Abstract
Virus-specific CD4+ T cells play a major role in viral infections, such as hepatitis C virus (HCV). Viral clearance is associated with vigorous and multi-specific CD4+ T-cell responses, while chronic infection has been shown to be associated with weak or absent T-cell responses. Most of these studies have used functional assays to analyze virus-specific CD4+ T-cell responses; however, these and other detection methods have various limitations. Therefore, the important question of whether virus-specific CD4+ T cells are completely absent or primarily impaired in specific effector functions during chronic infection, has yet to be analyzed in detail. A novel assay, in which virus-specific CD4+ T-cell frequencies can be determined by de novo CD154 (CD40 ligand) expression in response to viral antigens, can help to overcome some of the limitations of functional assays and restrictions of multimer-based methods. This and other current established methods for the detection of HCV-specific CD4+ T cells will be discussed in this review.
Keywords: viral hepatitis, hepatitis C, CD4 T cells, CD154, ELISpot, FACS, tetramers
Introduction
Hepatitis C virus (HCV) infection is a serious healthcare problem chronically affecting 170–200 million people worldwide (1), which is approximately 3% of the world’s population (2–4). Hepatotropic viruses, such as HCV, can lead to severe liver disease, such as liver cirrhosis and hepatocellular carcinoma (HCC) (5, 6). HCV is responsible for about 3–4 million infections per year and deaths of about 476,000 HCV-infected patients from HCV-associated diseases and their complications (4). Only around 30% of HCV-infected adults are able to clear the virus spontaneously and are often asymptomatic. Innate and adaptive host immune responses play an important role in eradication of the virus. No protective vaccine is yet available against HCV infection (7).
T cells are highly specific immune cells involved in adaptive immune responses. Through their antigen-specific T-cell receptor (TCR), T cells identify antigens specifically, as well as efficiently; these expand into specific effector responses, with a broad repertoire of functions, and eventually contract, forming a memory response. As important effector cells in the defense against pathogens such as HCV, T cells are likely the most highly scrutinized cell type in the immune system.
The cellular components of the adaptive immune response, i.e., CD4+ helper and CD8+ cytotoxic T-cell-mediated immune responses, have been shown to play a central role in determining the outcome of HCV infection (8). Spontaneous viral clearance of HCV infection is characterized by early, strong, vigorous, polyclonal, and multi-specific T-cell responses during the acute phase of infection (9, 10); whereas, chronic HCV infection is associated with late, transient, weak, or narrowly focused specific T-cell responses (11–13). These data, along with strong associations between HLA Class I and II genes in outcome (14–16), point to the involvement of T cells in controlling the infection. In addition, during persistence of HCV infection, typically only low frequencies of HCV-specific T cells are reported in blood, although with a potential higher frequency in the liver (17, 18), which is the primary site of infection. However, these are functionally weak T-cell responses leading to the development and maintenance of chronic HCV infection (11, 19, 20).
However, the data on the function and specificity of T cells in chronic HCV remain quite limited, partly due to methodological constraints. Given their importance in defining both disease outcome and potentially the progression of pathology, further information about the frequencies, phenotypes, and functional capacities of HCV-specific T-cell immune response would be of value.
Traditionally, the main effector cells that eradicate HCV-infected cells were considered to be the cytotoxic T lymphocytes (CTLs) (21). In terms of CD4+ T helper cell responses, much attention has been focused on type 1 or “Th1” CD4+ T cells, since secretion of interferon-γ has been proposed to be linked to control of hepatotropic viruses (22). CD4+ T cells are central to the adaptive immune response to potentially act in different ways to initiate and maintain adaptive immunity, such as providing help for CD8+ T cells by cytokine production and activation of antigen-presenting cells (APCs) and many other mechanisms. During HCV infection, CD4+ T-cell responses are observed to be very different in chronic and resolved individuals; Why CD4+ T-cell responses may fail in acute infection leading to chronic infection is a critical and unanswered question in the field. Therefore, it is important to develop specific and sensitive detection methods for HCV-specific CD4+ T cells.
Difficulties in Assessing HCV-Specific CD4+ T Cells
The frequency of T cells specific for a single peptide–MHC ligand is very low in naive repertoires, (range 0.2–60 cells/106 naive T cells) due to the high diversity of T cell repertoire, allowing a response to a different variety of antigens (23, 24). In the memory repertoire and in the absence of acute infections, the frequency of specific T cells in peripheral blood is typically well below 1% (23). Therefore, the major issue for the detection and identification of antigen-specific T cells is the detection of rare events. Specifically, pathogen-specific CD4+ T cells are often circulating in low frequencies in un-manipulated samples, i.e., less than 0.01–0.1%, and such antigen-specific CD4+ T cells are 10- to 100-fold less frequent than cytotoxic T cells (25). The frequency of pathogen-specific T cells can vary widely depending on the nature of the pathogen, the status of the immune response, and the persistence or clearance of the pathogen. Interestingly, the functionally important T-cell populations may occur at even lower frequencies, and such populations may require additional enrichment for detection. This includes the in vitro expansion of antigen-specific CD4+ T cells, magnetic enrichment to collect infrequent target cells from large cell samples, enrichment of cytokine-secreting cells, and tetramer enrichment techniques. Therefore, highly specific labeling methods, which are capable of processing large cell samples to detect rare specific T cells within the large numbers of non-specific cells are necessary and several methods have been proposed to assess HCV-specific CD4+ T cells.
Methods and their Limitations
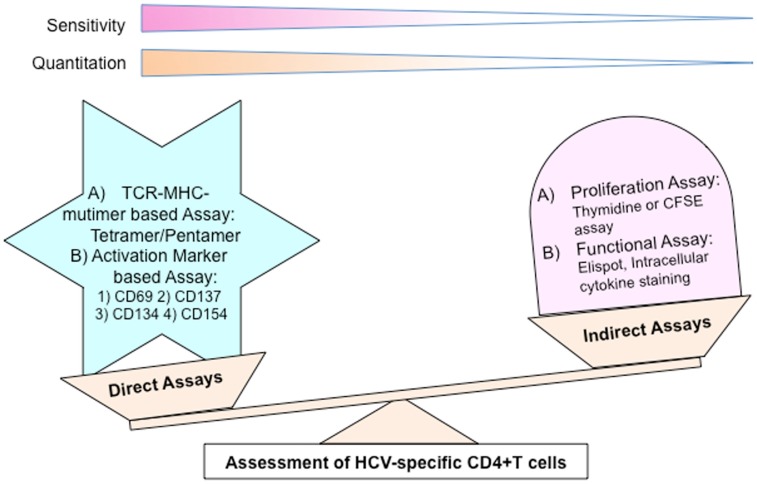
Several methods have been utilized to analyze HCV-specific T cells and can be divided into two groups (Figure 1): (A) indirect assays; (B) direct assays.
Figure 1.
Different methods to analyze HCV-specific CD4+ T cells.
Indirect assays
These assays depend on the functional characteristics of antigen-specific T cells after particular triggering of TCR, such as proliferation capacity, cytokine secretion, etc. Lefkovits et al. first described limiting dilution assay (26), by which the frequencies of antigen-specific CD4+ T cells participating in an immune response after particular stimulation were assessed (27) with estimations ranging from 1 in 10,000 to 1 in 1,000,000 PBMC. Traditionally, besides being extremely time consuming, it was technically difficult to identify rare cells of interest at frequencies below 10−3–10−4, thus making it hard to obtain reliable results. With the emergence of the latest high speed techniques, such as analyzers and sorters, these limitations could be overcome.
Proliferation assay
Thymidine incorporation assay is an assay that has been used for decades to measure the low frequencies of antigen-specific T cells on the basis of antigen-specific proliferation directly. In this assay, a radioactive nucleoside, 3H-thymidine, is incorporated into new strands of chromosomal DNA during mitotic cell division. It is measured by scintillation Beta counter in terms of radioactivity in DNA recovered from the cells in order to determine the extent of cell division due to the specific stimulation. This method can massively alter the phenotypic and functional properties of reactive cells and cell viability. However, the method has several limitations, including lower sensitivity, background DNA synthesis in other cells, and bystander cell activation. It was observed that PBMC proliferation cannot be equated with CD4+ T-cell proliferation because B cells and CD8+ T cells have also been shown to proliferate in response to recombinant viral proteins and/or their breakdown products (28). In a chimpanzee model study, peripheral HCV-specific CD4+ T-cell responses were observed in all HCV-infected animals without any correlation to the outcome of infection and independent of the kinetics, strength, specificity, or diversity of that response. However, a strong correlation between the intrahepatic HCV-specific T-cell response and course of infection could be found (29).
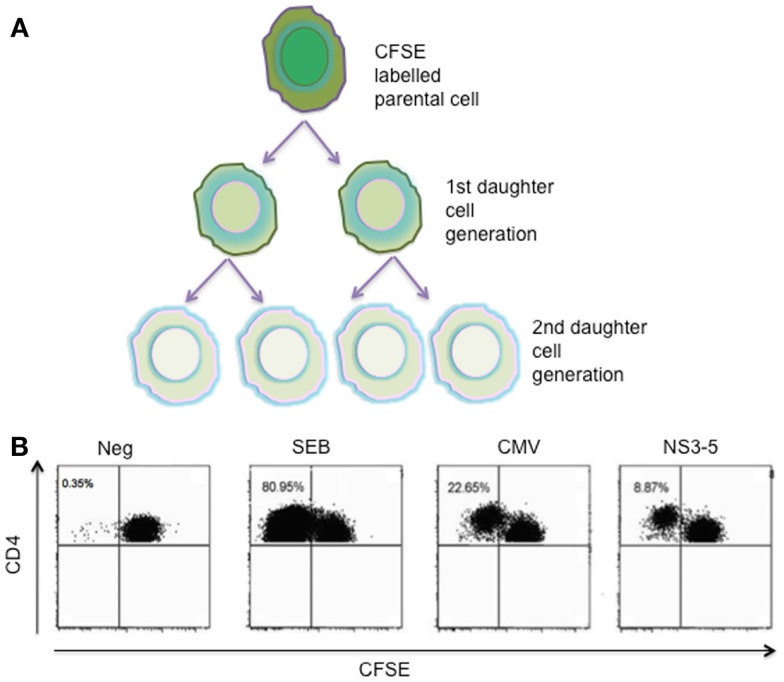
CFSE staining, a flow-cytometric approach, is used to directly monitor the rate of lymphocyte proliferation, due to progressive halving of CFSE fluorescence in cells following cell division (30) (Figure 2). Technically, CFSE can be toxic to cells at high concentrations, and it is therefore necessary to determine the optimum labeling conditions that give good fluorescence and preserve normal function. Furthermore, the analysis of dead cells by apoptosis during the time of analysis is not possible with this method. Therefore, the evaluation made with the technique, in which 3–5 days in vitro culture period is necessary, is not a direct evaluation of T cells dividing in response to specific antigen stimuli. In the case of HCV infection, the proliferative capacity assessed by the dilution of CFSE was analyzed in our previous study, in which only a minority of chronic HCV cases demonstrated HCV-specific proliferation with highest frequency of 0.46% proliferating CD4+ T cells. In contrast, strong proliferative responses were found in resolved HCV individuals (31). In conclusion, the lack of proliferative capacity of CD4+ T cells is linked to persistent HCV-infected cases.
Figure 2.
CFSE proliferation assay. (A) Decreasing fluorescence by equal distribution after each cell division. (B) Representative CFSE FACS plots: CFSE-labeled PBMCs on day 6 following stimulation with SEB or PHA, CMV, and HCV NS3–5 proteins are shown. Undivided CD4+ T cells are detected in the upper right quadrants of each FACS plot, and the CFSE signal is diluted with each cell division as the dye is distributed to the daughter cells. Numbers in the upper left quadrants of each plot represent the percentage of antigen-specific CD4+ T cells that have proliferated during the 6-day culture. SEB, staphylococcal enterotoxin B; PHA, Phytohemagglutinine; CMV, cytomegalovirus; CFSE, carboxyfluorescein diacetate succinimidyl ester; NS3-5, pool of HCV non-structural proteins 3, 4 and 5.
Although there are technical limitations for these assays, HCV-specific CD4+ T cells are mostly non-proliferative in such assay systems; thus, for studies of CD4+ T-cell responses during chronicity, these approaches are very limited.
Other functional assays
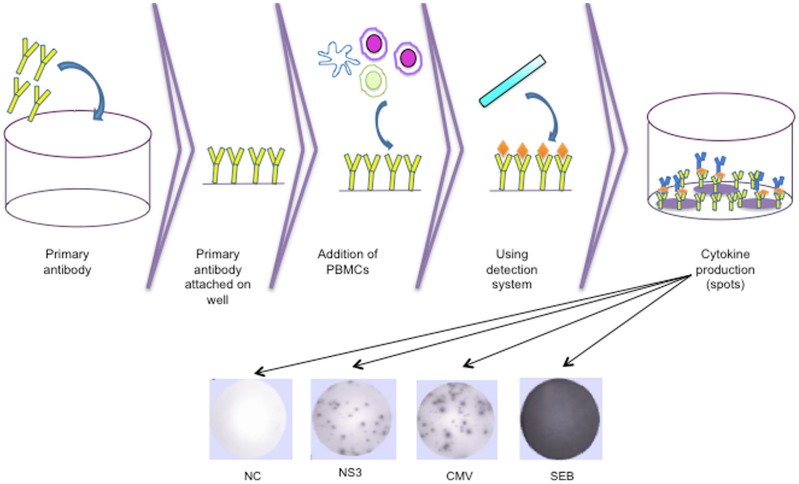
ELISpot is an established method for characterizing the T cell response in which magnitude and quality of T-cell immunity is measured at single cell resolution by detecting individual events of antigen-specific T cells that engage in secretion of cytokines, such as IFN-γ, IL-2, etc. (Figure 3). In the case of HCV infection, previous studies revealed that HCV-specific CD4+ T cells were often unable to produce cytokine after stimulation with HCV antigen in chronic HCV patients, whereas, strong CD4+ T-cell IFN-γ responses were observed in resolved HCV patients (19, 31–33). Correspondingly, IL-2 secretion capacity was also similar to IFN-γ secretion capacity in chronic HCV-infected cases (31, 32). In contrast, in another study, cytokine secretion could be detected in chronic HCV at least for core peptides; however, this was not the case for the non-structural regions (19). Overall, due to relative dysfunctionality of these cells in chronic HCV infection, especially for those directed against non-structural proteins, this method does not provide complete information about the actual frequency of antigen-specific T cells.
Figure 3.
Diagram of the technical procedure of T-cell ELISpot and representative ELISpot wells for a negative control, NS3, CMV lysate, and SEB, respectively. CMV, cytomegalovirus; SEB, staphylococcal enterotoxin B.
In flow cytometry cytokine production assays, TCR-activated T cells produce cytokines transiently. Different cytokines have different kinetics in the response of specific antigen. Intracellular cytokine production can be detected using Brefeldin A and Monensin, which interfere in protein-trafficking events. In addition, cytokines can be detected on the cell surface of the secreting cells by retention of the secreted cytokine via a cell-surface affinity matrix (34, 35). Therefore, methods based on the detection of HCV antigen-reactive cytokine expression are independent of proliferative capacity, MHC alleles, and peptides. However, HCV-specific T cells that do not produce cytokines after activation (31) or which produce alternative cytokines not in the assay protocol (e.g., type 2 or type 17) may be missed. Furthermore, use of one defined cytokine for detection of CD4+ T cells may lead to biased evaluation of the actual frequencies of HCV-specific CD4+ T cells.
Direct methods
In these methods, detection depends on direct labeling of antigen-specific T cells with fluorescent molecules, such as MHC Class II–peptide multimers (tetramers/pentamers) or particular receptor antibodies, and can be analyzed by flow cytometry.
With the traditional methods based on function, the detection of the actual frequency and phenotype of reactive T cells, as well as elimination of bystander proliferation, were difficult to avoid. Therefore, to achieve accuracy, flow cytometry techniques have advantages, and also provide an opportunity to examine multiple parameters of single cells from large cell samples. Polychromatic cytometry for identification of rare CD4+ T cells has the capacity to gain maximum information, e.g., up to 20 parameters from a single analysis. Limitation of flow-cytometric assays to detect rare events can further be minimized by a pre-enrichment strategy with magnetic cell separation, which collects the small number of rare events from large cell numbers (34).
Labeling with peptide–MHC-multimers
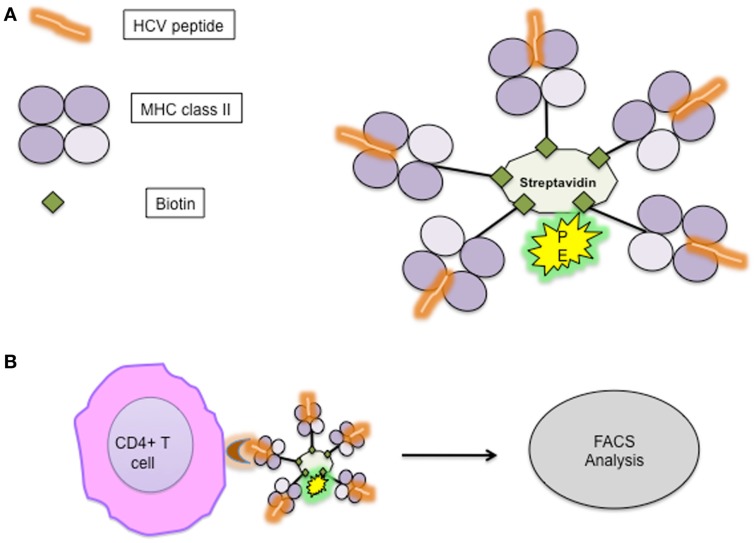
Detection of antigen-specific CD4+ T cells is possible ex vivo, based on direct labeling with specific peptide–MHC-multimers without restriction to certain functional parameters (Figure 4). The low binding affinity of TCR to MHC–peptide monomers (36) was overcome by multimerization of peptide–MHC complexes (37). Initially, MHC class II multimers were difficult to construct due to the problems of yield, the variety of MHC class structure, and peptide affinity; recently, however, different varieties of MHC II multimers for specific recognition of CD4+ T cells have become commercially available.
Figure 4.
(A) Outline of MHC-pentamer complex with HCV-specific peptide; (B) specific CD4+ T cells bind with HCV-specific pentamer complex. MHC, major histocompatibility complex.
However, there are some limitations for the tetramer technology, such as the knowledge of immunodominant epitopes and exact characterization of the MHC alleles of the patients are required. Hence, the detection of the entire repertoire of antigen-specific CD4+ T cells appears difficult (25). Additionally, there still remain issues regarding frequencies, since when using non-specific MHC II–peptide tetramers, background staining may approach 0.1% (38).
Labeling with activation markers
Prior specific stimulation with cognate antigen, i.e., single peptides, proteins, or whole antigen lysates, is necessary for detection of antigen-specific T cells on the basis of functional parameters. T-cell antigen reactivity-based assays to enumerate antigen-specific T cells have the advantage that they are independent of MHC alleles and not restricted to single peptides.
Independent of functional parameters, such as cytokine secretion or cytotoxicity, another approach for accessing the antigen-specific T cells by flow cytometer is on the basis of activation markers. The transient expression of activation markers on the T-cell surface depends on antigen-specific activation by TCR triggering. These activation markers may be constrained to a differentiation state of the T cells (e.g., naïve, central, effector memory) or T cell types. Several potential activation markers have been proposed, such as CD69, CD25, CD71, HLA-DR, CD134 (OX40), CRTAM, CD137 (4-1BB), and CD154 (CD40-L) (23). However, some limitations for many of these markers restrict precise enumeration due to sensitivity to bystander activation (CD69, CD25), constitutive expression on specialized T cell subsets (CD69, CD25, CRTAM), or late up-regulation after stimulation (HLA-DR, CD134, CD71) (23).
CD69
The extensively used activation marker, CD69 is expressed on activated CD4+ and CD8+ T cells, B cells, or NK cells. Nevertheless, non-stimulated T cells restrict the accurate enumeration of antigen-specific T cells (39). There is evidence that CD69 expression is not exclusively dependent on TCR activation (40).
CD137
Expression of CD137 (4-1BB), a member of the TNFR superfamily, is observed on CD4+ and CD8+ T cells after specific stimulation (41–43) and even on CD4+ Foxp+ regulatory T cells (44). Hence, CD137 expression-based assay can be used to detect antigen-specific CD4+ T cells after TCR activation with specific stimulation.
OX40
Similarly, recently a novel assay system has been developed and validated for the detection of HCV-specific CD4+ T cells. The assay system is based on ex vivo stimulation with HCV antigens, and HCV-specific CD4+ T cells can be detected with flow cytometry after staining with CD25 (IL-2R α) and CD134 (OX40) (45). TCR triggering stimulates up-regulation of CD25 and CD134 over 24–48 h, with the optimal readout determined to be 44 h (46). It is a highly sensitive method, which correlates with CFSE-based LPA, and successfully detects HCV-specific CD4+ T-cell responses in resolved and chronic HCV-infected patients (45), as well as HIV-infected individuals (47).
CD154 (CD40-L) Assay
This recently established method analyzing expression of CD154 is highly sensitive and specific for the overall assessment of antigen-specific CD4+ T cells. It avoids many of the limitations described above for the virus-specific CD4+ T cell detection. Hence, a virus-specific CD4+ T cell response can be detected not only through an antiviral function of CD4+ T cells, but also staining of PBMCs with surface marker CD154 (CD40-L) (31) or intracellular CD154 expression after stimulation with cognate antigen (48).
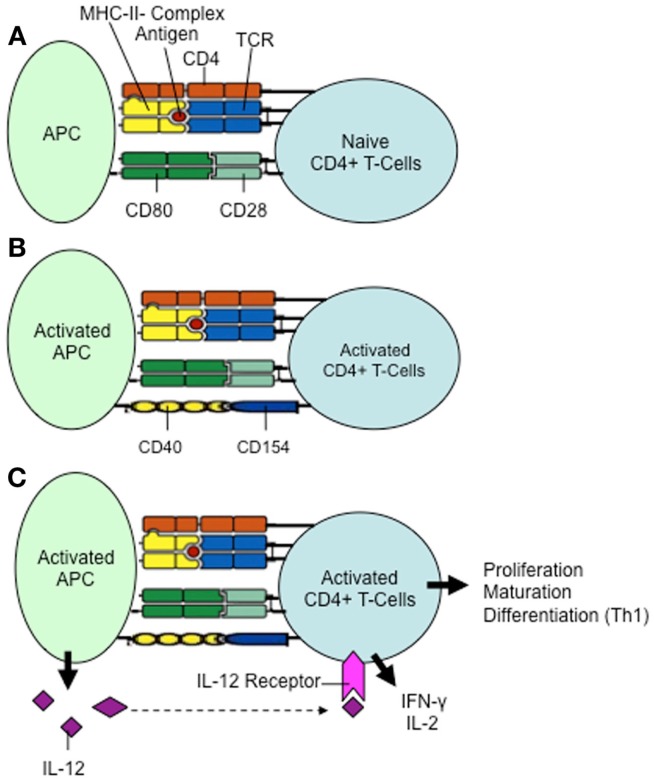
CD154, a type II member protein of 33 kDa, which belongs to the family of tumor necrosis factors (TNF), also called CD40 ligand (CD40-L), is a cell-surface molecule present primarily on activated T cells. Engagement of its receptor, CD40, on APCs results in priming and expansion of antigen-specific CD4+ T cells, induction of co-stimulatory molecules on APCs, and the release of cytokines (49) (Figure 5). This molecule plays a key role in the activation of antigen-specific CD4+ T cells; this is evident by treatment of blocking antibodies against CD154, leading to an activation inhibition of antigen-specific CD4+ T cells (50) (Figure 5).
Figure 5.
The role of CD154 in the activation of CD4+ T cells. (A) Activation of naive CD4+ T cells requires two signals: (1) binding of the TCR (T cell receptor) to the antigen-loaded MHC II complex on the antigen-presenting cell (APC). (2) Interaction of the co-stimulatory molecules CD28 and CD80. (B) Activated antigen-specific CD4+ T cells express CD154, which binds to the CD40 molecule on the surface of the antigen-presenting cell. Simultaneously, the further differentiation of the antigen-presenting cell is initiated via CD40/CD154-signaling, in which more co-stimulatory molecules are expressed (not shown). (C) The fully activated antigen-presenting cell now increasingly secretes IL-12. Proliferation, maturation, and differentiation of CD4+ T cells into Th1 lymphocytes with secretion of IFN-γ and IL-2 can be induced.
In addition to the detection of live antigen-specific CD4+ T cells, it is independent of other effector functions, such as proliferation or cytokine production, and independent of MHC haplotype or immunodominant epitopes. The method allows the analysis of co-expression of CD154 and effector cytokine production, such as IFN-γ or IL-2 and/or the phenotypes of the T cells with other surface markers. The detection of CD154 expression for assessing viral-specific CD4+ T cells is therefore a method which permits a quantitative and qualitative ex vivo and in vitro evaluation of antigen-specific CD4+ T cells. The CD154 expression-based method for the analysis of antigen-specific CD4+ T cells allows the identification of activated T cells even when their capacity to secrete cytokines is inadequate, such as in chronic HCV-infected individuals. The method is suitable for whole blood analysis (51).
In chronic HCV infection, one of the main reasons for the difficulty in assessing antigen-specific CD4+ T cells is their low frequency. Day et al. used MHC tetramer to detect antigen-specific CD4+ T cells and estimated about 1:1200–1: 111,000 frequencies of those cells (52). Interestingly, Möller et al. detected an average of 100,000–150,000 CD4+ T cells in analysis in the method based on CD154 expression (53). They used threshold in analysis around 0.01%; therefore, only T-cell populations with a frequency above 1:10,000 could be detected.
Lessons from Studying CD154 Expression in HCV Infection
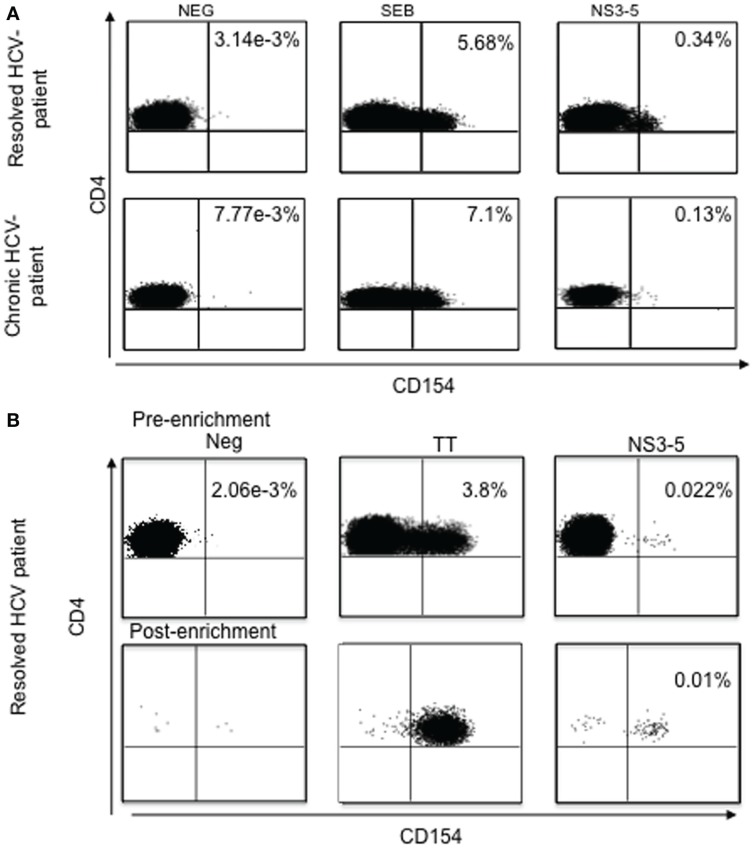
In recent studies, CD154 expression was examined on CD4+ T cells after stimulation with HCV-cognate antigen in peripheral blood from HCV chronic infected patients and in spontaneous viral resolved (SVR) HCV patients (31) (Figure 6). The results of these studies demonstrated that HCV-specific CD4+ T cells were present not only in spontaneous resolved HCV, but also in chronically infected HCV individuals. Similar findings by Bes et al. proved that HCV-specific CD4+ T cells, although dysfunctional, are present in the peripheral blood in most patients with chronic HCV infection and can be easily detected, irrespective of their functional profile, by transient antigen-specific up-regulation of CD154 (54).
Figure 6.
(A) Ex vivo analysis of antigen-specific CD154 expression without enrichment. Analysis of antigen-specific CD154+ CD4+ T cells from two representative individuals with spontaneously resolved infection and chronic HCV infection, respectively. SEB, staphylococcal enterotoxin B. (B) Ex vivo analysis of antigen-specific CD154 expression pre- and post-enrichment using the magnetic bead enrichment assay. TT, tetanus toxoid; NS3-5, pool of HCV non-structural proteins 3, 4 and 5.
Indeed, in our previous findings, detection of CD154 expression could be found in chronic HCV-infected patients, with frequencies of HCV-specific CD4+ T cells almost comparable with spontaneous viral clearance. However, when these frequencies were assessed for functional capacity, IFN-γ and IL-2 secretion, as well as proliferation, were significantly lower in chronic HCV infection when compared with the spontaneous HCV-resolved individuals, suggesting that HCV-specific CD4+ T cell responses are present in chronic HCV, although in a dysfunctional state (31). Several studies utilizing MHC class II tetramers have supported the conclusion that CD4+ T-cell responses in the majority of chronically infected HCV patients are absent (52). However, CD154 expression-based analysis of HCV-specific CD4+ T cells indicates that the HCV-specific CD4+ T cells are present in the peripheral blood and even liver, but they are dysfunctional. Several studies suggested that HCV-specific CD4+ T cells might be sequestered at the site of viral replication and inflammation (31, 55–58), and the CD154 up-regulation studies found higher antigen-specific CD4+ T-cell frequencies in the liver than the blood in HCV-infected patients. Overall, these studies indicated that the virus-specific CD4+ T cells are present and even enriched at the site of disease, and that the virus can persist despite the presence of these virus-specific T cells.
One advantage of the CD154 method for the assessment of viral-specific CD4+ T cells is that responses can not only be detected using whole protein as antigen, but also using peptides, allowing fine mapping of epitopes (31). Thus, overall this is a simple method for reliably characterizing the targeted peptides after stimulation with corresponding antigens.
Summary
In summary, antigen-specific CD4+ T-cell responses can be readily analyzed by detection of CD154 expression in HCV infection. This method is simple, reliable, and independent of both HLA type, knowledge of the epitopes, and effector functions, such as cytokine production or proliferation capacity of CD4+ T cells. Studies using CD154 expression-based methods for analysis of HCV-specific CD4+ T cells suggest that CD4+ T cells are not fully exhausted or deleted during chronic HCV infection, but some remain detectable and can trigger through their TCR. However, these cells typically lack proliferative capacity and cytokine secretion capacities, such as for IFN-γ and IL-2.
It will be of interest in the future to explore the mechanisms that lead to the dysfunction of virus-specific CD4+ T cells. The method to detect these “dysfunctional” antigen-specific CD4+ T cells in blood and at the site of infection, provides a new opportunity to pursue this important question experimentally and to understand the overall mechanisms that lead to chronic HCV infection. Defining the exact state of differentiation of CD154+ CD4+ T cells, the differences between chronically infected patients and patients with spontaneous viral clearance, and the impact of direct acting antivirals (DAA) therapy are all relevant questions for future study.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
- 1.Wendt A, Adhoute X, Castellani P, Oules V, Ansaldi C, Benali S, et al. Chronic hepatitis C: future treatment. Clin Pharmacol (2014) 6:1–17. 10.2147/CPAA.S30338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ascione A, Tartaglione T, Di Costanzo GG. Natural history of chronic hepatitis C virus infection. Dig Liver Dis (2007) 39(Suppl 1):S4–7. 10.1016/S1590-8658(07)80003-X [DOI] [PubMed] [Google Scholar]
- 3.Lavanchy D. The global burden of hepatitis C. Liver Int (2009) 29(Suppl 1):74–81 10.1111/j.1478-3231.2008.01934.x [DOI] [PubMed] [Google Scholar]
- 4.Shepard CW, Finelli L, Alter MJ. Global epidemiology of hepatitis C virus infection. Lancet Infect Dis (2005) 5(9):558–67. 10.1016/S1473-3099(05)70216-4 [DOI] [PubMed] [Google Scholar]
- 5.Afdhal NH. The natural history of hepatitis C. Semin Liver Dis (2004) 24(Suppl 2):3–8 10.1055/s-2004-832922 [DOI] [PubMed] [Google Scholar]
- 6.Lauer GM, Walker BD. Hepatitis C virus infection. N Engl J Med (2001) 345(1):41–52 10.1056/NEJM200107053450107 [DOI] [PubMed] [Google Scholar]
- 7.Houghton M, Abrignani S. Prospects for a vaccine against the hepatitis C virus. Nature (2005) 436(7053):961–6. 10.1038/nature04081 [DOI] [PubMed] [Google Scholar]
- 8.Klenerman P, Thimme R. T cell responses in hepatitis C: the good, the bad and the unconventional. Gut (2012) 61(8):1226–34. 10.1136/gutjnl-2011-300620 [DOI] [PubMed] [Google Scholar]
- 9.Shin EC, Seifert U, Kato T, Rice CM, Feinstone SM, Kloetzel PM, et al. Virus-induced type I IFN stimulates generation of immunoproteasomes at the site of infection. J Clin Invest (2006) 116(11):3006–14. 10.1172/JCI29832 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Thimme R, Oldach D, Chang KM, Steiger C, Ray SC, Chisari FV. Determinants of viral clearance and persistence during acute hepatitis C virus infection. J Exp Med (2001) 194(10):1395–406. 10.1084/jem.194.10.1395 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chang KM, Thimme R, Melpolder JJ, Oldach D, Pemberton J, Moorhead-Loudis J, et al. Differential CD4(+) and CD8(+) T-cell responsiveness in hepatitis C virus infection. Hepatology (2001) 33(1):267–76. 10.1053/jhep.2001.21162 [DOI] [PubMed] [Google Scholar]
- 12.Ulsenheimer A, Gerlach JT, Gruener NH, Jung MC, Schirren CA, Schraut W, et al. Detection of functionally altered hepatitis C virus-specific CD4 T cells in acute and chronic hepatitis C. Hepatology (2003) 37(5):1189–98. 10.1053/jhep.2003.50194 [DOI] [PubMed] [Google Scholar]
- 13.Wedemeyer H, He XS, Nascimbeni M, Davis AR, Greenberg HB, Hoofnagle JH, et al. Impaired effector function of hepatitis C virus-specific CD8+ T cells in chronic hepatitis C virus infection. J Immunol (2002) 169(6):3447–58. 10.4049/jimmunol.169.6.3447 [DOI] [PubMed] [Google Scholar]
- 14.Thio CL, Thomas DL, Goedert JJ, Vlahov D, Nelson KE, Hilgartner MW, et al. Racial differences in HLA class II associations with hepatitis C virus outcomes. J Infect Dis (2001) 184(1):16–21. 10.1086/321005 [DOI] [PubMed] [Google Scholar]
- 15.Ksiaa L, Ayed-Jendoubi S, Sfar I, Gorgi Y, Najjar HA, Abdallah TB, et al. Clearance and persistence of hepatitis C virus in a Tunisian population: association with HLA class I and class II. Viral Immunol (2007) 20(2):312–9. 10.1089/vim.2006.0060 [DOI] [PubMed] [Google Scholar]
- 16.Harris RA, Sugimoto K, Kaplan DE, Ikeda F, Kamoun M, Chang KM. Human leukocyte antigen class II associations with hepatitis C virus clearance and virus-specific CD4 T cell response among Caucasians and African Americans. Hepatology (2008) 48(1):70–9. 10.1002/hep.22287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.He XS, Rehermann B, Lopez-Labrador FX, Boisvert J, Cheung R, Mumm J, et al. Quantitative analysis of hepatitis C virus-specific CD8(+) T cells in peripheral blood and liver using peptide-MHC tetramers. Proc Natl Acad Sci U S A (1999) 96(10):5692–7. 10.1073/pnas.96.10.5692 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Grabowska AM, Lechner F, Klenerman P, Tighe PJ, Ryder S, Ball JK, et al. Direct ex vivo comparison of the breadth and specificity of the T cells in the liver and peripheral blood of patients with chronic HCV infection. Eur J Immunol (2001) 31(8):2388–94. [DOI] [PubMed] [Google Scholar]
- 19.Semmo N, Day CL, Ward SM, Lucas M, Harcourt G, Loughry A, et al. Preferential loss of IL-2-secreting CD4+ T helper cells in chronic HCV infection. Hepatology (2005) 41(5):1019–28. 10.1002/hep.20669 [DOI] [PubMed] [Google Scholar]
- 20.Spaan M, Janssen HL, Boonstra A. Immunology of hepatitis C virus infections. Best Pract Res Clin Gastroenterol (2012) 26(4):391–400. 10.1016/j.bpg.2012.09.005 [DOI] [PubMed] [Google Scholar]
- 21.Gremion C, Cerny A. Hepatitis C virus and the immune system: a concise review. Rev Med Virol (2005) 15(4):235–68. 10.1002/rmv.466 [DOI] [PubMed] [Google Scholar]
- 22.Guidotti LG, Rochford R, Chung J, Shapiro M, Purcell R, Chisari FV. Viral clearance without destruction of infected cells during acute HBV infection. Science (1999) 284(5415):825–9. 10.1126/science.284.5415.825 [DOI] [PubMed] [Google Scholar]
- 23.Bacher P, Scheffold A. Flow-cytometric analysis of rare antigen-specific T cells. Cytometry A (2013) 83(8):692–701. 10.1002/cyto.a.22317 [DOI] [PubMed] [Google Scholar]
- 24.Jenkins MK, Moon JJ. The role of naïve T cell precursor frequency and recruitment in dictating immune response magnitude. J Immunol (2012) 188(9):4135–40 10.4049/jimmunol.1102661 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Thiel A, Scheffold A, Radbruch A. Antigen-specific cytometry – new tools arrived! Clin Immunol (2004) 111(2):155–61. 10.1016/j.clim.2003.12.017 [DOI] [PubMed] [Google Scholar]
- 26.Lefkovits I. Induction of antibody-forming cell clones in microcultures. Eur J Immunol (1972) 2(4):360–6 10.1002/eji.1830020412 [DOI] [PubMed] [Google Scholar]
- 27.Waldmann H, Lefkovits I, Quintans J. Limiting dilution analysis of helper T-cell function. Immunology (1975) 28(6):1135–48. [PMC free article] [PubMed] [Google Scholar]
- 28.Rehermann B, Naoumov NV. Immunological techniques in viral hepatitis. J Hepatol (2007) 46(3):508–20 10.1016/j.jhep.2007.01.002 [DOI] [PubMed] [Google Scholar]
- 29.Thimme R, Bukh J, Spangenberg HC, Wieland S, Pemberton J, Steiger C, et al. Viral and immunological determinants of hepatitis C virus clearance, persistence, and disease. Proc Natl Acad Sci U S A (2002) 99(24):15661–8. 10.1073/pnas.202608299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lyons AB. Analysing cell division in vivo and in vitro using flow cytometric measurement of CFSE dye dilution. J Immunol Methods (2000) 243(1–2):147–54. 10.1016/S0022-1759(00)00231-3 [DOI] [PubMed] [Google Scholar]
- 31.Mueller M, Spangenberg HC, Kersting N, Altay T, Blum HE, Klenerman P, et al. Virus-specific CD4+ T cell responses in chronic HCV infection in blood and liver identified by antigen-specific upregulation of CD154. J Hepatol (2010) 52(6):800–11. 10.1016/j.jhep.2009.12.038 [DOI] [PubMed] [Google Scholar]
- 32.Semmo N, Krashias G, Willberg C, Klenerman P. Analysis of the relationship between cytokine secretion and proliferative capacity in hepatitis C virus infection. J Viral Hepat (2007) 14(7):492–502. 10.1111/j.1365-2893.2007.00842.x [DOI] [PubMed] [Google Scholar]
- 33.Sugimoto K, Ikeda F, Stadanlick J, Nunes FA, Alter HJ, Chang KM. Suppression of HCV-specific T cells without differential hierarchy demonstrated ex vivo in persistent HCV infection. Hepatology (2003) 38(6):1437–48. 10.1053/jhep.2003.09026 [DOI] [PubMed] [Google Scholar]
- 34.Brosterhus H, Brings S, Leyendeckers H, Manz RA, Miltenyi S, Radbruch A, et al. Enrichment and detection of live antigen-specific CD4(+) and CD8(+) T cells based on cytokine secretion. Eur J Immunol (1999) 29(12):4053–9. [DOI] [PubMed] [Google Scholar]
- 35.Manz R, Assenmacher M, Pfluger E, Miltenyi S, Radbruch A. Analysis and sorting of live cells according to secreted molecules, relocated to a cell-surface affinity matrix. Proc Natl Acad Sci U S A (1995) 92(6):1921–5. 10.1073/pnas.92.6.1921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Matsui K, Boniface JJ, Reay PA, Schild H, Fazekas de St Groth B, Davis MM. Low affinity interaction of peptide-MHC complexes with T cell receptors. Science (1991) 254(5039):1788–91. 10.1126/science.1763329 [DOI] [PubMed] [Google Scholar]
- 37.Altman JD, Moss PA, Goulder PJ, Barouch DH, McHeyzer-Williams MG, Bell JI, et al. Phenotypic analysis of antigen-specific T lymphocytes. Science (1996) 274(5284):94–6 10.1126/science.274.5284.94 [DOI] [PubMed] [Google Scholar]
- 38.Buckner JH, Holzer U, Novak EJ, Reijonen H, Kwok WW, Nepom GT. Defining antigen-specific responses with human MHC class II tetramers. J Allergy Clin Immunol (2002) 110(2):199–208. 10.1067/mai.2002.125976 [DOI] [PubMed] [Google Scholar]
- 39.Mardiney M, III, Brown MR, Fleisher TA. Measurement of T-cell CD69 expression: a rapid and efficient means to assess mitogen- or antigen-induced proliferative capacity in normals. Cytometry (1996) 26(4):305–10. [DOI] [PubMed] [Google Scholar]
- 40.Sun S, Zhang X, Tough DF, Sprent J. Type I interferon-mediated stimulation of T cells by CpG DNA. J Exp Med (1998) 188(12):2335–42. 10.1084/jem.188.12.2335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wehler TC, Karg M, Distler E, Konur A, Nonn M, Meyer RG, et al. Rapid identification and sorting of viable virus-reactive CD4(+) and CD8(+) T cells based on antigen-triggered CD137 expression. J Immunol Methods (2008) 339(1):23–37. 10.1016/j.jim.2008.07.017 [DOI] [PubMed] [Google Scholar]
- 42.Wolfl M, Kuball J, Eyrich M, Schlegel PG, Greenberg PD. Use of CD137 to study the full repertoire of CD8+ T cells without the need to know epitope specificities. Cytometry A (2008) 73(11):1043–9. 10.1002/cyto.a.20594 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wolfl M, Kuball J, Ho WY, Nguyen H, Manley TJ, Bleakley M, et al. Activation-induced expression of CD137 permits detection, isolation, and expansion of the full repertoire of CD8+ T cells responding to antigen without requiring knowledge of epitope specificities. Blood (2007) 110(1):201–10. 10.1182/blood-2006-11-056168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Schoenbrunn A, Frentsch M, Kohler S, Keye J, Dooms H, Moewes B, et al. A converse 4-1BB and CD40 ligand expression pattern delineates activated regulatory T cells (Treg) and conventional T cells enabling direct isolation of alloantigen-reactive natural Foxp3+ Treg. J Immunol (2012) 189(12):5985–94. 10.4049/jimmunol.1201090 [DOI] [PubMed] [Google Scholar]
- 45.Keoshkerian E, Helbig K, Beard M, Zaunders J, Seddiki N, Kelleher A, et al. A novel assay for detection of hepatitis C virus-specific effector CD4(+) T cells via co-expression of CD25 and CD134. J Immunol Methods (2012) 375(1–2):148–58. 10.1016/j.jim.2011.10.004 [DOI] [PubMed] [Google Scholar]
- 46.Zaunders JJ, Munier ML, Seddiki N, Pett S, Ip S, Bailey M, et al. High levels of human antigen-specific CD4+ T cells in peripheral blood revealed by stimulated coexpression of CD25 and CD134 (OX40). J Immunol (2009) 183(4):2827–36. 10.4049/jimmunol.0803548 [DOI] [PubMed] [Google Scholar]
- 47.Zaunders JJ, Dyer WB, Wang B, Munier ML, Miranda-Saksena M, Newton R, et al. Identification of circulating antigen-specific CD4+ T lymphocytes with a CCR5+, cytotoxic phenotype in an HIV-1 long-term nonprogressor and in CMV infection. Blood (2004) 103(6):2238–47. 10.1182/blood-2003-08-2765 [DOI] [PubMed] [Google Scholar]
- 48.Frentsch M, Arbach O, Kirchhoff D, Moewes B, Worm M, Rothe M, et al. Direct access to CD4+ T cells specific for defined antigens according to CD154 expression. Nat Med (2005) 11(10):1118–24. 10.1038/nm1292 [DOI] [PubMed] [Google Scholar]
- 49.Mackey MF, Barth RJ, Jr, Noelle RJ. The role of CD40/CD154 interactions in the priming, differentiation, and effector function of helper and cytotoxic T cells. J Leukoc Biol (1998) 63(4):418–28. [DOI] [PubMed] [Google Scholar]
- 50.Roy M, Aruffo A, Ledbetter J, Linsley P, Kehry M, Noelle R. Studies on the interdependence of gp39 and B7 expression and function during antigen-specific immune responses. Eur J Immunol (1995) 25(2):596–603. 10.1002/eji.1830250243 [DOI] [PubMed] [Google Scholar]
- 51.Meier S, Stark R, Frentsch M, Thiel A. The influence of different stimulation conditions on the assessment of antigen-induced CD154 expression on CD4+ T cells. Cytometry A (2008) 73(11):1035–42. 10.1002/cyto.a.20640 [DOI] [PubMed] [Google Scholar]
- 52.Day CL, Seth NP, Lucas M, Appel H, Gauthier L, Lauer GM, et al. Ex vivo analysis of human memory CD4 T cells specific for hepatitis C virus using MHC class II tetramers. J Clin Invest (2003) 112(6):831–42. 10.1172/JCI18509 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Moller JF, Moller B, Wiedenmann B, Berg T, Schott E. CD154, a marker of antigen-specific stimulation of CD4 T cells, is associated with response to treatment in patients with chronic HCV infection. J Viral Hepat (2011) 18(7):e341–9. 10.1111/j.1365-2893.2010.01430.x [DOI] [PubMed] [Google Scholar]
- 54.Bes M, Sauleda S, Casamitjana N, Piron M, Campos-Varela I, Quer J, et al. Reversal of nonstructural protein 3-specific CD4(+) T cell dysfunction in patients with persistent hepatitis C virus infection. J Viral Hepat (2012) 19(4):283–94. 10.1111/j.1365-2893.2011.01549.x [DOI] [PubMed] [Google Scholar]
- 55.Neumann-Haefelin C, Timm J, Spangenberg HC, Wischniowski N, Nazarova N, Kersting N, et al. Virological and immunological determinants of intrahepatic virus-specific CD8+ T-cell failure in chronic hepatitis C virus infection. Hepatology (2008) 47(6):1824–36. 10.1002/hep.22242 [DOI] [PubMed] [Google Scholar]
- 56.Penna A, Missale G, Lamonaca V, Pilli M, Mori C, Zanelli P, et al. Intrahepatic and circulating HLA class II-restricted, hepatitis C virus-specific T cells: functional characterization in patients with chronic hepatitis C. Hepatology (2002) 35(5):1225–36. 10.1053/jhep.2002.33153 [DOI] [PubMed] [Google Scholar]
- 57.Schirren CA, Jung MC, Gerlach JT, Worzfeld T, Baretton G, Mamin M, et al. Liver-derived hepatitis C virus (HCV)-specific CD4(+) T cells recognize multiple HCV epitopes and produce interferon gamma. Hepatology (2000) 32(3):597–603. 10.1053/jhep.2000.9635 [DOI] [PubMed] [Google Scholar]
- 58.Ulmer JB, Donnelly JJ, Parker SE, Rhodes GH, Felgner PL, Dwarki VJ, et al. Heterologous protection against influenza by injection of DNA encoding a viral protein. Science (1993) 259(5102):1745–9. 10.1126/science.8456302 [DOI] [PubMed] [Google Scholar]