2-year Follow-up. J Spinal Disord Tech. 2012 doi: 10.1097/BSD.0b013e3182706ce7. [DOI] [PubMed] [Google Scholar]
- 9.Acosta FL, Liu J, Slimack N, et al. Changes in coronal and sagittal plane alignment following minimally invasive direct lateral interbody fusion for the treatment of degenerative lumbar disease in adults: a radiographic study. J Neurosurg Spine. 2011;15:92–6. doi: 10.3171/2011.3.SPINE10425. [DOI] [PubMed] [Google Scholar]
- 10.Sharma AK, Kepler CK, Girardi FP, et al. Lateral lumbar interbody fusion: clinical and radiographic outcomes at 1 year: a preliminary report. J Spinal Disord Tech. 2011;24:242–50. doi: 10.1097/BSD.0b013e3181ecf995. [DOI] [PubMed] [Google Scholar]
- 11.Kuhns CA, Bridwell KH, Lenke LG, et al. Thoracolumbar deformity arthrodesis stopping at L5: fate of the L5-S1 disc, minimum 5-year follow-up. Spine (Phila Pa 1976) 2007;32:2771–6. doi: 10.1097/BRS.0b013e31815a7ece. [DOI] [PubMed] [Google Scholar]
- 12.Uribe JS, Smith DA, Dakwar E, et al. Lordosis restoration after anterior longitudinal ligament release and placement of lateral hyperlordotic interbody cages during the minimally invasive lateral transpsoas approach: a radiographic study in cadavers. J Neurosurg Spine. 2012 doi: 10.3171/2012.8.SPINE111121. [DOI] [PubMed] [Google Scholar]
- 13.Blondel B, Schwab F, Ungar B, et al. Impact of magnitude and percentage of global sagittal plane correction on health-related quality of life at 2-years follow-up. Neurosurgery. 2012;71:341–8. doi: 10.1227/NEU.0b013e31825d20c0. discussion 8. [DOI] [PubMed] [Google Scholar]
- 14.Glassman SD, Berven S, Bridwell K, et al. Correlation of radiographic parameters and clinical symptoms in adult scoliosis. Spine (Phila Pa 1976) 2005;30:682–8. doi: 10.1097/01.brs.0000155425.04536.f7. [DOI] [PubMed] [Google Scholar]
- 15.Schwab FJ, Blondel B, Bess S, et al. Radiographical spinopelvic parameters and disability in the setting of adult spinal deformity: a prospective multicenter analysis. Spine (Phila Pa 1976) 2013;38:E803–12. doi: 10.1097/BRS.0b013e318292b7b9. [DOI] [PubMed] [Google Scholar]
- 16.Johnson RD, Valore A, Villaminar A, et al. Pelvic parameters of sagittal balance in extreme lateral interbody fusion for degenerative lumbar disc disease. J Clin Neurosci. 2013;20:576–81. doi: 10.1016/j.jocn.2012.05.032. [DOI] [PubMed] [Google Scholar]
- 17.Johnson RD, Valore A, Villaminar A, et al. Sagittal balance and pelvic parameters-a paradigm shift in spinal surgery. J Clin Neurosci. 2013;20:191–6. doi: 10.1016/j.jocn.2012.05.023. [DOI] [PubMed] [Google Scholar]
- 18.Boulay C, Tardieu C, Hecquet J, et al. Sagittal alignment of spine and pelvis regulated by pelvic incidence: standard values and prediction of lordosis. Eur Spine J. 2006;15:415–22. doi: 10.1007/s00586-005-0984-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schwab F, Lafage V, Patel A, et al. Sagittal plane considerations and the pelvis in the adult patient. Spine (Phila Pa 1976) 2009;34:1828–33. doi: 10.1097/BRS.0b013e3181a13c08. [DOI] [PubMed] [Google Scholar]
- 20.Legaye J, Duval-Beaupere G, Hecquet J, et al. Pelvic incidence: a fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur Spine J. 1998;7:99–103. doi: 10.1007/s005860050038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Smith JS, Shaffrey CI, Fu KM, et al. Clinical and radiographic evaluation of the adult spinal deformity patient. Neurosurg Clin N Am. 2013;24:143–56. doi: 10.1016/j.nec.2012.12.009. [DOI] [PubMed] [Google Scholar]
- 22.Schwab F, Patel A, Ungar B, et al. Adult spinal deformity-postoperative standing imbalance: how much can you tolerate?. An overview of key parameters in assessing alignment and planning corrective surgery. Spine (Phila Pa 1976) 2010;35:2224–31. doi: 10.1097/BRS.0b013e3181ee6bd4. [DOI] [PubMed] [Google Scholar]
- 23.Klineberg E, Schwab F, Smith JS, et al. Sagittal spinal pelvic alignment. Neurosurg Clin N Am. 2013;24:157–62. doi: 10.1016/j.nec.2012.12.003. [DOI] [PubMed] [Google Scholar]
- 24.O’Brien MF, Kuklo TR, Blanke KM, et al., editors. Spinal Deformity Study Group Radiographic Measurement Manual. Minneapolis, MN: Medtronic Sofamor Danek, Inc; 2005. [Google Scholar]
- 25.Schwab F, Lafage V, Boyce R, et al. Gravity line analysis in adult volunteers: age-related correlation with spinal parameters, pelvic parameters, and foot position. Spine (Phila Pa 1976) 2006;31:E959–67. doi: 10.1097/01.brs.0000248126.96737.0f. [DOI] [PubMed] [Google Scholar]
- 26.Ploumis A, Transfledt EE, Denis F. Degenerative lumbar scoliosis associated with spinal stenosis. Spine J. 2007;7:428–36. doi: 10.1016/j.spinee.2006.07.015. [DOI] [PubMed] [Google Scholar]
- 27.Schwab F, Dubey A, Gamez L, et al. Adult scoliosis: prevalence, SF-36, and nutritional parameters in an elderly volunteer population. Spine (Phila Pa 1976) 2005;30:1082–5. doi: 10.1097/01.brs.0000160842.43482.cd. [DOI] [PubMed] [Google Scholar]
- 28.Mundis GM, Akbarnia BA, Phillips FM. Adult deformity correction through minimally invasive lateral approach techniques. Spine (Phila Pa 1976) 2010;35:S312–21. doi: 10.1097/BRS.0b013e318202495f. [DOI] [PubMed] [Google Scholar]
- 29.Yson SC, Sembrano JN, Santos ER, et al. Does Prone Re-positioning Prior to Posterior Fixation Produce Greater Lordosis in Lateral Lumbar Interbody Fusion (LLIF)? J Spinal Disord Tech. 2012 doi: 10.1097/BSD.0b013e318268007b. [DOI] [PubMed] [Google Scholar]


