Abstract
Purpose
To examine whether enhancing standard behavior weight loss interventions (SBWP) with additional strategies at the initiation of the intervention (ADOPT) or providing the additional strategies at predetermined times over the intervention period (MAINTAIN) enhances 18 month weight loss.
Methods
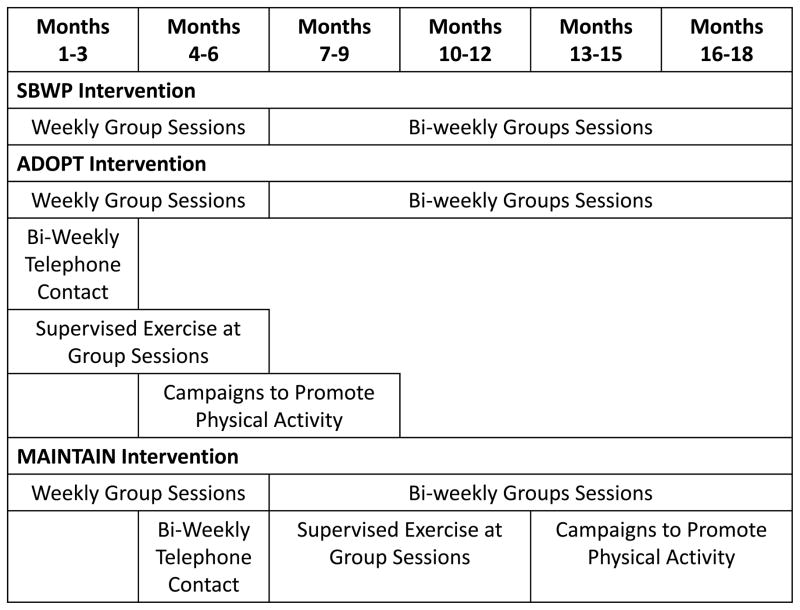
This was a clinical trial with participants (n=195; age= 43.2±8.6 yrs; BMI= 33.0±3.4 kg/m2) randomized to SBWP, ADOPT, or MAINTAIN. All were prescribed an energy restricted diet and physical activity, with group intervention sessions delivered over 18 months. ADOPT received additional phone contact (months 1–3), supervised exercise (months 1–6), and behavior campaigns (months 4–9). MAINTAIN received additional phone contact (months 4–6), supervised exercise (months 7–12), and behavior campaigns (months 13–18).
Results
There was a significant Group X Time interaction for weight loss (p=0.0032). SBWP lost 9.3±0.9, 7.8±1.1, and 5.9±1.2 kg at 6, 12, and 18 months, respectively. ADOPT lost 8.9±0.9, 7.6±1.2, and 5.8±1.2 kg, and MAINTAIN lost 9.7±0.9, 11.0±1.2, and 9.0±1.2 kg at 6, 12, and 18 months, respectively. The Group X Time interaction for SBWP vs. MAINTAIN (p=0.0033) and ADOPT vs. MAINTAIN (p=0.0075) was significant. There was a significant Group X Time interaction for change in fitness (p=0.0060). The Group X Time interaction for MAINTAIN vs. ADOPT (p=0.0018) was significant with a trend for MAINTAIN vs. SBWP (p=0.0525).
Conclusions
MAINTAIN improved 18-month weight loss compared to SBWP and ADOPT, with statistical trends that MAINTAIN resulted in greater improvements in fitness. These results suggest that time-based strategies emphasizing physical activity conferred greater benefits when delivered later and over the full course of intervention. This provides valuable information for the implementation of time-based strategies to improve long-term weight loss and fitness in overweight and obese adults.
Keywords: behavioral strategies, exercise, obesity, weight management program
INTRODUCTION
Excessive body weight has been shown to be associated with risk for numerous chronic diseases including heart disease, diabetes, some forms of cancer, and a variety of musculoskeletal disorders.(18) Estimates in the United States suggest that more than 65% of adults are overweight (Body Mass Index [BMI] ≥25 kg/m2) and more than 30% are obese (BMI ≥30 kg/m2).(7) Thus, there is a compelling need for interventions to treat obesity and mitigate associated health risks.
Behavioral interventions consisting of modifications to dietary and physical activity behaviors have long been considered a cornerstone in the treatment of overweight and obesity. These interventions have typically resulted in loss of approximately 10% of initial body weight.(25) However, available data indicate (24) that only 51% of subjects in a behavioral weight loss program actually achieve this magnitude of weight loss after 6 months of intervention. Moreover, longer-term data suggest that weight loss is difficult to sustain, and it is estimated that one-third to one-half of initial weight loss is regained within 12–18 months following treatment.(21) Thus, research aimed at enhancing initial effects of behavioral interventions on weight loss and improving longer-term weight loss maintenance is a public health priority.
Physical activity is a key contributor to enhancing initial weight loss. Indeed, the combination of reduced energy intake and increased physical activity has been shown to yield improvements in weight loss of 2–3 kg in comparison with reduced energy intake alone.(6) Moreover, physical activity is predictive of improved long-term weight loss and minimizing weight regain.(11–13) This is acknowledged in guidelines from leading organizations.(6) However, the maintenance of a sufficient dose of physical activity is challenging and adherence is typically less than optimal, with our own research suggesting that only 25–30% of individuals in behavioral weight loss programs perform sufficient physical activity to impact long-term weight outcomes.(12) Thus, more effective behavioral strategies are needed to enhance maintenance of physical activity, which may improve long-term weight loss outcomes.
The challenges of sustaining physical activity long-term in response to a behavioral weight loss intervention may be a result of a number of factors. It could be hypothesized that standard behavior weight loss interventions do not adequately teach behavioral skills that allow for sufficient adoption and maintenance of physical activity during initial phases of the program. Therefore, one strategy would be to enhance the intervention during the initial weeks of the intervention in an attempt to improve the engagement in physical activity. Alternatively, it could be hypothesized that a greater emphasis needs to be placed on physical activity at times during the intervention when it is likely that adherence to physical activity may start to decrease, and this decrease in adherence has been observed at 12, 24, and 52 weeks of a standard behavioral weight loss program.(10, 14) Thus, adding strategies as these specific time points of the intervention (i.e., time-based strategies) may be effective at sustaining physical activity, which may translate into improve long-term weight loss.
To our knowledge, there are no previous investigations that have examined the relative efficacy of targeted time-based strategies to enhance the adoption or maintenance of physical activity in the context of a comprehensive behavioral weight loss intervention. Therefore, the purpose of the present study was to examine whether time-based strategies added either initially or throughout an intervention weight loss, physical activity, and fitness over a period of 18 months compared to a standard behavioral weight loss intervention alone.
METHODS AND PROCEDURES
Design
This study was a randomized clinical trial. Eligible individuals were randomized to one of three intervention groups: 1) standard behavioral weight loss program (SBWP), 2) SBWP plus intervention strategies for physical activity implemented over the initial 9 months (ADOPT), or 3) SBWP plus additional intervention strategies for physical activity implemented between months 4–18 (MAINTAIN). The randomization sequence was generated by the study biostatistician (WL), and the randomization was stratified based on gender (male or female) using a computer generated allocation, and only occurred after the participant successfully completed the baseline assessments. The Principal Investigator (JMJ) was responsible for making the final determination on participant eligibility, clearing participants to be randomized, and for oversight of the implementation of the randomization process. Study participants were informed of their group assignment at their first intervention session. Outcomes were assessed at 0, 6, 12, and 18 months. All study procedures were approved by the University of Pittsburgh Institutional Review Board.
Subjects
Subjects were recruited through newspaper, television, radio, and direct mail advertisements in the Greater Pittsburgh Area. Recruitment occurred between September 2003 and February 2005 with outcome assessments completed by August 2006. Eligibility requirements included body mass index ≥25.0 to <40.0 kg/m2 and age between 18–55 years. Exclusion criteria included history of cardiovascular disease, presence of metabolic condition that might affect body weight (e.g., diabetes mellitus, hypothyroid), presence of a medical condition that would preclude reducing energy intake or increasing physical activity, taking medication that would affect body weight (e.g., thyroid medication, psychotropic medication) or heart rate response to exercise (e.g., beta blocker), sustained weight loss of ≥5% within the past 12 months, regular participation in physical activity ≥20 min/d on ≥3 days/wk over the prior 6 months. Moreover, women pregnant in the past 6 months, currently pregnant, or planning on becoming pregnant in the subsequent 18 months were excluded from participation. Subjects completed a detailed medical history and a physical activity readiness questionnaire, obtained written consent from their physician, and provided informed consent prior to participation in this study. The Principal Investigator (JMJ) was responsible for conducting all study orientation sessions and for obtaining written informed consent from the study particpants.
Outcome Assessments
The primary outcomes for this study, which are described in detail below, were assessed at 0, 6, 12, and 18 months. Subjects received compensation of $50 for completion of the assessments at 6, 12, and 18 months. Assessments were conducted at the Physical Activity and Weight Management Research Center at the University of Pittsburgh. Assessment staff knew that the participants were in an active weight loss intervention for this study because this study did not include a no-treatment control condition. To minimize the potential for bias, the staff did not have access to the prior assessment data when assessments were being conducted. There were no serious adverse events reported.
Body weight was assessed to the nearest 0.1 kg (0.25 pounds) using a calibrated scale with the subject clothed in a cloth hospital gown. A wall-mounted stadiometer was used to assess height to the nearest 0.1 cm. BMI was computed as kg/m2.
Body composition was assessed using bioelectrical impedance. The equation proposed by Segal et al. (22) was used to compute lean body mass (LBM), with percent body fat computed as: Percent Body Fat = [(weight – LBM)/weight]*100. Fat distribution was determined using anthropometry and included waist circumference measured horizontally at the level of the umbilicus, hip circumference measured at the widest observed aspect of the buttocks, and sagittal diameter measured at the iliac crest. All anthropometric measurements were represented as the average of two measures that differed by ≤1.0 cm.
A submaximal graded exercise treadmill test was used to assess cardiorespiratory fitness. The grade of the treadmill was 0% at the initiation of the test and increased by 2.5% at 3 minute intervals. Speed remained constant at 80.4 m/min (3.0 mph). Test termination occurred when the subject achieved ≥85% of age-predicted maximal heart rate measured by electrocardiography (ECG), with age-predicted maximal heart rate computed as 220 minus the age of the subject. A cardiologist reviewed the results, and subjects determined to have abnormalities on the ECG or evidencing other contraindications to exercise were referred to their primary care physician for follow-up evaluation prior to proceeding with participation in this study.
Energy expenditure (kcal/wk) in physical activity and bouts of physical activity performed over the previous week were assessed using the questionnaire developed for the Harvard Alumni Study.(20) A food frequency questionnaire was used to provide an estimate of energy intake (kcal/d) and percent of macronutrient composition (fat, carbohydrates, protein).(2, 3) The Eating Behavior Inventory (EBI) (19) was used to assess engagement in eating behaviors consistent with weight control.
Interventions
The details of the interventions used for SBWP, ADOPT, and MAINTAIN are provided below (also see Text, Supplemental Digital Content 1, additional details of the intervention components). The intervention occurred at the Physical Activity and Weight Management Research Center at the University of Pittsburgh, which includes intervention space, private weigh-in areas, and access to fitness facilities that were used for this study.
SBWP
Subjects in SBWP were instructed to attend group-based intervention sessions throughout the 18-month intervention. Sessions were conducted weekly for months 1–6 and every other week during months 7–18. Sessions were scheduled for approximately 45 minutes and were led by an interventionist trained in health psychology, nutrition, or exercise. These sessions were modeled after sessions as previously described.(10–13)
The dietary intervention included instruction to reduce energy intake and dietary fat consumption, and is based on dietary interventions implemented in other weight loss studies.(11–13, 15) Energy intake was prescribed at 1,200 kcal/d for subjects ≤90 kg (≤200 lbs) or 1,500 kcal/d for subjects >90 kg (>200 lbs). Dietary fat intake was prescribed at 20–30% of total energy intake. Meal plans were provided along with a published reference for calorie and fat composition of popular foods. Subjects were instructed to self-monitor food intake in a weekly diary provided to them, and completed diaries were reviewed by the interventionists and feedback was provided to the subjects in an effort to maximize adherence to the dietary recommendations of the study.
Structured periods of physical activity were also prescribed, which progressed from an initial duration of 100 minutes per week to 150 min/wk at week 5, and 200 min/wk at week 9, with subjects encouraged to maintain at least 200 min/wk of physical activity for the remainder of the 18 month intervention period. Subjects were encouraged to distribute activity over 5 d/wk, with the minimum duration of any bout of activity ≥10 min. We have previously demonstrated that this physical activity prescription is effective for enhancing physical activity participation.(10) Moderate-to-vigorous physical activity intensity was prescribed and defined as 11–15 on the 15-point rating of perceived exertion (RPE) scale.(1) Similar to dietary intake, subjects were instructed to self-monitor physical activity in a weekly diary that was reviewed and annotated by the interventionists.
ADOPT
Subjects in ADOPT received all of the components described above for SBWP. In addition, subjects received additional intervention strategies over the initial 9 months of the intervention aimed at enhancing compliance to the recommended dose of physical activity. These included telephone contacts (Month 1–3), supervised physical activity sessions (Month 1–6), and physical activity campaigns (Month 4–9). The timing of these intervention strategies is illustrated in Figure 1.
Figure 1.
Consort diagram
The additional telephone contact involved a bi-weekly 10-minute telephone call from a member of the intervention staff, and these were in addition to the in-person group intervention visit for weeks 1–12. The interventionist followed a structured script for the telephone intervention calls, with the goal to complete this call in ≤10 minutes. The focus of the call was to identify existing or anticipated barriers to the participant’s physical activity behaviors and to identify strategies to overcome these barriers.
During weeks 1–24, subjects in ADOPT were encouraged to participate in a supervised session with the intervention staff in conjunction with attending a group intervention meeting. These sessions involved the use of cardiovascular training equipment (treadmills and stationary cycles) that were located in the Physical Activity and Weight Management Research Center, or an outdoor walk. A minimum of 30 minutes per session was encouraged. All remaining exercise for this study was performed under non-supervised conditions.
During months 4–9 subjects in ADOPT participated in two 12-week campaigns to promote physical activity. These campaigns involved the use of pedometers to promote daily and weekly step goals consistent with the prescribed dose of exercise. Examples of campaigns included “10,000 Steps” where subjects were encouraged to achieve 10,000 steps per day or other campaigns that had a regional or seasonal theme.
MAINTAIN
Subjects in MAINTAIN received all of the components described above for SBWP. In addition, subjects received the ADOPT intervention strategies, but these were implemented across the full 18 months of intervention in contrast to the 9-month period utilized in the ADOPT intervention. Specifically, the telephone intervention contacts were provided during Months 4–6, supervised physical activity sessions were provided during Months 7–12 in conjunction with the behavioral group sessions, and physical activity campaigns were provided during Months 13–18. The timing of these intervention strategies is illustrated in Figure 1.
Statistical Analysis
An a-priori power calculation was computed based on expected differences in body weight at 18 months among the randomized groups. Results of this a-priori power analysis indicated that 63 subjects per group would provide 80% power at an alpha level of 0.05 to detect a 3.6 kg weight loss difference between the SBWP group and either the ADOPT or MAINTAIN group, equivalent to a 50% effect size. The outcomes presented include intention-to-treat analyses.
Statistical analyses were performed using SAS (version 9.2), with the type I error rate fixed at 0.05 (two-tailed). Normality of outcome variables was checked using the Kolmogorov-Smirnov test. Differences between treatment groups in baseline characteristics were examined using the Chi-square test for categorical variables and analysis of variance for continuous variables.
Separate mixed effects models using the Unstructured dependence structure, UN, were fit to the outcomes with 4 time points (baseline, 6, 12, and 18 months) for weight, BMI, waist circumference, hip circumference, waist-to-hip ratio, sagittal diameter, percent body fat, fitness, and physical activity measured via questionnaire, EBI, and dietary intake. Changes from baseline were calculated and modeled using a mixed effects model with 3 time points adjusting for baseline measure in the model as a covariate. Inferences were focused on the treatment effect, time effect, and treatment by time interaction effect. Least-square means and differences between least-square means were obtained from the models along with their standard error estimates. Intent-to-treat analyses were conducted using multiple imputation implemented using SAS procedures PROC MI and PROC MIANALYZE. For each outcome, ten datasets were imputed and results were then combined.
RESULTS
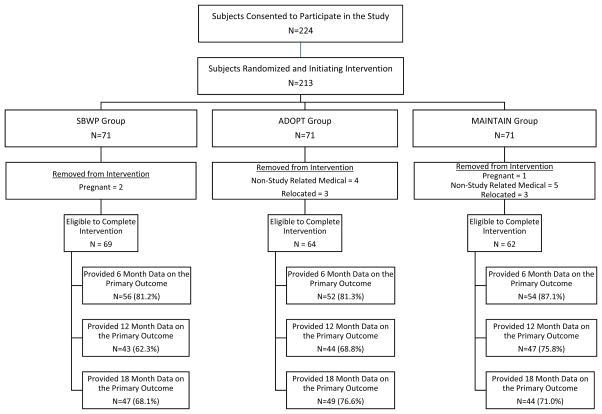
This study randomized 213 subjects to the three intervention groups. As shown in Figure 2, 18 subjects were removed from the study for reasons that made them ineligible to continue their participation after randomization. Thus, 195 subjects were eligible to continue with the intervention for the entire 18 month period. Of these 195 subjects, a total of 140 subjects (71.8%) provided data for the primary outcome of body weight at the 18 month assessment, which resulted in attrition of 28.2%. The retention rates by randomization group at the 6, 12, and 18 month assessment periods are shown in Figure 2, and there was no significant difference in retention between the groups. Results are presented with data analyzed using multiple imputation for intention-to-treat analysis for the 195 subjects eligible to complete the 18 month study. Descriptive characteristics are shown in Table 1.
Figure 2.
Timing of intervention components by condition.
Table 1.
Demographic Characteristics of Randomized Subjects (N=195).
| Total | SBWP | ADOPT | MAINTAIN | P-value# for treatment | |
|---|---|---|---|---|---|
| Number of Subjects | |||||
| Intention-to-Treat Analysis | N=195 | N=69 | N=64 | N=62 | |
| Completers | N=140 | N=47 | N=49 | N=44 | |
| Lost to Follow-Up | N=55 | N=22 | N=15 | N=18 | |
| Gender (Males) | |||||
| Intention-to-Treat Analysis | N=43 | N=14 | N=15 | N=14 | 0.9020 |
| Completers | N=31 | N=8 | N=12 | N=11 | 0.5827 |
| Lost to Follow-Up | N=12 | N=6 | N=3 | N=3 | 0.7072 |
| Age(years) | |||||
| Intention-to-Treat Analysis | 43.20±8.55 | 42.01±9.27 | 43.25±8.60 | 44.47±7.57 | 0.2622 |
| Completers | 44.61±8.23 | 42.86±9.35 | 44.65±8.26 | 46.44±6.50 | 0.1157 |
| Lost to Follow-Up | 39.60±8.39 | 40.21±9.03 | 38.67±8.36 | 39.64±8.00 | 0.8644 |
| Body Mass Index(kg/m2) | |||||
| Intention-to-Treat Analysis | 33.02±3.43 | 32.71±3.73 | 33.29±2.92 | 33.08±3.59 | 0.6240 |
| Completers | 32.73±3.31 | 32.30±3.51 | 33.26±2.96 | 32.60±3.44 | 0.3503 |
| Lost to Follow-Up | 33.75±3.65 | 33.60±4.11 | 33.38±2.89 | 34.25±3.76 | 0.7711 |
| Ethnicity+ | |||||
| Asian | N=1(N=1) | N=1(N=1) | N=0(N=0) | N=0(N=0) | 0.1968 |
| American Indian or Alaska Native | N=1(N=1) | N=1(N=1) | N=0(N=0) | N=0(N=0) | |
| Black or African-American | N=62(N=36) | N=25(N=13) | N=18(N=14) | N=19(N=9) | |
| Hispanic, Latino, Portuguese, Cape Verdean | N=1(N=36) | N=0(N=0) | N=0(N=0) | N=1(N=0) | |
| White | N=129(101) | N=41(N=31) | N=46(N=35) | N=42(N=35) | |
| Other | N=1(N=1) | N=1(N=1) | N=0(N=0) | N=0(N=0) | |
| Education Level+ | |||||
| High School(10–12 years) | N=23(N=14) | N=7(N=4) | N=9(N=5) | N=7(N=5) | 0.1824 |
| Vocational Training(beyond High School) | N=13(N=11) | N=5(N=5) | N=3(N=3) | N=5(N=3) | |
| Some College(less than 4 years) | N=57(N=39) | N=27(N=18) | N=16(N=10) | N=14(N=11) | |
| College/University Degree | N=59(N=39) | N=14(N=7) | N=22(N=19) | N=23(N=13) | |
| Graduate or Professional Education | N=42(N=36) | N=16(N=13) | N=14(N=12) | N=12(N=11) | |
| Not Reported | N=1(N=1) | N=0(N=0) | N=0(N=0) | N=1(N=1) | |
Indicates that numbers not in parenthesis are based on the intent-to-treat analysis and numbers in parenthesis are based on subjects completing 18 months.
P-values for between treatment group comparisons were obtained using the Chi-square test for categorical variables and the Student’s T-test for continuous variables.
Weight Change
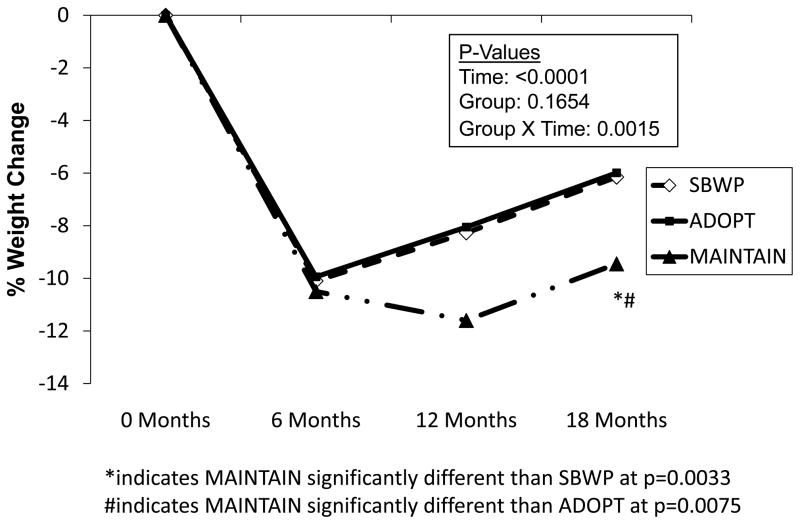
The primary outcome in this study was change in body weight at 18 months between the three intervention conditions (see Table 2 and Figure 3). Weight loss at 18 months was 5.9 (SEM=1.2) kg in SBWP, 5.8 (SEM=1.2) kg in ADOPT, and 9.0 (SEM=1.2) kg in MAINTAIN. The significant Group X Time interaction (p=0.0032) indicates that the pattern of weight loss varied between the intervention groups.
Table 2.
Change in body weight, body composition, fitness, energy intake, eating behavior, and physical activity by intervention condition.
| Outcome Variable | Intervention Group | Baseline | Change from Baseline to 6 Months |
Change from Baseline to 12 Months |
Change from Baseline to 18 Months |
p-values for Main Effects | p-values for Group X Time Interaction Effects |
||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||||
| Time | Group | Group X Time |
ADOPT vs. MAINTAIN |
ADOPT vs. SBWP |
MAINTAIN vs. SBWP |
||||||
|
| |||||||||||
| Weight (kg) | ADOPT (N=64) | 94.1±1.7 | −8.9±0.9 | −7.6±1.2 | −5.8±1.2 | 0.1654 | <.0001 | 0.0032 | 0.0075 | 0.7640 | 0.0033 |
| MAINTAIN (N=62) | 94.2±1.7 | −9.7±0.9 | −11.0±1.2 | −9.0±1.2 | |||||||
| SBWP (N=69) | 91.5±1.7 | −9.3±0.9 | −7.8±1.1 | −5.9±1.2 | |||||||
|
| |||||||||||
| Body Mass Index (kg/m2) | ADOPT (N=64) | 33.3±0.4 | −3.2±0.3 | −2.7±0.4 | −2.0±0.4 | 0.1488 | <.0001 | 0.0031 | 0.0058 | 0.7878 | 0.0038 |
| MAINTAIN (N=62) | 33.1±0.4 | −3.4±0.3 | −3.8±0.4 | −3.1±0.4 | |||||||
| SBWP (N=69) | 32.7±0.4 | −3.2±0.3 | −2.7±0.4 | −2.0±0.4 | |||||||
|
| |||||||||||
| Fitness (minutes) | ADOPT (N=64) | 10.0±0.5 | 4.6±0.5 | 4.0±0.6 | 3.1±0.6 | 0.2607 | 0.0001 | 0.0060 | 0.0018 | 0.5605 | 0.0525 |
| MAINTAIN (N=62) | 8.7±0.6 | 3.7±0.4 | 5.2±0.6 | 4.5±0.6 | |||||||
| SBWP (N=69) | 9.5±0.5 | 3.5±0.4 | 3.8±0.6 | 3.0±0.7 | |||||||
|
| |||||||||||
| Energy Intake (kcal/d) | ADOPT (N=64) | 2342±108.6 | −618±73.9 | −378±91.5 | −428±96.8 | 0.7017* | <.0001* | 0.3810* | 0.1181 | 0.3716 | 0.0879 |
| MAINTAIN (N=62) | 2043±110.3 | −622±71.2 | −524±89.3 | −436±102.4 | |||||||
| SBWP (N=69) | 1944±104.6 | −646±68.6 | −490±89.3 | −489±100.4 | |||||||
|
| |||||||||||
| Eating Behavior Inventory | ADOPT (N=64) | 69.4±1.1 | 17.0±1.3 | 13.95±1.5 | 10.53±1.7 | 0.4650 | <.0001 | 0.0390 | 0.6136 | 0.0126 | 0.0570 |
| MAINTAIN (N=62) | 70.1±1.1 | 19.0±1.3 | 15.57±1.5 | 12.77±1.8 | |||||||
| SBWP (N=69) | 69.1±1.1 | 18.7±1.2 | 13.44±1.5 | 14.08±1.6 | |||||||
|
| |||||||||||
| Physical Activity (kcal/week) | ADOPT (N=64) | 733.7±86.6 | 1213±157.7 | 861.4±176.7 | 624.3±212.2 | 0.1057* | 0.0576* | 0.2058* | 0.2798 | 0.1264 | 0.5562 |
| MAINTAIN (N=62) | 619.6±88.0 | 1171±154.8 | 1004±169.2 | 968.4±227.7 | |||||||
| SBWP (N=69) | 669.4±83.4 | 1087±158.4 | 809.1±164.9 | 1058±217.0 | |||||||
|
| |||||||||||
| Physical Activity (bouts/wk) | ADOPT (N=64) | 1.1±0.2 | 2.8±0.3 | 2.29±0.3 | 2.01±0.3 | 0.2508 | 0.0097 | 0.5076 | 0.3250 | 0.6630 | 0.3872 |
| MAINTAIN (N=62) | 0.9±0.2 | 3.0±0.3 | 3.15±0.3 | 2.54±0.4 | |||||||
| SBWP (N=69) | 1.1±0.2 | 2.8±0.3 | 2.48±0.3 | 2.38±0.3 | |||||||
Indicates that data were log transformed for the model.
Figure 3.
Percent change in body weight by intervention condition.
Additional analyses were performed to probe whether the differences in weight change could be attributed to different weight loss patterns between 0 and 6 months, 0 and 12 months, or 0 and 18 months. These analyses revealed no significant differences between the groups for weight loss from 0 to 6 months. MAINTAIN lost significantly more weight from 0 to 12 months compared to ADOPT (p=0.0408) with a trend for greater weight loss when compared to SBWP (p=0.0558), with no significant difference between SBWP and ADOPT (p=0.8850). There was also a non-significant trend for greater weight loss from 0 to 18 months in MAINTAIN compared to both SBWP (p=0.0652) and ADOPT (p=0.0768), with no difference in weight loss between SBWP and ADOPT (p=0.9334). A similar pattern of results was observed when BMI data were analyzed (see Table 2).
Body Composition and Body Fat Distribution
The pattern of change in body fatness and body fat distribution is similar to that observed for change in body weight and BMI (see Table, Supplemental Digital Content 2, change in antropometry, body composition, and macronutrient composition by intervention condition). There was a significant Group X Time interaction (p=0.0345) for the comparison of change in percent body fat between the groups. There was also a significant Group X Time interaction for comparison of change in hip (p=0.0009), with a trend for a significant Group X Time interaction for change in waist circumference (p=0.07) and sagittal diameter (p=0.0896).
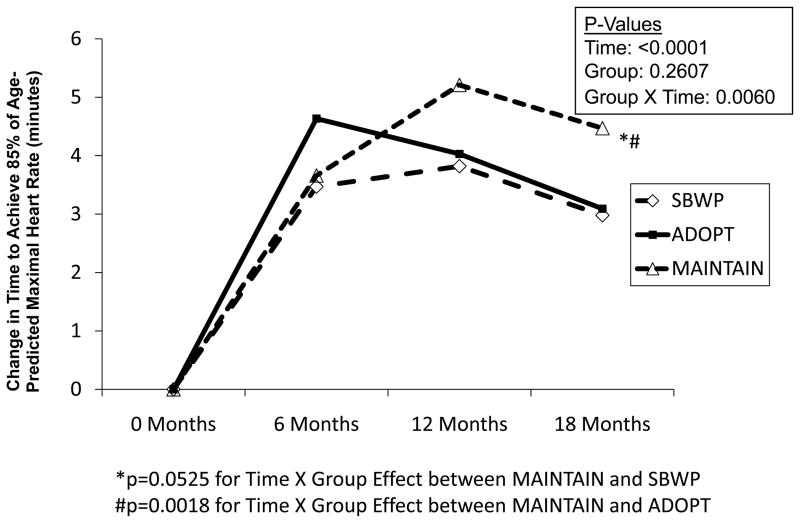
Cardiorespiratory Fitness
The pattern of change in fitness across the 18 month intervention is shown in Table 2 and Figure 4. Time to achieve 85% of age-predicted maximal heart rate increased in all groups from 0 to 18 months; however, the significant Group X Time interaction (p=0.0060) indicates that the pattern of change across this period differed between the groups. Post-hoc comparisons revealed a significant Group X Time interaction when comparing MAINTAIN and ADOPT (p=0.0018), with a non-significant trend for a Group X Time interaction when comparing MAINTAIN and SBWP (p=0.0525). The Group X Time interaction when comparing SBWP and ADOPT was not statistically significant (p=0.5605).
Figure 4.
Change in fitness by intervention condition.
Physical Activity
Overall, there was a non-significant time effect (p=0.1057) for change in physical activity energy expenditure assessed by questionnaire, and the lack of a significant Group X Time interaction suggests that the pattern of change in physical activity was similar across the three intervention groups. Analysis of data for bouts of physical activity revealed a similar pattern that was observed for energy expenditure (see Table 2).
Dietary Intake and Eating Behavior
Self-reported dietary intake showed significant decreases in energy intake (p<0.0001) and percent dietary fat intake (p<0.0001), with significant increases observed for percent carbohydrate intake (p=0.0015) and percent protein intake (p=0.0005) (see Table 2 and see Text, Supplemental Digital Content 2, change in antropometry, body composition, and macronutrient composition by intervention condition). However, there were no differences between intervention groups in macronutrient intake. Moreover, there was a significant (p<0.0001) improvement in eating behaviors recommended for weight control as measured by the EBI, and a significant Group X Time interaction (p=0.0390) across the 18 months of this study (see Table 2).
DISCUSSION
The major finding of the current investigation is that implementing enhanced physical activity strategies (MAINTAIN) across an intervention period of 18 months is associated with superior weight loss compared to both SBWP and ADOPT. Traditionally, a SBWP results in initial mean weight loss of approximately 10% of initial body weight, with initial weight loss followed by a period of weight regain.(25) A similar pattern was observed in this study in response to SBWP, with a 9.3 kg weight loss at 6 months followed by a weight regain of 3.4 kg over the subsequent 12 months (see Table 2 and Figure 3). Thus, weight regain after the six month weekly intervention was approximately 37% of initial weight loss, which is consistent with observed weight regains in behavioral weight management programs.(25) Similarly, the ADOPT intervention, which utilized enhanced physical activity strategies during the first half of the 18-month intervention, did not improve weight loss in comparison to SBWP. ADOPT resulted in initial weight losses of 8.9 kg followed by weight regain of 3.5 kg, which was equivalent to regain of 35% of initial weight loss. In contrast, MAINTAIN resulted in 9.7 kg of weight loss at 6 months with only 0.7 kg of weight regain between months 6 and 18, which was equivalent to regain of 6% of initial weight loss.
The present findings suggest that MAINTAIN may be a useful approach for sustaining weight loss, and this may be coupled with greater improvements in fitness (see Table 2 and Figure 3). These findings are important because increases in cardiorespiratory fitness have been shown to be important for reducing health risk in overweight and obese adults.(9) For example, Wing et al. (26) have reported a higher level of fitness, in both overweight and obese adults with diabetes, is associated with improved glucose control and decreased odds of hypertension. Jakicic et al.(16) have also reported improvements in fitness are associated with improved HbA1c in type 2 diabetics after controlling for weight loss and use of diabetes medication. It has also been shown that a higher level of fitness, independent of measures of obesity, is associated with a reduced risk of cardiovascular disease morbidity and mortality.(9) However, the results from this study should be interpreted with caution, because while there was an overall difference between the interventions, post-hoc comparisons showed only trends towards significant differences in fitness for MAINTAIN vs. SBWP.
Although MAINTAIN was effective at improving weight loss compared to both SBWP and ADOPT, while also improving fitness compared to ADOPT with a statistical trend toward improving fitness compared to SBWP (p=0.0525), MAINTAIN was not associated with increases in physical activity. The failure to detect differences in activity may be secondary to the use self-report rather than an objective methodology (e.g., accelerometers, etc.), particularly as overweight/obese adults have been shown to over-report their physical activity.(17) Moreover, individuals who over-report their physical activity have been shown to be less successful in weight loss programs,(8) and this cannot be discounted in this study. We also used a self-reported measure of energy intake, which may have limited the ability of this study to detect differences between groups that would explain the differences observed in weight loss for MAINTAIN compared to both SBWP and ADOPT.
The intervention enhancements provided to MAINTAIN included additional telephone contact, the opportunity for supervised exercise, and campaigns to promote physical activity. Although MAINTAIN appears to be effective for improving weight loss at 18 months compared to both SBWP and ADOPT, the study design does not allow for determination of whether this effect is due to the specific strategies that were used, the timing of strategy implementation, or a combination of these factors. Nevertheless, findings from the current investigation highlight that the use of time-based physical activity strategies appear to be an efficacious tool for maintaining recommended weight loss behaviors. Further research is needed to identify the specific strategies and to ascertain the most effective timing of the strategies to have the greatest weight loss benefit.
Study findings also provide important evidence that enhanced strategies to improve physical activity levels do not enhance weight loss outcomes when offered during the first half of an 18-month intervention. The ADOPT intervention was not effective at improving weight loss compared to SBWP, nor was it more effective at improving fitness. Thus, adding additional intervention strategies at the initiation of a behavioral weight loss intervention may add additional cost to the intervention without improving weight loss or fitness, and therefore this approach does not appear to be warranted. Rather, spreading these strategies over the entire intervention period, as in MAINTAIN, may be more effective for improving long-term outcomes of weight loss and fitness.
The MAINTAIN intervention provided additional behavior strategies to promote physical activity that were implemented at pre-specified times throughout the intervention period. An alternative would be to provide intervention enhancements only for individuals for whom predetermined weight loss, dietary behaviors, or physical activity behaviors were not achieved, which is similar to the stepped care approach proposed by Brownell et al.(4) An advantage to a stepped-care intervention is that it is a “self-correcting” intervention approach, which monitors results of interventions and new intervention decisions are based on the failure to meet intervention outcome expectations.(23) It has been suggested that this hierarchical approach to health-related interventions, including weight loss, may provide a cost-effective public health approach. Carels et al.(5) have shown modest success with this type of intervention in response to a self-help 18 week weight loss program that could be intensified if the participant did not achieve a weight loss of 2.5% after an initial period of 6 weeks. More recently Jakicic et al.(15) reported on the cost-effectiveness of an 18-month stepped-care intervention. However, direct comparison of the effectiveness of time-based versus stepped care interventions focused on physical activity have not been conducted and warrant investigation. Studies directly comparing time-based interventions similar to the MAINTAIN intervention included in the current study to a stepped-care approach are needed to determine if these are equally or differentially effective for weight loss and fitness change compared to SBWP.
Unfortunately, this study did not initially propose to conduct a cost-effectiveness analysis of the interventions (SBWP, ADOPT, MAINTAIN), and this is recognized as a limitation of this study. Prior to implementation, cost and cost-effectiveness analyses may be necessary to inform that likelihood that these interventions are feasible within clinical and community-based settings. Moreover, additional research may be needed to conceptualize strategies that can be used within a MAINTAIN intervention that has broad application in community-based settings and may be more generalizable to a broader population.
In summary, intervention strategies focused on physical activity behavior that are added after a 3 month period of SBWP (MAINTAIN) may be effective at improving weight loss and fitness across an 18 month intervention in overweight and obese adults compared to SBWP alone. Moreover, adding these strategies at the beginning of the SBWP, as in the ADOPT intervention, did not improve weight loss compared to SBWP. In light of the poor weight loss maintenance observed in the behavioral weight management literature, and the importance of improving fitness, the identification of successful strategies that focus on physical activity for long-term weight loss maintenance represent an important and promising step forward for intervention development and implementation.
Supplementary Material
Acknowledgments
This study was supported by grant HL 067826 from the National Institutes of Health and the National Heart, Lung, and Blood Institute.
We recognize the contribution of the staff and graduate students at the Physical Activity and Weight Management Research Center in the Department of Health and Physical Activity at the University of Pittsburgh for their contribution to recruitment, assessments, intervention delivery, and data management for this study.
The results of this study do not constitute endorsement by ACSM.
Funding: This study was supported by grant HL 067826 from the National Institutes of Health and the National Heart, Lung, and Blood Institute.
Footnotes
CONFLICTS OF INTEREST
Dr. Jakicic discloses the following conflicts of interest: Principal Investigator or Co-Investigator on a research grant from BodyMedia, Inc., NIH research grants, and an American Heart Association grant awarded to the University of Pittsburgh; honoraria from Kaiser Permanente, JennyCraig, and the Nestle Nutrition Institute; was on the Scientific Advisory Board for Alere Wellbeing.
Dr. Rickman: No Conflicts of Interest
Dr. Lang: No Conflicts of Interest
Dr. Davis: No Conflicts of Interest
Dr. Gibbs: No Conflicts of Interest
Ms. Neiberg: No Conflicts of Interest:
Dr. Marcus discloses the following conflicts of interest: Travel/accommodations/meeting expenses from the Academy of Eating Disorders and NIDDK.
Trial Registration: clinicaltrial.gov Identifier NCT00177476
LIST OF REFERENCES
- 1.Pescatello LS, editor. American College of Sports Medicine. ACSM’s Guidelines for Exercise Testing and Prescription. 9. Baltimore: Wolters Kluwer / Lippincott Williams & Wilkins; 2014. [Google Scholar]
- 2.Block G, Woods M, Potosky A, Clifford C. Validation of a self-administered diet history questionnaire using multiple diet records. J Clin Epidemiol. 1990;43:1327–1335. doi: 10.1016/0895-4356(90)90099-b. [DOI] [PubMed] [Google Scholar]
- 3.Block G, Hartman AM, Dresser CM, Carol MD, Gannon J, Gardner L. A data-based approach to diet questionnaire design and testing. Am J Epidemiol. 1986;108:161–175. doi: 10.1093/oxfordjournals.aje.a114416. [DOI] [PubMed] [Google Scholar]
- 4.Brownell KD. Public health approaches to obesity and its management. Ann Rev Public Health. 1986;7:521–533. doi: 10.1146/annurev.pu.07.050186.002513. [DOI] [PubMed] [Google Scholar]
- 5.Carels RA, Wott CB, Young KM, et al. Successful weight loss with self-help: a stepped-care approach. J Behav Med. 2009;32:503–509. doi: 10.1007/s10865-009-9221-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Donnelly JE, Blair SN, Jakicic JM, Manore MM, Rankin JW, Smith BK. ACSM position stand on appropriate intervention strategies for weight loss and prevention of weight regain for adults. Med Sci Sports Exerc. 2009;42(2):459–471. doi: 10.1249/MSS.0b013e3181949333. [DOI] [PubMed] [Google Scholar]
- 7.Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US aduls, 1999–2010. JAMA. 2012;307:491–497. doi: 10.1001/jama.2012.39. [DOI] [PubMed] [Google Scholar]
- 8.Jakicic JM, Polley BA, Wing RR. Accuracy of self-reported exercise and the relationship with weight loss in overweight women. Med Sci Sports Exerc. 1998;30(4):634–638. doi: 10.1097/00005768-199804000-00024. [DOI] [PubMed] [Google Scholar]
- 9.Jakicic JM, Mishler AE, Rogers R. Fitness, fatness, and cardiovascular disease risk and outcomes. Curr Cardiovasc Risk Rep. 2011;5:113–119. [Google Scholar]
- 10.Jakicic JM, Wing RR, Butler BA, Robertson RJ. Prescribing exercise in multiple short bouts versus one continuous bout: effects on adherence, cardiorespiratory fitness, and weight loss in overweight women. Int J Obes. 1995;19:893–901. [PubMed] [Google Scholar]
- 11.Jakicic JM, Winters C, Lang W, Wing RR. Effects of intermittent exercise and use of home exercise equipment on adherence, weight loss, and fitness in overweight women: a randomized trial. JAMA. 1999;282(16):1554–1560. doi: 10.1001/jama.282.16.1554. [DOI] [PubMed] [Google Scholar]
- 12.Jakicic JM, Marcus BH, Lang W, Janney C. Effect of exercise on 24-month weight loss in overweight women. Arch Int Med. 2008;168(14):1550–1559. doi: 10.1001/archinte.168.14.1550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jakicic JM, Marcus BH, Gallagher KI, Napolitano M, Lang W. Effect of exercise duration and intensity on weight loss in overweight, sedentary women. A randomized trial. JAMA. 2003;290:1323–1330. doi: 10.1001/jama.290.10.1323. [DOI] [PubMed] [Google Scholar]
- 14.Jakicic JM, Winters C, Lagally K, Ho J, Robertson RJ, Wing RR. The accuracy of the TriTrac-R3D accelerometer to estimate energy expenditure. Med Sci Sports Exerc. 1999;31(5):747–754. doi: 10.1097/00005768-199905000-00020. [DOI] [PubMed] [Google Scholar]
- 15.Jakicic JM, Tate D, Davis KK, et al. Effect of a stepped-care intervention approach on weight loss in adults: The Step-Up Study Randomized Trial. JAMA. 2012;307(24):2617–2626. doi: 10.1001/jama.2012.6866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jakicic JM, Egan CE, Fabricatore AN, et al. Change in cardiorespiratory fitness and influence on diabetes control and CVD risk factors in adults with type 2 diabetes: 4-year results from the Look AHEAD Trial. Diabetes Care. 2013;36 (5):1297–1303. doi: 10.2337/dc12-0712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Litchman SW, Pisarska K, Berman ER, et al. Discrepancy between self-reported and actual caloric intake and exercise in obese subjects. N Engl J Med. 1992;327:1893–1898. doi: 10.1056/NEJM199212313272701. [DOI] [PubMed] [Google Scholar]
- 18.National Institutes of Health National Heart Lung and Blood Institute. Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults - The Evidence Report. Obes Res. 1998;6(suppl 2) [PubMed] [Google Scholar]
- 19.O’Neil PM, Currey HS, Hirsch AA, et al. Development and validation of the eating behavior inventory. Journal of Behavioral Assessment. 1979;1(2):123–132. [Google Scholar]
- 20.Paffenbarger RS, Hyde RT, Wing AL, Hsieh CC. Physical activity, all-cause mortality, and longevity of college alumni. N Engl J Med. 1986;314:605–613. doi: 10.1056/NEJM198603063141003. [DOI] [PubMed] [Google Scholar]
- 21.Perri MG, Corsica JA. Improving the maintenance of weight lost in behavioral treatment of obesity. In: Wadden T, Stunkard AJ, editors. Handbook of Obesity Treatment. The Guilford Press; New York: 2002. pp. 357–379. [Google Scholar]
- 22.Segal KR, Gutin B, Presta E, Wang J, Van Itallie TB. Estimation of human body composition by electrical impedance methods: a comparative study. J Appl Physiol. 1985;58(5):1565–1571. doi: 10.1152/jappl.1985.58.5.1565. [DOI] [PubMed] [Google Scholar]
- 23.Sobell MB, Sobell LC. Stepped care as a heuristic approach to the treatment of alcohol problems. J Consult Clin Psychol. 2000;68(4):573–79. [PubMed] [Google Scholar]
- 24.Unick JL, Jakicic JM, Marcus BH. Contribution of behavior intervention components to 24 month weight loss. Med Sci Sports Exerc. 2010;42(4):745–753. doi: 10.1249/MSS.0b013e3181bd1a57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wing RR. In: Behavioral Weight Control, in Handbook of Obesity Treatment. Wadden TA, Stunkard AJ, editors. The Guilford Press; New York: 2002. pp. 301–316. [Google Scholar]
- 26.Wing RR, Jakicic J, Neiberg R, et al. Fitness, fatness, and cardiovascular risk factors in type 2 diabetes: Look AHEAD Study. Med Sci Sports Exerc. 2007;39(12):2107–2116. doi: 10.1249/mss.0b013e31815614cb. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.