Abstract
Objective: The aim of this study was to evaluate the influence of cavity preparation and restorative materials containing fluorides in the prevention of secondary caries lesion development in situ. Methods: A total of 120 blocks obtained from human teeth were divided into two groups and standardized cavities were prepared using diamond burs (DB) or Er,Cr:YSGG-laser [20 Hz, 4.0W, 55% water, 65% air (LA)]. They were divided into three subgroups according to the restorative material (n=20): glass-ionomer cement (GI), resin modified glass-ionomer (RM) or composite resin (CR). Blocks were fixed in palatal intra-oral appliances worn in situ by 20 human volunteers, who dropped 20% sucrose solution eight times daily. After 21 days, blocks were removed and restorations were cross-sectioned to evaluate microhardness [Knoop hardness number (KHN)] underneath enamel surface from 30 to 200 μm. Factors “cavity preparation,” “restorative materials,” and “depth” were evaluated by three way ANOVA, followed by Tukey test (p<0.05). Results: The results showed lower microhardness in cavities prepared with DB than in cavities prepared with LA. At 30 μm, there were no statistical significant differences with regard to “cavity preparation” or “restorative materials” factors. In depth evaluation, the enamel microhardness progressively increased as a function of depth for the GI groups. In the groups prepared with LA at 60 μm/90 μm, there were no significant differences between GI and RM materials, whose microhardnesses were significantly higher than that of CR. Conclusions: Cavity preparation using Er,Cr:YSGG laser increases caries resistance of enamel walls, and reduce caries lesion depth development regardless of fluoride presence in the restorative material. CR showed higher caries lesion development than GI, and RM showed intermediate results.
Introduction
Fluoride in the oral cavity can interfere with the phenomenum of demineralization, and can enhance dental remineralization.1,2 Fluorides are available in water, toothpastes, mouthwash, and by topical application, in gels or varnishes. Fluorides may also be released from restorative materials as a preventive method.1–5 Among them, adhesives and composite resins (CR) seem to provide little or no cariostatic effect.3 On the other hand, conventional glass ionomer cements (GI) have shown the highest cariostatic potential, and glass ionomer/resin composite hybrid materials (RM) have shown an intermediate effect on caries prevention.3–5
Several in vitro studies have suggested the use of high-intensity lasers at low doses, such as erbium and CO2, as a tool in the prevention of dental caries.5–10 Some in vitro and in situ studies were able to demonstrate the potential of erbium lasers to increase enamel acid resistance.5–10 However, erbium lasers were introduced in dentistry for cavity preparation, as they are well absorbed by water and hydroxyl radical in the hydroxyapatite, and they can promote enamel removal with minimal anesthesia needed.5–14 Enamel removal occurs by ablation.11–16 Heat and water vaporization results in high internal pressures that lead to removal of enamel, dentin, and carious tissue in the form of microexplosions.11–16 Therefore, there is no bur contact and no thermal damage to pulp or periodontal tissues, when lasers are used with appropriated refrigeration, repetition rate, and pulse duration.7,11–16
Although conventional bur cavity preparation is a fast procedure, tooth ablation generates residual energy in subablative densities through the cavity walls. It is possible that this energy could produce an acid resistant zone in the cavity margins, which can reduce the susceptibility of secondary caries formation.5–17 However, few studies have shown an increase in enamel acid resistance around cavities prepared with erbium lasers and restored with CR, GI, or RM,5–8 and there are no studies showing that residual energy of Er,Cr:YSGG-laser used on cavity preparation may improve the cavity walls and external surface acid resistance. Based on these properties, cavity preparation with erbium lasers could be indicated for high-caries- risk patients, in association with restorative materials with fluoride release, to prevent the development of secondary carious lesions.
Therefore, the aim of the present study was to evaluate the influence of cavity preparation with Er,Cr:YSGG laser and restorative materials on secondary caries prevention by an in situ caries model similar to a high-caries-risk patient, by cross-sectional microhardness test. The null hypothesis of the present study was that there is no difference in the enamel microhardness around cavities prepared with diamond bur (DB) or Er,Cr:YSGG laser (LA), regardless of restorative materials.
Materials and Methods
The research protocol was approved by the Research Ethics Committee of Guarulhos University in accordance with the resolution CNS# 18/2009 of the Brazilian Health Department.
Experimental design
The experimental units consisted of 120 dental blocks (n=20 per group) obtained from 58 unerupted human third molars. Sample power was based on a mean of 350 Knoop hardness number (KHN) for a noncarious enamel with standard deviation±100, considering 200 KHN demineralized enamel. The factors under study were “cavity preparation method” on two levels: DB and LA; “restorative material” on three levels (Table 1), and “depth,” on seven levels in a factorial design 2×3×7. The response variable was microhardness KHN.
Table 1.
Distribution of Experimental Groups
| Group | Method of cavity preparation | Restorative material |
|---|---|---|
| DBGI | Diamond bur | Glass ionomer cement |
| DBRM | Diamond bur | Resin modified glass ionomer |
| DBCR | Diamond bur | Composite resin |
| LAGI | Er,Cr:YSGG-laser | Glass ionomer cement |
| LARM | Er,Cr:YSGG-laser | Resin modified glass ionomer |
| LACR | Er,Cr:YSGG-laser | Resin composite |
Preparation of dental blocks
Following extractions, teeth were stored in a 0.1% thymol solution (pH 7.0) for no longer than 30 days. Soft tissues were removed using periodontal curettes (HU-FRIEDY do Brasil, Rio de Janeiro-Brazil) and cleaned using a slurry of pumice. Roots were removed, and the crowns were longitudinally and transversally sectioned to obtain 120 dental blocks measuring 4×4×3 mm using double-faced diamond discs (#7020, KG Sorensen, Sao Paulo, Brazil).
Cavity preparation and restoration
Standardized circular cavities were prepared in the enamel blocks. Sixty enamel blocks were prepared with DB (No. 2292) at high speed under a constant water spray coolant, with ∼1.6 mm diameter and 1.6 mm depth (KG Sorensen, Barueri, SP, Brazil). The other blocks were prepared with an Er,Cr:YSGG laser (Waterlase™, Biolase Technology Inc., Irvine, CA; wavelength of 2780 nm) with the cavity preparation handpiece with a sapphire tip (G4 - Biolase Technology Inc., Irvine, CA).
The irradiation was performed in the Special Laboratory of Lasers in Dentistry (LELO - Department of Restorative Dentistry, School of Dentistry, University of São Paulo) with a repetition rate set at 20 Hz, using a diode laser as a guide in the focused mode with 2 mm distance from the surface. The irradiation was performed under constant water cooling (55%) and air (65%) with an average power of 4.0 W.
After the cavity preparations, the blocks were randomized among the restorative material subgroups (Table 1) and the cavities were restored in one increment, according to the manufacturer's instructions.
Cavities filled with CR were acid conditioned for 15 sec (3M Scotch Bond etchant, 3M ESPE, St. Paul, MN), rinsed for 10 sec and air dried. Two coats of an adhesive system (3M Single Bond, 3M ESPE, St. Paul, MN) were applied, air dried for 5 sec and light activated for 10 sec by an light unit (Optilux 501, Demetron/Kerr, Danbury, CT). The power density was measured by placing the light tip at the radiometer of the light unit. The light curing unit had a light tip diameter of 11 mm with an irradiance of 700 mW/cm2. The composite resin (Z350, 3M ESPE, St. Paul, MN) was inserted and light activated for 20 sec.18
Cavities filled with GI were conditioned (Ketac conditioner, 3M ESPE, Seefeld, Germany) for 10 sec, rinsed, and dried for 10 sec. GI (Ketac-Fil, 3M ESPE, Seefeld, Germany) was prepared within 20–25 sec, inserted in the cavity with a Centrix injector, protected with a mylar strip (Dentart, Polidental, São Paulo, Brazil; dimension 10×120×0.05 mm) for 5 min, coated with a fluid resin (Vitremer Finish Gloss, 3M ESPE, St. Paul, MN) and light activated for 20 sec.
In cavities filled with RM, the Primer (Vitremer Primer, 3M ESPE, St. Paul, MN) was applied for 30 sec, dried for 5 sec, and light activated for 20 sec, and RC (Vitremer, 3M ESPE, St. Paul, MN) was prepared for 45 sec, inserted in the cavity with a Centrix injector, light activated for 40 sec, coated with a fluid resin (Vitremer Finish Gloss, 3M ESPE, St. Paul, MN), and light activated for 20 sec.
All restored blocks were stored in 100% humidity for 24 h and then polished using sequential abrasive disks (Sof-lex, 3M ESPE, St. Paul, MN) for 15 sec with each disk.
Cariogenic challenge in situ
Twenty volunteers signed a informec consent form to participate in the in situ study. These volunteers had good oral health, salivary flow>0.8 mL/min, and all permanent teeth present in the oral cavity without active caries; wore no fixed prosthesis or removable orthodontic appliance; had no gingival hyperplasia, no current periodontal sites with bleeding on probing and/or marginal bleeding, and no current periodontal sites with concomitant probing depth; and had clinical attachment levels>3 mm and no history of periodontitis. Two weeks before the in situ stage, volunteers were examined, impressions were taken with an alginate material (Jeltrate-Dentsply Industria e Comercio Ltda., Rio de Janeiro, RJ, Brazil) and volunteers then received hygiene instructions (Bass Technique) and prophylaxis with stone pumice and water. A week before the beginning of treatment, to standardize the oral conditions, the volunteers received a standard nonfluoride dentifrice (Sanikids, SANiFill, Curitiba, PR, Brazil), and a toothbrush (Oral-B Indicator 35 Plus, Oral-B Gillette Brazil, Manaus, Brazil) for use during the study. Intra-oral devices (removable appliances) were made, and the enamel blocks were fixed for the induction of in situ caries lesions.
Six enamel blocks (one of each group) were randomly attached with sticky wax to individual windows created in the palatal area of the removable devices, close to the pre-molars. Over the windows, a plastic screen was fixed, leaving a 1 mm space between the enamel-restored fragment and the screen, to allow cariogenic plaque growth.
Intra-oral appliances were installed and adjusted, and were used by volunteers for 21 days. To induce the cariogenic challenge, the devices were removed from the oral cavity by the volunteer and inserted in a box, and a 20% sucrose solution was dropped (1 drop) on each enamel-restored block eight times a day. The intra-oral appliance was covered with moist gauze and kept in the box for 5 min. Afterwards, the device was reinserted in the mouth, and only the surface in contact with palate could be cleaned. The methodology employed in this study was described by Benelli et al., and is similar to a condition of caries development in a high-caries-risk patient.19 Additionally, this protocol is very useful to predict the cariostatic potential of restorative materials and laser prevention treatment.7–20
Cross-sectional subsurface microhardness test
To evaluate the cross-sectional subsurface microhardness, the enamel blocks were sectioned at the center of the restorations and the subsurface was flattened in an electric rotary polisher machine (Teclago PL, RB LAB and Technical Ltda, Sao Paulo, SP, Brazil) at 300 rpm, with SiC paper (grits 400, 600, and 1200; Carborundum Abrasives Inc., Vinhedo, SP, Brazil) under water cooling. The final polishing was performed with polishing felt discs (Top, Supra and Ram; Arotec Ind. e Com, Cotia, SP, Brazil) and diamond pastes (6, 3, 1, and 0.5 μm; Arotec Ind. e Com, Cotia, Sao Paulo, Brazil) and refrigerated with mineral oil.3
Enamel demineralization was determined using a Knoop indenter with a load of 25 g per 5 sec. Two measurements were obtained from each block, on left and right enamel sides, located at 100 μm from the cavity walls and 30, 60, 90, 120, 150, and 200 μm below the enamel surface (Fig. 1). The average of these two measures at the same depth was considered as the microhardness value at each respective depth.
FIG. 1.
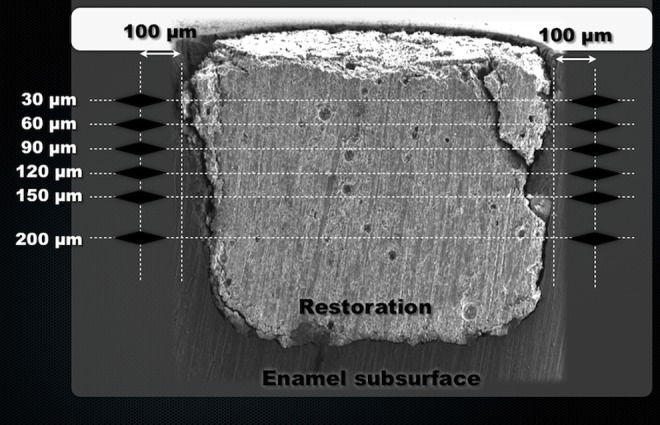
Scheme used for evaluation of cross-sectional subsurface microhardness. Cavity prepared with diamond bur and restored with glass-isonomer cement (GI).
Statistical analysis
Data presented normal distribution and were submitted to three way ANOVA considering the factorial 2×3×7 model to observe the factors and their interactions (α=0.05). Tukey post-hoc test was used to show statistical significant differences among groups (SANEST - EPAMIG, MG, Brazil).
Results
Mean microhardness values and standard deviations per depth and restorative material in DB and LA cavity preparations are presented in Table 2. There were statistically significant differences for all factors: triple interaction of “cavity preparation method” by “restorative material” by “depth” (p=0.00001); double interactions “cavity preparation method” by “depth” (p=0.00001); “cavity preparation method” by “restorative material” (p=0.00001); “restorative material” by “depth” (p=0.00001); and for main factors “cavity preparation method” (p=0.00001), “restorative material” (p=0.00001), and “depth” (p=0.00001). Table 2 shows the comparisons of subsurface microhardness at each depth individually.
Table 2.
Means (Standard Deviation) of Subsurface Microhardness (KHN) for Factors “Restorative Material” and “Depth” in DB Cavity Preparation
| DB | LA | |||||
|---|---|---|---|---|---|---|
| DBGI | DBRM | DBRC | LAGI | LARM | LARC | |
| 30 μm | 45.7 (22.6)Aa | 26.7 (9.3)Aa | 18.7 (13.0)Aa | 206.5 (56.7)Aa* | 91.2 (27.1)Ab* | 62.7 (18.9)Ab* |
| 60 μm | 84.2 (37.2)Ba | 46.8 (6.6)ABb | 23.3 (16.0)Ab | 294.0 (71.8) Ba* | 265.7 (69.7)Ba* | 73.4 (18.0)ABb* |
| 90 μm | 123.1 (40.0)Ca | 64.7 (10.9)BCb | 38.0 (14.0)ABb | 356.3 (57.1)Ca* | 330.3 (76.2)Ca* | 106.9 (36.1)Bcb* |
| 120 μm | 164.8 (49.4)Da | 78.8 (11.8)BCDb | 44.7 (15.1)ABb | 425.8 (56.2)Da* | 378.1 (47.3)Db* | 130.1 (36.7)Cc* |
| 150 μm | 226.8 (65.2)Ea | 92.1 (6.7)CDb | 64.5 (21.4)BCb | 468.7 (65.8)Ea* | 402.8 (34.7)DEb* | 137.9 (36.5)Cc* |
| 200 μm | 313.5 (78.7)Fa | 107.6 (13.2)Db | 84.5 (21.4)Cb | 610.5 (112.0)Fa* | 421.4 (48.0)Eb* | 143.9 (34.1)Cc* |
Statistical significant differences are shown by different letters: lower case for factor “restorative material,” upper case to factor “depth.” Asterisks compare factor “cavity preparation method,” by Tukey test (p=0.00001).
KHN, Knoop hardness number; DB, diamond bur; LA, Er,Cr:YSGG-laser; GI, glass-ionomer cement; RM, resin modified glass-ionomer; RC, composite resin.
All subsurface enamel around cavities prepared with diamond burs showed lower microhardness than in enamel around cavities prepared with LA.
Around cavities prepared with DB, at 30 μm there were no statistical significant differences on microhardness for the factor “restorative material.” Below, at 60 μm there were no statistically significant differences between the microhardnesses around RM and RC, which were significantly lower than that of GI.
In the groups prepared with LA at 30 μm, there were no significant differences among the enamel microhardnesses around cavities. At 60 and 90 μm, there were no significant differences between enamel microhardnesses around GI and RM, whose microhardnesses were significantly higher than that of RC. From 120 to 200 μm, the enamel around cavities restored with GI showed the highest microhardness values, the enamel around cavities restored with RC showed the lowest microhardness values, and there were intermediate results around RM.
In the evaluation of depth, enamel microhardness progressively increased as a function of depth. However, this increase was more pronounced around cavities restored with GI for both types of cavity preparations.
In cavities prepared with DB and restored with RM, there were no statistically significant differences between enamel microhardnesses at 30 and 60 μm; significant differences were observed between 30 μm and depths >90 μm, but there were no statistically significant differences from 60 to 120 μm, no statistically significant differences from 90 to 150 μm, and no statistically significant differences from 120 to 200 μm.
In cavities prepared with DB and restored with RC, there were no statistically significant differences between enamel microhardnesses from 30 to 120 μm; statistically significant differences were observed among depths of 30 and 60 μm to depths of 150 and 200 μm, but there were no statistically significant differences from 120 to 200 μm.
In cavities prepared with LA and restored with RM, there were statistically significant differences between enamel microhardness at 30 and 60 μm, 60 and 90 μm, and among depths ≥90 μm. There were no statistically significant differences between 120 and 150 μm, in which microhardnesses were statistically significant <200 μm.
In cavities prepared with LA and restored with RC, there were no statistically significant differences between enamel microhardnesses at 30 and 60 μm, 60 and 90 μm, and among depths ≥90 μm. There were statistically significant differences between depths of 30 and ≥90 μm; and there were differences between depths of 60 and ≥120 μm.
Discussion
The mechanism of enamel acid resistance improved by lasers is not yet fully clear. Enamel chemical alteration occurs gradually as temperature increases from 100° to 650°C. This temperatures decreases carbonate component and forms pyrophosphate, reducing the solubility rate. At 400°C, the formation of large crystals of beta-tricalcium phosphate (ß-CP) begins.21–23 At 800°–1100°C, enamel melting and a dramatically reduction on carbonate occurs.21–23 However, at temperatures>1100°C, ß-TCP is converted in alpha-tricalcium phosphate (α-TCP). Both ß-TCP and α-TCP are potentially soluble in acid environments.22,23
Thus low laser energy densities from Er,Cr:YSGG laser may be transformed from light into heat at the enamel surface, and may increase the temperature in the immediate subsurface, to incite only crystal transformation into a less soluble phase, and to promote the inhibition of subsurface lesion formation.23–26
Studies have shown that the energy necessary to reach enamel acid resistance using Er,Cr:YSGG-laser is ∼8–65 J/cm2.25–27 In the present study, the dental enamel was LA-irradiated with 20 Hz, 4.0 W, 55% water, 65% air, which is an ablative dose, and which promoted enamel removal for cavity preparation. However, residual energy below the ablation threshold was expected in the cavity walls, which had a temperature gradient that decreased toward the dentin junction.26 Surface heat may vary from 25% to 70% of subablative irradiation heat.28
Supported by this theory, it can be assumed that in the present study the enamel at cavity walls prepared with LA was changed by the residual heat,24 and turned into a more acid-resistant enamel, being able to reduce secondary caries development around all restorative materials tested. Therefore, the null hypothesis was rejected.
Similar results were observed by Perito et al., who found lower in vitro development of carious lesions around cavities prepared with Er:YAG (47 J/cm2, 6 Hz) by superficial Knoop microhardness test,5 and with polarized light microscopic results from Chimello et al. after cavities prepared with Er:YAG (62.5–87.5 J/cm2, 2–4 Hz) and caries challenge in situ.29
However, with laser ablation, the amount of tissue removed and the impact on adjacent tissues depends upon the tissue composition and on the parameter settings, such as irradiation time, pulse energy, pulse repetition rate, pulse duration, emission mode, tissue water cooling, and amount of water and air rate, as well as the focus and the target surface. These changes of the settings parameters may result in different interactions. Hadley et al.13 compared the in vivo performance of composite restorations in 66 cavities prepared with LA (4– W), with another 66 cavities prepared with DB in a split-mouth study design, and found that after 6 months, all restorations were present and without caries lesion.13
A synergistic effect of LA and restorations with fluoride release, which resulted in less caries depth in conventional glass ionomer (LAGI) and in the resin modified glass ionomer (LARM) was observed. In the hybrid material (LARM), the laser synergistic effect was more evident, considering that there was significantly less caries development than in the group that was laser prepared and restored with composite resin (LARC), compared with the cavities prepared with diamonds burs, which showed no differences between the hybrid material (DBRM), and the composite resin (DBRC). Also, above the 90 μm depth in LAGI and LARM, the enamel microhardness values were similar to those of sound enamel, and it is possible that caries lesion depth was ∼90 μm. On the other hand, LARC showed microhardness values lower than those of sound enamel at all depths, and it is possible that caries lesion were deeper than 200 μm.
As observed, LA settings used in the present study were able to enhance enamel acid resistance in an experimental in situ study model, but some concerns about the clinical safety, and longevity of adhesive restorations, and patient factors, such as diet, frequency of tooth brushing and flossing, and salivary rate must still be evaluated in a treatment plan.
The use of ablative energy densities (17.6–35.6 J/cm2) in the enamel treatment with LA did not affect the mean percentage weights of calcium, potassium, magnesium, sodium, and phosphate, or the calcium/phosphate ratio. However, the ablation process creates craters and irregularities, with exposition of enamel prisms that increases with increasing energy densities on the enamel surface.30 These adverse effects associated with the increase in enamel acid resistance may reduce the bond strength of adhesive systems to enamel.
Although some studies have shown similarity between lased surfaces and acid-etched ones, with absence of smear layer and increase in roughness, and have suggested the use of LA as a substitute for phosphoric acid for enamel and dentin etching before adhesive hybridization, it is still controversial. Enamel morphology may not be favorable to enamel adhesion, and the surface layer may lose the attachment to the underlying unaltered substrate, leading to poor bonding strength to restorative materials.
Baygin et al. recently showed that laser irradiation with Er,Cr:YSGG (2 W, 20 Hz or 2 W, 40 Hz) did not eliminate the need for acid etching prior to enamel adhesion, and negatively influenced marginal sealing, resulting in higher marginal leakage.31Also, cavities prepared with Er:YAG-laser showed higher microleakage than those prepared with DB.32
Therefore, the complete adhesive system technique after laser cavity preparation is still recommended, and may improve bond strength. Irrespective of the cavity preparation technique, DB or LA (5.25 W, 20 Hz, 140 μs pulse duration), an etch-and-rinse adhesive and a one-step self-etch adhesive applied strictly following the manufacturers' instructions showed similar microleakage in an in vitro study.33,34 Also, erbium laser treatment does not exclude the need for etching previous to GI or RM restoration.
This study compared the cariostatic potential of a conventional GI restorative material to an RMGI and a CR system, used in conventional DB cavity preparation, and observed no differences in the caries lesion at 30 μm of depth, regardless of the restorative material (DBGI-DBRM-DBRC). It showed that caries challenge at 30 μm overpassed the threshold of the cariogenic effect of GI. The caries demineralization was observed in the other evaluated depths, but was lower in the cavities restored with the conventional glass ionomer (DBGI) than in the cavities restored with the resin modified glass ionomer (DBRM) and composite resin (DBRC), corroborating the superior cariostatic effect of GI according to previous studies.3,5
Over the acid challenge in clinical conditions, the GI-based materials could release greater amounts of fluoride in dental plaque. The continuous presence of fluoride released by these restorative materials is an important feature in inhibiting enamel demineralization, and facilitating the recovery of minerals, enhancing remineralization of dental enamel. Possibly, the occurrence of these phenomena resulted in smaller development of caries lesions around the cavities restored with conventional GI in the present study. Also, the lesion caries depths around the conventional GI (DBGI) restorations were smaller than for the other groups in all depths analyzed.
Further development of artificial carious lesions in this study was observed in the group prepared with DB and restored with CR, which was expected, because CR and the adhesive system used do not contain fluoride in their composition, which is in agreement with other studies.3–5
Although in vitro studies have reported that hybrids of GI and CR present a cariostatic effect on a smaller scale than the conventional GIs, in this high-caries-risk in situ study model, the cariostatic effect on subsurface demineralization was not observed in the resin-modified GI (DBRM), which did not differ from CR (DBRC). Furthermore, the resin-modified glass ionomer (DBRM) and composite resin (DBRC) at 200 μm showed microhardness values lower than those of sound enamel, and it can be supposed that caries lesions were deeper than 200 μm.20 Therefore, considering only high-caries-risk patients, GI may be the restorative material of choice. But some factors, such as cavity configuration, location, and aesthetics must be considered, because GIs are a sensible technique and present lower mechanical properties than resin materials.3
As observed in this study, the use of LA in cavity preparation can change adjacent enamel, improving acid resistance, and can be used as an alternative in the prophylaxis and treatment of patients with high risk for dental caries in association with fluoride release restorative materials.
However, this is an in situ study, and the enamel was subjected to a high-caries challenge with sucrose exposition and no cariogenic biofilm disorganization. Caries lesion development was accelerated, and clinically, this process is slower. Also, the most rational way to treat a patient at high risk is by changing the caries disease modulation factors, and the use of laser and cariostatic materials should be used only for preventing or slowing down lesion progress by increasing enamel acid resistance.
Conclusions
It can be concluded that the use of LA is able to clinically reduce enamel demineralization depth around direct restorative material regardless of fluoride release, and may be indicated for treatment of high-caries-risk patients.
Acknowledgments
This study was supported by Sao Paulo Research Foundation, grants FAPESP#2008/08974-6 and CEPID/CEPOF# 98/14270-8.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Elderton RJ. Preventive (evidence-based) approach to quality general dental care. Med Princ Pract 2003;1:12–21 [DOI] [PubMed] [Google Scholar]
- 2.Lima YB, Cury JA. Seasonal variation of fluoride intake by children in a subtropical region. Caries Res 2003;37:335–338 [DOI] [PubMed] [Google Scholar]
- 3.Rodrigues JA, Marchi GM, Serra MC, Hara AT. Visual evaluation of in vitro cariostatic effect of restorative materials associated with dentifrices. Braz Dent J 2005;16:112–118 [DOI] [PubMed] [Google Scholar]
- 4.Tantbirojn D, Douglas WH, Versluis A. Inhibitive effect of a resin-modified glass ionomer cement on remote enamel artificial caries. Caries Res 1997;4:275–280 [DOI] [PubMed] [Google Scholar]
- 5.Perito MA, Jorge AC, de Freitas PM, Cassoni A, Rodrigues JA. Cavity preparation and influence of restorative materials on the prevention of secondary caries. Photomed Laser Surg 2009;5:729–734 [DOI] [PubMed] [Google Scholar]
- 6.Fried D, Featherstone JD, Le CQ, Fan K. Dissolution studies of bovine dental enamel surfaces modified by high-speed scanning ablation with a lambda=9.3-microm TEA CO(2) laser. Lasers Surg Med 2006;9:837–845 [DOI] [PubMed] [Google Scholar]
- 7.Apel C, Birker L, Meister J, Weiss C, Gutknecht N. The caries-preventive potential of subablative Er:YAG and Er:YSGG laser radiation in an intraoral model: a pilot study. Photomed Laser Surg 2004;4:312–317 [DOI] [PubMed] [Google Scholar]
- 8.Chimello DT, Serra MC, Rodrigues–Júnior AL, Pécora JD, Corona AS. Influence of Er:YAG laser on microhardness of enamel adjacent to restorations submitted to cariogenic challenge in situ. Photomed Laser Surg 2008;4:379–385 [DOI] [PubMed] [Google Scholar]
- 9.Cecchini RC, Zezell DM, de Oliveira E, de Freitas PM, Eduardo CP. Effect of Er:YAG laser on enamel acid resistance: morphological and atomic spectrometry analysis. Lasers Surg Med 2005;5:366–372 [DOI] [PubMed] [Google Scholar]
- 10.Bevilácqua FM, Zezell DM, Magnani R, da Ana PA, Eduardo CP. Fluoride uptake and acid resistance of enamel irradiated with Er:YAG laser. Lasers Med Sci 2008;2:141–147 [DOI] [PubMed] [Google Scholar]
- 11.Fried D, Zuerlein M, Featherstone JDB, Seka W, McCormack SM. IR laser ablation of dental enamel: mechanistic dependence on the primary absorber. Appl Surf Sci 1997;127–129:852–856 [Google Scholar]
- 12.Aoki A, Sasaki KM, Watanabe H, Ishikawa I. Lasers in nonsurgical periodontal therapy. Periodontol 2000 2004;36:59–97 [DOI] [PubMed] [Google Scholar]
- 13.Hadley J, Young DA, Eversole LR, Gornbein JA. A laser-powered hydrokinetic system for caries removal and cavity preparation. J Am Dent Assoc 2000;6:777–785 [DOI] [PubMed] [Google Scholar]
- 14.Soares LE, Brugnera Junior A, Zanin FA, Pacheco MT, Martin AA. Effects of treatment for manipulation of teeth and Er:YAG laser irradiation on dentin: a Raman spectroscopy analysis. Photomed Laser Surg 2007;1:50–57 [DOI] [PubMed] [Google Scholar]
- 15.Keller U, Hibst R. Effects of Er:YAG laser in caries treatment: a clinical pilot study. Lasers Surg Med 1997;20:32–38 [DOI] [PubMed] [Google Scholar]
- 16.Liu Y, Hsu CY. Laser-induced compositional changes on enamel: a FT-Raman study. J Dent 2007;35:226–230 [DOI] [PubMed] [Google Scholar]
- 17.Apel C, Schäfer C, Gutknecht N. Demineralization of Er:YAG and Er,Cr:YSGG laser-prepared enamel cavities in vitro. Caries Res 2003;37:34–37 [DOI] [PubMed] [Google Scholar]
- 18.Cassoni A, Ferla JD, Albino LG, Youssef MN, Shibli JA, Rodrigues JA. Argon ion laser and halogen lamp activation of a dark and light resin composite: microhardness after long-term storage. Lasers Med Sci 2010;6:829–834 [DOI] [PubMed] [Google Scholar]
- 19.Benelli EM, Serra MC, Rodrigues AL, Jr, Cury JA. In situ anticariogenic potential of glass ionomer cement. Caries Res 1993;27:280–421 [DOI] [PubMed] [Google Scholar]
- 20.Featherstone JD, ten Cate JM, Shariati M, Arends J. Comparison of artificial caries like-lesion by quantitative microradiography and microhardness profiles. Caries Res 1983;17:385–391 [DOI] [PubMed] [Google Scholar]
- 21.Hsu J, Fox JL, Higuchi WI, Otsuka M, Yu D, Powell GL. Heat-treatment-induced reduction in the apparent solubility of human dental enamel. J Dent Res 1994;73:1848–1853 [DOI] [PubMed] [Google Scholar]
- 22.Featherstone JD, Nelson DG. Laser effects on dental hard tissues. Adv Dent Res 1987;1:21–26 [DOI] [PubMed] [Google Scholar]
- 23.Palamara J, Phakey PP, Rachinger WA, Orams HJ. The ultrastructure of human dental enamel heat-treated in the temperature range 200 degrees C to 600 degrees C. J Dent Res 1987;66:1742–1747 [DOI] [PubMed] [Google Scholar]
- 24.Perhavec T, Diaci J. Comparison of heat deposition of Er:YAG and Er,Cr:YSGG lasers in hard dental tissues. J Laser Health Acad 2009;2:1–6 [Google Scholar]
- 25.Geraldo–Martins VR, Lepri CP, Palma–Dibb RG. Influence of Er,Cr:YSGG laser irradiation on enamel caries prevention. Lasers Med Sci 2013;28:33–39 [DOI] [PubMed] [Google Scholar]
- 26.Fowler BO, Kuroda S. Changes in heated and in laser-irradiated human tooth enamel and their probable effects on solubility. Calcif Tissue Int 1986;38:197–208 [DOI] [PubMed] [Google Scholar]
- 27.de Freitas PM, Rapozo–Hilo M, Eduardo CP, Featherstone JD. In vitro evaluation of erbium, chromium:yttrium-scandiumgallium- garnet laser–treated enamel demineralization. Lasers Med Sci 2010;25:165–170 [DOI] [PubMed] [Google Scholar]
- 28.Fried D, Ragadio J, Champion A. Residual heat deposition in dental enamel during IR laser ablation at 2.79, 2.94, 9.6, and 10.6 microm. Lasers Surg Med 2001;29:221–229 [DOI] [PubMed] [Google Scholar]
- 29.Chimello DT, Serra MC, Rodrigues–Júnior AL, Pécora JD, Corona ASM. Influence of cavity preparation with Er:YAG laser on enamel adjacent to restorations submitted to cariogenic challenge in situ: a polarized light microscopic analysis. Lasers Surg Med 2008;40:634–643 [DOI] [PubMed] [Google Scholar]
- 30.Secilmis A, Usumez A, Usumez S, Berk G. Evaluation of mineral content of enamel prepared by erbium, chromium:yttrium-scandium-gallium-garnet laser. Lasers Med Sci 2010;25:467–472 [DOI] [PubMed] [Google Scholar]
- 31.Baygin O, Korkmaz FM, Tüzüner T, Tanriver M. The effect of different enamel surface treatments on the microleakage of fissure sealants. Lasers Med Sci 2012;27:153–160 [DOI] [PubMed] [Google Scholar]
- 32.Yaman BC, Guray BE, Dorter C, Gomeç Y, Yazıcıoglu O, Erdilek D. Effect of the erbium:yttrium-aluminum-garnet laser or diamond bur cavity preparation on the marginal microleakage of class V cavities restored with different adhesives and composite systems. Lasers Med Sci 2012;27:785–794 [DOI] [PubMed] [Google Scholar]
- 33.Yazici AR, Baseren M, Gorucu J. Clinical comparison of bur- and laser-prepared minimally invasive occlusal resin composite restorations: two-year follow-up. Oper Dent 2010;35:500–507 [DOI] [PubMed] [Google Scholar]
- 34.Quo BC, Drummond JL, Koerber A, Fadavi S, Punwani I. Glass ionomer microleakage from preparations by an Er/YAG laser or a high-speed handpiece. J Dent 2002;30:141–146 [DOI] [PubMed] [Google Scholar]


