Abstract
Background
Health care-associated infections (HAIs) are a major health concern, despite being largely avoidable. The emergency department (ED) is an essential component of the health care system and subject to workflow challenges, which may hinder ED personnel adherence to guideline-based infection prevention practices.
Methods
The purpose of this review was to examine published literature regarding adherence rates among ED personnel to selected infection control practices, including hand hygiene (HH) and aseptic technique during the placement of central venous catheters and urinary catheters. We also reviewed studies reporting rates of ED equipment contamination. PubMed was searched for studies that included adherence rates among ED personnel to HH during routine patient care, aseptic technique during the placement of central venous catheters and urinary catheters, and rates of equipment contamination.
Results
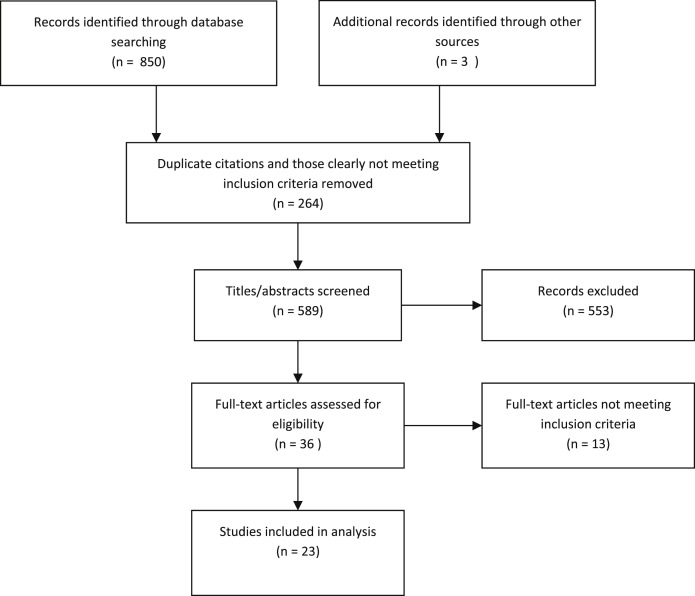
In total, 853 studies was screened, and 589 abstracts were reviewed. The full texts of 36 papers were examined, and 23 articles were identified as meeting inclusion criteria. Eight studies used various scales to measure HH compliance, which ranged from 7.7% to 89.7%. Seven articles examined central venous catheters inserted in the ED or by emergency medicine residents. Detail of aseptic technique practices during urinary catheterization was lacking. Four papers described equipment contamination in the ED.
Conclusion
Standardized methods and definitions of compliance monitoring are needed to compare results across settings.
Key Words: Infection prevention, Adherence
Health care-associated infections (HAIs) are a significant public health concern. Despite being largely preventable, these infections are a significant contributor to patient mortality and morbidity and are expensive to health care systems.1, 2 It is estimated that up to 70% of some types of HAIs are preventable through improved infection control practices among health care providers.3 Whereas a large proportion of preventable HAIs can be attributed to invasive procedures and devices such as urinary and central venous catheters,1 cross contamination may also occur through person-to-person spread after handling of contaminated equipment or other fomites.4
The emergency department (ED) is an essential component of the health care system, and its potential impact continues to grow as more individuals seek care and are admitted to the hospital through the ED.5 Invasive procedures such as central lines are placed with increased frequency in certain EDs, but adherence to best practices (eg maximum barrier precautions) varies.6, 7 ED clinicians also face numerous workflow challenges that may foster the spread of infections including crowding,8 frequent interruptions to care delivery,9 use of nontraditional care areas such as hallways and conference rooms,10 and close proximity of patients, who are often separated only by curtains.11 Given that many of these barriers have been identified as infection prevention threats,12, 13 it is critical to understand the infection prevention practices of ED providers and their potential role in the risk of HAIs.
We conducted a literature review to examine adherence rates among ED personnel to selected infection control practices: hand hygiene (HH) and aseptic technique during the placement of central venous catheters and urinary catheters, as well as the use of appropriate decision criteria for the insertion of a urinary catheter. We also examined rates of equipment contamination in the ED.
Methods
In collaboration with a research librarian, we searched the PubMed electronic database for studies that were published between June 1, 2002, and June 1, 2012. Using a Boolean combination of keywords and medical subject headings (Appendix 1), we conducted separate searches to capture adherence rates of HH during routine patient care, adherence rates of aseptic technique during the placement of central venous catheters and urinary catheters, adherence rates to urinary catheter insertion guidelines, and rates of equipment contamination. We selected these procedures because they are more likely to increase the risk of infection when compared with less invasive procedures such as peripheral intravenous catheter insertion. Articles were excluded if they concerned the contamination of cultures; described self-reported compliance; did not separate ED data from other areas under study; were review articles; and were commentaries, editorials, or discussions of the issue (ie, not data based). We also excluded studies that examined compliance during outbreaks or pandemics such as severe acute respiratory syndrome or emergency situations because we were interested in standard practices during routine care.
Using the same terms and time frame, we also electronically searched the tables of contents of the following journals: Academic Emergency Medicine, Emergency Medicine Journal, Emergency Medicine, Journal of Emergency Nursing, Annals of Emergency Medicine, European Journal of Emergency Medicine American Journal of Infection Control, Journal of Hospital Infection, and Infection Control and Hospital Epidemiology. Finally, we hand searched the reference sections of pertinent review articles that were identified in the PubMed search.
One researcher initially screened study titles and abstracts for overall relevance. The 3 authors then independently reviewed remaining study titles and abstracts. Collectively, study authors discussed the rationale for remaining articles based on the aforementioned inclusion and exclusion criteria. Disagreements were resolved through discussion and consensus. Articles that appeared to meet the inclusion criteria were reviewed in full text.
Results
As depicted in Figure 1 , at the initial screening phase, 853 articles were identified (850 from the original PubMed search; 3 through supplemental means). After removing duplicate citations and limiting articles to those published in English with available abstracts, 589 abstracts were screened. An additional 553 studies were excluded because they did not meet our inclusion criteria, primarily because they were self-reports of practices, did not report ED data separately, and/or observations of the placement of devices were made during emergency procedures. The full texts of 36 papers were reviewed, and 23 articles were identified as meeting study inclusion. These are summarized below.
Fig 1.
Flowchart of study selection.
Adherence to HH
HH was the most commonly observed infection prevention practice in studies reviewed, and adherence rates varied widely. In 6 major Kuwaiti hospitals, rates of HH were reported to be only 14.7% (57/387) using a rating scale published in 1974 to identify “dirty contacts.”14, 15 This contrasts with a rate of 89.7% (5,261/5,865) reported in an academic ED in New England that observed HH compliance using a modified version of the World Health Organization (WHO) observational tool to observe HH compliance before and after patient contact.13, 16 In a third paper, HH was assessed between patient encounters in 2 EDs. Among HH observations, compliance was 14% in the United Kingdom (UK) and 12% in New Zealand.17
Several studies examined HH practices before and after interventions. Haas and Larson used WHO guidelines to assess the impact of a wearable alcohol hand sanitizer dispenser among ED personnel in one New York hospital.18 Researchers observed a total of 757 HH opportunities. The adherence rate improved from 43% to 62% during the first intervention month of the study but was not sustained, with a 51% adherence rate after the second quarter.
A team from the United States and Italy published a series of papers examining the immediate and sustained impact of campaigns to improve HH.19, 20, 21 In 2005, a campaign was initiated in Tuscany, Italy, to improve HH practices. Three years after the start of the campaign, Saint et al20 examined the HH practices of health care workers in 5 hospital units in Tuscany, one of which was an ED. Observers were trained using WHO materials to observe HH before patient contact. HH rates in the ED were reported as 19.2% (46/239) for nurses and 7.7% (14/181) for physicians. A multimodal intervention was then implemented to improve HH in the previously studied ED, and the same team and observers again assessed adherence to HH prior to patient contact.19, 21 HH rates improved among nurses (40.7%, 107/263) and physicians (50.5%, 101/200), for an overall rate of 44.9%, which represented a 30.6% improvement in practice. This was sustained over a 1-year period postintervention, with an overall HH rate of 45.2% (206/456).
Another study used WHO guidelines to examine HH practices among ED personnel after the implementation of a HH educational campaign. This study was conducted over a 1-year period by researchers from Saudi Arabia.22 At the completion of the campaign, adherence rates were reported as 60% for nurses, 50% for patient care technicians, and 20% for physicians.
Aseptic technique during urinary catheterization
We found one study that observed aseptic technique during urinary catheterization.17 In this study, medical students used standardized observation tools to observe aseptic technique in one ED in the UK and another ED in New Zealand. Procedures observed included urinary catheterization, wound examination or closure, injections or intravascular cannulation, lumbar puncture, and pleural aspiration. Overall, 27% (UK) and 58% (New Zealand) of invasive procedures (n = 65) were performed using aseptic technique. Adherence to aseptic technique was reported in aggregate and not categorized by procedure type.
Appropriateness of urinary catheterization
Four studies examined the extent to which urinary catheter insertion was appropriate. In one descriptive study, Fakih et al23 reported that 69.7% (371/532) of catheters inserted in the ED were indicated and that 58.6% (312/532) were documented in a physician's order. Researchers noted that elderly women were at greater risk for inappropriate catheterization.
Three other studies assessed the effect of interventions on reducing rates of inappropriate urinary catheterization. Gokula et al24 conducted 6 educational sessions over a period of 6 weeks for ED physicians and nurses to review the criteria for appropriate catheter use and also developed a catheter indication sheet. Subsequently, 100 medical records pre- and postintervention were reviewed to assess the percentage of patients with appropriate urinary catheterization. Whereas there was an overall decrease in the number of urinary catheters placed, which was sustained over several years, there was no statistically significant difference in appropriate catheter use before and after the educational sessions (37% and 51%, respectively, P = .06).
A similar pre-/postintervention study evaluated the impact of institutional urinary catheter guidelines, which were presented in a lecture to the ED medical staff.25 Whereas there was an overall reduction in urinary catheterization from 14.9% to 10.6% of patients (P = .002), there was no significant difference in the proportion of inappropriate urinary catheterizations before and after the intervention (33.6% and 29.5%, respectively, P = .41). This same research team in 2011 assessed the impact of resident peer-to-peer education on the placement of medically appropriate urinary catheters. The intervention for 30 residents consisted of lectures, pocket cards, and weekly peer review of guidelines. Although knowledge scores improved among residents pre- and postintervention, there was no reduction in the proportion of admitted patients who were catheterized or in the percentage of appropriate urinary catheterizations (14.2% and 14.1%; 74.1% and 68.9%, pre- and postintervention, respectively).26
Aseptic technique during central venous catheter insertion
We found 7 articles that examined central venous catheters inserted in the ED or by emergency medicine residents. One study examined the effect of a video review on the sterile technique practices of surgical and emergency medicine residents during the placement of central lines.27 Compliance to aseptic technique was higher among those who received the video-based online training than those who received paper-based training or no training (74% vs 33%, respectively; odds ratio, 6.1). In a separate evaluation, the same research team also assessed maximum barrier precautions among primary and secondary operators through a video recording. Among elective central lines, maximum barrier precautions were used by 88% (99/113) of primary operators and 69% (31/45) of secondary operators or senior medical staff.28
ED-placed central venous catheters and infectious outcomes
Whereas further investigators did not detail sterile technique practices during line insertion, study authors did report infectious complications among ED-placed central lines. In one study, researchers found that central lines placed in high-risk departments including the ED and intensive care unit were more likely be become infected than catheters placed in less high-risk departments.29 Another research team found similar bloodstream infection rates among ED- and intensive care unit-placed central lines,30 and, in a separate evaluation, no central line-associated bloodstream infections occurred among 50 central lines placed in the ED.31 Two additional studies reported higher rates of bloodstream infection or colonization among catheters inserted in the ED when compared with central catheters placed in other hospital units.32, 33
Equipment contamination
Four papers described equipment contamination in the ED; of primary focus was contamination with methicillin-resistant Staphylococcus aureus (MRSA). In one large ED from a United States tertiary care hospital, 7% (5/69) of environmental surfaces (chairs, keyboards, telephones, and others) were positive for MRSA compared with no positive sites (0/63) in an outpatient clinic.34 Another research team35 took 63 samples of computer mice in an ED in Northern Ireland over a 1-year period and found only normal skin flora, with no MRSA. In a United States ED, Frazee et al36 took surveillance cultures of ultrasonographic probes used in the ED; approximately two thirds (111/164) were contaminated with skin or environmental flora, 8 samples had heavy growth of skin or environmental flora, and 3.7% (6/164) grew organisms including methicillin-sensitive S aureus, Aspergillus, Acinetobacter spp, and mixed gram-negative rods. Finally, Tang et al37 cultured the stethoscopes of ED nurses and physicians in 3 Canadian EDs. Of the 100 stethoscopes samples, 70% were contaminated. A majority of specimens grew coagulase-negative staphylococci (54/100).
Discussion
To our knowledge, this is the first literature review detailing adherence rates with common infection prevention practices in the ED setting. In this small but growing body of literature, there are several lessons to be learned and gaps to be filled. Whereas there were a number of papers that reported HH practices, there was a wide range in reported rates, from 7.7% to 89.7%. Unfortunately, it is not possible to draw conclusions from the data because the methods of observation varied widely. In one study, the definition of a HH indication was prior to patient contact; in another, prior to a “dirty contact”; and other studies adopted or adapted the WHO “Five Moments of HH.”16 Because the WHO observational methods were first published in 2007 and are becoming the state of the art for HH observation, it is likely that future studies using direct observation to assess HH practices will be more standardized, making it possible for the first time to compare across sites. Even more promising are newer methods of electronic monitoring of HH, which avoid the problem of the “Hawthorne effect” and observer bias, are nonintrusive, and are much more likely to provide a real-time accurate picture of HH practices.38
We were unable to find detailed information regarding aseptic practices during urinary catheterization, probably not surprising because of the private nature of the procedure. Despite this, data show that the ED is a common source of urinary catheterization and that guidelines for when a catheter is indicated are often not followed. Guidelines to prevent catheter-associated urinary tract infections have been consistently published for decades.39 Nevertheless, in a survey of 415 US intensive care units, Conway et al40 found that only a small proportion actually had policies consistent with these guidelines and concluded that little attention is currently being paid to the prevention of catheter-associated urinary tract infections.
This raises the issue of how to successfully intervene to reduce unnecessary urinary catheterizations. Intervention studies included in our review consisted of guidelines and education, which targeted physicians, nurses, and/or residents. Whereas these interventions generally resulted in an overall reduction of urinary catheter utilization, they had little impact on urinary catheter appropriateness. Studies in other acute care settings found that interventions that have successfully improved adherence to catheter guidelines include reviews and reminders and empowering nurses to determine when catheters are indicated or should be removed.41, 42, 43
Although this review was not designed to examine infectious outcomes related to ED catheters, we did find several studies that linked ED-placed central venous catheters to subsequent infection. Many of these studies are detailed in a recent systematic review, where authors conclude that ED-placed central venous catheters are a source of infection.7 Notably, few studies included in this review detailed compliance with infection prevention protocols during ED central line insertion. Future research should examine the adoption of best practices aimed to prevent infection in the ED. Similarly, whereas several studies examined environmental or equipment contamination in the ED, future studies should focus on critical items likely to come in direct contact with patients. Such was the case in the study reporting contamination of ultrasonographic probes ready for patient use,36 but studies of computer keyboards or other less critical items generally yield predictable results that add little new information.
This review was limited by the inclusion of only articles in English and those with abstracts, and use of a single data source with a limited number of search terms. Clearly, it is possible that studies were missed. Additionally, studies cited were conducted in several countries that certainly vary in terms of culture and services provided (eg, levels of care, local guidelines and standards, and skills and workloads of staff). Nevertheless, several recommendations can be made. First, if infection prevention practices are to be observed or monitored, standardized methods and definitions are essential so that results can be compared across settings. Second, more efforts are needed to reduce unnecessary urinary catheterization in the ED (as well as in other clinical settings), and interventions to improve adherence to guidelines may include staff review and reminders regarding practice. Third, environmental sampling should be targeted to critical equipment and surfaces likely to contaminate patients. Finally, studies are needed to examine the impact of infection prevention practices in the ED on subsequent risk of infection.
Footnotes
Conflicts of interest: None to report.
Appendix 1. Search terms and strategies used
Search: Asepsis & CVCs in ED (57 articles; limited to English language and humans = 50 articles)
(“catheterization, central venous”[MeSH Terms] OR “catheterization”[MeSH Terms] OR “catheters”[MeSH Terms] OR “central line”[All Fields] OR “central lines”[All Fields]) AND (“asepsis”[MeSH Terms] OR “asepsis”[All Fields] OR “guideline adherence”[MeSH Terms] OR “catheter-related infections”[MeSH Terms]) AND (“emergency service, hospital”[MeSH Terms] OR “emergency medical services”[MeSH Terms] OR “emergencies”[MeSH Terms] OR (“emergency”[All Fields] AND department[All Fields]) OR (“emergency”[All Fields] AND room[All Fields]) OR (“emergency”[All Fields] AND ward[All Fields]) OR “emergency nursing” [MeSH Terms] OR “emergency medicine”[MeSH Terms]) AND (“2002/06/01”[PDAT] : “2012/06/01”[PDAT])
Search: Asepsis & UCs in ED (55 articles; limited to English language and humans = 48 articles)
(“urinary catheterization”[MeSH Terms] OR “intermittent urethral catheterization”[MeSH Terms] OR “foley catheter”[All Fields] OR “catheterization”[MeSH Terms]) AND (“asepsis”[MeSH Terms] OR “asepsis”[All Fields] OR “guideline adherence”[MeSH Terms] OR “catheter-related infections”[MeSH Terms]) AND (“emergency service, hospital”[MeSH Terms] OR “emergency medical services” [MeSH Terms] OR “emergencies”[MeSH Terms] OR (“emergency”[All Fields] AND department[All Fields]) OR (“emergency”[All Fields] AND room[All Fields]) OR (“emergency”[All Fields] AND ward[All Fields]) OR “emergency nursing”[MeSH Terms] OR “emergency medicine”[MeSH Terms]) AND (“2002/06/01”[PDAT] : “2012/06/01”[PDAT])
Search: HH in ED (768 articles; limited to English language and humans = 676 articles).
(“handwashing”[MeSH Terms] OR “universal precautions”[MeSH Terms] OR (“standard”[All Fields] AND precautions[All Fields]) OR (“hand”[MeSH Terms] AND “hygiene”[MeSH Terms]) OR “infection control”[MeSH Terms] OR “cross infection”[MeSH Terms]) AND (“emergency service, hospital”[MeSH Terms] OR “emergency medical services”[MeSH Terms] OR “emergencies”[MeSH Terms] OR (“emergency”[All Fields] AND department[All Fields]) OR (“emergency”[All Fields] AND room[All Fields]) OR (“emergency”[All Fields] AND ward[All Fields]) OR “emergency nursing”[MeSH Terms] OR “emergency medicine”[MeSH Terms]) AND (“2002/06/01”[PDAT] : “2012/06/01”[PDAT])
Date of search: 7/21/2012
Search: Equipment Contamination in ED (82 articles; limited to English and humans = 71; not included in above search = 27)
(“equipment contamination”[MeSH Terms] OR “equipment contamination”[All Fields] OR “equipment hygiene”[All Fields]) AND (“emergency service, hospital”[MeSH Terms] OR “emergency medical services”[MeSH Terms] OR “emergencies”[MeSH Terms] OR (“emergency”[All Fields] AND department[All Fields]) OR (“emergency”[All Fields] AND room[All Fields]) OR (“emergency”[All Fields] AND ward[All Fields]) OR “emergency nursing”[MeSH Terms] OR “emergency medicine”[MeSH Terms]) AND (“2002/06/01”[PDAT] : “2012/06/01”[PDAT])
References
- 1.Scott R. Centers for Disease Control and Prevention; Atlanta [GA]: 2009. The direct medical costs of healthcare-associated infections in US hospitals and the benefits of prevention. [Google Scholar]
- 2.Klevens R.M., Edwards J.R., Richards C.L., Jr., Horan T.C., Gaynes R.P., Pollock D.A. Estimating health care-associated infections and deaths in US hospitals, 2002 (Washington, DC: 1974) Public Health Rep. 2007;122:160–166. doi: 10.1177/003335490712200205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Umscheid C.A.M.D.M., Mitchell M.D.P., Doshi J.A.P., Agarwal R.M.D.M.P.H., Williams K.M.D.M.P.H., Brennan P.J.M.D. Estimating the proportion of healthcare-associated infections that are reasonably preventable and the related mortality and costs. Infect Control Hosp Epidemiol. 2011;32:101–114. doi: 10.1086/657912. [DOI] [PubMed] [Google Scholar]
- 4.Hardy K.J., Oppenheim B.A., Gossain S., Gao F., Hawkey P.M. A study of the relationship between environmental contamination with methicillin-resistant Staphylococcus aureus (MRSA) and patients' acquisition of MRSA. Infect Control Hosp Epidemiol. 2006;27:127–132. doi: 10.1086/500622. [DOI] [PubMed] [Google Scholar]
- 5.Schuur J.D., Venkatesh A.K. The growing role of emergency departments in hospital admissions. N Engl J Med. 2012;367:391–393. doi: 10.1056/NEJMp1204431. [DOI] [PubMed] [Google Scholar]
- 6.Glickman S.W., Krubert C., Koppenhaver J., Glickman L.T., Schulman K.A., Cairns C.B. Increased rate of central venous catheterization procedures in community EDs. Am J Emerg Med. 2010;28:208–212. doi: 10.1016/j.ajem.2008.10.016. [DOI] [PubMed] [Google Scholar]
- 7.Lemaster C.H., Agrawal A.T., Hou P., Schuur J.D. Systematic review of emergency department central venous and arterial catheter infection. Int J Emerg Med. 2010;3:409–423. doi: 10.1007/s12245-010-0225-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hoot N.R., Aronsky D. Systematic review of emergency department crowding: causes, effects, and solutions. Ann Emerg Med. 2008;52:126–136. doi: 10.1016/j.annemergmed.2008.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Magid D.J., Sullivan A.F., Cleary P.D., Rao S.R., Gordon J.A., Kaushal R. The safety of emergency care systems: Results of a survey of clinicians in 65 US emergency departments. Ann Emerg Med. 2009;53 doi: 10.1016/j.annemergmed.2008.10.007. 715-23, e1. [DOI] [PubMed] [Google Scholar]
- 10.McNaughton C., Self W.H., Jones I.D., Arbogast P.G., Chen N., Dittus R.S. ED crowding and the use of nontraditional beds. Am J Emerg Med. 2012;30:1474–1480. doi: 10.1016/j.ajem.2011.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Moskop J.C., Marco C.A., Larkin G.L., Geiderman J.M., Derse A.R. From Hippocrates to HIPAA: privacy and confidentiality in emergency medicine, part II: challenges in the emergency department. Ann Emerg Med. 2005;45:60–67. doi: 10.1016/j.annemergmed.2004.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Harbarth S., Sudre P., Dharan S., Cadenas M., Pittet D. Outbreak of Enterobacter cloacae related to understaffing, overcrowding, and poor hygiene practices. Infect Control Hosp Epidemiol. 1999;20:598–603. doi: 10.1086/501677. [DOI] [PubMed] [Google Scholar]
- 13.Venkatesh A.K., Pallin D.J., Kayden S., Schuur J.D. Predictors of hand hygiene in the emergency department. Infect Control Hosp Epidemiol. 2011;32:1120–1123. doi: 10.1086/662374. [DOI] [PubMed] [Google Scholar]
- 14.Al-Wazzan B., Salmeen Y., Al-Amiri E., Abul A., Bouhaimed M., Al-Taiar A. Hand hygiene practices among nursing staff in public secondary care hospitals in Kuwait: self-report and direct observation. Med Princ Pract. 2011;20:326–331. doi: 10.1159/000324545. [DOI] [PubMed] [Google Scholar]
- 15.Fox M.K., Langner S.B., Wells R.W. How good are hand washing practices? Am J Nurs. 1974;74:1676–1678. [PubMed] [Google Scholar]
- 16.Sax H., Allegranzi B., Chraiti M.N., Boyce J., Larson E., Pittet D. The World Health Organization hand hygiene observation method. Am J Infect Control. 2009;37:827–834. doi: 10.1016/j.ajic.2009.07.003. [DOI] [PubMed] [Google Scholar]
- 17.Al-Damouk M., Pudney E., Bleetman A. Hand hygiene and aseptic technique in the emergency department. J Hosp Infect. 2004;56:137–141. doi: 10.1016/j.jhin.2003.09.022. [DOI] [PubMed] [Google Scholar]
- 18.Haas J.P., Larson E.L. Impact of wearable alcohol gel dispensers on hand hygiene in an emergency department. Acad Emerg Med. 2008;15:393–396. doi: 10.1111/j.1553-2712.2008.00045.x. [DOI] [PubMed] [Google Scholar]
- 19.Saint S., Conti A., Bartoloni A., Virgili G., Mannelli F., Fumagalli S. Improving healthcare worker hand hygiene adherence before patient contact: a before-and-after five-unit multimodal intervention in Tuscany. Qual Saf Health Care. 2009;18:429–433. doi: 10.1136/qshc.2009.032771. [DOI] [PubMed] [Google Scholar]
- 20.Saint S., Bartoloni A., Virgili G., Mannelli F., Fumagalli S., di Martino P. Marked variability in adherence to hand hygiene: a 5-unit observational study in Tuscany. Am J Infect Control. 2009;37:306–310. doi: 10.1016/j.ajic.2008.08.004. [DOI] [PubMed] [Google Scholar]
- 21.di Martino P., Ban K.M., Bartoloni A., Fowler K.E., Saint S., Mannelli F. Assessing the sustainability of hand hygiene adherence prior to patient contact in the emergency department: a 1-year postintervention evaluation. Am J Infect Control. 2011;39:14–18. doi: 10.1016/j.ajic.2010.06.015. [DOI] [PubMed] [Google Scholar]
- 22.Bukhari S.Z., Hussain W.M., Banjar A., Almaimani W.H., Karima T.M., Fatani M.I. Hand hygiene compliance rate among healthcare professionals. Saudi Med J. 2011;32:515–519. [PubMed] [Google Scholar]
- 23.Fakih M.G., Shemes S.P., Pena M.E., Dyc N., Rey J.E., Szpunar S.M. Urinary catheters in the emergency department: very elderly women are at high risk for unnecessary utilization. Am J Infect Control. 2010;38:683–688. doi: 10.1016/j.ajic.2010.04.219. [DOI] [PubMed] [Google Scholar]
- 24.Gokula R.M., Smith M.A., Hickner J. Emergency room staff education and use of a urinary catheter indication sheet improves appropriate use of foley catheters. Am J Infect Control. 2007;35:589–593. doi: 10.1016/j.ajic.2006.12.004. [DOI] [PubMed] [Google Scholar]
- 25.Fakih M.G., Pena M.E., Shemes S., Rey J., Berriel-Cass D., Szpunar S.M. Effect of establishing guidelines on appropriate urinary catheter placement. Acad Emerg Med. 2010;17:337–340. doi: 10.1111/j.1553-2712.2009.00677.x. [DOI] [PubMed] [Google Scholar]
- 26.Dyc N.G., Pena M.E., Shemes S.P., Rey J.E., Szpunar S.M., Fakih M.G. The effect of resident peer-to-peer education on compliance with urinary catheter placement indications in the emergency department. Postgrad Med J. 2011;87:814–818. doi: 10.1136/postgradmedj-2011-130287. [DOI] [PubMed] [Google Scholar]
- 27.Xiao Y., Seagull F.J., Bochicchio G.V., Guzzo J.L., Dutton R.P., Sisley A. Video-based training increases sterile-technique compliance during central venous catheter insertion. Crit Care Med. 2007;35:1302–1306. doi: 10.1097/01.CCM.0000263457.81998.27. [DOI] [PubMed] [Google Scholar]
- 28.Guzzo J.L., Seagull F.J., Bochicchio G.V., Sisley A., Mackenzie C.F., Dutton R.P. Mentors decrease compliance with best sterile practices during central venous catheter placement in the trauma resuscitation unit. Surg Infect. 2006;7:15–20. doi: 10.1089/sur.2006.7.15. [DOI] [PubMed] [Google Scholar]
- 29.Nagashima G., Kikuchi T., Tsuyuzaki H., Kawano R., Tanaka H., Nemoto H. To reduce catheter-related bloodstream infections: is the subclavian route better than the jugular route for central venous catheterization? J Infect Chemother. 2006;12:363–365. doi: 10.1007/s10156-006-0471-x. [DOI] [PubMed] [Google Scholar]
- 30.LeMaster C.H., Schuur J.D., Pandya D., Pallin D.J., Silvia J., Yokoe D. Infection and natural history of emergency department-placed central venous catheters. Ann Emerg Med. 2010;56:492–497. doi: 10.1016/j.annemergmed.2010.05.033. [DOI] [PubMed] [Google Scholar]
- 31.Diaz K., Kelly S.G., Smith B., Malani P.N., Younger J.G. A prospective study of central venous catheters placed in a tertiary care emergency department: indications for use, infectious complications, and natural history. Am J Infect Control. 2012;40:65–67. doi: 10.1016/j.ajic.2011.03.018. [DOI] [PubMed] [Google Scholar]
- 32.Trick W.E., Miranda J., Evans A.T., Charles-Damte M., Reilly B.M., Clarke P. Prospective cohort study of central venous catheters among internal medicine ward patients. Am J Infect Control. 2006;34:636–641. doi: 10.1016/j.ajic.2006.02.008. [DOI] [PubMed] [Google Scholar]
- 33.Gowardman J.R., Robertson I.K., Parkes S., Rickard C.M. Influence of insertion site on central venous catheter colonization and bloodstream infection rates. Intensive Care Med. 2008;34:1038–1045. doi: 10.1007/s00134-008-1046-3. [DOI] [PubMed] [Google Scholar]
- 34.Otter J.A., Passaretti C.L., French G.L., Ross T., Carroll K.C., Perl T.M. Low frequency of environmental contamination with methicillin-resistant Staphylococcus aureus in an inner city emergency department and a human immunodeficiency virus outpatient clinic. Am J Infect Control. 2011;39:151–153. doi: 10.1016/j.ajic.2010.05.022. [DOI] [PubMed] [Google Scholar]
- 35.Gray J., McNicholl B., Webb H., Hogg G. Mice in the emergency department: vector for infection or technological aid? Euro J Emerg Med. 2007;14:160–162. doi: 10.1097/MEJ.0b013e3280bef922. [DOI] [PubMed] [Google Scholar]
- 36.Frazee B.W., Fahimi J., Lambert L., Nagdev A. Emergency department ultrasonographic probe contamination and experimental model of probe disinfection. Ann Emerg Med. 2011;58:56–63. doi: 10.1016/j.annemergmed.2010.12.015. [DOI] [PubMed] [Google Scholar]
- 37.Tang P.H., Worster A., Srigley J.A., Main C.L. Examination of staphylococcal stethoscope contamination in the emergency department (pilot) study (EXSSCITED pilot study) CJEM. 2011;13:239–244. doi: 10.2310/8000.2011.110242. [DOI] [PubMed] [Google Scholar]
- 38.Boyce J.M. Measuring healthcare worker hand hygiene activity: current practices and emerging technologies. Infect Control Hosp Epidemiol. 2011;32:1016–1028. doi: 10.1086/662015. [DOI] [PubMed] [Google Scholar]
- 39.Conway L.J., Larson E.L. Guidelines to prevent catheter-associated urinary tract infection: 1980 to 2010. Heart Lung. 2012;41:271–283. doi: 10.1016/j.hrtlng.2011.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Conway L.J., Pogorzelska M., Larson E., Stone P.W. Adoption of policies to prevent catheter-associated urinary tract infections in United States intensive care units. Am J Infect Control. 2012;40:705–710. doi: 10.1016/j.ajic.2011.09.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Andreessen L., Wilde M.H., Herendeen P. Preventing catheter-associated urinary tract infections in acute care: the bundle approach. J Nurs Care Qual. 2012;27:209–217. doi: 10.1097/NCQ.0b013e318248b0b1. [DOI] [PubMed] [Google Scholar]
- 42.Meddings J., Rogers M.A., Macy M., Saint S. Systematic review and meta-analysis: reminder systems to reduce catheter-associated urinary tract infections and urinary catheter use in hospitalized patients. Clin Infect Dis. 2010;51:550–560. doi: 10.1086/655133. [DOI] [PubMed] [Google Scholar]
- 43.Rothfeld A.F., Stickley A. A program to limit urinary catheter use at an acute care hospital. Am J Infect Control. 2010;38:568–571. doi: 10.1016/j.ajic.2009.12.017. [DOI] [PubMed] [Google Scholar]