Abstract
Background
Bipolar disorder has a high co-occurrence with substance abuse disorders, but the pathophysiological mechanisms have not been adequately explored.
Aims
Review the role of stress in the onset and recurrence of affective episodes and substance abuse.
Method
We review the mechanisms involved in sensitization (increased responsivity) to recurrence of stressors, mood episodes, and cocaine use.
Results
Evidence suggests that intermittent stressors, mood episodes, and bouts of cocaine use not only show sensitization to themselves, but cross sensitization to the others contributing to illness progression. However, common mechanisms of sensitization, (such as regionally selective alterations in brain derived neurotrophic factor (BDNF) and hyperactivity of striatally-based habit memories), could also result in single therapies (such as N-acetylcysteine) having positive effects in all 3 domains.
Conclusions
These interacting sensitization processes suggest the importance of early intervention in attempting to prevent increasingly severe manifestations of bipolar illness and substance abuse progression.
Bipolar disorder is accompanied by multiple comorbidities, but substance abuse is particularly common (1), and its co-occurrence often leads to a more pernicious and difficult to treat course of illness. Genetic and family studies also suggested a considerable overlap and interaction of the two disorders suggest that early onset bipolar disorder and substance abuse disorder share at least some common genetic vulnerabilities (2). Those with early onset bipolar disorder are also more prone to substance abuse disorders than those with adult onsets (3).
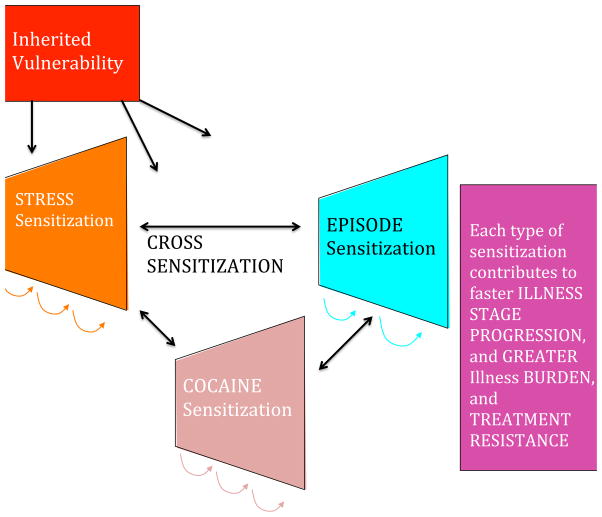
In this manuscript we focus on the role of stressors in the initiation of both bipolar disorder and substance abuse, as well as their role in precipitating mood episode recurrence and addiction reinstatement. Behavioral sensitization (increased behavioral responsivity) also occurs to the repeated occurrence of 1) stressors, 2) psychomotor stimulants, and 3) episodes of bipolar disorder, as well as cross-sensitization among each of these that may further drive illness progression. While we focus on bipolar disorder, much of the discussion is equally relevant to recurrent unipolar depression (4).
Stressors as Precipitants of Affective Illness Substance Abuse Onset, and Recurrence
A very robust clinical and preclinical literature indicates that experience of early life adversity and stressors is a strong risk factor for animals and humans subsequently adopting drug self-administration and addiction (5). This is best demonstrated for psychomotor stimulants, but also is seen with other drugs including opiates and alcohol (6). In a parallel fashion, stressors are also involved in the precipitation of initial episodes of the recurrent unipolar and bipolar mood disorders (5). Those with a history of early severe psychosocial adversity experience a more severe and treatment-refractory course of bipolar disorder and have an increased incidence of substance abuse (5).
In animal studies, a history of early stressful life experiences can lead to increased stressor responsivity to stressors in adulthood (stress sensitization). There is considerable evidence for similar phenomena in humans. In the classic study of Caspi et al. (7), only those individuals who had multiple early life stressors were vulnerable to the occurrence of depression following stressors in adulthood, and this also varied as a function of the type of serotonin transporter that one inherited. In addition, repeated defeat stress in adult animals sensitizes to cocaine, and cocaine sensitization increases the susceptibility to social defeat stress (8).
In those with the recurrent unipolar and bipolar mood disorders, stressors also appear to be involved in the relapse and recurrence of new episodes (5), as well as the relapse into substance abuse in those who have been abstinent (9). New mood episodes can, in turn, result in renewed drug use. As predicted in the sensitization model of affective disorders, stressors are more likely to be involved in the precipitation of initial episodes and less successively crucial for the occurrence of episodes later in the course of illness which can also begin to occur more autonomously (5). Thus, there appears to be the potential for a vicious cycle in which stressors, episodes, and substances of abuse can each increase vulnerability to the recurrence and magnitude of responsivity to the others. (Figure 1).
Figure 1.
Episode Sensitization and Increased Vulnerability to Recurrence
Emil Kraepelin described the tendency for episodes to occur more readily and with a shorter well-interval between successive episodes. The strongest modern supporting data are those from the Danish case registry showing that vulnerability and latency to relapse vary directly as a function of number of prior hospitalizations for either unipolar or bipolar depression (10).
Stimulant-Induced Behavioral Sensitization
Repeated intermittent administration of psychomotor stimulants (amphetamine, cocaine, and methylphenidate) results in increasing motor hyperactivity and stereotypy rather than a tolerance pattern of adaptation and decreased behavioral response (5, 9). Conditioned responses and an environmental context-dependency to the behavioral sensitization is also apparent (5). This sensitized increased magnitude of response is most readily seen if cocaine is repeatedly administered in the same environmental context, but not when the animal is tested in a dissimilar environmental context. We focus the discussion here on the psychomotor stimulant cocaine, but data also supports similar sensitization effects to amphetamine and methylphenidate, and some components of opiate and phenocypidone (PCP) can also sensitize, as can repeated bouts of alcohol withdrawal.
Animals that are taught to self-administer cocaine by pressing a bar to have the drug delivered intravenously are difficult to extinguish from this habit (9). While animals will eventually stop bar pressing if cocaine is no longer delivered, they will rapidly reinstate bar pressing if a stressor or cues that cocaine is again available are presented. This animal model of cocaine reinstatement mirrors that in the clinical condition, in which stresses and episodes of mood dysfunction are also known to be precipitants of relapse to cocaine self-administration, even in humans who have been abstinent for long periods of time (9). Depression and associated dysphoric affect are known precipitants of substance abuse relapse, as are the search for excitement and the poor judgment of mania (9).
Chronic cocaine not only induces a variety of long-term biochemical and physiological effects, but also induces changes in the shape of the dendritic spines on the medium spiny neurons containing the neurotransmitter GABA in the ventral striatum (nucleus accumbens). These GABA neurons receive converging input on these spines from terminades from the frontal cortex (glutamate) and the ventral tegmental area (dopamine) (9, 11).
The change in spine shape following chronic cocaine is accompanied by a loss of synaptic flexibility and regulation, in that long-term potentiation (LTP) and long-term depression (LTD), that are normally observed in the nucleus accumbens following high and low frequency stimulation of cortical neurons, no longer occur (11, 12). This deficit in plasticity occurs in concert with increases in BDNF in the ventral-tegmental area and nucleus accumbens and decreases in BDNF occur in the prefrontal cortex, and each of these changes are important to the manifestation of cocaine sensitization or reinstated cocaine-seeking. BDNF is co-secreted from glutamatergic neurons. It is crucial for synaptogenesis, the development of LTP and long-term memory (6).
Mechanistic Convergences in Animal Models and Human Depression
These observations of differential effects of cocaine on BDNF in different brain regions are of interest in relationship to similar observations occurring following repeated bouts of defeat stress in an animal model of depression, as well as in clinical depression. In this defeat stress model, intruder mice are repeatedly exposed to (but protected from lethal attack by) an aggressive rodent protecting his home cage territory. The intruder animal eventually develops depressive-like behaviors associated with BDNF decrements in the hippocampus and increases in BDNF in the nucleus accumbens (13, 14). If either of the two alterations in BDNF levels is prevented by pharmacological or genetic manipulations, the defeat stress behaviors do not occur.
These regionally selective alterations in BDNF in this animal model of depression are mirrored by similar changes seen in depressed humans who have committed suicide, compared with non-depressed controls. BDNF decreases in the human hippocampus in suicide victims have been multiply replicated, and BDNF increases in the nucleus accumbens have been recently reported (15). Taken together, these observations suggest common effects of stressors, episodes of depression, and repeated stimulant administration in increasing BDNF in nucleus accumbens and decreasing it in hippocampus and prefrontal cortex.
If there are some mechanisms in common mediating the long-term biochemical and behavioral effects of stressors, episodes of depressive-like behaviors, and substances of abuse, these not only have the potentially unfortunate consequences of each exacerbating the others (fig. 1), but the potential for a single therapeutic manipulation in one domain dampening or reversing the increased vulnerability or hyper-responsiveness in the other domains as well. A current example of this is N-acetylcysteine. However, many other mechanisms may occur in common in response to repeated stressors, episodes, or stimulants as evidenced by prefrontal cortical hypofuction, glucocorticoid hypersecretion, and alteration in prefrontal dopamine, that could account for common deficits in executive functioning, and could also become therapeutic targets (16).
N-Acetylcysteine (NAC) Inhibits Cocaine and Gambling Addictions and Other Habits
In exploring the mechanisms of cocaine-induced behavioral sensitization, several groups have observed an increase in the number and diameter of spines on the dendrites of the medium spiny neurons of the nucleus accumbens, associated with a loss of LTP and LTD from prefrontal neurons and glutamate hypersecretion (11, 17).
Because many of the cocaine-induced neuroadaptations could be prevented by altering the disposition of extracellular glutamate, it was proposed that drugs restoring the function of glial proteins regulating extracellular glutamate might prove a means of reducing the vulnerability to relapse. N-acetylcysteine (NAC) acts at the glial cystine-glutamate exchanger in the accumbens to promote glutamatergic tone on extrasynaptic inhibitory metabotropic glutamate receptors, and thereby decreasing the hyperactive glutamate response to the environmental triggers of reinstated cocaine seeking (11, 12). Daily administration of NAC reversed the electrophysiological, morphological, and neurochemical changes in the nucleus accumbens produced by cocaine self-administration, and these reversals and decreased proneness for cocaine reinstatement endured for at least 3 weeks after discontinuing daily NAC (12).
Based on these preclinical studies, the findings were quickly translated into pilot clinical trials showing that NAC also decreased cocaine and gambling addiction proneness (18) (see Table 1). It also decreased other repetitive habits such as those in trichotillomania, OCD, and autism.
The striatum has been associated with processes of habit memory, which is automatic and unconscious, in contrast to conscious, declarative, or representational memory which involves structures of medial temporal lobe, including amygdala and hippocampus (19). The ventral striatum appears involved in memory pertaining to habits that have particular reward value such as substance administration, gambling proclivity, or perhaps even in the initial anxiety reduction occurring in the context of hair pulling in trichotillomania or repetitious behaviors in OCD.
Thus, the NAC reset of the hyper-responsive cued glutamate signal in the N. accumbens a key reward area of the brain may be a critical component to suppressing overlearned mechanisms in the habit-memory system of the striatum. This sensitized hyper-responsivity in the N. accumbens may then be further exacerbated by the inability of prefrontal cortex to exert its normal modulatory control over the accumbens and sensory-motor striatum (12, 18). This may have parallels in the clinic wherein patients are unable to make appropriate cortically-based risk/benefit evaluations of their behavior (16) and become dominated by processes in the unconscious habit memory system. This deficit may be further exacerbated by the finding that the degree of depression in affective ill and in cocaine-addicted individuals is correlated with the degree of decreased activity of prefrontal cortex, as revealed in PET scans (9).
N-acetylcysteine in Depression, A Relationship to Habit-Based Recurrences?
Based on an entirely different rationale of reducing oxidative stress, Mike Berk and colleagues (4) in Australia independently assessed the therapeutic effects of N-acetyl cysteine (NAC) in patients who were inadequately responsive to their therapeutic regimens for bipolar disorder. They found that NAC compared with placebo exerted remarkably beneficial effects, particularly on depression, after a period of three months, and these effects were lost following NAC discontinuation at six months. Acute antidepressant effects have also been observed in unipolar depression. Berk postulated that NAC might be exerting these therapeutic effects because of its antioxidant effects and its glutathione precursor properties. However, it is also possible that some of the glutamatergic mechanisms in the nucleus accumbens and prefrontal cortical involved in an overactive habit system, described above in the cocaine reinstatement paradigm, could be involved as well.
In the experience of the stress sensitization in the defeat paradigm, intruder animals are repeatedly subjected to the imminent threat and cues of an aggressive home cage animal intent on maiming it, eventually leading to the manifestation of depressive-like behaviors. A similar conversion to a habit-based process could also be occurring following multiple experience of episodes of depression. While the initial episodes of clinical depression are often precipitated by psychosocial stressors (5), following many depressive recurrences, episodes can also occur more autonomously, and these depressions might increasingly engage the more unconscious and automatic mechanisms of the habit memory system. At this stage of illness evolution, one would hypothesize that effective psycho-therapeutic maneuvers might require targeting the striatal habit memory system, such as the repeated work and practice involved in cognitive/behavioral techniques that have been shown to be effective in unipolar and bipolar depression. Alternatively, work within the reconsolidation window (lasting 5 minutes to 1 hour) after recall of long-term memories may also be effective in substance abuse and mood disorders (20).
To the extent that NAC is helping to reprogram and dampen pathological or overlearned habit memories based in the nucleus accumbens reward and punishment system based on hyperreactive glutamate signaling and associated changes in BDNF, it is possible that this action could also account for the therapeutic effects of NAC in depressive recurrences, as well as in substance abuse.
In accord with this possibility, enhancing glutamate clearance from the synaptic space by increasing glial glutamate transporters in the n. accumbens was also sufficient to decrease cocaine reinstatement behaviors and reverse some of the behavioral, biochemical, and physiological effects of cocaine sensitization (6). Such findings would be consistent with the clinical data that glial numbers and glial activity are reported deficient in autopsy studies of patients with mood disorders compared to controls (at least in cortex), further suggesting the potential benefits of targeting glial deficits in the domains of episode and stress sensitization. This suggestion converges with the finding that glial, but not neural, toxins are capable of inducing depressive-like behaviors in several animal models.
The Epigenetic Connection of BDNF to Stress, Substance Use, and Depression
These environmentally-induced effects of repeated defeat stress and cocaine on biochemistry and behavior that persist for indefinitely long periods of time could be mediated by acute alterations in transcription factors activating or repressing gene sequences in DNA to induce new proteins, neurotrophic factors and long-term changes in synaptic excitability (5).
However, additional neurobiological mechanisms for inducing such long-lasting changes in “epigenetic’ regulation of gene transcription induced by events in the environment have recently been elucidated. Epigenetic regulation involves environmentally-induced changes in DNA and methylation and histone acetylation and methylation that facilitates or reduces DNA transcription (14). Typically, DNA methylation is repressive, while acetylation of histones (around which the DNA is tightly wrapped) renders DNA less tightly wrapped and, therefore, more easily activated or transcribed. This process has been termed “epigenetics” or “above genetics” because it does not change the inherited nucleotide or gene sequences conveying vulnerability to certain traits and diseases. Since these methyl, acetyl, and other small chemical marks tend to be long-lasting, both genetic (inherited) and epigenetic (environmental) effects could contribute to long-term pathological and adaptive biochemical and behavioral changes conveying sustained increases in illness vulnerability (5, 21).
In the defeat stress paradigm in adult animals, the decrements in hippocampal BDNF are caused by a repressive epigenetic mechanism involving trimethylation of histone H3K27 (22). If antidepressants are given which increase hippocampal BDNF and reverse the defeat stress behaviors, it is most interesting that the trimethylation of H3K27 is not reversed. This suggests that the antidepressants increase BDNF through other mechanisms and leave the initial defeat stress-induced epigenetic marks in place. Lifelong persistence of the epigenetic marks related to stressors early in life is likely a mechanism for increased reactivity of animals and humans to subsequent stressors later in life (7, 21).
While such persistence of epigenetic marks suggests that they might convey relatively permanent alterations in reactivity and vulnerability, drugs are now being explored that directly alter these epigenetic marks. These include DNA methyl transferase facilitators and inhibitors, histone deacetylases and an entire group of drugs known as histone-de-acetylase inhibitors, one of which is valproic acid (Depakote) (23).
Roth et al. (21) also found that rodent neonates subject to poor mothering experiences exhibit life-long decrements in BDNF in prefrontal cortex, based on increases in DNA methylation of the BDNF promoter. If these animals are given zebularine, an inhibitor of DNA methylation, the BDNF decrements in the cortex and associated behaviors do not occur. Interestingly DNA methylation is also involved in cocaine-induced behavioral sensitization in mice, and the sensitized response is again blocked by the methylation inhibitor zebularine.
When animals are subjected to early repeated, prolonged (3 hour but not 15 minute) maternal separation, they develop life-long increases corticosterone and anxiety behaviors, in part based on deficient expression of the glucocorticoid receptor based on methylation of its DNA promotor. Parallel findings occur in humans in those who committed suicide and had had a history of physical or sexual abuse in childhood; they had an increase in glucocorticoid receptor methylation compared with those without these early stressors (24)
CLINICAL IMPLICATIONS
The long-term consequences of increased reactivity (sensitization) to recurrent stressors, episodes, and substances of abuse and their cross-sensitization to each other have a number of important implications for clinical therapeutics. To the extent that each of these processes is environmentally mediated, it is amenable to current efforts at reducing or preventing their occurrence and the consequent long-term adverse effects on behavior. The long-term persistence of the sensitization effects and many of their epigenetic mechanisms makes it all that more important to consider the early and consistent initiation of long-term prophylactic treatment in bipolar disorder in an effort to avoid illness progression by the further recurrence of new episodes, the accumulation of stressors, and the all-too-common acquisition of substance abuse comorbidities.
In the recurrent unipolar and bipolar disorders, there appears to be not only a more adverse course of illness in those with childhood onset compared with adult onset illness (such as more episodes, substance use, and disability) (3, 5), but long delays to first treatment that are inversely correlated with age of onset of illness (25). This delay to first treatment for mania or depression in bipolar disorder is independently correlated with a more adverse outcome in adulthood as seen by more time and more severity of depression, less time euthymic, and the experience of more episodes in prospectively rated adults.
Thus, it would appear imperative to begin to address recurrent mood disorders from the perspective of the potential of the progressive and sensitization effects of accumulating mood episodes with their potential for cross-sensitization to stressors and substances of abuse, in order to refocus efforts at earlier and more effective long-term prophylactic strategies. The potential cross-sensitization among stressors, episodes, and substances of abuse raises the specter of an adverse positive feedback mechanism in each domain of illness vulnerability, with recurrences of each not only increasing responsivity to themselves, but also to the others (fig 1). The potential liabilities of this process may be particularly relevant to persons with bipolar illness living in the U.S (25, 26). Compared to patients from Germany and the Netherlands, those from the U.S. experience: 1) more stressors not only in childhood, but in the year prior to illness onset, and prior to the last episode; 2) more substance abuse comorbidity; as well as 3) more episodes, and more rapid cycling (4 or more episodes/year). Each of these could engage sensitization mechanisms and propel illness progression, which is further confirmed by findings of increased treatment refractoriness in those from the U.S. compared with Germany and the Netherlands (26). Thus, the convergence of more stressors, episodes, and substance use in the U.S. may lead to greater accumulation of epigenetically-based vulnerability and severity of illness progression than in some European countries.
The partially converging mechanisms discussed in this manuscript also yield a new perspective on the frequent co-occurrence of substance abuse comorbidities in the affective disorders and the linkage of childhood stressors to early onset and more rapid cycling illness, as well as the adoption of substance use and abuse. Thus, it appears more than mere coincidence that there is a high incidence of substance abuse comorbidities in the recurrent affective disorders and that stressors play etiopathological roles in the onset and relapse of both syndromes.
While the substance abuse comorbidities vastly complicate the course and treatment of recurrent affective illness, we hope that the clinical and theoretical exposition of some convergent pathways illustrated in this manuscript (such as changes in BDNF, cued-glutamate reactivity in the N. Accumbens, possibly engaging habit memory systems) also offer a hopeful perspective about prevention as well as new modes of therapeutic intervention, such as with N-acetylcysteine currently and perhaps epigenetics in the future. While awaiting such future possibilities to arrive, this overview suggests the importance of employing available clinical strategies and public health measures. These might include reconfiguring efforts aimed at more frequent and consistent long-term prophylaxis, employing stress immunization and coping techniques, and initiating primary prophylaxis of substance abuse in the youth with bipolar disorders who have not yet started abusing drugs, but are at such high risk for doing so. Reductions in or prevention of any one of the domains of stress-, episode-, or substance abuse-sensitization is likely to yield therapeutic benefits in each of the other domains as well.
Footnotes
Dr. Robert Post reports no financial conflict of interest pertinent to this manuscript.
Dr. Peter Kalivas reports no competing interests.
References
- 1.Merikangas KR, Herrell R, Swendsen J, Rossler W, Ajdacic-Gross V, Angst J. Specificity of bipolar spectrum conditions in the comorbidity of mood and substance use disorders: results from the Zurich cohort study. Arch Gen Psychiatry. 2008;65(1):47–52. doi: 10.1001/archgenpsychiatry.2007.18. Epub 2008/01/09. [DOI] [PubMed] [Google Scholar]
- 2.Lin PI, McInnis MG, Potash JB, Willour V, MacKinnon DF, DePaulo JR, et al. Clinical correlates and familial aggregation of age at onset in bipolar disorder. The American journal of psychiatry. 2006;163(2):240–6. doi: 10.1176/appi.ajp.163.2.240. [DOI] [PubMed] [Google Scholar]
- 3.Perlis RH, Miyahara S, Marangell LB, Wisniewski SR, Ostacher M, DelBello MP, et al. Long-term implications of early onset in bipolar disorder: data from the first 1000 participants in the systematic treatment enhancement program for bipolar disorder (STEP-BD) Biological psychiatry. 2004;55(9):875–81. doi: 10.1016/j.biopsych.2004.01.022. Epub 2004/04/28. [DOI] [PubMed] [Google Scholar]
- 4.Berk M, Copolov DL, Dean O, Lu K, Jeavons S, Schapkaitz I, et al. N-acetyl cysteine for depressive symptoms in bipolar disorder--a double-blind randomized placebo-controlled trial. Biological psychiatry. 2008;64(6):468–75. doi: 10.1016/j.biopsych.2008.04.022. [DOI] [PubMed] [Google Scholar]
- 5.Post RM, Leverich GS. Treatment of Bipolar Illness: A Case Book for Clinicians and Patients. WW Norton, Inc; 2008. [Google Scholar]
- 6.Knackstedt LA, Melendez RI, Kalivas PW. Ceftriaxone restores glutamate homeostasis and prevents relapse to cocaine seeking. Biological psychiatry. 2010;67(1):81–4. doi: 10.1016/j.biopsych.2009.07.018. Epub 2009/09/01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Caspi A, Sugden K, Moffitt TE, Taylor A, Craig IW, Harrington H, et al. Influence of life stress on depression: moderation by a polymorphism in the 5-HTT gene. Science. 2003;301(5631):386–9. doi: 10.1126/science.1083968. Epub 2003/07/19. [DOI] [PubMed] [Google Scholar]
- 8.Covington HE, 3rd, Maze I, Sun H, Bomze HM, DeMaio KD, Wu EY, et al. A role for repressive histone methylation in cocaine-induced vulnerability to stress. Neuron. 2011;71(4):656–70. doi: 10.1016/j.neuron.2011.06.007. Epub 2011/08/27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kalivas PW, Volkow ND. The neural basis of addiction: a pathology of motivation and choice. The American journal of psychiatry. 2005;162(8):1403–13. doi: 10.1176/appi.ajp.162.8.1403. [DOI] [PubMed] [Google Scholar]
- 10.Kessing LV, Andersen PK. Predictive effects of previous episodes on the risk of recurrence in depressive and bipolar disorders. Current psychiatry reports. 2005;7(6):413–20. doi: 10.1007/s11920-005-0061-0. [DOI] [PubMed] [Google Scholar]
- 11.Moussawi K, Pacchioni A, Moran M, Olive MF, Gass JT, Lavin A, et al. N-Acetylcysteine reverses cocaine-induced metaplasticity. Nat Neurosci. 2009;12(2):182–9. doi: 10.1038/nn.2250. Epub 2009/01/13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Moussawi K, Zhou W, Shen H, Reichel CM, See RE, Carr DB, et al. Reversing cocaine-induced synaptic potentiation provides enduring protection from relapse. Proc Natl Acad Sci U S A. 2011;108(1):385–90. doi: 10.1073/pnas.1011265108. Epub 2010/12/22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Berton O, McClung CA, Dileone RJ, Krishnan V, Renthal W, Russo SJ, et al. Essential role of BDNF in the mesolimbic dopamine pathway in social defeat stress. Science. 2006;311(5762):864–8. doi: 10.1126/science.1120972. [DOI] [PubMed] [Google Scholar]
- 14.Tsankova NM, Berton O, Renthal W, Kumar A, Neve RL, Nestler EJ. Sustained hippocampal chromatin regulation in a mouse model of depression and antidepressant action. Nat Neurosci. 2006;9(4):519–25. doi: 10.1038/nn1659. [DOI] [PubMed] [Google Scholar]
- 15.Krishnan V, Berton O, Nestler E. The use of animal models in psychiatric research and treatment. The American journal of psychiatry. 2008;165(9):1109. doi: 10.1176/appi.ajp.2008.08071076. Epub 2008/09/04. [DOI] [PubMed] [Google Scholar]
- 16.Butts KA, Weinberg J, Young AH, Phillips AG. Glucocorticoid receptors in the prefrontal cortex regulate stress-evoked dopamine efflux and aspects of executive function. Proc Natl Acad Sci U S A. 2011;108(45):18459–64. doi: 10.1073/pnas.1111746108. Epub 2011/10/29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kalivas PW. The glutamate homeostasis hypothesis of addiction. Nature reviews Neuroscience. 2009;10(8):561–72. doi: 10.1038/nrn2515. Epub 2009/07/03. [DOI] [PubMed] [Google Scholar]
- 18.Olive MF, Cleva RM, Kalivas PW, Malcolm RJ. Glutamatergic medications for the treatment of drug and behavioral addictions. Pharmacol Biochem Behav. 2012;100(4):801–10. doi: 10.1016/j.pbb.2011.04.015. Epub 2011/05/04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mishkin M, Appenzeller T. The anatomy of memory. Scientific American. 1987;256(6):80–9. doi: 10.1038/scientificamerican0687-80. [DOI] [PubMed] [Google Scholar]
- 20.Xue YX, Luo YX, Wu P, Shi HS, Xue LF, Chen C, et al. A memory retrieval-extinction procedure to prevent drug craving and relapse. Science. 2012;336(6078):241–5. doi: 10.1126/science.1215070. Epub 2012/04/14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Roth TL, Lubin FD, Funk AJ, Sweatt JD. Lasting epigenetic influence of early-life adversity on the BDNF gene. Biological psychiatry. 2009;65(9):760–9. doi: 10.1016/j.biopsych.2008.11.028. Epub 2009/01/20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tsankova N, Renthal W, Kumar A, Nestler EJ. Epigenetic regulation in psychiatric disorders. Nature reviews. 2007;8(5):355–67. doi: 10.1038/nrn2132. [DOI] [PubMed] [Google Scholar]
- 23.Bredy TW, Wu H, Crego C, Zellhoefer J, Sun YE, Barad M. Histone modifications around individual BDNF gene promoters in prefrontal cortex are associated with extinction of conditioned fear. Learning & memory (Cold Spring Harbor, NY. 2007;14(4):268–76. doi: 10.1101/lm.500907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.McGowan PO, Sasaki A, D’Alessio AC, Dymov S, Labonte B, Szyf M, et al. Epigenetic regulation of the glucocorticoid receptor in human brain associates with childhood abuse. Nat Neurosci. 2009;12(3):342–8. doi: 10.1038/nn.2270. Epub 2009/02/24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Post RM, Leverich GS, Kupka RW, Keck PE, Jr, McElroy SL, Altshuler LL, et al. Early-onset bipolar disorder and treatment delay are risk factors for poor outcome in adulthood. The Journal of clinical psychiatry. 2010a;71(7):864–72. doi: 10.4088/JCP.08m04994yel. Epub 2010/07/30. [DOI] [PubMed] [Google Scholar]
- 26.Post RM, Leverich GS, Altshuler LL, Frye MA, Suppes T, Keck PE, et al. Differential clinical characteristics, medication usage, and treatment response of bipolar disorder in the US versus The Netherlands and Germany. Int Clin Psychopharmacol. 2011;26(2):96–106. doi: 10.1097/YIC.0b013e3283409419. Epub 2010/12/24. [DOI] [PubMed] [Google Scholar]