Abstract
Objective
Lower socioeconomic status (SES) has been linked with higher obesity rates but not with weight gain. This study examined whether SES can predict short-term weight change.
Design and Methods
The Seattle Obesity Study II was based on an observational cohort of 440 adults. Weights and heights were measured at baseline and at 1 y. Self-reported education and incomes were obtained by questionnaire. Home addresses were linked to tax parcel property values from the King Co. tax assessor. Associations among SES variables, prevalent obesity, and 1 y weight change were examined using multivariable linear regressions.
Results
Low residential property values at tax parcel predicted prevalent obesity at baseline and at 1 y. Living in the top quartile of house prices reduced obesity risk by 80% at both time points. At 1 year, about 38% of the sample lost >1kg body weight; 32% maintained (± 1kg), and 30% gained >1kg. In adjusted models, none of the baseline SES measures had any impact on 1 y weight change.
Conclusions
SES variables, including tax parcel property values predicted prevalent obesity but did not predict short-term weight change. These findings, based on longitudinal cohort data, suggest other mechanisms are involved in short-term weight change.
Introduction
Prevalent obesity in the US is associated with lower socioeconomic status (SES), especially among women (1,2). However, the same social gradient has not been observed for body weight gain (3). All segments of the US population are reported to have experienced the same rise in obesity rates, regardless of age, gender, race/ethnicity, education, or incomes (2,4,5).
Whether some SES groups have had higher rates of incident obesity than others cannot be readily determined from US federal surveys. The National Health and Nutrition Examination Survey (NHANES) (2,6) and the Behavioral Risk Factors Surveillance System (BRFSS) (4,7) are cross-sectional studies that are only able to compare different socio-demographic groups at one point in time. To better assess the impact of SES variables on incident obesity or on short- or long-term weight gain, longitudinal cohorts are required (4).
However, longitudinal cohort studies on weight gain have produced inconsistent results. Some studies showed no significant links between SES variables and long-term weight gain (8,9), while others reported significant effects of SES (10-14). European studies, in particular, have noted that lower SES was associated with higher obesity rates and with greater weight gain among both children and adults (14-16). By contrast, US-based studies have reported only a limited impact of low SES on incident obesity and on body weight gain (17-19). The common consensus in the US is that disparities by income seem to be weakening with time (17).
Although cross-sectional studies have pointed to social disparities in obesity rates (20), they cannot prove that low SES is the direct cause of weight gain (21). Most of the published studies have relied, moreover, on self-reported SES, as indexed by education and incomes. The Seattle Obesity Study II (SOS II) was based on a well-characterized longitudinal cohort, with heights and weights measured over the period of 1 year. The present study is unique in multiple ways: a) it introduced tax parcel residential property values from the County tax assessor as an objective measure of SES (22); (b) it examined whether multiple measures of SES (both self-reported and objective) predict prevalent obesity, and longitudinal weight change using the same cohort.
Methods
Participant sampling and recruitment
The sample frame was established by selecting residential units from about 450,000 tax parcels (land lots) within King County Urban Growth Boundary (UGB). UGB refers to the urbanized area of King County and is used by the local government for zoning and land use decisions. Cadastral land parcels (tax lots) are used by local government to collect real estate taxes. The provision of urban services: roads, water, sewer, and fire and police services is limited by the UGB. Residential units in 3 bands of residential property values: <199K; >=200K-<299K; and >=300K were weighted to provide equal distributions by SES and were apportioned to correspond to the county distribution of 58% as single-family units and 42% as multifamily units. The property value cut offs were based on past results linking property values with income and health outcomes such as self-related health and obesity rates (21,23,24). The selected residential units were sent to a commercial supplier for reverse telephone matching of addresses with telephone numbers. The matching rate was 55% for single and 40% for multifamily categories. After eliminating duplicates and incomplete records, 25,460 addresses and phone numbers were provided to the Battelle Memorial Institute Survey Research Group for telephone screening of potential study participants.
Battelle mailed out pre-notification postcards to potential participants and followed with up to 3 telephone calls. Eligible participants were English speaking, aged 18-55y, were primary food shoppers in their household, and did not have mobility issues. Contact information for 712 potential eligible respondents who provided the verbal consent to participate was then provided by Battelle to SOS II research staff.
Data Collection
Eligible persons, identified by Battelle, were contacted by phone and were invited to an in-person meeting. Of the eligible participants, 516 (72.5%) agreed to enroll in the study. To minimize response bias and to allow participation by working mothers, single parents, and lower-income groups, respondents were given the choice of location for the first in person meeting: the UW location or another location of their choice, including at his/her home. About 56% of study participants (n=291) chose the latter option. At the first in-person visit, participants provided written consent before data collection and were then weighed and measured. Participants were compensated for completing all baseline protocols and for completing the second visit, 12 mo. later. The protocol was approved by the institutional review board (IRB) at the University of Washington.
Measured heights and weights
Height and weight was measured for each participant at baseline and at 1 y. Weight was measured in street clothes, without shoes, using a portable scale with a capacity of 350lbs. Two participants (out of 440) exceeded the 350 lb limit (the maximum limit allowed on the weighing scale); in these cases, participant self-reported weight was used instead. Height was measured using a portable stadiometer. Following past studies using weight change over the period of 1 year as the outcome of interest (25), small weight gain was defined as ≥1 kg to <2 kg, large weight gain was defined as ≥2 kg; small weight loss as ≤−1 kg to > −2 kg; large weight loss as ≤−2 kg; and weight maintenance as +/− 1 kg.
The Health Behaviors Survey (HBQ)
A computer-aided questionnaire was administered during the first in person visit. Data were collected on socio-demographics, self-rated health and weight, and a variety of dietary, food shopping, and health behaviors. Many of the questions were based on the Behavioral Risk Factors Surveillance System (BRFSS). Demographic variables included age, gender, race/ethnicity, household size, and home ownership. For analyses, annual household income was grouped into 3 categories: low (<$50,000/year), medium ($50,000 = <$100,000/year) and high (≥ $100,000/year). Educational attainment was also grouped into 3 categories: <12y (“high school or less”, 12-16y (“some college”), and >16y (“college graduates or higher”). Further questions addressed smoking: 72.8% of the sample never smoked; 25.3% were former smokers and only 2.0% were current smokers.
Follow Up at 1 year
After 11 mo, baseline participants were re-contacted by the same SOS II research staff member to schedule the follow up visit. Participants who did not become pregnant and who still lived in King Co. were followed after 1 year. Participants were again given the choice of either meeting at the UW research site or at a location convenient to them. Of the 516 baseline participants, 478 participants completed the 2nd appointment, a lower attrition rate than expected. Participants completed a follow up Health Behaviors Questionnaire (HBQ) and were weighed and measured for the second time. The follow-up HBQ asked participants if they had tried to lose weight over the previous year and if they had tried not to gain weight over the previous year. Data analyses were based on those participants for whom complete data at the two time points were available, including self-reported household incomes, property values, demographic and behavior data from both questionnaires, and measured heights and weights (n=440). Participants were compensated for completing all baseline protocols and for completing the second visit.
Residential property values
Data from King County tax assessor records for 2008 were used to develop the residential property value metric at the tax parcel level. When parcels had multiple units, the mean value per unit was used (21,23). The use of this method has been documented before (23).
Statistical Analysis
We calculated unadjusted proportions, means and standard deviations for prevalent obesity and longitudinal weight change variables, by key socio-demographic variables. P-values were computed to test for the overall statistical significance of the bivariate associations.
A series of linear and logistic regressions were used to examine the associations between SES measures, prevalent obesity, and weight change. Income, education and residential property values were used as the three primary independent variables. Prevalent obesity at baseline and at 1 year, and percent weight change over 1 year were each used as the dependent variables of interest. First, we fit three logistic regression models assessing the bivariate relationship between income, education and residential property values on prevalent obesity, after adjusting for age, gender and race/ethnicity. Second, we fit one regression model to evaluate if income and education were independently associated with prevalent obesity. The last and the final model further included residential property values to evaluate which of the three SES measures are independently associated with prevalent obesity. All results presented were calculated using robust standard errors. The same series of models were replicated for three other outcome measures: prevalent obesity at 1 year and percent weight change at 1 year. All analyses used Stata 10.1 (College Station, TX). An α level of 0.05 was used to define statistical significance.
RESULTS
Table 1 shows that prevalent obesity at baseline was strongly and inversely linked to the 3 SES measures: residential property values, education, and incomes. Similarly, prevalent obesity at 1 y was strongly and inversely linked to baseline residential property values, education, and incomes.
Table 1.
Characteristics of the SOS II population sample
| Total (n) |
Prevalent obese at baseline n (%) |
Prevalent obese at 1 y n (%) |
% weight change at 1 y (Mean±SD) |
|
|---|---|---|---|---|
| N (%) | 438 | 145 (33.1) | 133 (30.3) | −0.46 (4.53) |
| Gender | ||||
| Men | 136 | 43 (31.6) | 42 (30.8) | −0.28 (3.93) |
| Women | 302 | 102 (33.7) | 91 (30.1) | −0.54 (4.77) |
| p-value | 0.657 | 0.875 | 0.583 | |
| Age categories (years) | ||||
| 21-39 | 70 | 18 (25.7) | 14 (20.0) | −0.05 (3.92) |
| 40-49 | 198 | 63 (31.8) | 58 (29.2) | −0.24 (4.59) |
| ≥ 50 | 170 | 64 (37.6) | 61 (35.8) | −0.89 (4.67) |
| p-value | 0.064 | 0.015 | 0.128 | |
| Race/ethnicity | ||||
| Whites | 351 | 107 (30.4) | 101 (28.7) | −0.30 (4.62) |
| Non Whites | 87 | 38 (43.6) | 32 (36.7) | −1.12 (4.08) |
| p-value | 0.020 | 0.147 | 0.129 | |
| Annual household income | ||||
| <35,000 | 77 | 34 (44.1) | 31 (40.2) | −1.00 (5.35) |
| 35,000 - <50,000 | 51 | 21 (41.1) | 19 (37.2) | −0.27 (3.83) |
| ≥ 50,000 - < 100,000 | 157 | 53 (33.7) | 46 (29.3) | −0.63 (4.94) |
| ≥ 100,000 | 153 | 37 (24.1) | 37 (24.1) | −0.09 (3.80) |
| p-value | 0.001 | 0.007 | 0.200 | |
| Education | ||||
| High school or less | 46 | 24 (52.1) | 21 (45.6) | −0.42 (6.14) |
| Some college | 115 | 54 (46.9) | 52 (45.2) | −0.56 (5.26) |
| College 4 years | 154 | 43 (27.9) | 36 (23.3) | −0.39 (3.89) |
| College 5 years or more | 123 | 24 (19.5) | 24 (19.5) | −0.47 (3.83) |
| p-value | <0.0001 | <0.0001 | 0.935 | |
| Residential property value | ||||
| Category 1 (26,855 - 204K) | 110 | 51 (46.3) | 47 (42.7) | −0.61 (5.26) |
| Category 2 (205,650 - 268K) | 108 | 44 (40.7) | 37 (34.2) | 0.36 (3.85) |
| Category 3 (269K - 378K) | 111 | 36 (32.4) | 37 (33.3) | −1.02 (4.79) |
| Category 4 (379K - 914K) | 109 | 14 (12.8) | 12 (11.0) | −0.56 (3.99) |
| p-value | <0.0001 | <0.0001 | 0.525 |
No short-term weight gain (1y) was observed in this population sample; on the contrary, there was a minor short-term weight loss (mean 0.46% body weight). In bivariate analyses, percent weight change was unrelated to SES.
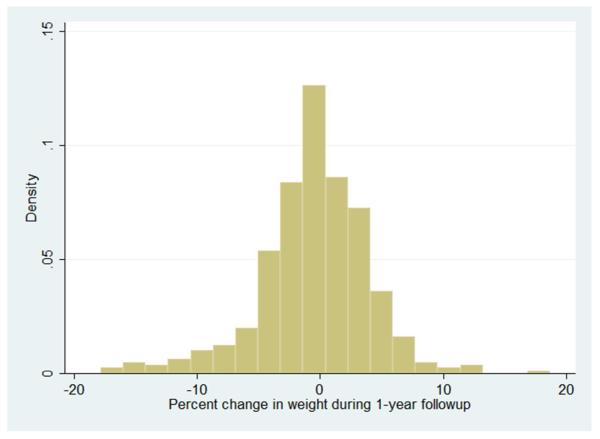
Figure 1 shows large weight changes occurring in the short term. About 38% of the study sample lost >1kg body weight, 32% maintained weight (± 1kg), and about 30% gained >1kg body weight. About 25% of the sample had a large weight loss of >2kg whereas 21% had a large weight gain of >2kg. When questioned about their weight behaviors over the previous year, 233 participants reported trying to lose weight, whereas 222 said they were not trying to lose weight. The majority of study participants reported trying not to gain weight over the previous year (291 yes; 165 no). The direction or the magnitude of 1 y weight change were not linked to residential property values.
Figure 1.
Distribution of weight change in the SOS II cohort over 1 year
As shown in Table 2, multivariable regressions explored the association between SES and prevalent obesity at baseline. In adjusted models, property values showed the strongest association with prevalent obesity, followed by education. Self-reported household income was no longer significance once property values were included in the model. Living in the highest quartile of house values was associated with an 80% drop in obesity rates.
Table 2.
Multivariate logistic regression to examine the association between prevalent obesity at baseline and key SES indicators
|
|
|
|
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | |||||||
| OR | 95% CI | p-value | OR | 95% CI | p-value | OR | 95% CI | p-value | |
|
|
|||||||||
| Annual household income | |||||||||
| <35,000 | 1 | 1 | 1 | ||||||
| 35,000 - <50,000 | 0.94 | 0.45, 1.95 | 0.877 | 1.16 | 0.55, 2.44 | 0.68 | 1.33 | 0.59, 2.97 | 0.482 |
| ≥ 50,000 - < 100,000 | 0.65 | 0.36, 1.15 | 0.141 | 0.88 | 0.48, 1.61 | 0.685 | 1.09 | 0.56, 2.11 | 0.797 |
| ≥ 100,000 | 0.40 | 0.22, 0.73 | 0.003 | 0.63 | 0.33, 1.20 | 0.167 | 1.14 | 0.54, 2.40 | 0.715 |
| Education | |||||||||
| High school or less | 1 | 1 | 1 | ||||||
| Some college | 0.79 | 0.39, 1.59 | 0.514 | 0.83 | 0.40, 1.70 | 0.619 | 0.74 | 0.35, 1.54 | 0.418 |
| College 4 years | 0.37 | 0.18, 0.73 | 0.005 | 0.40 | 0.19, 0.82 | 0.013 | 0.43 | 0.20, 0.90 | 0.026 |
| College 5 years or more | 0.23 | 0.11, 0.48 | 0.000 | 0.28 | 0.13, 0.62 | 0.002 | 0.29 | 0.13, 0.65 | 0.003 |
| Residential property value | |||||||||
| Category 1 (27K - 204K) | 1 | 1 | |||||||
| Category 2 (206 - 268K) | 0.78 | 0.45, 1.36 | 0.393 | 0.86 | 0.46, 1.59 | 0.639 | |||
| Category 3 (269K - 378K) | 0.53 | 0.30, 0.93 | 0.029 | 0.65 | 0.34, 1.22 | 0.186 | |||
| Category 4 (379K - 914K) | 0.15 | 0.07, 0.30 | 0.000 | 0.20 | 0.09, 0.44 | 0.000 | |||
Model 1: Adjusted for age + gender + race/ethnicity
Model 2: Model 1 + mutually adjusted for income and education
Model 3: Model 2 + Adjusted for residential property values
Table 3 shows the associations between SES and prevalent obesity at 1 year. In adjusted models, property values showed the strongest association with prevalent obesity, followed by education. Self-reported household income was no longer significance once property values were included in the model. Living in the highest quartile of house values was associated with an 82% drop in obesity rates.
Table 3.
Multivariate logistic regression to examine the association between prevalent obesity at 1 y follow up and key SES indicators.
|
|
|
|
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | |||||||
| OR | 95% CI | p-value | OR | 95% CI | p-value | OR | 95% CI | p-value | |
|
|
|||||||||
| Annual household income | |||||||||
| <35,000 | 1 | 1 | 1 | ||||||
| 35,000 - <50,000 | 0.93 | 0.44, 1.96 | 0.868 | 1.17 | 0.55, 2.51 | 0.670 | 1.36 | 0.60, 3.05 | 0.448 |
| ≥ 50,000 - < 100,000 | 0.62 | 0.35, 1.12 | 0.117 | 0.81 | 0.43, 1.50 | 0.509 | 1.04 | 0.54, 2.02 | 0.895 |
| ≥ 100,000 | 0.48 | 0.26, 0.87 | 0.017 | 0.76 | 0.39, 1.46 | 0.412 | 1.35 | 0.64, 2.81 | 0.422 |
| Education | |||||||||
| High school or less | 1 | 1 | 1 | ||||||
| Some college | 0.95 | 0.47, 1.92 | 0.907 | 0.97 | 0.49, 1.97 | 0.968 | 0.91 | 0.44, 1.87 | 0.799 |
| College 4 years | 0.37 | 0.18, 0.74 | 0.005 | 0.39 | 0.19, 0.79 | 0.010 | 0.42 | 0.20, 0.88 | 0.022 |
| College 5 years or more | 0.30 | 0.14, 0.62 | 0.002 | 0.34 | 0.15, 0.73 | 0.006 | 0.37 | 0.16, 0.82 | 0.015 |
| Residential property value | |||||||||
| Category 1 (27K - 204K) | 1 | 1 | |||||||
| Category 2 (206K - 268K) | 0.69 | 0.39, 1.22 | 0.21 | 0.74 | 0.40, 1.37 | 0.350 | |||
| Category 3 (269K - 378K) | 0.66 | 0.37, 1.15 | 0.146 | 0.75 | 0.40, 1.42 | 0.388 | |||
| Category 4 (379K - 914K) | 0.15 | 0.07, 0.32 | 0.000 | 0.18 | 0.08, 0.42 | 0.000 | |||
Model 1: Adjusted for age + gender + race/ethnicity
Model 2: Model 1 + mutually adjusted for income and education
Model 3: Model 2 + Adjusted for residential property values
As shown in Table 4, none of the SES variables, including residential property values, had any impact on percent weight change at 1 y, before or after adjusting for covariates. Subsequent multivariable regression models tested the impact of SES variables on weight maintenance, weight loss or weight gain. There was no effect of any of the SES variables on the direction or the magnitude of short term (1y) weight change.
Table 4.
Multivariate linear regression to examine the association between 1 y weight change and key SES indicators.
|
|
|
|
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | |||||||
| β | 95% CI | p-value | β | 95% CI | p-value | β | 95% CI | p-value | |
|
|
|||||||||
| Annual household income | |||||||||
| <35,000 | 0 | 0 | 0 | ||||||
| 35,000 - <50,000 | 0.63 | −0.99, 2.26 | 0.444 | 0.70 | −0.90, 2.31 | 0.393 | 0.66 | −0.96, 2.29 | 0.424 |
| ≥ 50,000 - < 100,000 | 0.34 | −1.11, 1.80 | 0.643 | 0.44 | −1.00, 1.90 | 0.546 | 0.48 | −1.00, 1.98 | 0.519 |
| ≥ 100,000 | 0.90 | −0.50, 2.31 | 0.207 | 1.08 | −0.32, 2.48 | 0.133 | 1.36 | −0.14, 2.87 | 0.077 |
| Education | |||||||||
| High school or less | 0 | 0 | 0 | ||||||
| Some college | −0.09 | −2.13, 1.94 | 0.926 | −0.16 | −2.15, 1.83 | 0.874 | −0.28 | −2.28, 1.70 | 0.777 |
| College 4 years | −0.07 | −2.00, 1.85 | 0.935 | −0.31 | −2.15, 1.52 | 0.733 | −0.28 | −2.10, 1.54 | 0.762 |
| College 5 years or more | −0.14 | −2.09, 1.79 | 0.881 | −0.52 | −2.38, 1.34 | 0.583 | −0.46 | −2.31, 1.37 | 0.617 |
| Residential property value | |||||||||
| Category 1 (27K - 204K) | 0 | 0 | |||||||
| Category 2 (206K - 268K) | 0.94 | −0.30, 2.19 | 0.138 | 0.73 | −0.51, 1.98 | 0.248 | |||
| Category 3 (269K - 378K) | −0.45 | -1.82, 0.90 | 0.510 | −0.78 | −2.18, 0.62 | 0.275 | |||
| Category 4 (379K - 914K) | 0.06 | −1.22, 1.35 | 0.924 | −0.53 | −1.92, 0.86 | 0.452 | |||
Model 1: Adjusted for age + gender + race/ethnicity
Model 2: Model 1 + mutually adjusted for income and education
Model 3: Model 2 + Adjusted for residential property values
DISCUSSION
The observed SES gradient for prevalent obesity in the US was confirmed in the SOS II study, using both – the self-reported measures of SES (income and education) and an objective measure (residential property values at tax parcel). Consistent with other studies, residential property values predicted prevalent obesity better than self-reported household incomes (26), an often problematic variable in health surveys (27,28).
The present data were also consistent with some past interpretations of cross-sectional Federal surveys (3,17). In those surveys, prevalent obesity was linked to lower SES; yet patterns of weight gain were reported for all SES groups (17,29). In the SOS II, SES variables had no impact on the direction or the magnitude of short term weight change, measures over only 1 y. Residential property values and education, powerful predictors of prevalent obesity, did not predict the direction or the magnitude of 1 y weight change.
Consistent with other Federal reports (30), no increase in obesity prevalence was observed. To the contrary, there was a very minor weight loss of 0.46% body weight. However, that seeming stability of population mean weight masked significant gains or losses at the individual level. Participants in this purely observational (i.e. non-intervention) study were equally split among those who gained, lost, or maintained body weight. In past studies (31), weight gain of 0.5-2kg per year was classified as moderate and a weight gain of >2kg per year was classified as large. In the present cohort, one in four participants lost >2kg, whereas one in five gained >2kg.
Even obesity prevention studies have observed weight loss and weight gain within the same cohort. In one study (32) 15% of the cohort (n=823) lost 5% percent body weight while 9.3% gained >5% body weight. The authors suggested that short term weight change (1 y) was a phenomenon that deserved more research attention.
The present use of residential property values, an objective measure of SES, has implications for future studies on obesity and the built environment (33). In this study, tax parcel property values served as an individual SES metric, complementing self-reported education and incomes (23,27,28). However, neighborhood property values, a related measure defined as the mean residential property value within certain distances from respondent’s residence, can reflect the quality of the surrounding built environment (34). In other studies, rather than using residential property values at the tax parcel level, we have used average residential property values for all dwellings within a 400 m or an 800 m buffer of the study respondent’s residence. In one Seattle-based study (24), multiple perceived aspects of “obesogenic” environments were linked to neighborhood residential property values in a predictable manner. Whereas perceived traffic, crime and the reported presence of fast foods and convenience stores were linked to lower property values within 800 m, the presence of parks was linked to higher property values (23). In turn, lower neighborhood residential property values were associated with higher prevalent obesity among women (21,26).
Multiple studies have tried to link rising obesity rates with selected features of the built environment, with mixed results (21). Even though the data were almost entirely cross-sectional, the implication was that living in an “obesogenic” neighborhood was causally linked to weight gain. Whether objective features of the built environment, as captured by neighborhood property values can predict weight gain remains to be seen.
The present study had several limitations. The chief limitation was that duration of exposure was only 1 y; consequently our conclusions only apply to short term weight change. Ideally, weight changes need to be studied over a much longer period. There may have been selection bias in study enrollment; however, the direction of weight change does not show that the study sample was predisposed to weight loss. The SES variables were obtained only at baseline – we do not have data on how changes in SES would affect body weight change.
The present data have some public policy implications. First, low individual SES did not predispose to weight gain and was no barrier to weight loss, at least in the short term. These findings offer significant new hope for community-level obesity prevention and control. While long-term obesity may be strongly influenced by SES (23, 24), weight dynamics may be more closely linked to individual attitudes, dietary behaviors, diet quality, and diet cost. More studies are needed to determine what dietary and behavioral mechanisms can potentiate or override the observed SES constraints on body weight.
What is already known about this subject?
Analyses of consecutive cross-sectional studies (NHANES, BRFSS) in the US suggest that the SES gradient in obesity prevalence does not apply to weight gain.
Higher self-reported SES has been linked repeatedly to lower obesity prevalence.
Only longitudinal cohort data can determine the impact of SES on weight gain.
What does this study add?
The SOS II was a population-based observational study with objective SES measures (property values) and heights and weights measured over 1 y.
Property values predicted obesity but not 1 y weight change.
Mechanisms other than SES may account for short term weight loss or weight gain.
Acknowledgments
Funding source: NIH grants P20 RR020774-03 and R01 DK076608-04. Conflict of Interest: None
REFERENCES
- 1.Drewnowski A, Specter SE. Poverty and obesity: the role of energy density and energy costs. Am J Clin Nutr. 2004;79:6–16. doi: 10.1093/ajcn/79.1.6. [DOI] [PubMed] [Google Scholar]
- 2.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity in the United States, 2009-2010. NCHS Data Brief. :20121–8. [PubMed] [Google Scholar]
- 3.Sturm R, An R. Obesity and economic environments. CA Cancer J Clin. 2014 doi: 10.3322/caac.21237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sturm R. Stemming the global obesity epidemic: what can we learn from data about social and economic trends? Public Health. 2008;122:739–746. doi: 10.1016/j.puhe.2008.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chang VW, Lauderdale DS. Income disparities in body mass index and obesity in the United States, 1971-2002. Arch Intern Med. 2005;165:2122–2128. doi: 10.1001/archinte.165.18.2122. [DOI] [PubMed] [Google Scholar]
- 6.Kant AK, Graubard BI. Secular trends in the association of socio-economic position with self-reported dietary attributes and biomarkers in the US population: National Health and Nutrition Examination Survey (NHANES) 1971-1975 to NHANES 1999-2002. Public Health Nutr. 2007;10:158–167. doi: 10.1017/S1368980007246749. [DOI] [PubMed] [Google Scholar]
- 7.Kilmer G, Roberts H, Hughes E, et al. Surveillance of certain health behaviors and conditions among states and selected local areas--Behavioral Risk Factor Surveillance System (BRFSS), United States, 2006. MMWR Surveill Summ. 2008;57:1–188. [PubMed] [Google Scholar]
- 8.Mujahid MS, Diez Roux AV, Borrell LN, Nieto FJ. Cross-sectional and longitudinal associations of BMI with socioeconomic characteristics. Obes Res. 2005;13:1412–1421. doi: 10.1038/oby.2005.171. [DOI] [PubMed] [Google Scholar]
- 9.Ruel E, Reither EN, Robert SA, Lantz PM. Neighborhood effects on BMI trends: examining BMI trajectories for black and white women. Health Place. 2010;16:191–198. doi: 10.1016/j.healthplace.2009.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Coogan PF, Cozier YC, Krishnan S, et al. Neighborhood socioeconomic status in relation to 10-year weight gain in the Black Women’s Health Study. Obesity (Silver Spring) 2010;18:2064–2065. doi: 10.1038/oby.2010.69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Molarius A, Seidell JC, Sans S, Tuomilehto J, Kuulasmaa K. Educational level, relative body weight, and changes in their association over 10 years: an international perspective from the WHO MONICA Project. Am J Public Health. 2000;90:1260–1268. doi: 10.2105/ajph.90.8.1260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Martikainen PT, Marmot MG. Socioeconomic differences in weight gain and determinants and consequences of coronary risk factors. Am J Clin Nutr. 1999;69:719–726. doi: 10.1093/ajcn/69.4.719. [DOI] [PubMed] [Google Scholar]
- 13.Prattala R, Sippola R, Lahti-Koski M, Laaksonen MT, Makinen T, Roos E. Twenty-five year trends in body mass index by education and income in Finland. BMC Public Health. 2012;12:936. doi: 10.1186/1471-2458-12-936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stafford M, Brunner EJ, Head J, Ross NA. Deprivation and the development of obesity a multilevel, longitudinal study in England. Am J Prev Med. 2010;39:130–139. doi: 10.1016/j.amepre.2010.03.021. [DOI] [PubMed] [Google Scholar]
- 15.Brunner EJ, Chandola T, Marmot MG. Prospective effect of job strain on general and central obesity in the Whitehall II Study. Am J Epidemiol. 2007;165:828–837. doi: 10.1093/aje/kwk058. [DOI] [PubMed] [Google Scholar]
- 16.Hermann S, Rohrmann S, Linseisen J, et al. The association of education with body mass index and waist circumference in the EPIC-PANACEA study. BMC Public Health. 2011;11:169. doi: 10.1186/1471-2458-11-169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kumanyika SK, Obarzanek E, Stettler N, et al. Population-based prevention of obesity: the need for comprehensive promotion of healthful eating, physical activity, and energy balance: a scientific statement from American Heart Association Council on Epidemiology and Prevention, Interdisciplinary Committee for Prevention (formerly the expert panel on population and prevention science) Circulation. 2008;118:428–464. doi: 10.1161/CIRCULATIONAHA.108.189702. [DOI] [PubMed] [Google Scholar]
- 18.Wang Y, Beydoun MA. The obesity epidemic in the United States--gender, age, socioeconomic, racial/ethnic, and geographic characteristics: a systematic review and meta-regression analysis. Epidemiol Rev. 2007;29:6–28. doi: 10.1093/epirev/mxm007. [DOI] [PubMed] [Google Scholar]
- 19.Wang Y, Zhang Q. Are American children and adolescents of low socioeconomic status at increased risk of obesity? Changes in the association between overweight and family income between 1971 and 2002. Am J Clin Nutr. 2006;84:707–716. doi: 10.1093/ajcn/84.4.707. [DOI] [PubMed] [Google Scholar]
- 20.Wallander JL, Kerbawy S, Toomey S, et al. Is obesity associated with reduced health-related quality of life in Latino, Black and White children in the community? Int J Obes (Lond) 2013;37:920–925. doi: 10.1038/ijo.2013.31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Drewnowski A, Rehm CD, Arterburn D. The geographic distribution of obesity by census tract among 59 767 insured adults in King County, WA. Int J Obes (Lond) 2014;38:833–839. doi: 10.1038/ijo.2013.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Michael YL, Nagel CL, Gold R, Hillier TA. Does change in the neighborhood environment prevent obesity in older women? Soc Sci Med. 2014;102:129–137. doi: 10.1016/j.socscimed.2013.11.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Moudon AV, Cook AJ, Ulmer J, Hurvitz PM, Drewnowski A. A neighborhood wealth metric for use in health studies. Am J Prev Med. 2011;41:88–97. doi: 10.1016/j.amepre.2011.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Drewnowski A, Aggarwal A, Rehm CD, Cohen-Cline H, Hurvitz PM, Moudon AV. Environments perceived as obesogenic have lower residential property values. Am J Prev Med. 2014;47:260–274. doi: 10.1016/j.amepre.2014.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schulz M, Kroke A, Liese AD, Hoffmann K, Bergmann MM, Boeing H. Food groups as predictors for short-term weight changes in men and women of the EPIC-Potsdam cohort. J Nutr. 2002;132:1335–1340. doi: 10.1093/jn/132.6.1335. [DOI] [PubMed] [Google Scholar]
- 26.Rehm CD, Moudon AV, Hurvitz PM, Drewnowski A. Residential property values are associated with obesity among women in King County, WA, USA. Soc Sci Med. 2012;75:491–495. doi: 10.1016/j.socscimed.2012.03.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Braveman P, Gottlieb L. The social determinants of health: it’s time to consider the causes of the causes. Public Health Rep. 2014;129(Suppl 2):19–31. doi: 10.1177/00333549141291S206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Braveman PA, Cubbin C, Egerter S, et al. Socioeconomic status in health research: one size does not fit all. Jama. 2005;294:2879–2888. doi: 10.1001/jama.294.22.2879. [DOI] [PubMed] [Google Scholar]
- 29.Truong KD, Sturm R. Weight gain trends across sociodemographic groups in the United States. Am J Public Health. 2005;95:1602–1606. doi: 10.2105/AJPH.2004.043935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Roundtable on Obesity S, Food, Nutrition B, Institute of M . The Current State of Obesity Solutions in the United States: Workshop Summary. National Academies Press (US) Copyright 2014 by the National Academy of Sciences; Washington (DC): 2014. [Google Scholar]
- 31.Golubic R, Ekelund U, Wijndaele K, et al. Rate of weight gain predicts change in physical activity levels: a longitudinal analysis of the EPIC-Norfolk cohort. Int J Obes (Lond) 2013;37:404–409. doi: 10.1038/ijo.2012.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jeffery RW, McGuire MT, French SA. Prevalence and correlates of large weight gains and losses. Int J Obes Relat Metab Disord. 2002;26:969–972. doi: 10.1038/sj.ijo.0802015. [DOI] [PubMed] [Google Scholar]
- 33.Lovasi GS, Hutson MA, Guerra M, Neckerman KM. Built environments and obesity in disadvantaged populations. Epidemiol Rev. 2009;31:7–20. doi: 10.1093/epirev/mxp005. [DOI] [PubMed] [Google Scholar]
- 34.Drewnowski A, Aggarwal A, Rehm C, Cohen-Cline H, Hurvitz PM, Moudon AV. Environments perceived as obesogenic have lower residential property values. Am J Prev Med. 2014 doi: 10.1016/j.amepre.2014.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]