Abstract
A chimeric flavivirus infectious cDNA was constructed by exchanging the premembrane (prM) and envelope (E) genes of the yellow fever virus vaccine strain 17D (YF17D) with the corresponding genes of Modoc virus (MOD). This latter virus belongs to the cluster of the “not-known vector” flaviviruses and is, unlike YF17D, neuroinvasive in SCID mice. Replication of in vitro-transcribed RNA from this chimeric flavivirus was shown by [3H]uridine labeling and RNA analysis. Expression of the MOD prM and E proteins was monitored by radioimmunoprecipitation and revealed that the MOD proteins were correctly and efficiently produced from the chimeric precursor protein. The MOD E protein was shown to be N-linked glycosylated, whereas prM, as predicted from the genome sequence, did not contain N-linked carbohydrates. In Vero cells, the chimeric virus replicated with a similar efficiency as the parental viruses, although it formed smaller plaques than YF17D and MOD. In SCID mice that had been infected intraperitoneally with the chimeric virus, the viral load increased steadily until death. The MOD/YF virus, like MOD from which it had acquired the prM and E structural proteins, but unlike YF, proved neuroinvasive in SCID mice. Animals developed neurological symptoms about 15 days after inoculation and died shortly thereafter. The distribution of MOD/YF RNA in the brain of infected mice was similar to that observed in MOD-infected mice. The observations provide compelling evidence that the determinants of neuroinvasiveness of flaviviruses are entirely located in the envelope proteins prM and E.
The flaviviruses (family Flaviviridae) consist of nearly 80 viruses that are distributed worldwide. These small, enveloped viruses contain a single positive-strand RNA genome of ca. 11 kb. Translation of the genome results in the synthesis of a single polyprotein precursor that is co- and posttranslationally processed by cellular proteases and a virus-encoded protease into capsid (C), premembrane (prM) and envelope (E) proteins and the nonstructural (NS) proteins NS1, NS2A, NS2B, NS3, NS4A, NS4B, and NS5 (36). Many flaviviruses are neurotropic, exhibiting various degrees of neuroinvasiveness and neurovirulence in experimentally infected rodents and primates. Both host- and virus-related factors are believed to influence the course of the infection (4).
Yellow fever 17D virus (YF17D), considered to be one of the most effective and safest vaccines available, is neurovirulent, but not neuroinvasive, in adult (SCID) mice. Several studies suggest that the E protein, in particular, plays a dominant role as a determinant of flavivirus neurovirulence, since single amino acid substitutions in the E protein were shown to cause major effects on neurovirulence (reviewed in reference 29). It is not well understood, however, how these various mutations alter the functional properties of the flavivirus E protein and thus increase the particular characteristics of neurovirulence (29).
The mechanisms and determinants underlying the neuroinvasiveness of flaviviruses are even less well understood. To further analyze the role of viral envelope proteins in neuroinvasiveness of flaviviruses in mice, we constructed the first viable chimeric flavivirus between a vector-borne and a not-known vector (NKV) flavivirus. This chimeric flavivirus consists of the genetic backbone of the non-neuroinvasive YF17D of which the prM+E genes have been replaced by the corresponding genes of the highly neuroinvasive Modoc virus (MOD). MOD is a murine flavivirus that was originally isolated from white-footed deer mice (Peromyscus maniculatus) collected in Modoc County, Calif., in 1958 (21). It belongs to the cluster of the NKV flaviviruses (23). The virus is neuroinvasive in immunodeficient (SCID) mice and in immunocompetent hamsters and causes a lethal destruction of neural tissue that, particularly in hamsters, is very much reminiscent of the pathology of flavivirus encephalitis in humans (23-26). At present there is no information available on the particular characteristics of structural proteins expressed by MOD or other NKV flaviviruses.
All chimeric flaviviruses that have been constructed thus far are between two vector-borne flaviviruses. These chimeric flaviviruses have mainly been constructed in an attempt to develop vaccines against flaviviruses that cause disease in humans. Most of these chimeric viruses are derived from the infectious clone of YF17D (44). YF17D has been used as a “vector” for engineering new vaccines against other flaviviruses (e.g., the ChimeriVax vaccines ChimeriVax-JE [9, 37] and ChimeriVax-DEN1, -2, -3, and -4 [13-16] and other chimeras, i.e., WN/YF17D [34, 35] and DEN2/YF17D, that are based on other dengue type 2 virus strains than the one used for ChimeriVax-DEN2 [5, 49]).
We report here on the particular characteristics of the first chimera between a (non-neuroinvasive) virus belonging to the vector-borne cluster and a (neuroinvasive) virus belonging to the NKV cluster. This chimeric virus (i) proved instrumental in obtaining information on the expression and processing of the envelope proteins of an NKV flavivirus and (ii) allowed us to gain further insight into the determinants underlying flavivirus neuroinvasiveness.
MATERIALS AND METHODS
Cells, viruses, and plasmids.
Vero (African green Monkey kidney) cells and MOD were obtained from the American Type Culture Collection (ATCC CCL-81 and VR-415, respectively). BHK-21J (baby hamster kidney) cells (27) were kindly provided by C. M. Rice. YF17D was derived from pACNR-FLYF17Da (2, 33). The construction of the chimeric vector pACNR-MOD/YF containing the full-length MOD/YF cDNA (Fig. 1) by a convenient two-step fusion-PCR technology has recently been described (11).
FIG. 1.
Genomic organization of the MOD/YF17D chimeric virus, that had been constructed by replacing the prM and E genes of YF17D by the homologous genes of MOD (gray box). The amino acid sequence of the hinge regions C/prM and E/NS1 are indicated (the sequence of MOD is underlined; a shill indicates the predicted cleavage site).
RNA transcription and transfection.
Plasmid DNA containing full-length YF or MOD/YF cDNA was linearized with AflII and purified by proteinase K digestion, phenol-chloroform extraction, and ethanol precipitation. Runoff RNA transcripts were produced in vitro by using Sp6 RNA polymerase (11). Transcripts were used for electroporation of BHK-21J cells without any additional purification (50). Cell culture medium was harvested at the time the transfected cells displayed nearly complete cytopathogenicity. Medium was cleared from cell debris by centrifugation and subsequently used to prepare MOD/YF stocks in Vero cells.
Monitoring viral kinetics.
Monolayers of Vero cells were inoculated with 107 PFU of MOD, YF17D, or MOD/YF17D at 37°C in 25-cm2 culture flasks. Cell culture medium was harvested every 2 days (between day 0 and 10) and titrated for infectious virus content on Vero cells. Plaque assays were done on confluent Vero cells as described previously (2). Samples were also analyzed by means of real-time quantitative reverse transcription-PCR (qRT-PCR) (see below).
Metabolic labeling and immunoprecipitation.
After electroporation with YF17D or MOD/YF RNA, BHK cells were seeded in 35-mm tissue culture dishes (2 ml/dish). Alternatively, 106 cells were infected with MOD at a multiplicity of infection of 10. At 18 h posttransfection (postinfection), the medium was replaced by 1 ml of RPMI 1640 medium lacking fetal calf serum, methionine, and cysteine (BioWhittaker). Cells were metabolically labeled for 2 h with 100 μCi of 35S-labeled methionine and cysteine (Promix; Amersham)/ml. Cells were lysed with 1 ml of 50 mM Tris-Cl (pH 7.5), 200 mM NaCl, 1 mM EDTA, 0.5% Triton X-100, and 0.1% sodium dodecyl sulfate (SDS). For immunoprecipitation, 0.5 ml of lysate was mixed with 1 μl of hamster hyperimmune serum Mod1 (serum from hamsters that recovered after infection with MOD). After overnight incubation, immunoprecipitates were collected with Pansorbin (Calbiochem) and washed with 50 mM Tris-Cl (pH 7.5), 200 mM NaCl, 1 mM EDTA, and 0.1% SDS. The immunoprecipitated proteins were split into two samples. One sample was treated overnight at 37°C with endo-β-N-acetylglucosamidase H (EndoH; Boehringer Mannheim), whereas the second sample served as untreated control. Precipitated proteins were analyzed by SDS-polyacrylamide gel electrophoresis (15% gel).
qRT-PCR of MOD, MOD/YF, and YF RNA.
RNA extraction was performed by using the Qiagen Viral RNA kit (Qiagen) according to the manufacturer's instructions. For elution of RNA, the columns were incubated with 50 μl of RNase-free water at 80°C. The samples were normalized by extracting RNA from 140 μl of undiluted serum or culture supernatant. An equal volume of this extracted RNA was used in the qRT-PCR. Primers and probes were designed for MOD/YF17D (sense primer 5′-TGGGTTTTGGTCTTCTAGCTTTCA-3′, antisense primer 5′-CTTGTTCAGCCAGTCATCAGAGTCT-3′, and probe 5′-CAGGAGTGATGGGAAATCAAGGATGC-3′) and YF17D (sense primer 5′-AATCGAGTTGCTAGGCAATAAACAC-3′, antisense primer 5′-TCCCTGAGCTTTACGACCAGA-3′, and probe 5′-ATCGTTCGTTGAGCGATTAGCAG-3′). The probes were labeled with FAM (6-carboxyfluorescein) at the 5′ end and TAMRA (6-carboxy-N,N,N′,N′-tetramethylrhodamine) at the 3′ end. Primers and probe for quantitation of MOD RNA and the reaction conditions for MOD/YF17D, YF17D, and MOD were as reported earlier (26). Thermal cycling in a LightCycler (Roche Molecular Biochemicals, Mannheim, Germany) involved RT at 45°C for 20 min, denaturation at 95°C for 5 min, followed by 45 cycles of 5 s at 95°C and 35 s at 57°C (for YF) or 20 s at 60°C (for MOD and MOD/YF) (12, 51).
Immunofluorescence assay.
BHK-cells that had been transfected with YF17D RNA or MOD/YF RNA or that had been infected with MOD 24 h earlier were fixed in paraformaldehyde and prepared for immunofluorescence essentially as described previously (2). Monoclonal antibody 1A5 (kindly provided by J. J. Schlesinger), which is specific for the YF NS1 protein (47), and Mod1 serum were used to detect the YF NS1 and MOD antigens, respectively.
Animals.
Severe combined immune deficiency (SCID) mice (10 days or 16 weeks old and weighing 16 to 20 g) were used throughout the experiments. All animals were bred at the Rega Institute under specific-pathogen-free conditions. All animal experiments were conducted in accordance with the guidelines of the Ethical Committee on Vertebrate Animal Experiments of the University of Leuven.
Infection of SCID mice with MOD, YF17D, and MOD/YF.
Infection of SCID mice with the parental or chimeric viruses (all passaged on Vero cells) was carried out in a BSL3 facility. Adult SCID mice were inoculated with either 104 PFU of virus via the intraperitoneal route or with 2.5 × 103 PFU via the intracerebral route. The animals were examined daily for signs of morbidity and for mortality. The statistical significance of differences in the mean day of death (MDD) was assessed by means of the Student t test. Every 3 days, three animals were euthanized, blood was collected by cardiac puncture, and total RNA was extracted from the serum and subsequently analyzed by real-time quantitative RT-PCR. To obtain tissue samples for in situ hybridization, mice with severe signs of paralysis were euthanized and transcardially perfused with 20 ml of a buffered 4% formalin solution. Fixed brain samples were embedded in paraffin and further processed by using standard histological procedures or were subjected to in situ hybridization.
Preparation of digoxigenin-labeled cRNA and in situ hybridization.
MOD cDNA encompassing 605 nucleotides of the E region of the MOD genome (sense primer 5′-GGACCCTGGAGAGGGATGGACAA-3′ and antisense primer 5′-CAGATCAAAGATTCTCAGCCATTAATTTGATGGATCT-3′) and YF cDNA encompassing 709 nucleotides of the NS1 region of the YF genome (sense primer 5′-GACTTGGGGTAAGAACCTTGTGTTC-3′ and antisense primer 5′-CTGGTGCGCTCCTGGGTTACAGCT-3′) were each cloned into the transcription vector pGEM-T (Promega, Madison, Wis.). To generate runoff transcripts, the plasmids containing MOD cDNA and YF cDNA were linearized with NcoI and SacII (Promega), respectively. Transcription reactions were carried out as described earlier (10). Paraffin-embedded tissue was sectioned, hydrated, fixed, denatured, and acetylated according to standard procedures (3). In situ hybridization was performed essentially as described before (10).
Sequence analysis.
One-Step RT-PCR (Qiagen) was carried out to obtain DNA fragments of 1 to 2 kb that spanned the entire genome of the virus. Sequence analysis was carried out by using an ABI 373 automatic sequencer (Perkin-Elmer, Applied Biosystems Division, Foster City, Calif.).
RESULTS
Characterization of MOD/YF chimera in cell culture.
Using a fusion-PCR strategy, a full-length MOD/YF cDNA was constructed in the low-copy-number vector pACNR. Details on the construction of this plasmid have been reported (11). In this chimera the prM and E coding regions of YF17D were replaced with the complete prM and E genes of MOD (Fig. 1). Translation of the chimeric RNA should result in the synthesis of MOD/YF precursor protein from which MOD prM and E would be released by a signalase mediated cleavage.
To analyze the replication of this chimeric RNA, BHK-21J cells were electroporated with in vitro transcripts of the full-length MOD/YF cDNA and subsequently labeled with [3H]uridine in the presence of actinomycin D. As shown in Fig. 2A, a labeled RNA molecule with a size similar to that of YF and MOD RNA was detected in the MOD/YF RNA transfected cells, which demonstrates that the chimeric RNA was replication competent.
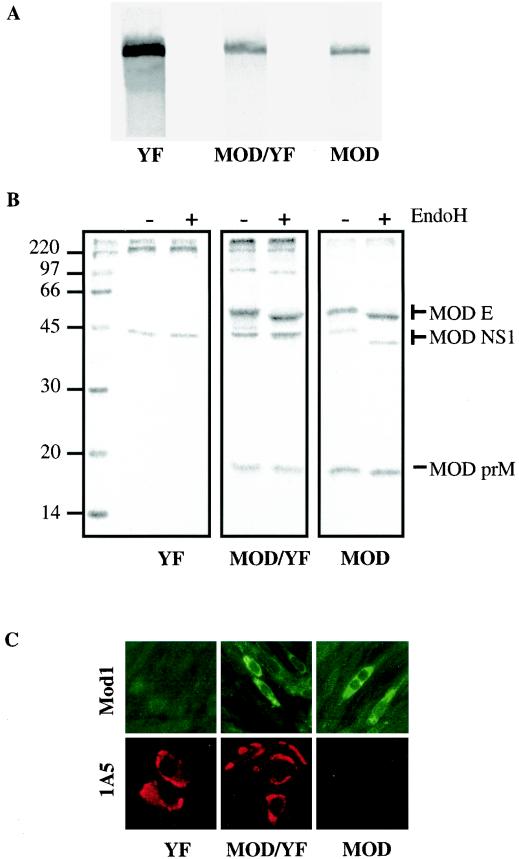
FIG. 2.
(A) Detection of viral RNA replication in Vero cells that had either been transfected with YF17D, MOD/YF17D or that had been infected with MOD. Cultures were labeled with [3H]uridine in the presence of actinomycin D and analyzed by autoradiography. (B) Radioimmunoprecipitation of MOD and YF17D proteins with the polyclonal antiserum Mod1 before and after EndoH treatment. (C) Immunostaining of MOD, YF17D, or MOD/YF17D-infected BHK cells with either monoclonal antiserum 1A5 (directed against the YF NS1 protein) or polyclonal antiserum Mod1 (collected from hamsters 8 months after infection with MOD).
The virus generated by transfection of BHK-21J cells was further cultured in Vero cells for one passage after which the genomic sequence was determined. Compared to the sequence of the chimeric vector, four mutations—prM, Thr144→Ala (MOD); NS2A, Val1294→Met (YF); NS4B, Glu2392→Lys (YF); and 3′-untranslated region (UTR), G10427→A (YF)—were detected in the genome of the chimeric MOD/YF virus obtained from Vero cells.
Immunostainings were performed on Vero cells that had either been infected with the MOD/YF chimera, MOD, or YF. Monoclonal antibodies directed against the YF NS1 protein recognized epitopes in BHK-cells that had been transfected with YF or MOD/YF RNA but did not result in a positive signal in cells transfected with MOD RNA. Conversely, Mod1 antiserum recognized epitopes of the MOD prM, E (and NS1) protein in BHK cells that had been transfected with either MOD or MOD/YF RNA, but did not detect antigens in cells that had been transfected with YF RNA (Fig. 2C).
To study whether the translation of the chimeric MOD/YF RNA resulted in the proper expression of the MOD prM and E proteins, transfected cells were labeled with [35S]methionine, lysed, and used for radioimmunoprecipitation. Since the MOD proteins have never been identified before in cell culture, MOD-infected and YF-RNA transfected cells were used as controls, respectively. As shown in Fig. 2B, the hamster polyclonal anti-MOD serum Mod1 reacted specifically with proteins of 18, 44, and 53 kDa in the lysate of the MOD-infected BHK cells. Treatment with EndoH resulted in a shift of the 53-kDa protein to 51 kDa and of the 44-kDa protein to 39 kDa, whereas the 18-kDa protein was unaffected by EndoH. On the basis of the predicted molecular mass of the unglycosylated MOD proteins, the immunoprecipitated proteins are prM (18 kDa), NS1 (39 kDa), and E (51 kDa), respectively. The results of the EndoH treatment were also consistent with the fact that MOD E and NS1 contain putative N-linked glycosylation sites, whereas prM contains none. The Mod1 antiserum precipitated an ∼40-kDa protein from the lysates of the cells that were transfected with YF transcripts. The molecular mass of this protein indicated that it was unlikely to be a YF protein and therefore probably of host origin. In addition to this presumed host protein, MOD prM and E were precipitated from lysates of cells that were transfected with MOD/YF transcripts. The prM and E proteins expressed by the chimera had a molecular mass and EndoH sensitivity profile similar to those of prM and E in the MOD-infected cells, indicating that the proteins were properly released from the precursor proteins and posttranslationally modified.
Approximately 48 h postelectroporation of the BHK cells with MOD/YF RNA, pronounced cytopathogenic effect was noted. The medium was harvested and used for plaque assay in Vero cells. After incubation for 4 days, the MOD/YF-infected cells showed clear plaques that were however somewhat smaller than those seen with YF. The average size of the MOD/YF plaques was 0.5 mm versus 3 mm for the YF plaques and 2.5 mm for the MOD plaques (Fig. 3A). The kinetics of the replication of the three viruses in infected Vero cells were assessed by means of quantitative RT-PCR. Production of virus (genome) in the supernatant reached a plateau at approximately 6 days postinfection. MOD replicated somewhat more efficiently than YF17D and MOD/YF; the latter two had very comparable kinetics of replication (Fig. 3B). Similar data were obtained in an independent experiment.
FIG. 3.
(A) Plaque morphology of YF17D, MOD, and the MOD/YF17D chimeric virus on Vero cells 4 days after infection; (B) growth kinetics of MOD (▴), YF17D (□) and MOD/YF17D (•) in Vero cells. Quantification of viral RNA in the supernatant was performed (in triplicate) by real-time quantitative RT-PCR (the standard deviation of triplicate determinations was <15% [not shown]). Comparable data were obtained in an independent experiment. (PCRU, PCR-units [one PCR-unit is defined as the lowest template copy number detectable in three of three replicative reactions as determined by limiting dilution series.)
To determine the virion/PFU ratio Vero cells were infected with the chimeric MOD/YF virus, and supernatant was collected at different times postinfection (i.e., at 24, 48, 72, and 96 h). A plaque assay was used to determine the number of PFU of each sample and a qRT-PCR was used to determine the copy numbers of viral RNA. Ratios (copy number/PFU) of 2.4 × 103, 5.3 × 103, 5.8 × 103, and 2.1 × 104, respectively, was calculated on days 1, 2, 3, and 4 postinfection. In time, the ratio increased which can be explained by expanding CPE due to ongoing infection. This results in cell lysis and thus the release of naked intracellular RNA and immature virions in the medium, which will increase the apparent viral load, as determined by the qRT-PCR.
Infection of SCID mice with MOD, YF17D, and MOD/YF.
Intracerebral inoculation of 10-day-old or adult SCID mice with 2.5 × 103 PFU of YF17D, MOD, or chimeric virus caused 100% mortality within 2 weeks postinfection (MDDs of 8.5 ± 0.85, 6.5 ± 0.58, and 9.3 ± 1.56, respectively) (Fig. 4). Morbidity was characterized by ruffled fur, paralysis of the hind legs, and a wasting syndrome. The day of appearance of the first symptoms was approximately 2 days before death for all three viruses.
FIG. 4.
Virus (MOD/YF17D, MOD, or YF17D)-induced mortality (MDDs ± the standard deviations) in SCID mice after intraperitoneal (▪) or intracerebral (░⃞) inoculation. Statistical significant difference in the MDD of the MOD- or YF17D-infected mice compared to the corresponding group of the MOD/YF17D-infected mice are indicated. NS, not significant or P > 0.05.
Next, we studied whether the chimeric virus would be neuroinvasive. To this end, mice were infected intraperitoneally with 104 PFU of YF, MOD and MOD/YF. In contrast to the parental YF17D, but akin to MOD, the MOD/YF chimera proved to be highly neuropathic for both young and adult SCID mice. All (adult) mice developed neurological symptoms (including paralysis) and finally succumbed (MDDs of 16.4 ± 5.37 for MOD/YF and 12.8 ± 1.3 for MOD) (Fig. 4). Intracerebrally MOD/YF-infected animals died significantly later than those infected intracerebrally with MOD. A similar trend (but not significant) was observed for intraperitoneally infected mice. Interestingly, the mice that had been infected with the chimeric virus showed neurological abnormalities only about 24 h before they died, whereas MOD-infected animals presented these symptoms for a period of at least 2 days before they succumbed.
Total RNA was extracted (every 3 days) from the serum of SCID mice that had been infected intraperitoneally with MOD/YF, MOD, or YF and was subjected to a sensitive real-time RT-PCR assay each time with the appropriate primer-probe set to avoid false-positive signals. The viral RNA load in the serum of MOD-infected SCID mice and in the serum of MOD/YF-infected mice increased (steadily) until death. No viral RNA was detected in serum of YF-infected mice (Fig. 5).
FIG. 5.
Detection of viral RNA (by means of real-time qRT-PCR) in sera of SCID mice that had been infected via the intraperitoneal route with the MOD/YF17D chimeric virus (•), MOD (▴), and YF 17D (□). Sera from three mice were collected and pooled every third day after infection (✻, all mice died). Quantification of the viral RNA load was done in triplicate.
The entire nucleotide sequence of the virus isolated from the serum of MOD/YF-infected mice (at 16 days postinfection) was determined. Only a single mutation, more specifically in the prM region (Thr144→Ala), was detected compared to the chimeric virus that was used to infect these mice and that was obtained from Vero cells.
MOD/YF RNA in the brain.
The brain of SCID mice that had been infected intraperitoneally with MOD/YF was dissected at the time the animals had signs of paralysis. The entire sequence of the chimeric virus obtained from this brain tissue was determined and proved to be identical to the virus obtained from serum (see above). The localization of viral RNA was determined by means of in situ hybridization with probes that specifically target either the MOD E region or the YF NS1 region. Viral RNA was detected in the gray matter of the olfactory bulbs, pyriform cortex, temporal lobes (Fig. 6A and B), the midbrain structures (thalamus, hypothalamus) (data not shown), the hippocampus (Fig. 6C), and the medulla oblongata (data not shown). Viral RNA was also detected in the cerebellum where infection of virtually all Purkinje cells was noted (Fig. 6D). Overall, MOD/YF RNA was present in the cytoplasm of infected cells and infection appeared to be confined to the neurons. The brain of SCID mice that had been infected intraperitoneally with MOD or intracerebrally with YF showed no signal with the same YF NS1 probe and MOD E probe that had been used for the detection of MOD/YF RNA in the various brain tissues (data not shown). In situ hybridization with the YF NS1 probe of brain tissue of SCID mice that had been infected intracerebrally with YF resulted in the detection of YF-positive cells throughout the brain. The distribution of infected neurons did not correlate well with that of MOD or MOD/YF, which is, given the fact that YF was infected intracerebrally and MOD and MOD/YF intraperitoneally, not a surprising observation.
FIG. 6.
Localization of MOD/YF17D RNA in the brain of SCID mice at the time of paralysis (15 days postinfection by the intraperitoneal route) by in situ hybridization with a MOD-specific probe. Neurons in the temporal cortex (A [magnification, ×40] and B [magnification, ×10]) and in the hippocampus (C [magnification, ×2.5]), and Purkinje cells in the cerebellum (D [magnification, ×10]).
DISCUSSION
Introduction of the infectious clone technology has opened new opportunities in flavivirus vaccine research. The use of YF17D as a backbone for the construction of chimeric viruses has been applied to the development of new vaccines for Japanese encephalitis virus (JE) and dengue virus (DEN) (9, 15, 16, 37). The rationale for this approach is based on the efficacy and safety of the YF17D vaccine. We report here the characterization of a viable chimeric flavivirus based on the 5′ UTR, C gene, NS genes, and 3′ UTR of the vector-borne YF17D and the prM and E genes of MOD, a flavivirus that belongs to the NKV cluster. The constructed chimeric RNA replicated relatively efficiently in cell culture and directed the production of chimeric virus particles that were infectious for BHK and Vero cells. MOD/YF grew in Vero cells about as efficiently as YF17D. The chimeric virus was neuroinvasive and caused neurodestruction and paralysis in adult immunodeficient (SCID) mice.
As part of the characterization of this chimeric MOD/YF virus in cell culture, we obtained for the first time information about the expression of proteins of NKV flaviviruses, in particular of MOD. The MOD prM, E, and NS1 proteins have molecular masses of, respectively 18, 53, and 44 kDa. As expected on the basis of the translation of the MOD nucleotide sequence (23), it was shown that both the MOD E and NS1 protein were N-linked glycosylated. For the MOD E protein, three potential N-linked glycosylation sites at amino acid positions 426, 598, and 731, respectively, were predicted. Given the relative shift in mobility after treatment of the immunoprecipitated MOD E, it appears that only one of these sites is actually used for glycosylation, most likely the glycosylation site at position 427 (sequence N-V-S). The site at position 599 has the sequence N-D-T which is often a poor acceptor for N-linked glycans (22), whereas the potential glycosylation site at position 732 (N-F-S) is unlikely to be used because it is located in the hydrophobic carboxyl-terminal domain of the E protein and is likely to be buried in the RER membrane.
The MOD NS1 protein contains two potential N-linked glycosylation sites. Although mutational analysis may be required to provide a definitive answer, detailed measurements on the shifts in mobility between native and EndoH-treated NS1 suggests that both glycosylation sites are used for the addition of N-linked glycans. The MOD prM was not modified by N-linked glycosylation, which is in agreement with the sequence prediction. This is quite unique since prM of all other flaviviruses studied thus far (all of which belong to the vector-borne cluster) (reviewed in reference 7) were shown to be modified by the addition of N-linked glycans. Also, analysis of the amino acid sequences of the prM gene of Montana Myotis leukoencephalitis virus, Rio Bravo virus, and Apoi virus (which, together with MOD, belong to the NKV cluster) revealed the presence of potential sites for N-linked glycosylation of prM of these viruses.
The prM and E proteins expressed by the MOD/YF virus appear to have the same molecular weight and EndoH profile as their counterparts expressed by MOD. This indicates that the prM and E are released by signalase at the predicted fusion sequences from the recombinant YF-MOD-YF precursor protein. This cleavage appears to occur efficiently since no MOD prM or E containing precursor was detected in pulse-chase experiments in cells transfected with MOD/YF transcripts (data not shown). The kinetics of replication of the chimeric MOD/YF virus was very comparable to that of YF17D and MOD. However, the average size of the MOD/YF plaques was five to six times smaller than the MOD plaques and the YF plaques, respectively. This observation may suggest that there exists a relative “incompatibility” between the prM+E genes and other genes in the chimeric virus that may have an impact on the ability of the chimeric virus to replicate and spread in cell culture.
We used the MOD/YF to gain further insight into the mechanism underlying neuroinvasiveness of flaviviruses. The MOD/YF chimeric virus contains in the genome of a non-neuroinvasive virus (YF17D) the prM and E genes of a virus that is highly neurotropic for mice (i.e., MOD).
The flavivirus major envelope glycoprotein E appears to be an important determinant of neurovirulence in animals (36). However, little is known about the determinants of neuroinvasiveness of flaviviruses. Halevy et al. (17) showed that loss of neuroinvasiveness of West Nile virus (WN) in ICR mice correlates with the acquisition of an N-linked glycosylation site in the E protein (17). It was later shown that glycosylation was not the primary cause loss of neuroinvasiveness of WN in mice; a second mutation (Leu68→Pro) within the E protein sequence was also shown to be involved (8). A number of authors have demonstrated that loss of neuroinvasiveness can be achieved by introducing specific amino acid substitutions within the E protein of flaviviruses, i.e., for YF17D, JE, Murray Valley encephalitis virus, Langat virus (LGT), tick-borne encephalitis virus (TBE), and louping ill virus (1, 6, 8, 18-20, 28, 30-32, 38-41, 45, 46, 48). It can, however, not be excluded that other regions within the flavivirus genome are important in the attenuation of neuroinvasion. When a non-neuroinvasive mutant of WN with a mutation in the E protein reverted to the parental E sequence, the parental neuroinvasive phenotype proved only partially neuroinvasive (8).
A chimeric DEN4, containing the envelope glycoproteins of TBE, was, in contrast to the parental TBE, not neuroinvasive in adult BALB/c mice (41). These findings suggested that determinants other than prM and E may contribute to the neuroinvasive properties of TBE, or, alternatively, that the prM+E genes of TBE do not suffice to cause neuroinvasiveness in the context of the DEN4 genome. Similar observations were made with chimeric viruses that consist of the DEN4 backbone and the prM+E genes of LGT. LGT (strain TP21) is neuroinvasive in Swiss mice and SCID mice, whereas the chimeric LGT(TP21)/DEN virus was not (42). Also, chimeric WN/DEN4 viruses lost the neuroinvasive properties of WN from which they had obtained the prM+E genes (43). Exchanging the prM and E genes of YF (which is non-neuroinvasive) with the homologous genes of a neuroinvasive flavivirus, i.e., JE, did not result in a virus that was neuroinvasive in adult ICR mice. However, using this JE/YF chimeric virus, neuroinvasiveness was observed in 20% of the infected mice if C57BL/6 mice were used instead of ICR mice (9). This indicates that strain-specific differences in the susceptibility of mice to chimeric flaviviruses may have an impact on the neuroinvasive properties of the virus.
MOD causes neurological symptoms and death in 100% of adult SCID mice that have been infected peripherally (26). The YF17D vaccine strain is neurovirulent in adult SCID mice (16) but not neuroinvasive in SCID mice older than 3 days of age (unpublished observations). Akin to the parental YF17D and MOD, the chimeric MOD/YF reported here proved neurovirulent in adult SCID mice. Because of the absence of functional B and T cells in SCID mice, the neurological symptoms must be caused by dysfunction and destruction of neurons, as shown for MOD (25), and not be an inflammatory component. According to the aforementioned studies in which the prM+E of neuroinvasive viruses such as WN, JE, and LGT were not able to transfer the neuroinvasive phenotype one would predict the MOD/YF to be not neuroinvasive. However, unlike the parent YF(17D) strain, and akin to MOD from which it had acquired the prM and E genes, the chimeric MOD/YF was neuroinvasive in 100% of the infected SCID mice. The chimeric virus obtained from the brain (and serum) differed only in one amino acid from the virus obtained from Vero cells. This mutation was located in the N-terminal part of prM. During maturation of the viral particles, this part is cleaved off and does therefore not cooperate in the infection. It is therefore unlikely that this mutation would play a role in the neuroinvasive properties of this chimeric virus. The distribution of viral RNA in the brain was very similar to the situation in MOD-infected mice (26), indicating that the MOD prM+E directs, in addition to the spread of the virus from the periphery to the brain, the localization of the replication in the brain.
Our findings, together with earlier published observations that mutations within E can destroy the neuroinvasive properties of a flavivirus, provide compelling evidence that the flavivirus envelope proteins are the principal determinants of neuroinvasiveness and thus attest that the characteristics of neuroinvasiveness of the donor of prM and E genes are conferred to the receiving virus. This information may be instrumental to further understand the molecular basis of flavivirus neuroinvasiveness and may have implications for engineering live attenuated chimeric vaccines.
Acknowledgments
We thank J. J. Schlesinger for kindly providing the anti-YF NS1 monoclonal antibody and W. Zeegers for excellent technical assistance with the animal experiments.
N.C. and P.L. are postdoctoral research fellows from the Research Council of the K.U. Leuven. J.P. is a research fellow from the Instituut voor Wetenschappelijk Onderzoek and Technologie (IWT/SB/13148/Paeshuyse). This study was supported by a grant from the Geconcerteerde Onderzoeksacties-Vlaamse Gemeenschap (project 00/12) and the Fonds voor Wetenschappelijk Onderzoek-Vlaanderen (G. 0122-00). R.M. was supported by the EU FP5 grant QLK2-1999-00356.
REFERENCES
- 1.Bray, M., R. Men, I. Tokimatsu, and C. J. Lai. 1998. Genetic determinants responsible for acquisition of dengue type 2 virus mouse neurovirulence. J. Virol. 72:1647-1651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bredenbeek, P. J., E. A. Kooi, B. Lindenbach, N. Huijkman, C. M. Rice, and W. J. Spaan. 2003. A stable full-length yellow fever virus cDNA clone and the role of conserved RNA elements in flavivirus replication. J. Gen. Virol. 84:1261-1268. [DOI] [PubMed] [Google Scholar]
- 3.Breitschopf, H., G. Suchanek, R. M. Gould, D. R. Colman, and H. Lassmann. 1992. In situ hybridization with digoxigenin-labeled probes: sensitive and reliable detection method applied to myelinating rat brain. Acta Neuropathol. 84:581-587. [DOI] [PubMed] [Google Scholar]
- 4.Burke, D. S., and T. P. Monath. 2001. Flaviviruses, p. 1043-1125. In D. M. Knipe and P. M. Howley (ed.), Fields virology, 4th ed. Lippincott/The Williams & Wilkins Co., Philadelphia, Pa.
- 5.Caufour, P. S., M. C. Motta, A. M. Yamamura, S. Vazquez, I. I. Ferreira, A. V. Jabor, M. C. Bonaldo, M. S. Freire, and R. Galler. 2001. Construction, characterization, and immunogenicity of recombinant yellow fever 17D-dengue type 2 viruses. Virus Res. 79:1-14. [DOI] [PubMed] [Google Scholar]
- 6.Cecilia, D., and E. A. Gould. 1991. Nucleotide changes responsible for loss of neuroinvasiveness in Japanese encephalitis virus neutralization-resistant mutants. Virology 181:70-77. [DOI] [PubMed] [Google Scholar]
- 7.Chambers, T. J., C. S. Hahn, R. Galler, and C. M. Rice. 1990. Flavivirus genome organization, expression, and replication. Annu. Rev. Microbiol. 44:649-688. [DOI] [PubMed] [Google Scholar]
- 8.Chambers, T. J., M. Halevy, A. Nestorowicz, C. M. Rice, and S. Lustig. 1998. West Nile virus envelope proteins: nucleotide sequence analysis of strains differing in mouse neuroinvasiveness. J. Gen. Virol. 79:2375-2380. [DOI] [PubMed] [Google Scholar]
- 9.Chambers, T. J., A. Nestorowicz, P. W. Mason, and C. M. Rice. 1999. Yellow fever Japanese encephalitis chimeric viruses: construction and biological properties. J. Virol. 73:3095-3101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Charlier, N., P. Leyssen, J. Paeshuyse, C. Drosten, H. Schmitz, A. Van Lommel, E. De Clercq, and J. Neyts. 2002. Infection of SCID mice with Montana Myotis leukoencephalitis virus as a model for flavivirus encephalitis. J. Gen. Virol. 83:1887-1896. [DOI] [PubMed] [Google Scholar]
- 11.Charlier, N., R. Molenkamp, P. Leyssen, A. M. Vandamme, E. De Clercq, P. Bredenbeek, and J. Neyts. 2003. A rapid and convenient variant of fusion-PCR to construct chimeric flaviviruses. J. Virol. Methods 108:67-74. [DOI] [PubMed] [Google Scholar]
- 12.Drosten, C., S. Gottig, S. Schilling, M. Asper, M. Panning, H. Schmitz, and S. Gunther. 2002. Rapid detection and quantification of RNA of Ebola and Marburg viruses, Lassa virus, Crimean-Congo hemorrhagic fever virus, Rift Valley fever virus, dengue virus, and yellow fever virus by real-time reverse transcription-PCR. J. Clin. Microbiol. 40:2323-2330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Guirakhoo, F., J. Arroyo, K. V. Pugachev, C. Miller, Z. X. Zhang, R. Weltzin, K. Georgakopoulos, J. Catalan, S. Ocran, K. Soike, M. Ratterree, and T. P. Monath. 2001. Construction, safety, and immunogenicity in nonhuman primates of a chimeric yellow fever-dengue virus tetravalent vaccine. J. Virol. 75:7290-7304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Guirakhoo, F., K. Pugachev, J. Arroyo, C. Miller, Z. X. Zhang, R. Weltzin, K. Georgakopoulos, J. Catalan, S. Ocran, K. Draper, and T. P. Monath. 2002. Viremia and immunogenicity in nonhuman primates of a tetravalent yellow fever-dengue chimeric vaccine: genetic reconstructions, dose adjustment, and antibody responses against wild-type dengue virus isolates. Virology 298:146-159. [DOI] [PubMed] [Google Scholar]
- 15.Guirakhoo, F., R. Weltzin, T. J. Chambers, Z. X. Zhang, K. Soike, M. Ratterree, J. Arroyo, K. Georgakopoulos, J. Catalan, and T. P. Monath. 2000. Recombinant chimeric yellow fever-dengue type 2 virus is immunogenic and protective in nonhuman primates. J. Virol. 74:5477-5485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Guirakhoo, F., Z. X. Zhang, T. J. Chambers, S. Delagrave, J. Arroyo, A. D. Barrett, and T. P. Monath. 1999. Immunogenicity, genetic stability, and protective efficacy of a recombinant, chimeric yellow fever-Japanese encephalitis virus (ChimeriVax-JE) as a live, attenuated vaccine candidate against Japanese encephalitis. Virology 257:363-372. [DOI] [PubMed] [Google Scholar]
- 17.Halevy, M., Y. Akov, N. D. Ben, D. Kobiler, B. Lachmi, and S. Lustig. 1994. Loss of active neuroinvasiveness in attenuated strains of West Nile virus: pathogenicity in immunocompetent and SCID mice. Arch. Virol. 137:355-370. [DOI] [PubMed] [Google Scholar]
- 18.Hasegawa, H., M. Yoshida, T. Shiosaka, S. Fujita, and Y. Kobayashi. 1992. Mutations in the envelope protein of Japanese encephalitis virus affect entry into cultured cells and virulence in mice. Virology 191:158-165. [DOI] [PubMed] [Google Scholar]
- 19.Holzmann, H., F. X. Heinz, C. W. Mandl, F. Guirakhoo, and C. Kunz. 1990. A single amino acid substitution in envelope protein E of tick-borne encephalitis virus leads to attenuation in the mouse model. J. Virol. 64:5156-5159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jiang, W. R., A. Lowe, S. Higgs, H. Reid, and E. A. Gould. 1993. Single amino acid codon changes detected in louping ill virus antibody-resistant mutants with reduced neurovirulence. J. Gen. Virol. 74(Pt. 5):931-935. [DOI] [PubMed] [Google Scholar]
- 21.Johnson, H. N. 1967. Ecological implications of antigenically related mammalian viruses for which arthropod vectors are unknown and avian associated soft tick viruses. Jpn. J. Med. Sci. Biol. 20:160-166. [PubMed] [Google Scholar]
- 22.Kornfeld, R., and S. Kornfeld. 1985. Assembly of asparagine-linked oligosaccharides. Annu. Rev. Biochem. 54:631-664. [DOI] [PubMed] [Google Scholar]
- 23.Leyssen, P., N. Charlier, P. Lemey, F. Billoir, A.-M. Vandamme, E. De Clercq, X. de Lamballerie, and J. Neyts. 2002. Complete genome sequence, taxonomic assignment, and comparative analysis of the untranslated regions of the Modoc virus, a flavivirus with no known vector. Virology 239:125-140. [DOI] [PubMed] [Google Scholar]
- 24.Leyssen, P., R. Croes, P. Rau, S. Heiland, E. Verbeken, R. Sciot, J. Paeshuyse, N. Charlier, E. De Clercq, U. Meyding-Lamade, and J. Neyts. 2003. Acute encephalitis, a poliomyelitis-like syndrome and neurological sequelae in a hamster model for flavivirus infections. Brain Pathol. 13:279-290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Leyssen, P., J. Paeshuyse, N. Charlier, A. Van Lommel, C. Drosten, E. De Clercq, and J. Neyts. 2003. Impact of direct virus-induced neuronal dysfunction and immunological damage on the progression of flavivirus (Modoc) encephalitis in a murine model. J. Neurovirol. 9:69-78. [DOI] [PubMed] [Google Scholar]
- 26.Leyssen, P., A. Van Lommel, C. Drosten, H. Schmitz, E. De Clercq, and J. Neyts. 2001. A novel model for the study of the therapy of Flavivirus infections using the Modoc virus. Virology 279:27-37. [DOI] [PubMed] [Google Scholar]
- 27.Lindenbach, B. D., and C. M. Rice. 1997. Trans-complementation of yellow fever virus NS1 reveals a role in early RNA replication. J. Virol. 71:9608-9617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mandl, C. W., S. L. Allison, H. Holzmann, T. Meixner, and F. X. Heinz. 2000. Attenuation of tick-borne encephalitis virus by structure-based site-specific mutagenesis of a putative flavivirus receptor binding site. J. Virol. 74:9601-9609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.McMinn, P. C. 1997. The molecular basis of virulence of the encephalitogenic flaviviruses. J. Gen. Virol. 78:2711-2722. [DOI] [PubMed] [Google Scholar]
- 30.McMinn, P. C., L. Dalgarno, and R. C. Weir. 1996. A comparison of the spread of Murray Valley encephalitis viruses of high or low neuroinvasiveness in the tissues of Swiss mice after peripheral inoculation. Virology 220:414-423. [DOI] [PubMed] [Google Scholar]
- 31.McMinn, P. C., E. Lee, S. Hartley, J. T. Roehrig, L. Dalgarno, and R. C. Weir. 1995. Murray valley encephalitis virus envelope protein antigenic variants with altered hemagglutination properties and reduced neuroinvasiveness in mice. Virology 211:10-20. [DOI] [PubMed] [Google Scholar]
- 32.McMinn, P. C., I. D. Marshall, and L. Dalgarno. 1995. Neurovirulence and neuroinvasiveness of Murray Valley encephalitis virus mutants selected by passage in a monkey kidney cell line. J. Gen. Virol. 76:865-872. [DOI] [PubMed] [Google Scholar]
- 33.Molenkamp, R., E. A. Kooi, M. A. Lucassen, S. Greve, J. C. Thijssen, W. J. Spaan, and P. J. Bredenbeek. 2003. Yellow fever virus replicons as an expression system for hepatitis C virus structural proteins. J. Virol. 77:1644-1648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Monath, T. P. 2001. Prospects for development of a vaccine against the West Nile virus. Ann. N. Y. Acad. Sci. 951:1-12. [DOI] [PubMed] [Google Scholar]
- 35.Monath, T. P., J. Arroyo, C. Miller, and F. Guirakhoo. 2001. West Nile virus vaccine. Curr. Drug Targets Infect. Disord. 1:37-50. [DOI] [PubMed] [Google Scholar]
- 36.Monath, T. P., and F. X. Heinz. 1996. Flaviviruses, p. 961-1034. In B. N. Fields, D. M. Knipe, and P. M. Howley (ed.), Fields virology, 3rd ed. Lippincott-Raven Publishers, Philadelphia, Pa.
- 37.Monath, T. P., K. Soike, I. Levenbook, Z. X. Zhang, J. Arroyo, S. Delagrave, G. Myers, A. T. Barrett, R. E. Shope, M. Ratterree, T. J. Chambers, and F. Guirakhoo. 1999. Recombinant, chimaeric live, attenuated vaccine (ChimeriVax[trade]) incorporating the envelope genes of Japanese encephalitis (SA14-14-2) virus and the capsid and nonstructural genes of yellow fever (17D) virus is safe, immunogenic and protective in nonhuman primates. Vaccine 17:1869-1882. [DOI] [PubMed] [Google Scholar]
- 38.Ni, H., and A. D. Barrett. 1996. Molecular differences between wild-type Japanese encephalitis virus strains of high and low mouse neuroinvasiveness. J. Gen. Virol. 77(Pt. 7):1449-1455. [DOI] [PubMed] [Google Scholar]
- 39.Nickells, M., and T. J. Chambers. 2003. Neuroadapted yellow fever virus 17D: determinants in the envelope protein govern neuroinvasiveness for SCID mice. J. Virol. 77:12232-12242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Pletnev, A. G. 2001. Infectious cDNA clone of attenuated Langat tick-borne flavivirus (strain E5) and a 3′ deletion mutant constructed from it exhibit decreased neuroinvasiveness in immunodeficient mice. Virology 282:288-300. [DOI] [PubMed] [Google Scholar]
- 41.Pletnev, A. G., M. Bray, and C. J. Lai. 1993. Chimeric tick-borne encephalitis and dengue type 4 viruses: effects of mutations on neurovirulence in mice. J. Virol. 67:4956-4963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Pletnev, A. G., G. G. Karganova, T. I. Dzhivanyan, V. A. Lashkevich, and M. Bray. 2000. Chimeric Langat/Dengue viruses protect mice from heterologous challenge with the highly virulent strains of tick-borne encephalitis virus. Virology 274:26-31. [DOI] [PubMed] [Google Scholar]
- 43.Pletnev, A. G., R. Putnak, J. Speicher, E. J. Wagar, and D. W. Vaughn. 2002. West Nile virus/dengue type 4 virus chimeras that are reduced in neurovirulence and peripheral virulence without loss of immunogenicity or protective efficacy. Proc. Natl. Acad. Sci. USA 99:3036-3041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Rice, C. M., A. Grakoui, R. Galler, and T. J. Chambers. 1989. Transcription of infectious yellow fever RNA from full-length cDNA templates produced by in vitro ligation. New Biol. 1:285-296. [PubMed] [Google Scholar]
- 45.Ryman, K. D., T. N. Ledger, G. A. Campbell, S. J. Watowich, and A. D. Barrett. 1998. Mutation in a 17D-204 vaccine substrain-specific envelope protein epitope alters the pathogenesis of yellow fever virus in mice. Virology 244:59-65. [DOI] [PubMed] [Google Scholar]
- 46.Ryman, K. D., H. Xie, T. N. Ledger, G. A. Campbell, and A. D. Barrett. 1997. Antigenic variants of yellow fever virus with an altered neurovirulence phenotype in mice. Virology 230:376-380. [DOI] [PubMed] [Google Scholar]
- 47.Schlesinger, J. J., M. W. Brandriss, and T. P. Monath. 1983. Monoclonal antibodies distinguish between wild and vaccine strains of yellow fever virus by neutralization, hemagglutination inhibition, and immune precipitation of the virus envelope protein. Virology 125:8-17. [DOI] [PubMed] [Google Scholar]
- 48.Sumiyoshi, H., G. H. Tignor, and R. E. Shope. 1995. Characterization of a highly attenuated Japanese encephalitis virus generated from molecularly cloned cDNA. J. Infect. Dis. 171:1144-1151. [DOI] [PubMed] [Google Scholar]
- 49.van der Most, R. G., K. Murali-Krishna, R. Ahmed, and J. H. Strauss. 2000. Chimeric yellow fever/dengue virus as a candidate dengue vaccine: quantitation of the dengue virus-specific CD8 T-cell response. J. Virol. 74:8094-8101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.van Dinten, L. C., J. A. den Boon, A. L. Wassenaar, W. J. Spaan, and E. J. Snijder. 1997. An infectious arterivirus cDNA clone: identification of a replicase point mutation that abolishes discontinuous mRNA transcription. Proc. Natl. Acad. Sci. USA 94:991-996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wittwer, C. T., K. M. Ririe, R. V. Andrew, D. A. David, R. A. Gundry, and U. J. Balis. 1997. The LightCycler: a microvolume multisample fluorimeter with rapid temperature control. BioTechniques 22:176-181. [DOI] [PubMed] [Google Scholar]