Abstract
Objective
To investigate the risk and injury severity on the regional body (head, neck, and chest) of obese children in frontal motor vehicle crashes.
Design and Methods
No physical surrogates (i.e., crash dummies) for obese children are available and experiments on pediatric cadavers are generally not feasible. Therefore, we developed computational models of obese children using medical imaging processing and state-of-the-art modeling techniques. A hybrid modeling technique was used to integrate finite element model for torso fat layer into the standard multibody model to represent various levels of obese children for 3- and 6-year-old age group. The models were used to investigate injury severity under various crash scenarios through model simulations.
Results
The head injury criterion and chest acceleration were observed to increase as body mass index (BMI) increased. Meanwhile, no such correlations were found between BMI and neck injury and chest deformation. Forward head and torso excursions were observed to increase as obesity increased, owing to the momentum effect of greater body mass.
Conclusions
Obese children appear to have greater risks of the head and chest injuries than do their non-obese counterparts in frontal motor vehicle crashes, owing to higher head and chest accelerations induced by greater body excursion.
Introduction
According to current definitions (1), individuals ages 2 to 18 years are determined to be overweight (≥ 85th and < 95th percentile [of prior population distributions]) or obese (≥ 95th percentile) based on US age- and sex-specific body mass index (BMI; kg/m2) charts updated by the Centers for Disease Control and Prevention (CDC) in 2000 (2). The prevalence of being obese among children has increased over the last several decades and is a major public health concern. A recent survey (3) indicated that 16.9% of children and adolescents in the US aged 2 to 19 years were at or above the 95th percentile.
Motor vehicle crashes (MVCs) are one of the leading causes of death and injury for children (4). Considerable efforts have been made to improve occupant safety for children. One of these efforts, child safety seats, are very effective in lessening serious injury or death in MVCs (5). Biomechanical studies using pediatric cadavers have been limited. Therefore, physical crash dummies representing average-sized children of certain ages (1-, 3-, and 6-year-olds) have been used in automotive crash safety assessments. Many studies have been conducted on injury prevention based solely on average-sized children and their surrogates. Whether current child protective and restraint systems optimized for average-sized children are also adequate for obese children remains an open question.
Obese children cannot fit properly in age-specific child safety seats (CSSs) and could, therefore, be at risk in standard CSSs (6, 7). Pollack et al. (8) investigated a relationship between BMI and injury risk in MVCs using a probability sample of children and concluded that although there was no overall increase in injury risk by BMI, overweight and obese children (34% of the 3,232 samples) were at an increased risk of lower and upper extremity injuries. The odds ratio of an injury severity score from moderate to untreatable was 2.64 for overweight and 2.54 for obese children. Similar conclusions were drawn by Zonfrillo et al. (9), who collected data pertaining to 9,327 children aged 3 to 8 involved in MVCs via insurance claims records and a telephone survey. Rana et al. (10), who reviewed 1,314 pediatric trauma cases, also found that the obese group (23% of the samples) had a higher incidence of extremity fracture but a lower incidence of head and abdominal injuries. No mechanistic study, however, has been performed for the injury risk, severity, and pattern of obese children involved in MVCs.
The objective of this study was to mechanistically investigate the risk and injury severity on regional body (head, neck, and chest) of obese children in MVCs. No physical surrogates (i.e., crash dummies) for obese children are available and experiments on pediatric cadavers are generally not feasible. Therefore, we used computational modeling and simulation methods and computational models of obese children were developed using state-of-the-art techniques. The models were used to investigate injury mechanism under a variety of frontal MVC scenarios through computer crash simulations. A hypothesis to be tested was that injury levels of obese children will be greater than those of non-obese counterparts.
Methods and Procedures
A modeling tool
In general, computational crash analyses are carried out using finite element or multibody models. The finite element method, which is currently the most popular computational method used in all engineering fields, provides a far more accurate representation of human anatomy and its properties than does the multibody method. In contrast, the multibody method is an attractive technique because of its capability to rapidly analyze complex kinematics of the human body with easy modeling.
Mathematical Dynamical Model (MADYMO) (TNO, The Netherlands), which employs a multibody method, is a powerful and widely used program for occupant kinematic analyses in MVCs. Validated MADYMO models using standard crash test dummies (i.e., 50th percentile male, 5th percentile female, and 1-, 3-, and 6-year-old child models) are routinely used in testing and development of vehicle safety systems (11, 12). Among the dummy models in MADYMO, Hybrid III 3- and 6-year-old ellipsoid dummies were used as standard (non-obese) models in this study. The weights of MADYMO standard dummies are 14.5 kg (95 cm height, BMI 16.0, 50th percentile) for the 3-year-old (3YO) and 23 kg (117 cm height, BMI 16.8, 80th percentile) for the 6-year-old (6YO). Finite element models of safety seats were developed, a toddler seat (for 3YO) and a booster seat (for 6YO), by the use of a 3-dimensional laser printing technique, Computer-Aided Design (CAD) software tool, finite element mesh generation, and government regulations (13, 14) followed by a validation study using computer simulation tools to ensure that the generic seat models are adequate. The properties of commonly used materials (e.g., impact copolymer polypropylene) were applied for the body of the seats (Elastic modulus of 1350 MPa).
Model validation
The MADYMO 3YO standard dummy model was seated on the toddler seat and constrained by the use of a five-point harness system. The toddler seat was then seated on rear seat and constrained by a three-point seatbelt. The seatbelt was modeled by finite elements and belt segments with webbing elongation setting to 10% at 10 kN force. A deceleration pulse obtained from a 48 km/h crash test (15) was applied to the dummy and toddler seat models. Similarly, the MADYMO 6YO standard dummy model was seated on the belt-positioning booster seat. A deceleration pulse obtained from a 56 km/h crash test (16) was applied to the dummy and booster seat models. The head and chest accelerations were measured to validate the models against the experimental data using anthropometric test dummies (15, 16). MADYMO version 7.3 was used for model simulations.
Modeling of obese dummies
The existing MADYMO Hybrid III 3YO and 6YO dummy models were modified to develop obese child models with a range of BMI levels. For this, computed tomography (CT) scan data of torso parts of 3YO and 6YO obese children were acquired from the Children’s of Alabama, Birmingham, Alabama with consent from the parents and approval from our Institutional Review Board. Among the acquired 22 sets of CT scan data, three data sets for each age were selected, which correspond to the 95th, 97th, and over 99th percentiles, in terms of BMI.
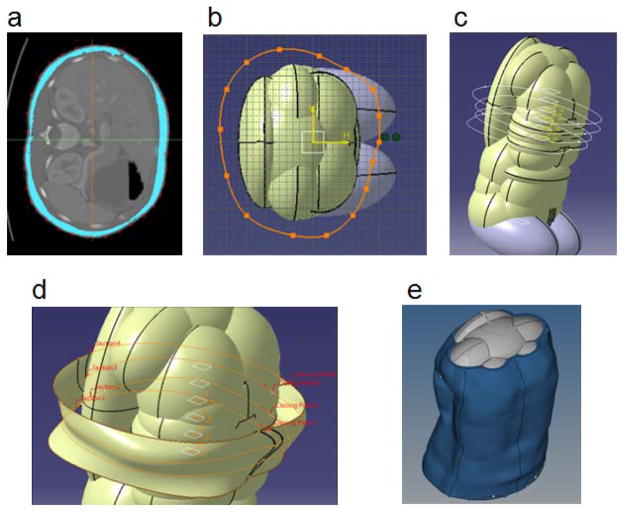
Two different modeling techniques were used to model obese children. The first one was to increase the inertial parameters (mass and moment of inertia) and sizes of body segments. This technique was used primarily for modifying the limbs. The second technique was to take account of subcutaneous adipose tissue (SAT) layers in the torso of obese children by a new layer of material that surrounds the chest and abdomen of the subjects. Finite element modeling was adopted to account for the complex geometry and soft tissue properties of the SAT layer. A sophisticated in-house mapping technique (17) was used to integrate the SAT into the dummy model. Several cross-sectional images of the SAT geometry from pelvis to chest were extracted from the CT scan data and thicknesses of the SAT were measured (Figure 1a). In the meantime, the outer surface of MADYMO torso was extracted. Several cross-sections of the outer surface at the same locations as the SAT geometry were also extracted. Based on the measured SAT thicknesses, a contour of the skin was then generated by spline curves at each cross-section to warrant equivalent sectional area of the SAT (Figure 1b). An artificial three-dimensional SAT geometry, referred to as ‘fat vest’ in this study, was then generated by connecting each section using an interpolation method (Figures 1c and 1d).
FIGURE 1.
Modeling process of obese dummy. (a) A slice of CT scan. (b) Mapping measured SAT thickness to the dummy. (c) Multiple contours of SAT thickness. (d) Interpolation of SAT layer. (e) Integration of ‘fat vest’ to the dummy.
HyperMesh version 11.0 (Altair Engineering, Troy, MI) was employed to create a finite element mesh for the fat vest by around 66,000 tetrahedral elements for the SAT and around 14,000 shell elements for the skin. Since shell elements are geometrically modeled in their mid plane, the contour of the skin was offset by half skin thickness for geometric fidelity. For the SAT, a hyperelastic model, the two-parameter Mooney-Rivlin constitutive model, was used with coefficients of 6.33 kPa and 1.58 kPa (18) and a density of 900 kg/m3 (19). For the skin, an isotropic elastic material model was used with a thickness of 2.0 mm (20), an elastic modulus of 635 kPa (21), a Poisson’s ratio of 0.45 (22), and a density of 1000 kg/m3 (23). Coincide nodes were used at the boundary of the SAT and skin. The finite element fat vest model was then integrated into the standard model to represent an obese model (Figure 1e). Consequentially, three models for obese 3YO children were developed, the 95th, 97th, and over 99th percentiles, on the basis of the age-specific BMI charts; which BMIs are 18.3, 18.8, and 19.5, respectively. Similarly, three models for obese 6YO children were developed, the 95th, 97th, and over 99th percentiles, on the basis of the age-specific BMI charts; which BMIs are 18.6, 19.5, and 20.4, respectively. Table 1 lists the body mass distributions for 3YO and 6YO on the basis of pediatric body segment and anthropometric parameters in the literature (24–27). Gender difference was not taken into account for the model development because it is not significant in young children.
Table 1.
Body mass distribution (kg)
| 3-year-old | 50th percentile | 95th percentile | 97th percentile | Over 99th percentile | References |
|---|---|---|---|---|---|
| Height (cm) | 95 | 95 | 95 | 95 | |
| Weight | 14.50 | 16.52 | 16.97 | 17.60 | |
|
| |||||
| BMI | 16.07 | 18.30 | 18.80 | 19.50 | 4 |
|
| |||||
| Head | 2.39 (16.5)a | 2.65 (16.0) | 2.68 (15.8) | 2.75 (15.7) | 24 |
| Trunk | 4.12 (28.4) | 4.72 (28.6) | 4.87 (28.7) | 5.07 (28.8) | 24, 25 |
| Pelvis | 2.62 (18.1) | 3.02 (18.3) | 3.11 (18.3) | 3.25 (18.5) | 24, 25 |
| Upper arms | 0.81 (5.6) | 0.93 (5.6) | 0.95 (5.6) | 0.99 (5.6) | 24 |
| Forearms | 0.64 (4.4) | 0.73 (4.4) | 0.75 (4.4) | 0.78 (4.4) | 24 |
| Hand | 0.23 (1.6) | 0.26 (1.6) | 0.27 (1.6) | 0.28 (1.6) | 24 |
| Thighs | 1.82 (12.5) | 2.07 (12.5) | 2.12 (12.5) | 2.21 (12.5) | 24, 26 |
| Shanks | 1.31 (9.0) | 1.52 (9.2) | 1.58 (9.3) | 1.66 (9.4) | 24, 26 |
| Feet | 0.57 (3.9) | 0.61 (3.7) | 0.62 (3.7) | 0.62 (3.5) | 24, 27 |
| Fat vest | 0.00 (0.0) | 1.45 (8.8) | 1.58 (9.3) | 1.75 (9.9) | |
|
| |||||
| Sum | 14.50 (100.0) | 16.52 (100.0) | 16.97 (100.0) | 17.60 (100.0) | |
| 6-year-old | 80th percentile | 95th percentile | 97th percentile | Over 99th percentile | References |
|---|---|---|---|---|---|
| Height (cm) | 117 | 117 | 117 | 117 | |
| Weight | 23.00 | 25.46 | 26.69 | 27.93 | |
|
| |||||
| BMI | 16.80 | 18.60 | 19.50 | 20.40 | 4 |
|
| |||||
| Head | 4.13 (18.0) | 4.32 (17.0) | 4.34 (16.3) | 4.36 (15.6) | 24 |
| Trunk | 6.03 (26.2) | 6.87 (27.0) | 7.34 (27.5) | 7.83 (28.0) | 24 |
| Pelvis | 5.03 (21.9) | 5.78 (22.7) | 6.21 (23.3) | 6.64 (23.8) | 24 |
| Upper arms | 0.87 (3.8) | 0.99 (3.9) | 1.05 (4.0) | 1.12 (4.0) | 24 |
| Forearms | 0.83 (3.6) | 0.92 (3.6) | 0.96 (3.6) | 1.01 (3.6) | 24 |
| Hands | 0.33 (1.4) | 0.34 (1.3) | 0.34 (1.3) | 0.34 (1.2) | 24 |
| Thighs | 2.29 (10.0) | 2.53 (10.0) | 2.66 (10.0) | 2.78 (10.0) | 24, 25 |
| Shanks | 2.76 (12.0) | 2.95 (11.6) | 3.02 (11.3) | 3.08 (11.0) | 24, 25 |
| Feet | 0.73 (3.2) | 0.77 (3.0) | 0.78 (2.9) | 0.79 (2.8) | 24, 26 |
| Fat vest | 0.00 (0.0) | 2.63 (10.3) | 3.22 (12.1) | 3.83 (13.7) | |
|
| |||||
| Sum | 23.00 (100.0) | 25.46 (100.0) | 26.69 (100.0) | 27.93 (100.0) | |
Values in parentheses are percentages (mass/total mass*100).
Frontal MVC simulations
Computational crash simulations were performed with the standard and developed obese models under a variety of frontal MVC scenarios. A baseline configuration (referred to as Case 1) is the following. A crash deceleration pulse from a full rigid frontal barrier impact (48 km/h) (28) was applied. The friction coefficients between the seatbelt and dummy, between the dummy and safety seats, and between the safety seats and rear seat were set to 0.25, 0.3, and 0.3, respectively. LATCH (Lower Anchors and Tethers for Children) is a restraint system that makes child safety seat installation easier using lower anchors and top tethers (28). This LATCH system was modeled and tested for 3YO dummies on the toddler seat. The seatbelt was equipped with pretensioner and load limiter for some cases with a maximum load limiter force of 4 kN. The load limiter was invented to reduce belt-related injuries (e.g., rib fractures, abdominal injuries) by spooling out the seatbelt webbing from the retractor when the belt loads reach a preset maximum force (29). Case studies were performed to consider the variations of restraint systems and crash pulses.
The test cases for 3YO are:
Case 2: 50% stiffened five-point harness property
Case 3: pretensioner/load limiter
Case 4: LATCH
Case 5: 50% stiffened five-point harness property and LATCH
Case 6: a higher crash pulse from a frontal impact of 56 km/h (30)
Case 7: 56 km/h pulse and 50% stiffened five-point harness property
Case 8: 56 km/h pulse and pretensioner/load limiter
Case 9: 56 km/h pulse and LATCH
Case 10: 56 km/h pulse and twice stiffened LATCH property
The test cases for 6YO are:
Case 2: pretensioner/load limiter
Case 3: a higher crash pulse from a frontal impact of 56 km/h (30)
Case 4: 56 km/h pulse and pretensioner/load limiter
Case 5: seatbelt elongation set to 10% at 7.5 kN
Case 6: friction coefficient between the seatbelt and dummy set to 0.4
Case 7: friction coefficient between the dummy and booster seat set to 0.5
Case 8: friction coefficient between the booster seat and rear seat set to 0.5
Case 9: elastic modulus of booster seat set to 825 MPa
Case 10: no booster seat and friction coefficient between the dummy and rear seat set to 0.3
From simulation results, the accelerations/decelerations, forces, moments, and deflections of the body components were measured and they were used to assess the following regional body injuries, proposed by NHTSA (National Highway Traffic Safety Administration) (31). The head injury criterion (HIC) is a measure of the likelihood of head injury based on acceleration ( a(t) ) at the center of gravity of the dummy’s head.
| (1) |
where t1 and t2 are the selected initial and final times of the interval so as to maximize HIC. The time interval is set to 15 milliseconds to calculate HIC15. The recommended limit of HIC15 is 570 for 3YO and 700 for 6YO. The neck injury criteria, called Nij, are critical limits for all four possible modes of neck loading: tension or compression ( FZ ) combined with either flexion or extension ( MY ).
| (2) |
The proposed critical intercept values for axial force ( Fint ) are 2120 N (tension and compression) for 3YO and 2800 N (tension and compression) for 6YO. The proposed critical intercept values for moment ( Mint ) are 68 N (flexion) and 27 N (extension) for 3YO, and 93 N (flexion) and 37 N (extension) for 6YO. The recommended limit of Nij is 1.0. The resultant chest acceleration (3 ms clip) and maximum chest deflection are used for thoracic injury criteria. The recommended limit of chest acceleration (3 ms clip) is 55 g (539.4 m/s2) for 3YO and 60 g (588.4 m/s2) for 6YO, and the recommended limits of chest deflection are 34 mm for 3YO and 40 mm for 6YO. The recommended limits and intercept values are from the NHTSA standards (31). The results from obese child dummies were compared to those from the standard dummy to examine the effect of childhood obesity on frontal MVC injuries.
Results
Results of model validation
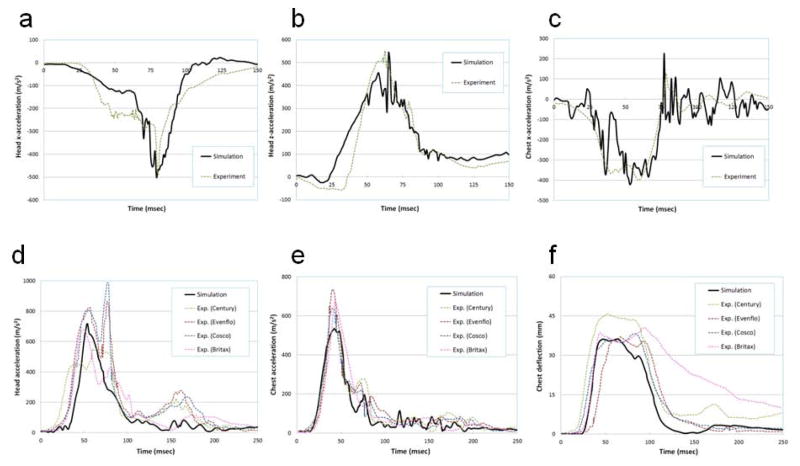
Figure 2 (a, b, and c) shows the comparisons of head and chest accelerations of 3YO between model simulation and anthropometric dummy test (15). The responses from the model simulation showed excellent agreement with the experimental data. The percent differences of maximum acceleration between the experimental data and simulation results were 2.2%, 2.1%, and 5.2% for the head x-direction (impact direction), head z-direction (vertical direction), and chest x-direction, respectively. Figure 2 (d, e, and f) shows the comparisons of head and chest accelerations and chest deflection of 6YO between the experimental data (16) and simulation results. The responses from the model simulation were kept within the corridors of the experimental data that were from the tests of four different booster seats. The percent differences of maximums between the means of experimental data and simulation results were 5.3%, 13.4%, and 7.6% for the resultant head and chest accelerations and chest deflection, respectively.
FIGURE 2.
Model validation. (a) 3YO head x-acceleration. (b) 3YO head z-acceleration. (c) 3YO chest x-acceleration. (d) 6YO resultant head acceleration. (e) 6YO resultant chest acceleration. (f) 6YO chest deflection.
Results of the case study
The HIC15, Nij, and maximum chest acceleration (CA) and deflection (CD) were measured for all cases and listed in Tables 2 and 3 for 3YO and 6YO, respectively. The values of injury measured were normalized by the recommended limits (31). Regarding the simulation results of 3YO, all injury measures were below the recommended limit. The change of harness property (Case 2) was observed to have a minor effect on the injury measures. The pretensioner/load limiter system (Case 3) effectively mitigated all injuries (average 14% decrease based on the Case 1, baseline model), especially chest deflection (27% decrease). The LATCH system (Case 4) also mitigated all injuries (average 8% decrease). The injury measures from the higher pulse of 56 km/h (Cases 6–10) were average 40% greater than those from the lower pulse of 48 km/h (Cases 1–5). Regarding the simulation results of 6YO, all injury measures were below the recommended limit, except the chest acceleration of obese subjects. The pretensioner/load limiter system (Case 2) still mitigated all injuries (average 8% decrease). The higher pulse (56 km/h, Case 3) increased average 27% of injuries. The variations of seatbelt property, friction coefficients, and booster property (Cases 5–9) were observed to have minor effects on the injury measures. No booster seat (Case 10) increased the injury measures on average 10%. The video files (Supporting Information) are the animated results of Case 6 of 3YO (S1) and Case 4 of 6YO (S2), in which the model indexes of standard, overweight, obese, and morbid obese are corresponding to the 50th/80th, 95th, 97th, and over 99th percentile models, respectively.
Table 2.
Injury measures of 3YO
| Injury | BMI | percentile | case 1 | case 2 | case 3 | case 4 | case 5 | case 6 | case 7 | case 8 | case 9 | case 10 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| HIC15a | 16.07 | 50th | 0.30 | 0.34 | 0.29 | 0.25 | 0.29 | 0.65 | 0.62 | 0.42 | 0.42 | 0.56 |
| 18.30 | 95th | 0.32 | 0.36 | 0.30 | 0.36 | 0.37 | 0.67 | 0.65 | 0.49 | 0.58 | 0.59 | |
| 18.80 | 97th | 0.34 | 0.35 | 0.31 | 0.35 | 0.35 | 0.70 | 0.65 | 0.53 | 0.60 | 0.60 | |
| 19.50 | over 99th | 0.42 | 0.40 | 0.38 | 0.37 | 0.43 | 0.78 | 0.79 | 0.52 | 0.62 | 0.59 | |
|
| ||||||||||||
| Nijb | 16.07 | 50th | 0.39 | 0.41 | 0.38 | 0.37 | 0.32 | 0.49 | 0.51 | 0.48 | 0.45 | 0.46 |
| 18.30 | 95th | 0.40 | 0.42 | 0.39 | 0.38 | 0.33 | 0.49 | 0.53 | 0.48 | 0.48 | 0.47 | |
| 18.80 | 97th | 0.41 | 0.45 | 0.39 | 0.37 | 0.35 | 0.49 | 0.50 | 0.50 | 0.50 | 0.48 | |
| 19.50 | over 99th | 0.42 | 0.40 | 0.39 | 0.38 | 0.38 | 0.51 | 0.50 | 0.48 | 0.46 | 0.46 | |
|
| ||||||||||||
| CAc | 16.07 | 50th | 0.38 | 0.39 | 0.36 | 0.34 | 0.38 | 0.50 | 0.45 | 0.46 | 0.47 | 0.45 |
| 18.30 | 95th | 0.40 | 0.41 | 0.37 | 0.35 | 0.39 | 0.49 | 0.48 | 0.47 | 0.50 | 0.46 | |
| 18.80 | 97th | 0.41 | 0.42 | 0.38 | 0.37 | 0.37 | 0.49 | 0.50 | 0.48 | 0.47 | 0.46 | |
| 19.50 | over 99th | 0.40 | 0.43 | 0.37 | 0.39 | 0.39 | 0.53 | 0.51 | 0.48 | 0.49 | 0.51 | |
|
| ||||||||||||
| CDd | 16.07 | 50th | 0.63 | 0.63 | 0.47 | 0.50 | 0.52 | 0.80 | 0.81 | 0.75 | 0.77 | 0.83 |
| 18.30 | 95th | 0.59 | 0.63 | 0.46 | 0.55 | 0.56 | 0.78 | 0.81 | 0.76 | 0.75 | 0.81 | |
| 18.80 | 97th | 0.67 | 0.63 | 0.47 | 0.60 | 0.52 | 0.75 | 0.77 | 0.72 | 0.76 | 0.81 | |
| 19.50 | over 99th | 0.67 | 0.65 | 0.48 | 0.60 | 0.53 | 0.77 | 0.79 | 0.72 | 0.78 | 0.81 | |
HIC15, Head injury criterion, normalized by 570
Nij, Neck injury criterion
CA, Chest acceleration, normalized by 55 g
CD, Chest deflection, normalized by 34 mm
Table 3.
Injury measures of 6YO
| Injury | BMI | percentile | case 1 | case 2 | case 3 | case 4 | case 5 | case 6 | case 7 | case 8 | case 9 | case 10 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| HIC15a | 16.80 | 80th | 0.34 | 0.31 | 0.67 | 0.38 | 0.36 | 0.35 | 0.34 | 0.37 | 0.33 | 0.40 |
| 18.60 | 95th | 0.35 | 0.30 | 0.68 | 0.43 | 0.40 | 0.39 | 0.33 | 0.37 | 0.33 | 0.47 | |
| 19.50 | 97th | 0.37 | 0.34 | 0.69 | 0.51 | 0.42 | 0.40 | 0.36 | 0.39 | 0.36 | 0.57 | |
| 20.40 | over 99th | 0.36 | 0.35 | 0.77 | 0.56 | 0.41 | 0.41 | 0.35 | 0.42 | 0.36 | 0.60 | |
|
| ||||||||||||
| Nijb | 16.80 | 80th | 0.80 | 0.73 | 0.96 | 0.78 | 0.76 | 0.80 | 0.79 | 0.75 | 0.82 | 0.87 |
| 18.60 | 95th | 0.73 | 0.74 | 0.94 | 0.79 | 0.81 | 0.83 | 0.74 | 0.77 | 0.79 | 0.90 | |
| 19.50 | 97th | 0.74 | 0.74 | 0.93 | 0.89 | 0.79 | 0.75 | 0.79 | 0.76 | 0.88 | 0.89 | |
| 20.40 | over 99th | 0.79 | 0.71 | 0.83 | 0.85 | 0.77 | 0.77 | 0.82 | 0.79 | 0.91 | 0.90 | |
|
| ||||||||||||
| CAc | 16.80 | 80th | 0.81 | 0.63 | 0.96 | 0.71 | 0.73 | 0.81 | 0.79 | 0.80 | 0.82 | 1.05 |
| 18.60 | 95th | 1.08 | 1.07 | 1.40 | 1.26 | 1.03 | 1.03 | 1.13 | 1.11 | 1.03 | 1.10 | |
| 19.50 | 97th | 1.10 | 1.09 | 1.44 | 1.33 | 1.12 | 1.14 | 1.25 | 1.13 | 1.23 | 1.19 | |
| 20.40 | over 99th | 1.25 | 1.15 | 1.45 | 1.38 | 1.24 | 1.16 | 1.19 | 1.37 | 1.27 | 1.17 | |
|
| ||||||||||||
| CDd | 16.80 | 80th | 0.72 | 0.62 | 0.78 | 0.74 | 0.68 | 0.68 | 0.70 | 0.70 | 0.66 | 0.65 |
| 18.60 | 95th | 0.71 | 0.62 | 0.76 | 0.70 | 0.67 | 0.64 | 0.69 | 0.70 | 0.64 | 0.64 | |
| 19.50 | 97th | 0.71 | 0.60 | 0.73 | 0.70 | 0.70 | 0.67 | 0.72 | 0.74 | 0.63 | 0.67 | |
| 20.40 | over 99th | 0.72 | 0.67 | 0.69 | 0.72 | 0.73 | 0.64 | 0.64 | 0.67 | 0.66 | 0.66 | |
HIC15, Head injury criterion, normalized by 700
Nij, Neck injury criterion
CA, Chest acceleration, normalized by 60 g
CD, Chest deflection, normalized by 40 mm
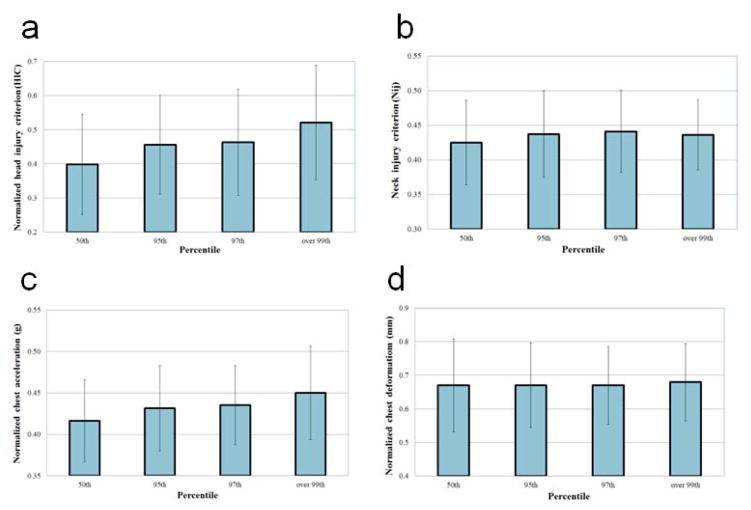
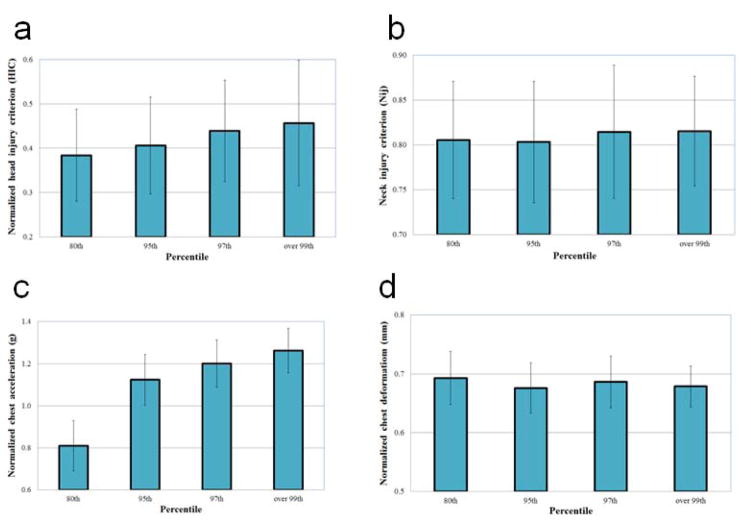
Figures 3 and 4 show the variations of each injury measure (HIC, Nij, CA, and CD) as BMI increases, indicating the mean values and ± standard deviations from the 10 cases for 3YO and 6YO, respectively. The observed large standard deviations were caused by the two different crash pulses (48 km/h and 56 km/h) tested in the case study that yielded significantly different body kinematics and injury measures.
FIGURE 3.
Means and ± standard deviations of each injury measure from the 10 cases for 3YO.
(a) HIC15. (b) Nij. (c) CA. (d) CD.
FIGURE 4.
Means and ± standard deviations of each injury measure from the 10 cases for 6YO.
(a) HIC15. (b) Nij. (c) CA. (d) CD.
Discussion
Since no obese child anthropometric test dummy or computational model exists and no cadaveric tests have been conducted, the injury severity and mechanism of obese children in MVCs are unknown. This study aimed at investigating the injury severity of regional body (head, neck, and chest) of obese children in frontal MVCs. Based on the standard (average-sized) dummies, three obese dummy models (95th, 97th, and over 99th percentile) were developed for each age group (3YO and 6YO), using a medical imaging processing and a hybrid modeling technique that integrated finite element model of torso fat layer into the standard multibody model. A hyperelastic material model with human adipose tissue properties was then assigned to the torso fat layer. The inertial parameters and sizes of body components were also increased in the obese models according to the pediatric body segment and anthropometric parameters.
As shown in Figures 3 and 4, no strong correlations were found between the Nij and BMI and between the CD and BMI, which may be the cause of a composition of the cushion effect (force attenuating effect) of torso fat layer and the momentum effect of greater body mass of obese children. Meanwhile, it is worth noting that the HIC15 and CA were observed to increase significantly as BMI increased. Both HIC15 and CA are acceleration-based injury measures, whereas Nij and CD are force- and deformation-based ones. Our previous study (17) that examined the injury severity sustained by overweight adult drivers in frontal MVCs found that there is a strong correlation between the acceleration-based injury measures and forward body excursion. To examine whether the same mechanism is valid for obese children, the body excursions (head, sternum and pelvis) were measured to evaluate the association between the levels of injuries and forward body excursions (Table 4). The body excursions were observed to increase as obesity increased, owing to the momentum effect of greater body mass, which is related to the increase of acceleration-related injury measures (i.e., HIC15 and CA) and is consistent with the finding from the previous study (17).
Table 4.
Average body excursions from the 10 cases (cm)
| Dummy | Body components | 3-year-old | 6-year-old |
|---|---|---|---|
| 50th/80th | Head | 27.1 | 21.0 |
| Sternum | 9.1 | 4.8 | |
| Pelvis | 7.7 | 5.3 | |
| 95th | Head | 28.7 | 21.7 |
| Sternum | 9.9 | 5.8 | |
| Pelvis | 7.9 | 6.6 | |
| 97th | Head | 29.6 | 22.6 |
| Sternum | 10.1 | 6.4 | |
| Pelvis | 8.0 | 7.3 | |
| Over 99th | Head | 31.3 | 23.3 |
| Sternum | 10.7 | 7.4 | |
| Pelvis | 8.3 | 9.1 |
The advanced seatbelt system with pretensioner and load limiter is common in front seats but far less common in rear seats in which younger children are seated. The tested pretensioner/load limiter seatbelt system effectively mitigated the levels of injuries (14% decrease for 3YO and 8% decrease for 6YO) by eliminating belt slack and then spooling out the belt to maintain the belt load within a predefined maximum force, which mitigated the levels of accelerations of body components. The LATCH system for 3YO also mitigated all injuries (average 8% decrease) by firmly restraining the toddler seat from rear seat using tethers and anchors, which reduced forward body excursions and consequently mitigated the acceleration-related injury measures. One study found that a LATCH system equipped with a load limiter significantly reduced HIC (32). Additional studies on advanced safety systems are warranted (e.g., body weight-sensitive load limiter and LATCH) to improve safety for children of various weights.
There are some limitations of this study. First, in terms of the head, neck, and chest injury severity sustained by obese children in MVCs, no experimental data exist to assess the findings of this study (to our knowledge). Instead, previous studies (8–10) found that obese children are at an increased risk of injury to the lower and upper extremities. This may be the cause of the momentum effect of greater body mass that would induce excessive forward body excursions in frontal MVCs, which is consistent with the findings of this study. Excessive body excursions would have a higher probability of excessive impact with vehicle components. Second, the effect of the variation of fat distribution within the same percentile and the variation of the height was beyond the scope of this study. Therefore, we did not modify the height of the dummies to effectively investigate the effect of the torso fat and body mass of the obese subjects on the crash injuries. Third, the Hybrid III ellipsoidal dummy models have inherent limitations to examine the details of injury mechanism due to lack of biofidelity. Child full body finite element models including details of anatomical features of neck and chest structures would be imperative to thoroughly examine neck and chest injuries. Such a model, however, is not currently available. Future efforts could go toward a more biofidelic model development and more case studies considering a variety of configurations to further validate our findings. Fourth, the recommended limits and intercept values for assessing injury criteria of standard (non-obese) children were used for obese children in this study due to lack of such data. Lastly, this study considered only frontal crashes.
In conclusion, obese children would have greater risks of the head and chest injuries than observed in non-obese counterparts in frontal MVCs, owing to higher head and chest accelerations induced by greater body excursion. A further implication is that a strategy (device, safety, and restraint system) will be needed to mitigate accelerations of body components to improve safety for obese children in MVCs.
Supplementary Material
What is already known about this subject?
Obese children are under suboptimal protection in motor vehicle crashes
Obese children are at an increased risk of injury to the lower and upper extremities in motor vehicle crashes
What does this study add?
This study proposed an efficient computational modeling technique to overcome barriers to research in pediatric injury biomechanics
Obese children appear to have greater risks of the head and chest injuries than do their non-obese counterparts in frontal motor vehicle crashes
The greater risks in obese children are caused by higher head and chest accelerations induced by greater forward body excursion
Acknowledgments
Funding: This project was supported by a grant from the Eunice Kennedy Shriver A of the National Institutes of Health (grant R21HD067784-01, Risk and Injury Severity of Obese Child Passengers in Motor Vehicle Crashes).
Footnotes
Disclosure: The authors have no conflict of interest in relation to the present study.
Role of the Sponsor: The funding organization had no role in the design and conduct of the study, in the collection, management, analysis, and interpretation of the data, or in the preparation, review, or approval of the manuscript.
References
- 1.Barlow SE the Expert Committee. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: Summary report. Pediatrics. 2007;120:5164–5192. doi: 10.1542/peds.2007-2329C. [DOI] [PubMed] [Google Scholar]
- 2.Kuczmarski RJ, Ogden CL, Guo SS, et al. CDC growth charts for the United States: methods and development. Vital Health Stat. 2000;11(246):1–190. [PubMed] [Google Scholar]
- 3.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999–2010. JAMA. 2012;307(5):483–490. doi: 10.1001/jama.2012.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Peden M, et al. World report on road traffic injury prevention: Summary. 2004. World Health Organization; Geneva: [Google Scholar]
- 5.National Highway Traffic Safety Administration (NHTSA) Traffic Safety Facts. 2005 Available at http://www-nrd.nhtsa.dot.gov/Pubs/809778.pdf.
- 6.Trifiletti LB, Shields W, Bishai D, McDonald E, Reynaud F, Gielen A. Tipping the scales: obese children and child safety seats. Pediatrics. 2006;117(4):1197–1202. doi: 10.1542/peds.2005-1379. [DOI] [PubMed] [Google Scholar]
- 7.Basco WT, Jr, Hletko PJ, West L, Darden PM. Determining the proportion of children too heavy for age appropriate car seats in a practice-based research network. Clinical Pediatrics. 2009;48:37–43. doi: 10.1177/0009922808321676. [DOI] [PubMed] [Google Scholar]
- 8.Pollack KM, Xie D, Arbogast KB, Durbin DR. Body mass index and injury risk among US children 9–15 years old in motor vehicle crashes. Injury Prevention. 2008;14(6):366–371. doi: 10.1136/ip.2008.019208. [DOI] [PubMed] [Google Scholar]
- 9.Zonfrillo MR, Nelson KA, Durbin DR, Kallan MJ. The association of weight percentile and motor vehicle crash injury among 3 to 8 year old children. Ann Adv Automot Med. 2010;54:193–199. [PMC free article] [PubMed] [Google Scholar]
- 10.Rana AR, Michalsky MP, Teich S, Groner JI, Caniano DA, Schuster DP. Childhood obesity: a risk factor for injuries observed at a level-1 trauma center. J Pediatr Surg. 2009;44(8):1601–1605. doi: 10.1016/j.jpedsurg.2008.11.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Van Rooij L, Sherwood CP, Crandall JR. A comparison of the injury risk for 12-month-old children in forward and rearward facing seats and the effect of a front-row seat. TNO MADYMO 5th Users’ Meeting of the Americas; 2003. [Google Scholar]
- 12.Menon R, Ghati Y, Jain P. MADYMO simulation study to optimize the seating angles and belt positioning of high back booster seats. 20th International Technical Conference on the Enhanced Safety of Vehicles (ESV); Lyon, France. 2007. [Google Scholar]
- 13.National transportation Safety Board (NTSB) Analysis. Safety Study NTSB/SS-96/01. Vol. 1. Washington, DC: 1996. The performance and use of child restraint systems, seatbelt, and air bags for children in passenger vehicles. [Google Scholar]
- 14.National Highway Traffic Safety Administration (NHTSA) Child passenger safety. 2005 Available at: http://www.nhtsa.gov/Laws+&+Regulations/Child+Passenger+Safety.
- 15.Kapoor T, Altenhof W, Wang Q, Howard A. Injury potential of a three-year-old Hybrid III dummy in forward and rearward facing positions under CMVSS 208 testing conditions. Accid Anal Prev. 2006;38(4):786–800. doi: 10.1016/j.aap.2006.02.005. [DOI] [PubMed] [Google Scholar]
- 16.Menon RA, Ghati YS, Roberts D. Proceedings of the 19th International Technical Conference on the Enhanced Safety of Vehicles. Paper Number 05-0366. National Highway Traffic Safety Administration; Washington, DC: 2005. Performance evaluation of various high back booster seats tested at 56 kph using a 6-year-old hybrid III dummy. [Google Scholar]
- 17.Kim JE, Kim IH, Shum PC, Shih AM, Pintar F, Shen W, Ma X, Laud PW, Heymsfield SB, Allison DB, Zhu S. A computational study of injury severity and pattern sustained by overweight drivers in frontal motor vehicle crashes. Comput Meth Biomech Biomed Eng. 2014;17(9):965–977. doi: 10.1080/10255842.2012.728589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Todd BA, Thacker JG. Three-dimensional computer model of the human buttocks in vivo. J Rehabil Res Dev. 1994;31(2):111–119. [PubMed] [Google Scholar]
- 19.Fidanza F, Keys A, Anderson JT. Density of body fat in man and other mammals. J Appl Physiol. 1953;6:252–256. doi: 10.1152/jappl.1953.6.4.252. [DOI] [PubMed] [Google Scholar]
- 20.Seidenari S, Giusti G, Bertoni L, Magnoni C, Pellacani G. Thickness and echogenicity of the skin in children as assessed by 20-MHz ultrasound. Dermatology. 2000;201(3):218–222. doi: 10.1159/000018491. [DOI] [PubMed] [Google Scholar]
- 21.Agache P, Monneur C, Leveque JL, De Rigal J. Mechanical properties and Young's modulus of human skin in vivo. Arch Derm Res. 1980;269:221–232. doi: 10.1007/BF00406415. [DOI] [PubMed] [Google Scholar]
- 22.Zheng Y, Mak AFT, Lue B. Objective assessment of limb tissue elasticity: Development of a manual indentation procedure. J Rehabil Res Dev. 1999;36(2):71–85. [PubMed] [Google Scholar]
- 23.Alekseev SI, Radzievsky AA, Logani MK, Ziskin MC. Millimeter wave dosimetry of human skin. Bioelectrom. 2008;29(1):65–70. doi: 10.1002/bem.20363. [DOI] [PubMed] [Google Scholar]
- 24.Yokoi T, Shibukawa K, Ae M. Body segment parameters of Japanese children. Jpn J Phys Educ. 1986;31:53–66. [Google Scholar]
- 25.Schwandt P, von Eckardstein A, Haas GM. Percentiles of Percentage Body Fat in German Children and Adolescents: An International Comparison. Int J Prev Med. 2012;3(12):846–852. doi: 10.4103/2008-7802.104855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bauer JJ, Pavol MJ, Snow CM, Hayes WC. MRI-derived body segment parameters of children differ from age-based estimates derived using photogrammetry. J Biomech. 2007;40:2904–2910. doi: 10.1016/j.jbiomech.2007.03.006. [DOI] [PubMed] [Google Scholar]
- 27.Ganley KJ, Powers CM. Anthropometric parameters in children: a comparison of values obtained from dual energy X-ray absorptiometry and cadaver-based estimates. Gait Posture. 2004;19:133–140. doi: 10.1016/S0966-6362(03)00038-9. [DOI] [PubMed] [Google Scholar]
- 28.National Highway Traffic Safety Administration (NHTSA) Proposed amendment to FMVSS No 213. Frontal test procedure. 2002 [Google Scholar]
- 29.National Highway Traffic Safety Administration (NHTSA) Effectiveness of pretensioners and load limiters for enhancing fatality reduction by seat belts. Report No. DOT HS 811 835. 2013 [Google Scholar]
- 30.Rouhana SW, Bedewi PG, Kankanala SV, Prasad P, Zwolinski JJ, Medufsky A, Rupp J, Jeffreys T, Schneider L. Biomechanics of 4-point seat belt systems in frontal impacts. Stapp Car Crash J. 2003;47:367–399. doi: 10.4271/2003-22-0017. [DOI] [PubMed] [Google Scholar]
- 31.Eppinger R, Sun E, Kuppa S, Saul R. Technical Report. U.S. Department of transportation; Washington, DC: 2000. Supplement: Development of improved injury criteria for the assessment of advanced automotive restraint systems - II, National Highway Traffic Safety Administration. [Google Scholar]
- 32.Kapoor T, Altenhof W, Tot M, Zhang W, Howard A, Rasico J, Zhu F, Mizuno K. Load limiting behavior in CRS tether anchors as a method to mitigate head and neck injuries sustained by children in frontal crash. Traffic Inj Prev. 2008;9(3):243–255. doi: 10.1080/15389580801975210. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.