Abstract
Objective
To determine the risk factors for Deliberate Self-Harm (DSH) in patients presenting to the Emergency Departments (EDs) of three tertiary care hospitals of Karachi, Pakistan.
Study Design
Multicentre matched case control study.
Place and Duration of Study
EDs of the Aga Khan University Hospital, Karachi, Civil Hospital, Karachi and Jinnah Postgraduate Medical Centre, Karachi, from March 2011 to February 2012.
Methodology
A total of 201 cases and 201 matched controls were taken from three hospitals situated in Karachi. All patients of 16 years and above presenting to the EDs of the hospitals with DSH attempt were invited to participate in the study. Controls were ED patients with complaints other than DSH. A control was matched with case for hospital, gender and age. Two questionnaires were used to collect information on the risk factors of DSH. Conditional Logistic Regression (CLR) was used to assess the association of various risk factors with DSH.
Results
Risk factors of DSH in Karachi included current history of mental disorder (OR = 4.53, 95% CI = 1.59 – 12.92), not sharing problems with someone (OR = 4.67, 95% CI = 2.4 – 9.0), living in rented houses (OR = 2.58, 95% CI = 1.37 – 4.84), Pathan ethnicity (OR = 5.05, 95% CI = 1.01–25.38) followed by others (OR = 3.88, 95% CI = 0.77 – 19.69) and Urdu speaking (OR = 2.71, 95% CI = 0.59 – 12.45). Absence of physical illness in the past month had an inverse association with DSH (OR = 0.17, 95% CI = 0.07 – 0.37).
Conclusion
Mental illnesses, low socio-economic status and loneliness were the risk factors of DSH patients presenting to the three EDs of Karachi. Physical illness in the last month was protective against DSH in these patients. Psychiatric evaluation of DSH patients in the ED is important for early diagnosis and management of mental disorders.
Keywords: Risk factors, Deliberate self-harm, Emergency departments
INTRODUCTION
Deliberate Self Harm (DSH) is defined as ‘intentional self-injury or self-poisoning, irrespective of type of motivation or degree of suicidal intent’.1 The estimated number of DSH attempts per year in Pakistan is more than 100,000.2 Both DSH and suicide are considered criminal offences, punishable with a jail term and/or fine.3 Religious and social factors also influence the diagnosis and registering of DSH and suicide in Pakistan since Islam strictly forbids the act of suicide.4 Although, in reality, prosecution is rare, harassment of the DSH victim is not uncommon. People avoid going to public hospitals (which are designated as ‘Medico-Legal Centers (MLCs)’ and where under law all suspected cases of DSH should be taken) and instead seek treatment from private hospitals, which neither register these cases as DSH nor report them to the police.5 Families do not disclose the true nature of a DSH or suicidal act, for fear of harassment by police and/or social stigma instead claiming it to be an accident.6
A review of published literature on DSH attempts and suicides from Pakistan showed that psychiatric illness, family discord, relationship problems, marital problems, psychiatric illness (depression), unemployment and female gender are the risk factors for DSH.7 However, these studies were mostly retrospective, with small sample size and from a single centre. There was also no control group in these studies. The problem needs immediate attention as there is evidence that incidence of DSH and suicides have increased in recent years in Pakistan.8 Previous history of DSH attempt is a strong predictor of future suicide.9 As DSH patients are at high risk for reattempting with a fatal outcome, proper counselling of such patients can prevent both reattempt as well as possible suicide. This can be effectively carried out in the ED, which serves as the first point of contact for DSH patients and they are uniquely receptive to education about suicidal behavior and risk reduction interventions.5 This is particularly so in developing countries like Pakistan, where primary healthcare services are poorly organized and mental healthcare facilities and professionals are severely limited.10 It was against this background that the present study was designed.
The objective of the study was to determine the risk factors for DSH in patients presenting to the EDs of three tertiary care hospitals of Karachi, Pakistan.
METHODOLOGY
This pair-matched case-control study was conducted between March 2011 to February 2012 in the EDs of The Aga Khan University Hospital (AKUH), Civil Hospital, Karachi (CHK) and Jinnah Postgraduate Medical Centre (JPMC).
One hundred cases and 100 age and gender matched controls were taken from AKUH while a total of 101 cases and 101 matched controls were taken from both the CHK (50 cases) and JPMC (51 cases).
Ethical approval was obtained from all three institutions (AKUH, CHK and JPMC) before starting the study. Data was collected using convenience sampling technique. All patients of 16 years and above presenting to the EDs of the respective hospitals with DSH attempt were invited to participate in the study. For each case, a control was enrolled in the study, matched with case for hospital, gender and age (± 4 years). Controls included patients admitted to EDs with diagnosis other than DSH and who were not critically ill (intubated and obtunded patients, those with third degree burns and life-threatening injuries). Written informed consent was taken from both cases and control.
Two interviewers’ administered questionnaires were developed to collect information on the risk factors of DSH. The first questionnaire was named DSH-Risk Factors and was a modified version of the questionnaire used in a study to identify risk factors associated with suicide in Karachi, Pakistan.11 Information on demographic status of participants, education and employment, mental and physical health, social network, details of life events and difficulties, history of DSH in relatives/peers/friends and on substance and or alcohol abuse. This questionnaire included a section on details on current and previous DSH attempts for cases. The questionnaire was translated into Urdu and then translated back to English to retain the original meaning of the question. It was pre-tested on 5% of the study population in the ED of AKUH.
The second questionnaire, Self Reporting Questionnaire (SRQ), was a validated questionnaire used to assess anxiety and depression.12 The questionnaires were administered by trained interviewers (medical students and psychologists, especially hired for the study) who were based in the EDs of each of the three hospitals for the period of the study. All interviewers underwent a 4-day training to achieve high inter-rater reliability.
Descriptive analysis for all variables was reported as frequency and percentages. Since it was a matched case control study, Conditional Logistic Regression (CLR) was conducted to assess the association of various risk factors with DSH. Risk factors found to be significant in univariate analysis were included in the final multivariate model. Odds ratios with their 95% confidence intervals were calculated and p-value of < 0.05 was considered significant. Data was analyzed using Statistical Package for the Social Sciences (SPSS) version 19. Post-hoc power analysis was done. Web based sample size calculator was used to calculate the power. Power analysis was based on effect size of major risk factor (mental illness). Odds ratio of mental illness (Table III) was 3.6 and the percentage of exposed (mental illness) in control group (Table III) was 6.5%. The number of cases (sample size per group) was 201 and the number of controls per case was one. Keeping the alpha risk of 5% and 1:1 matched study design the power of the study was 99.1213%.
Table III.
Mental health, physical health and social network related characteristics of cases of DSH and controls and conditional logistic regression analysis.
| Variables | Cases (n=201) | Controls (n=201) | Crude MOR | 95% CI
|
p-value | |
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| Do you currently have mental illness? | < 0.001 | |||||
| Yes | 43 (71.7) | 17 (28.3) | 3.6 | 1.79 | 7.25 | |
| No | 158 (46.2) | 184 (53.8) | 1.0 | |||
|
| ||||||
| Type of mental illness (current) | < 0.001 | |||||
| Unipolar depression | 25 (73.5) | 9 (26.5) | 4.1 | 1.65 | 10.57 | |
| Bipolar depression and others | 13 (76.5) | 4 (23.5) | 4.0 | 1.26 | 12.91 | |
| No mental illness | 163 (46.4) | 188 (53.6) | 1 | |||
|
| ||||||
| Past history of mental illness | < 0.001 | |||||
| Yes | 29 (90.6) | 3 (9.4) | 14.0 | 3.34 | 58.77 | |
| No | 172 (46.5) | 198 (53.5) | 1.0 | |||
|
| ||||||
| Type of mental illness (past) | < 0.001 | |||||
| No mental illness | 172 (46.5) | 198 (53.5) | 1.0 | |||
| Unipolar depression | 21(95.5) | 1(4.5) | 25.3 | 3.24 | 198 | |
| Bipolar depression and others | 8 (80) | 2 (20) | 6.4 | 1.06 | 39.47 | |
|
| ||||||
| Any physical illness in the past month? | < 0.001 | |||||
| Yes | 28 (28.9) | 69 (71.1) | 0.2 | 0.17 | 0.50 | |
| No | 173 (56.7) | 132 (43.3) | 1.0 | |||
|
| ||||||
| Do you share problems with someone? | < 0.001 | |||||
| Yes | 92 (36.5) | 160 (63.5) | 1.0 | |||
| No | 109 (72.7) | 41 (27.3) | 4.5 | 2.79 | 7.52 | |
|
| ||||||
| Sharing problems (relationship) | < 0.001 | |||||
| Parents | 51 (40.5) | 75 (59.5) | 0.26 | 0.14 | 0.47 | |
| Siblings | 14 (43.8) | 18 (56.3) | 0.28 | 0.11 | 0.67 | |
| Spouse | 10 (20) | 40 (80) | 0.09 | 0.04 | 0.23 | |
| Others | 17 (40.5) | 25 (59.5) | 0.30 | 0.13 | 0.68 | |
| No one | 109 (71.7) | 43 (28.3) | 1.0 | |||
|
| ||||||
| Do you know someone with DSH attempt? | 0.857 | |||||
| Yes | 15 (48.38) | 16 (51.6) | 0.9 | 0.46 | 1.90 | |
| No | 186 (50.13) | 185 (49.86) | 1.0 | |||
|
| ||||||
| Total SRQ score* | < 0.001 | |||||
| Mean (standard deviation)* | 9.0 (6.2) | 6.4 (5.1) | 1.10 | 1.05 | 1.14 | |
Mean (Standard deviation)*
RESULTS
The number of cases (sample size per group) was 201 and the number of controls per case was one.
Socio-demographic profile of the cases is shown in Table I. Of the 201 DSH patients included in the study, 62% were females (male:female ratio 1:1.6). The majority 89 (44.3%) were Urdu speaking. There were 7 (3.4%) Balochis, 27 (13.4%) Pathans, 22 (11%) Sindhis, 14 (7%) Punjabis and 42 (20.9%) others including Seraikis, Gujaratis and Memons etc. Eighty five (42%) of the cases were married. When marital status was stratified with gender, it was found that among married cases 67% were females. Of the ‘ever married’ and engaged cases (n=106), their spouse was chosen by the parents or the relatives in 55% of the cases. Seventy two percent of the cases lived in joint family system and 70% of cases had secondary or higher level education. One hundred twenty seven (63.2%) people were unemployed, of whom 45% (57/127) were housewives. More than half the cases stated that they found it difficult to share their problems or worries with someone.
Table I.
Distribution of cases and pair-matched controls by demographic and educational characteristics.
| Variable | Cases (n = 201) | Controls (n = 201) |
|---|---|---|
| Gender | ||
| Male | 77 (38.3) | 77 (38.3) |
| Female | 124 (61.7) | 124 (61.7) |
|
| ||
| Ethnicity | ||
| Urdu speaking | 89 (44.3) | 81 (40.3) |
| Sindhi | 22 (10.9) | 47 (23.4) |
| Punjabi | 14 (7.0) | 15 (7.5) |
| Pathan | 27 (13.4) | 15 (7.5) |
| Balochi | 07 (3.4) | 18 (9.0) |
| Others | 42 (20.9) | 25 (12.4) |
|
| ||
| Education | ||
| Illiterate | 33 (16.4) | 48 (23.9) |
| Primary | 28 (13.9) | 20 (10.0) |
| Secondary | 24 (11.9) | 25 (12.4) |
| Matric | 44 (21.9) | 28 (13.9) |
| Intermediate | 37 (18.4) | 33 (16.4) |
| Graduate/postgraduate | 35 (17.4) | 47 (23.4) |
|
| ||
| Marital status | ||
| Single | 94 (46.8) | 87 (43.3) |
| Engaged | 11 (5.5) | 14 (7.0) |
| Married | 85 (42.3) | 99 (49.3) |
| Separated/divorced/widowed | 11 (5.5) | 01 (0.5) |
|
| ||
| Choice in selection of spouse | ||
| Parents/relatives | 58 (28.9) | 74 (36.8) |
| Own choice | 20 (10.0) | 23 (11.4) |
| Both | 28 (13.9) | 17 (8.5) |
| Not applicable | 95 (47.3) | 87 (43.3) |
|
| ||
| Living with | ||
| Alone | 06 (3.0) | 05 (2.5) |
| Nuclear family | 26 (12.9) | 31 (15.4) |
| Joint family | 144 (71.6) | 145 (72.1) |
| Extended family/don’t know/others | 25 (12.4) | 20 (10.0) |
|
| ||
| Do you have children? | ||
| Yes | 65 (69.9) | 68 (68.0) |
| No | 28 (30.1) | 32 (32.0) |
|
| ||
| Do you have infants? | ||
| Yes | 16 (8.0) | 20 (10.0) |
| No | 185 (92.0) | 181 (90.0) |
|
| ||
| Accommodation | ||
| Owned | 56 (27.6) | 86 (42.8) |
| Rented | 42 (21) | 57 (28.4) |
| Owned by parents | 59 (29.4) | 43 (21.4) |
| Owned by spouse/hostel/others | 44 (22) | 15 (7.5) |
|
| ||
| Employment | ||
| Yes | 51 (25.4) | 58 (28.9) |
| No | 70 (34.8) | 88 (43.8) |
| Students | 23 (11.4) | 20 (10.0) |
| Housewife | 57 (28.4) | 35 (17.4) |
|
| ||
| Do you have problems at work? | ||
| Yes | 35(21.7) | 29(19.1) |
| No | 126(78.3) | 123(80.9) |
|
| ||
| Are you treated for physical illness? | ||
| Yes | 28 (13.9) | 69 (34.3) |
| No | 173 (86.1) | 132 (65.7) |
|
| ||
| Do you share problems with someone? | ||
| Yes | 92 (45.8) | 160 (79.6) |
| No | 109 (54.2) | 41 (20.4) |
|
| ||
| Sharing problems (relationship) | ||
| Parents | 51 (25.4) | 75 (37.3) |
| Siblings | 14 (7.0) | 18 (9.0) |
| Spouse | 10 (5.0) | 40 (19.9) |
| Others | 17 (8.5) | 25 (12.4) |
| No one | 109 (54.2) | 43 (21.4) |
|
| ||
| Are you suffering from mental disorder? | ||
| Yes | 43 (21.4) | 17 (8.5) |
| No | 158 (78.6) | 184 (91.5) |
The most common reason of DSH (58.5%) were interpersonal problems with close family members (spouse, parents, siblings or in-laws). Mental illnesses were observed in 9% of cases; financial crisis was the reason in 10.5% cases. It was also observed that 8% patients committed DSH because they were not allowed to be engaged to or marry the person of their choice. Unemployment was the cause in 4.5% cases. Other reasons stated included: problems in education (2.5%); a death of ‘beloved one’ (2%); recent divorce and medical illness (1% each), infertility (1.5%) and one case each due to pregnancy, rejection of visa, post-delivery and problems in the jobs.
Demographic, socio-economic and work related characteristics are shown in Table II. Majority of the cases recruited in the study were of Pathan ethnicity (64.3%), while majority of the controls were of Sindhi ethnicity (68.1%). Among cases 28.9% had arranged marriages where the selection of spouses was made by the parents compared to controls where 36.8% marriages were arranged by their parents. Only one case had written a suicidal note before DSH. Other characteristics of the participants are given in Table II.
Table II.
Demographic, socio-economic and work related characteristics of cases of DSH and controls and conditional logistic regression analysis.
| Variables | Cases (n=201) | Controls (n=201) | Crude MOR | 95% CI
|
p-value | |
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| Ethnicity | < 0.001 | |||||
| Balochi | 7 (28) | 18 (72) | 1.00 | |||
| Urdu speaking | 89 (52.4) | 81 (47.6) | 3.08 | 1.12 | 8.47 | |
| Punjabi | 14 (48.3) | 15 (51.7) | 2.34 | 0.76 | 7.16 | |
| Pathan | 27 (64.3) | 15 (35.7) | 4.67 | 1.52 | 14.39 | |
| Sindhi | 22 (31.9) | 47 (68.1) | 1.12 | 0.37 | 3.35 | |
| Others | 42 (62.7) | 25 (37.3) | 5.03 | 1.68 | 15.04 | |
|
| ||||||
| Marital status | 0.633 | |||||
| Never married (single and engaged) | 105 (50.9) | 101 (49.1) | 1.00 | - | - | |
| Ever married (with children) | 96 (48.9) | 100 (51.1) | 1.12 | 0.70 | 1.79 | |
|
| ||||||
| Choice in selection of spouse (Ever married and engaged n=106) | 0.149 | |||||
| Parents/relatives | 58 (43.9) | 74 (56.1) | 1.00 | - | - | |
| Own | 20 (46.5) | 23 (53.5) | 1.13 | 0.54 | 2.34 | |
| Both (Parents/relatives and own) | 28 (62.3) | 17 (37.7) | 2.08 | 1.04 | 4.14 | |
|
| ||||||
| Do you have children? (n=193) | 0.346 | |||||
| Yes | 65 (48.7) | 68 (51.3) | 1.57 | 0.61 | 4.05 | |
| No | 28 (46.7) | 32 (53.3) | 1.00 | - | - | |
|
| ||||||
| Do you have infants? (n=193) | 0.617 | |||||
| Yes | 16 (44.4) | 20 (55.6) | 0.78 | 0.29 | 2.09 | |
| No | 185 (50.5) | 181 (49.5) | 1.00 | - | - | |
|
| ||||||
| Accommodation | 0.002 | |||||
| Owned | 56 (39.4) | 86 (60.6) | 1.00 | - | - | |
| Rented/owned by others | 145 (55.8) | 115 (44.2) | 1.94 | 1.26 | 2.97 | |
|
| ||||||
| Education | 0.378 | |||||
| No education/primary | 61 (47.3) | 68 (52.7) | 0.80 | 0.49 | 1.31 | |
| Secondary and above | 140 (51.3) | 133 (48.7) | 1.00 | - | - | |
|
| ||||||
| Current employment status | 0.345 | |||||
| Yes | 51 (46.8) | 58 (53.2) | 1.00 | - | - | |
| No | 150 (51.2) | 143 (48.8) | 1.29 | 0.76 | 2.20 | |
|
| ||||||
| Do you have problems at work? (313) | 0.446 | |||||
| Yes | 35 (54.7) | 29 (45.3) | 1.26 | 0.69 | 2.31 | |
| No | 126 (50.6) | 123 (49.4) | 1.00 | - | - | |
MOR = Matched Odds Ratio
Mental health, physical health and social network related characteristics are shown in Table III. Current history of mental illness (OR=3.6), currently having depression (OR=4.0), those under treatment for mental disorder (OR=3.8), past history of mental illness (OR=14), past history of unipolar depression (OR=25.3), not sharing problems with someone (OR=4.5) were all positively associated with the risk of DSH. There was no association with any physical illness in the past month, type of relationship having someone to share with their problems or knowing someone who had made a DSH attempt. Mean SRQ score of DSH cases was 9.0 as compared to controls of 6.4.
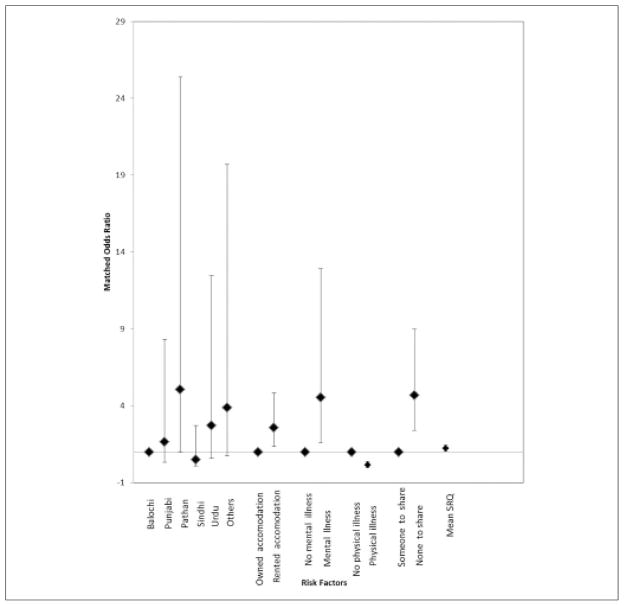
On multivariate conditional logistic regression analysis, individuals of Pathan ethnicity (OR = 5.05, 95% CI 1.01 – 25.38) had a greater risk of committing DSH. Likewise individuals residing in rented accommodation had a greater risk (OR = 2.58, 95% CI = 1.37 – 4.84) compared to those living in their own accommodation. Individuals with a mental disorder (OR = 4.53, 95% CI = 1.59 – 12.92) and those who did not share problems with someone (OR = 4.67, 95% CI = 2.4 – 9.0) were also at increased risk of DSH. Absence of physical illness in the past month had an inverse association with DSH (Figure 1). The multivariate model also inquired about the knowledge of any close person (friend or relative) who had made a DSH attempt in the past but this was not found to be significantly associated with DSH.
Figure 1.
Association of risk factors with DSH in tertiary care hospitals in Karachi
DISCUSSION
DSH is now considered as a major public health problem in Pakistan.13 Local studies on DSH are mostly descriptive case series.14,15 This is the first case-control study that has described risk factors of patients with DSH presenting to the EDs of general hospitals in Pakistan, to the best of author’s knowledge. Despite of limitations, the study highlights some interesting findings. The female to male ratio in this study was not too dissimilar to previous studies from Pakistan.5 However, almost 70% of the study sample had received at least secondary or higher education. This may reflect the relatively higher literacy rate in Karachi of 74%, compared to the national literacy rate (58.5%).16
This study showed that most (71%) DSH patients lived in a joint family system. Although it is generally assumed that joint family system is a protective factor against mental distress and suicidal behavior, this is not borne by this study. In fact it appears that joint and extended family systems may be the cause of mental distress and suicidal behavior in many cases.17 This observation needs to be studied further. Forty six percent of the females (n=124) in our sample were housewives. The findings are similar to another hospital based study.18 A number of studies from Pakistan show that unlike the West, marriage is a risk factor for psychiatric morbidity and DSH in Pakistan.19 An important factor in marriages in Pakistan is the issue of autonomy in selection of marital partner. Most marriages in Pakistan continue to be arranged, with the parents choosing the prospective marital partner for their children.14 There is high incidence of marital morbidity in marriages in Pakistan20 and this appears to be reflected in this study. Those people who are not living with the families like Pathans are isolated and have lack of social support may explain higher number of events in this group.
Many patients in this study had underlying mental illnesses (mainly depression) and having current or past history of treatment for mental disorders. It was also seen from other studies that mental illnesses are increasing in Pakistan21 especially in DSH patients.22 Physical illness in the past month was a protective factor against DSH. This could be due to the fact that patients who get ill may make contact with health professionals and facilities and hence their mental health issues are addressed indirectly. This study shows the importance of recognizing and managing mental illnesses in Pakistan at an early stage. Given the fact there is a delay, on average, of 4.5 years from the onset of symptoms of depression to seeking help from a mental health professional in Pakistan, this is a huge challenge.23
This study has certain limitations. Convenience sampling technique was used to collect the data which can lead to under or over representation of the groups. However, this technique was used for ease, low cost and time. History of mental illness/issue was taken directly from the patient that can sometimes be misleading in the emergency situation especially when the patient has already committed DSH and is in the initial phase of medical management. Estimated numbers of DSH in Karachi could be as high as 3000 – 6000 per year, of which approximately 350 cases are admitted to JPMC, National Poisons Control Center only.24 Equal number of patients were inducted from both public hospitals in order to compare public and private hospital patients simultaneously. This may explain the small number of patients recruited from JPMC in this study. Also, since only the patients presenting to the EDs of three hospitals in Karachi were studied, hence these findings may not be generalizable to other parts of the country.
CONCLUSION
Risk factors of DSH patients presenting to the EDs of Karachi included current history of mental disorder, loneliness (not sharing problems with someone) and low socio-economic status (those who live in rented houses). Inverse association of DSH was observed with absence of physical illness in the past month. Patients who present to an ED with DSH should undergo a psychiatric evaluation. This will help in early diagnosis and management of mental illnesses in these patients.
Table IV.
Based on multivariable conditional logistic analysis showing the association of risk factors with DSH.
| Variables | MOR (adjusted) | 95% CI
|
p-value | |
|---|---|---|---|---|
| Lower | Upper | |||
|
| ||||
| Ethnicity | 0.003 | |||
| Balochi | 1.00 | -f | - | |
| Punjabi | 1.66 | 0.33 | 8.31 | |
| Pathan | 5.05 | 1.01 | 25.38 | |
| Sindhi | 0.51 | 0.09 | 2.73 | |
| Urdu speaking | 2.71 | 0.59 | 12.45 | |
| Others | 3.88 | 0.77 | 19.69 | |
|
| ||||
| Accommodation | 0.003 | |||
| Owned | 1.00 | - | - | |
| Rented/owned by others | 2.58 | 1.37 | 4.84 | |
|
| ||||
| Current history of mental disorder | 0.005 | |||
| Yes | 4.53 | 1.59 | 12.92 | |
| No | 1.00 | - | - | |
|
| ||||
| Any physical illness in past month | <0.001 | |||
| Yes | 0.17 | 0.07 | 0.37 | |
| No | 1.00 | - | - | |
|
| ||||
| Someone to share your problems with | <0.001 | |||
| Yes | 1.00 | - | - | |
| No | 4.67 | 2.4 | 9.0 | |
|
| ||||
| Total SRQ score* | 1.12 | 1.05 | 1.19 | <0.001 |
Mean (Standard deviation)*
Acknowledgments
We are thankful to Aysha Khan (AKUH), Dr Badar Afzal (AKUH), Sumaiya Tauseeq Khan (CHK), Syeda Asra Qadri (AKUH), Hatem Adel (CHK), Shahzad Saleem (CHK) and Salwa Tauseeq Khan (Baqai Medical University) for collecting the data from three Emergency Departments of Karachi and Dr Seemin Jamali (JPMC) and Dr Razia Sheikh (CHK) for helping the research assistants in collecting the data. We also appreciate the efforts of Dr Junaid Bhatti (AKUH), Dr Amna Zeb (Johns Hopkins University), Jawaid Shah (AKUH) for translating the questionnaire into Urdu and Dr Haider Naqvi (AKUH), Dr Kiran Ejaz (AKUH) and Dr Amna Zeb (Johns Hopkins University) for training the research assistants before conducting the study. We are thankful to Mr Iqbal Azam (AKU) for helping in interpreting the data.
We gratefully acknowledge the support from the United States National Institutes of Health (NIH) John E. Fogarty International Center for Advanced Study in the Health Sciences, under the Johns Hopkins-Aga Khan Fogarty International Trauma and Injury Training Program grant (D43-TW007-292).
Footnotes
The contents of this paper are solely the responsibility of the authors and do not necessarily represent the official views of NIH.
References
- 1.Hawton K, Harriss L, Hall S, Simkin S, Bale E, Bond A. Deliberate self-harm in Oxford, 1990–2000: a time of change in patient characteristics. Psychol Med. 2003;33:987–95. doi: 10.1017/s0033291703007943. [DOI] [PubMed] [Google Scholar]
- 2.Khan MM. Suicide prevention in Pakistan: an impossible challenge? J Pak Med Assoc. 2007;57:478–9. [PubMed] [Google Scholar]
- 3.Khan MM, Reza H. The pattern of suicide in Pakistan. Crisis. 2000;21:31–5. doi: 10.1027//0227-5910.21.1.31. [DOI] [PubMed] [Google Scholar]
- 4.Khan MM. Suicide and attempted suicide in Pakistan. Crisis. 1998;19:172–6. doi: 10.1027/0227-5910.19.4.172. [DOI] [PubMed] [Google Scholar]
- 5.Shahid M, Khan MM, Khan MS, Jamal Y, Badshah A, Rehmani R. Deliberate self-harm in the Emergency Department: experience from Karachi, Pakistan. Crisis. 2009;30:85–9. doi: 10.1027/0227-5910.30.2.85. [DOI] [PubMed] [Google Scholar]
- 6.Khan MM, Prince M. Beyond rates: the tragedy of suicide in Pakistan. Trop Doct. 2003;33:67–9. doi: 10.1177/004947550303300203. [DOI] [PubMed] [Google Scholar]
- 7.Shahid M, Hyder AA. Deliberate-self harm and suicide: a review from Pakistan. Int J Inj Contr Saf Promot. 2008;15:233–41. doi: 10.1080/17457300802149811. [DOI] [PubMed] [Google Scholar]
- 8.Khalid N. Pattern of suicide: causes and methods employed. J Coll Physicians Surg Pak. 2001;11:759–61. [Google Scholar]
- 9.Hawton K, Heeringen KV. Suicide. Lancet. 2009;373:1372–81. doi: 10.1016/S0140-6736(09)60372-X. [DOI] [PubMed] [Google Scholar]
- 10.Shahid M, Naqvi HA. Role of emergency physicians in psychiatric care in Pakistan. J Pak Psych Soc. 2006;3:115. [Google Scholar]
- 11.Khan MM, Mahmud S, Karim MS, Zaman M, Prince M. Case-control study of suicide in Karachi, Pakistan. Br J Psychiatry. 2008;193:402–5. doi: 10.1192/bjp.bp.107.042069. [DOI] [PubMed] [Google Scholar]
- 12.Husain N, Richard G, Tomenson B, Creed F. Comparison of the personal health questionnaire and the self reporting questionnaire in rural Pakistan. J Pak Med Assoc. 2006;56:366–70. [PubMed] [Google Scholar]
- 13.Shahid M. Deliberate self-harm prevention in Pakistan. J Coll Physicians Surg Pak. 2013;23:101–2. [PubMed] [Google Scholar]
- 14.Khan MM, Islam S, Kundi AK. Parasuicide in Pakistan: experience at a university hospital. Acta Psychiatr Scand. 1996;93:264–7. doi: 10.1111/j.1600-0447.1996.tb10646.x. [DOI] [PubMed] [Google Scholar]
- 15.Haider SI, Haider I. Deliberate self poisoning (unemployment and debt) Pak J Med Sci. 2002;18:122–5. [Google Scholar]
- 16.Pakistan Bureau of Statistics. Pakistan: labour force survey 2010–11 [Internet] Available from: http://www.pbs.gov.pk/content/labour-force-survey-2010-11.
- 17.Bhattacharya AK, Bhattacharjee S, Chattopadhyay S, Roy P, Kanji D, Singh OP. Deliberate self-harm: a search for distinct group of suicide. Indian J Psychol Med. 2011;33:182–7. doi: 10.4103/0253-7176.92057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Patel MJ, Shahid M, Riaz M, Kashif W, Tariq M, Ayaz SI, et al. Drug over dose: A wake-up call. Experience at a tertiary care in Karachi. J Pak Med Assoc. 2008;58:298–301. [PubMed] [Google Scholar]
- 19.Shahid M, Khan MZ, Afzal B, Khan ST, Nakeer R. Deliberate self-harm patients visiting public and private emergency departments of Karachi. J Pak Psych Soc. 2014;11:28–30. [PMC free article] [PubMed] [Google Scholar]
- 20.Qadir F, de Silva P, Prince M, Khan M. Marital satisfaction in Pakistan: a pilot investigation. Sexual Rel Ther. 2005;20:195–209. [Google Scholar]
- 21.Mirza I, Jenkins R. Risk factors, prevalence, and treatment of anxiety and depressive disorders in Pakistan: systematic review. BMJ. 2004;328:794–8. doi: 10.1136/bmj.328.7443.794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bashir F, Ara J, Kumar S. Deliberate self poisoning at National Poisoning Control Centre. J Liaquat Uni Med Health Sci. 2014;13:3–8. [Google Scholar]
- 23.Sadruddin S. Thesis. Toronto: University of Toronto; 2007. Predictors of treatment delay in depressive disorders in Pakistan. [Google Scholar]
- 24.Turabi A, Danyal A, Hasan S, Durrani A, Ahmed M. Organophosphate poisoning in the urban population; study conducted at National Poison Control Center, Karachi. Biomedica. 2008;24:124–9. [Google Scholar]