Abstract
Iron oxide nanoparticles (IONPs) are chemically inert materials and have been mainly used for imaging applications and drug deliveries. However, the possibility whether they can be used as therapeutic drugs themselves has not yet been explored. We reported here that Fe2O3 nanoparticles (NPs) can protect hearts from ischemic damage at the animal, tissue and cell level. The cardioprotective activity of Fe2O3 NPs requires the integrity of nanoparticles and is not dependent upon their surface charges and molecules that were integrated into nanoparticles. Also, Fe2O3 NPs showed no significant toxicity towards normal cardiomyocytes, indicative of their potential to treat cardiovascular diseases.
Cardiovascular disease is the leading cause of death worldwide and the deaths have increased at a fast rate1. Myocardial ischemia, caused by lack of blood flow to the heart, is the most common and primary cause of myocardium damage. This, in turn, leads to myocardial hypoxia. Myocardial ischemia and hypoxia can cause coronary artery heart disease, angina pectoris, even myocardial infarction. Treatment for myocardial ischemic injury is timely and effective myocardial reperfusion for improving blood flow to the heart muscle. However, the process of reperfusion can in itself paradoxically inflict further injury to the myocardium, including cardiomyocyte death, arrhythmia2, even cardiac rupture3. A variety of pharmaceutical drugs have been investigated, including oxygen free radical scavengers, antioxidants, calcium channel blockers, anti-apoptotic agents and so forth. Myocardial injury is associated with multiple pathological mechanisms, while a pharmacologically active compound fights only one of them. Therefore there is still no proven effective therapy3.
IONPs, including Fe2O3 and Fe3O4 NPs, have been extensively used as medical diagnostic agents4, drug carriers5, hyperthermia for cancer treatment6, separation tools7, and cancer diagnoses and therapies. IONPs are generally considered as inert materials. Thus, to endow these NPs with biological properties, they are often bound to certain biologically active molecules such as antibodies, drugs, and DNAs to create nano-composites. Interestingly, it has been recently reported that Fe3O4 NPs in a catalytic reaction in vitro show a peroxidase-like activity in a manner depending upon sizes in a range from 30 to 300 nm8. After that, a dual enzyme (peroxidase and catalase-like) activities of IONPs in vitro were reported and the relative potency of Fe3O4 NPs is higher than that of Fe2O3 NPs9. However, it is unclear whether IONPs themselves can actually be used as a drug to treat diseases. Here, we reported that 2, 3-dimercaptosuccinic acid modified Fe2O3 NPs (Fe2O3@DMSA NPs) in a range of small sizes exhibit a cardioprotective activity in vitro and in vivo. We also compared the activity with those of Verapamil (calcium channel blockers) and Salvia miltiorrhiza extract (antioxidant), two drugs that have been extensively used as cardioprotective drugs in the treatment of angina pectoris, coronary artery heart disease and so on10,11,12. Our data suggest that these NPs have a clinically potential to treat cardiovascular diseases.
Results
Cardioprotection of Fe2O3@DMSA NPs
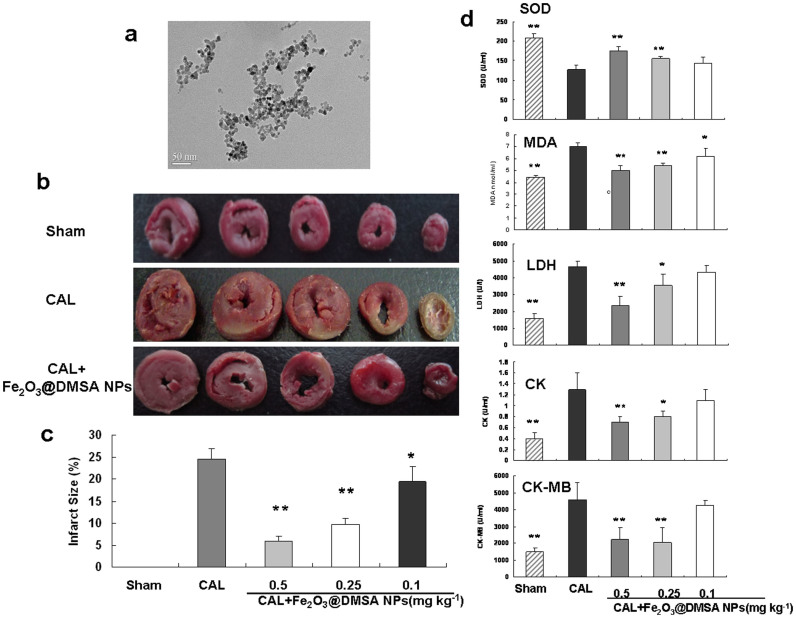
We prepared Fe2O3@DMSA NPs by a co-precipitation method. The prepared NPs have a spherical core with an average diameter of 9.8 nm as measured by TEM (Fig. 1a). To analyze the potential ability of NPs to protect cardiac, the effect of NPs on the size of myocardial infarct and biochemical indexes were investigated at animal level by using a rat coronary artery ligature (CAL) model. The Sprague-Dawley rats were injected with Fe2O3@DMSA NPs (CAL + Fe2O3@DMSA NPs group, 0.1, 0.25, 0.5 mg Fe kg−1) or normal saline solution (CAL group) via tail veins once-a-day before induction of injury by CAL surgery. Fe2O3@DMSA NPs-treated rats had infarct regions significantly smaller than did the normal saline-treated group after 30 min of injury (Fig. 1b). The Fe2O3@DMSA NPs-mediated improvement was also dose-dependent with a highest improvement at 0.5 mg kg−1. To verify the protection, we measured several biochemcial indexes in serum, including the levels of superoxide dismutase (SOD), malondialdehyde (MDA), lactate dehydrogenase (LDH), creatine kinase (CK) and creatine kinase isoenzyme-MB (CK-MB). The SOD activity of the Fe2O3@DMSA NPs-treated rats at 0.5 and 0.25 mg kg−1 doses was significantly higher than that of the normal saline-treated rats. The activities of MDA, LDH, CK, and CK-MB and the content of MDA in Fe2O3@DMSA NPs-treated rats at the same doses were also significantly lower than those of the normal saline-treated rats. These results demonstrated that Fe2O3@DMSA NPs protected myocardium from ischemia injury at animal level.
Figure 1. Fe2O3@DMSA NPs protected coronary artery ligature (CAL) induced injury in rats.
(a) TEM image of Fe2O3@DMSA NPs of 9.8 nm. (b) Representative images for heart sections (stained with triphenyltetrazolium chloride solution) derived from the sham-operated control (Sham), normal saline-treated (CAL) and Fe2O3@DMSA NPs-treated (CAL + Fe2O3@DMSA NPs) rats at 0.25 mg kg−1. (c) Quantification of the size of heart infarcts of sham-operated control, normal saline- and Fe2O3@DMSA NPs-treated rats. (d) Quantification of several serum index (SOD, MDA, LDH, CK, and CK-MB) of sham-operated control, normal saline- and Fe2O3@DMSA NPs-treated rats. * p < 0.05 vs the CAL group; ** p < 0.01 vs the CAL group; n = 8.
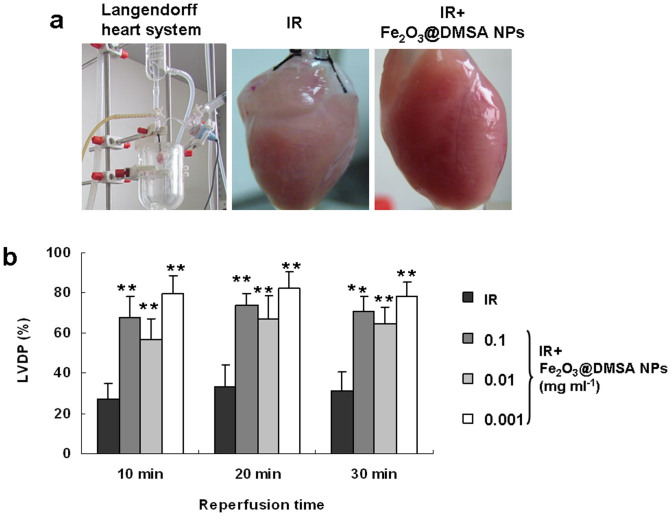
To confirm the cardioprotective activity of Fe2O3@DMSA NPs, we prepared Guinea pig Langendorff heart (Fig. 2a), a widely used model at tissue level for assessing potential cardiovascular drugs. The perfused hearts were subjected to ischemia and reperfusion (IR) with or without Fe2O3@DMSA NPs. The treatment with Fe2O3@DMSA NPs did not change the heart rate significantly during reperfusion. However, compared with the untreated hearts (IR group), the hearts treated with Fe2O3@DMSA NPs (IR + Fe2O3@DMSA group) at 0.001–0.1 mg ml−1 within 30 min of reperfusion exhibited a significant recovery in the left ventricular developed pressure (LVDP) (Fig. 2b). Also, while the untreated hearts looked pale, the Fe2O3@DMSA NPs-treated hearts were ruddy and seemed to be normal in color (Fig. 2a middle and right).
Figure 2. Fe2O3@DMSA NPs have a caridoprotective activity in guinea pig Langendorff heart following 30 min of ischemia and 30 min of reperfusion (IR).
(a) The Langendorff heart system (left), a heart perfused without (IR, middle) and with 0.001 mg ml−1 of Fe2O3@DMSA NPs (IR + Fe2O3@DMSA NPs, right) after ischemia. (b) LVDPs were recorded with perfused hearts without and with 0.1, 0.01 and 0.001 mg ml−1 of Fe2O3@DMSA NPs at 10, 20 and 30 min after perfusion. ** p < 0.01 vs the IR group; n = 6.
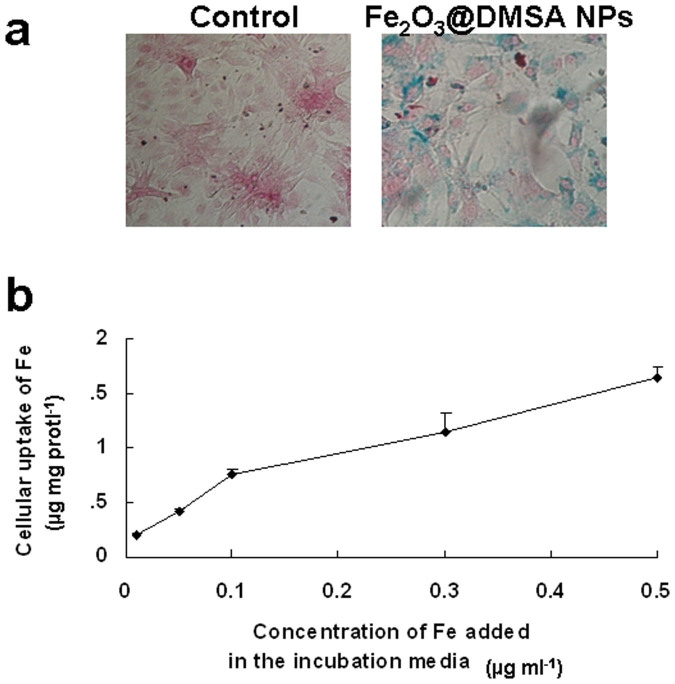
To further understand the Fe2O3@DMSA NPs-induced cardioprotective activity, we investigated the effect of Fe2O3@DMSA NPs on neonatal rat cardiomyocytes. Cardiomyocytes were cultured without (control group) and with of NPs for 24 h, and cellular Fe2O3@DMSA NPs were visualized by Prussian blue staining (Fig. 3a). The uptake of NPs was apparently dose-dependent as detected by potassium ferrocyanide colorimetric assay (Fig. 3b). The viability of cardiomyocytes incubated with 0.01, 0.1 and 0.5 mg ml−1 of NPs was 94.0 ± 9.2, 94.6 ± 9.2 and 96.2 ± 7.1%, respectively. No significant difference (p > 0.05) of cell viability between 0 and 0.01–0.5 mg ml−1 of NPs was detected, indicating that the NPs at those doses were non-toxic to normal cardiomyocytes.
Figure 3. The uptake of Fe2O3@DMSA NPs by cardiomyocytes.
(a) Prussian blue staining of cardiomyocytes incubated without (control) and with 0.1 mg ml−1 of Fe2O3@DMSA NPs. (b) The uptake of Fe2O3@DMSA NPs at different doses (n = 6).
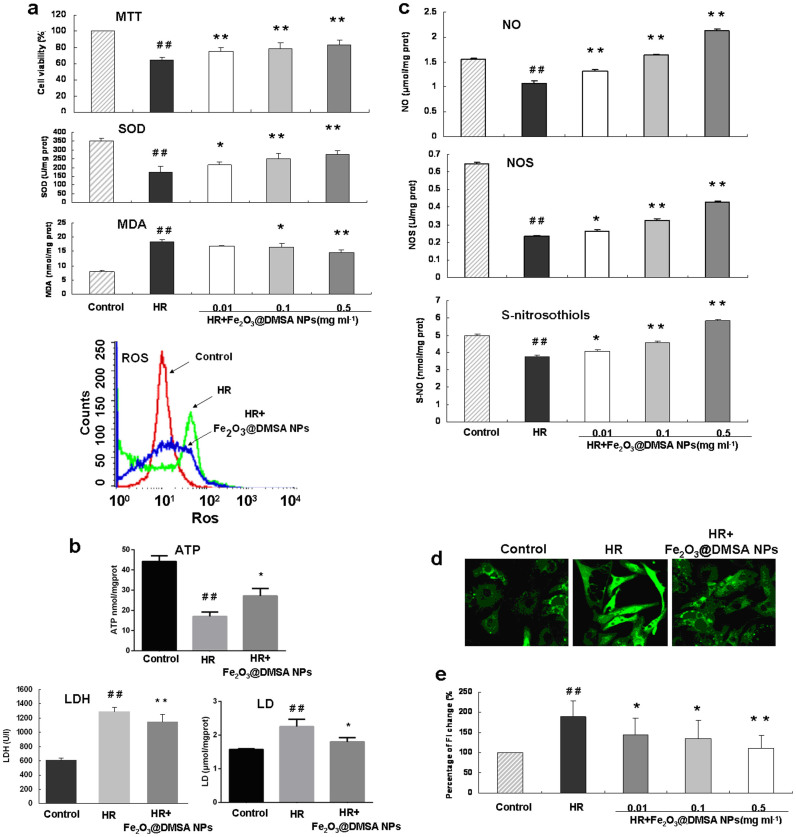
Hypoxia and reoxygenation (HR) is a cell model of heart ischemia and reperfusion injury. When cardiomyocytes were exposed to HR, Fe2O3@DMSA NPs treatment significantly increased the viability and cellular SOD activity, and decreased the content of cellular MDA and reactive oxygen species (ROS) (Fig. 4a). In addition, Fe2O3@DMSA NPs treatments significantly impacted on the cell energy metabolism as indicated by decrease of the generation of LDH and lactate (LD), and increase of the generation of adenosine triphosphate (ATP) (Fig. 4b). The contents of nitric oxide (NO), activity of nitric oxide synthase (NOS) and the level of S-nitrosothiols in cardiomyocytes were also significantly increased upon Fe2O3@DMSA NPs after HR (Fig. 4c). On the other hand, Fe2O3@DMSA NPs treatment significantly decreased intracellular calcium concentration in a dose-dependent manner (Fig. 4d and 4e). These results demonstrate Fe2O3@DMSA NPs could protect cardiomyocytes from HR injury in many aspects at cell level.
Figure 4. Effects of Fe2O3@DMSA NPs on cardiomyocytes under a hypoxia and reoxygenation (HR) condition.
(a), Cardiomyocytes were exposed to hypoxia (95% N2 and 5% CO2) for 6 h followed by 6 h of reoxygenation (95% O2 and 5% CO2) (HR) and effects of Fe2O3@DMSA NPs on cell viability, generation of SOD, MDA and ROS (a), on LDH, LD and ATP (b), and on generation of NO, NOS and S-NO were measured (c). Confocal images of intracellular calcium signal of cardiomyocytes of control, HR and HR + Fe2O3@DMSA NPs (0.1 mg ml−1) group (d). The fluorescent intensity (FI), which indicates intracellular Ca2+ concentration, was quantified (e). * p < 0.05 vs the IR group; ** p < 0.01 vs the IR group; ## p < 0.01 vs the control group; n = 6.
Fe2O3 is critical for the activity of NPs
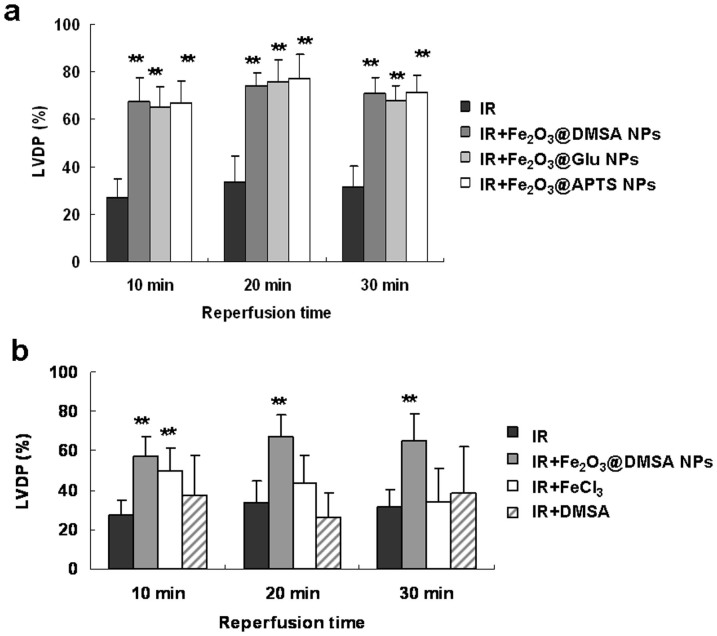
It is known that the surface charge and chemical components play an important role in many biological activities of NPs13,14,15. Therefore, it is possible that the negatively charged Fe2O3@DMSA NPs and surface factors might have attributed to the observed cardioprotective activity. To examine the possible role of charges, we prepared 3-amino-propyltriethoxysilane-modified NPs (Fe2O3@APTs NPs, which are positively charged) and L-glutamic acid-modified Fe2O3 NPs (Fe2O3@Glu NPs, which are near-neutrally charged) (Characterization are shown in Supplementary Fig. S1 and S2). The zeta potentials of Fe2O3@DMSA NPs, Fe2O3@APTs NPs and Fe2O3@Glu NPs were −43.1, 28.9 and −2.1 mV at pH 7.4, respectively. In IR model, however, all types of NPs with same concentration (0.1 mg ml−1) showed a significant potency in protecting perfused Langendorff hearts (Fig. 5a, p < 0.01 vs the IR group) and the difference between them was not significant (p > 0.05). Thus, the cardioprotective activity of the NPs does not depend on the surface charge.
Figure 5. Charges, surface molecules and iron ions do not contribute to the cardioprotective activity in guinea pig Langendorff heart following IR.
(a) Fe2O3 NPs were coated with three different molecules and used to treat perfused hearts. (b) Perfused hearts were treated with Fe2O3@DMSA NPs, FeCl3 solution and DMSA, respectively, and subjected to LVDP recovery examination. ** p < 0.01 vs the IR group, n = 6.
To examine the possible role of surface molecules, the Langendorff hearts were perfused with 0.8 μg ml−1 DMSA, the concentration equivalent to that on the surface of 0.01 mg ml−1 Fe2O3@DMSA NPs. Treatment with DMSA alone did not impact significantly on the LVDP of Langendorff hearts (Fig. 5b, p > 0.05 vs the IR group), indicating that DMSA did not attribute to the observed cardioprotective activity of Fe2O3 NPs.
Next, we analyzed whether or not the cardioprotective activity was due to a trace amount of iron ions leached from Fe2O3@DMSA NPs. Thus, we measured the concentration of iron ions by ultrafiltrating 0.1 mg ml−1 Fe2O3@DMSA NPs in perfusion solution. However, we did not detect iron ions in the ultrafiltrate as measured by inductively coupled plasma atomic emission spectroscopy. Also, the ultrafiltrate had no effects on perfused hearts, indicating that the observed cardioprotective activity was likely due to intact NPs. To further confirm the necessity of NPs, Langendorff hearts were perfused with FeCl3 at the same iron concentration as that present in 0.01 mg ml−1 Fe2O3@DMSA NPs. Fig. 5c shows that the LVDP of FeCl3 solution-treated hearts was only transiently recovered at 10 min of reperfusion (p < 0.01 vs the IR group), while the activity of Fe2O3@DMSA NPs was more sustainable from 10 to 30 min. These results demonstrate that the integrity of NPs is essential for its optimal activity.
The activity of Fe2O3@DMSA NPs with a smaller size is more effective than those with larger size
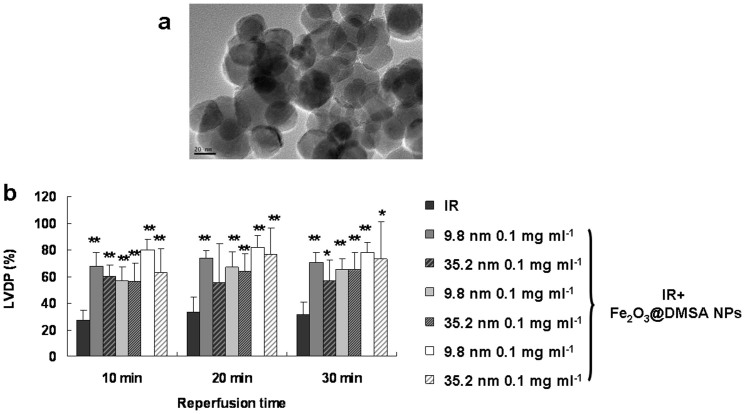
IONPs with different sizes often show different properties16,17. Thus, we studied the cardioprotective activities of Fe2O3@DMSA NPs of an average core size of 9.8 and 35.2 nm (Fig. 4a), respectively. Although Fe2O3@DMSA NPs of 35.2 nm recovered injured hearts significantly as indicated by improving LVDP (p < 0.01, vs the IR group), they were apparently less effective than Fe2O3@DMSA NPs of 9.8 nm in the doses ranging from 0.001 to 0.1 mg ml−1 (Fig. 6).
Figure 6. The cardioprotective activity of Fe2O3@DMSA NPs is dependent on their core sizes in guinea pig Langendorff heart following IR.
(a) TEM image of Fe2O3@DMSA NPs of 35.2 nm. (b) Injured hearts were treated with Fe2O3@DMSA NPs of different sizes and then examined for LVDP recovery. * p < 0.05 vs the IR group; ** p < 0.01 vs the IR group; n = 6.
Fe2O3@DMSA NPs protected heart injury more effectively than Verapamil and Salvia miltiorrhiza extract
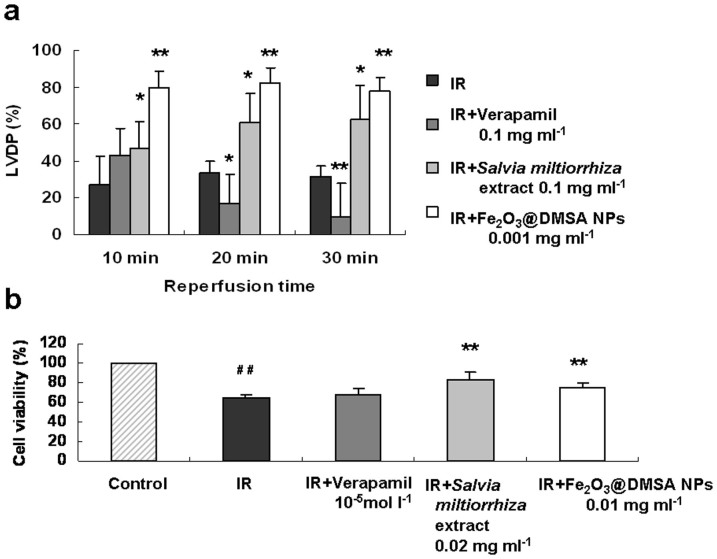
Certain natural organic molecules have been used in clinic for cardiovascular therapies. We compared Fe2O3@DMSA NPs with Verapamil (synthetic drug) and Salvia miltiorrhiza extract (natural product). Verapamil was reported to reduce ischemic injury of heart by inhibiting calcium influx18, just like Fe2O3@DMSA NPs, but it can not improve the LVDP recovery in guinea pig Langendorff heart under the condition where Fe2O3@DMSA NPs worked effectively (Fig. 7a). Salvia miltiorrhiza extract also improved injured hearts significantly (p < 0.05) at 0.1 mg ml−1. However, it was apparently less potent than Fe2O3@DMSA NPs at 10 min of reperfusion (p < 0.05). Also, unlike Fe2O3@DMSA NPs-treated rats, the hearts derived from Verapamil or Salvia miltiorrhiza extract–treated rats had a pale appearance as that of the IR group (Supplementary Fig. S3).
Figure 7. Comparison of cardioprotective effects of Fe2O3@DMSA NPs with Verapamil and Salvia miltiorrhiza extract.
(a) LVDPs of guinea pig Langendorff hearts without (IR) and with 0.1 mg ml−1 of Verapamil (IR + Verapamil), 0.2 mg ml−1 of Salvia miltiorrhiza extract (IR + Salvia miltiorrhiza extract) and 0.001 mg ml−1 of Fe2O3@DMSA NPs (IR + Fe2O3@DMSA NPs) under IR condition. (b) Effects of Verapamil, Salvia miltiorrhiza extract and Fe2O3@DMSA NPs on the viability of cardiomyocytes under HR condition. * p < 0.05 vs the IR or HR group; ** p < 0.01 vs the IR or HR group; ## p < 0.01 vs the control group; n = 6.
It has been reported that Verapamil is toxic to normal neonatal rat cardiomyocytes19,20 and may impact negatively on the function of thyroid and saccharide metabolism. Under HR, Verapamil also failed to improve the viability of injured cardiomyocytes (Fig. 7b), which is constant with previously reported results21. Salvia miltiorrhiza extract improved the viability of injured cells similarly as Fe2O3@DMSA NPs at a concentration 20-fold higher than that of Fe2O3@DMSA NPs.
Discussion
Cardiovascular diseases are the leading cause of mortality in the worldwide22 and a variety of pharmaceutical drugs have been used to target specifically pathological processes for myocardial injury. Yet, these compounds are often associated with side effects and currently there is still no effective therapy to prevent heart injuries23. In this study we reported for the first time a cardioprotective activity of Fe2O3@DMSA NPs. Our results suggest that the NPs can protect heart from ischemic damages in vivo as well as in vitro. The cardioprotective activity of Fe2O3@DMSA NPs is dependent on the core sizes but independent on the molecules used to coat NPs. In addition, the integrity of “nanoparticle” is necessary for its protective activity.
The mechanism of IR injury is complex, including production of free radicals, calcium overload, altered energy metabolism etc. When the heart is exposed to IR, on one hand, ATP catabolism leads to adenosine diphosphate (ADP), adenosine monophosphate (AMP), adenine nucleoside, hypoxanthine nucleoside and then hypoxanthine. On the other hand, ATP depletion leads to the loss of calcium pump function and then the rise in membrane permeability to calcium. Increased concentration of intracellular calcium could activate the calmodulin-dependent protein kinase (CaM kinase),which could induce the conversion of xanthine dehydrogenase (XDH) to xanthine oxidase (XO)18. XO catalyzes hypoxanthine to produce xanthine and large amount of ROS (a kind of free radical)19. Fe2O3@DMSA NPs could inhibit intracellular ROS and then decrease the peroxidation injury of membrane lipid. MDA, the end-products of membrane lipid peroxidation, can also form a conjugated Schiff base product by reacting with the amino group of proteins or phospholipid of membrane20, which induce low fluidity, high permeability and damage of membrane14. Decrease of MDA could reduce membrane damage-induced intracellular LDH leakage to culture supernatant19 and extracellular Ca2+ entrance into cell along the concentration gradient20. Fe2O3@DMSA NPs could inhibit calcium influx, which could then inhibit the ROS. Recently, NO, synthesized from L-arginine by a group of hemoproteins (NOS), is recognized as an important mediator of pathological processes of IR injury24. Fe2O3@DMSA NPs could increase the NOS activity and then increase NO production. NO signal pathway also could be activated by decrease of XO-generated ROS25. Protein S-nitrosylation is a new type of protein post-translational modification, which is a reversible attachment of NO moiety to specific cysteine residues of selected proteins and then produces labile S-nitrosothiol structure and functional alternations. This modification could confer protective effects against myocardial IR26,27,28. Fe2O3@DMSA NPs could increase the level of S-nitrosothiols and then participate in NO-mediated protection against IR injury. In addition, S-nitrosation could control calcium channel and then inhibit calcium influx29. The molecular mechanisms by which ROS, NO and calcium modulate cellular signal transduction remain incompletely understood and crosstalk among ROS-, NO- and calcium-regulated pathways may occur under the Fe2O3@DMSA NPs treatment.
The cardioprotective activity of Fe2O3@DMSA NPs appeared to be higher than those of Salvia miltiorrhiza extract and Verapamil because the NPs showed equal or better protections at lower concentrations. Fe2O3@DMSA NPs also show a restorative effect on ischemic hearts and cell damages, the activity that was not observed with Verapamil. Our observed bioactivity of Fe2O3@DMSA NPs is apparently conflicted with a previously reports that IONPs have a peroxidative activity8,30 and are toxic to tumor cells31. The differential activity of IONPs may be due to (1) cell types, (2) experimental conditions (such as concentrations, under HR, and others), (3) the distribution and intracellular microenvironment of NPs, and (4) different composites of NPs. To explore the natural and basic laws of IONPs function require further study of the interaction between IONPs and more cell types under different physiological and pathological conditions.
Our discovered cardioprotective activity of Fe2O3@DMSA NPs may have a clinical implication because the NPs are easier to be prepared under the condition avoiding environmental contaminations. We expect that application of Fe2O3@DMSA NPs to treat cardiovascular diseases would reduce significantly the costs associated with currently used cardioprotective drugs that are made from either natural sources or chemical syntheses.
Methods
Synthesis and characterization of IONPs
Fe2O3 NPs with approximately 10 nm were synthesized and coated with 2, 3-dimercaptosuccinic acid (DMSA), 3-amino-propyltriethoxysilane (APTs) and L-glutamic acid (Glu) according to our previous work4,32. 35.2 nm Fe2O3 NPs were purchased from XCNM Co., Ltd (China) and coated with DMSA as the same method mentioned above. The core diameters of NPs were characterized by TEM (JEM-200CX, JEOL). The hydrodynamic diameters and zeta potential were measured by electrophoresis instrument (Brookhaven Zetaplus, Malvern).
Coronary artery ligature and assessments
The animals used for the experiment were treated according to the protocols evaluated and approved by the ethical committee of Southeast University (Nanjing, China). Sprague-Dawley rats (200–250 g) were administrated with Fe2O3@DMSA NPs through tail veins. After 7 days, the treated rats were subjected to coronary artery ligature as described below. For the sham and the CAL group, rats were administrated with normal saline solution only.
To perform coronary artery ligature, rats were anesthetized through intraperitoneal injection with 10% chloral hydrate and subsequently fixed on an operation table in a supine position. The limbs of an anesthetized rat were connected to an electrocar diographer (ECG-6511, Nihon Kohden), which recorded the electrocardiogram of the animal's heart. The rat was then ventilated 60 times per min with a volume-cycled respirator. The left coronary artery was ligated as follows: a left thoracotomy incision was introduced to the rat, and the left anterior descending the coronary artery was ligated with a surgical thread, which resulted in ischemia. The treated rat was placed back to a cage and maintained. After 7 d, the treated rat was sacrificed and the blood was collected from the carotid artery for the subsequent study. The heart of the rat was also dissected for assessing the size and the degree of the myocardial infarction. The rats in the sham group experienced the same procedure except that the ligature of the left coronary artery was not performed33.
The dissected hearts were washed with saline and both atria were removed. The cardiac ventricles were sectioned from the apex to the base parallel to the atrioventricular groove into serial slices of 7–10 mm, which were weighed and incubated in a solution of 2,3,5-triphenyltetrazolium chloride (TTC) in PBS at 37°C for 5–10 min. This procedure stains only the healthy myocardium as red, resulting in an infarct as a pale and clearly outlined area34. After staining, the healthy and infarcted areas were separated by dissection, and the infarction ratio was calculated according to the following formula: infarction ratio (%) = (weight of infarcted ventricle/weight of whole ventricle) × 100.
Langendorff perfusion and assessments
The animals used for the experiment were treated according to the protocols evaluated and approved by the ethical committee of Southeast University (Nanjing, China). Guinea pigs (250–350 g) were anesthetized with intraperitoneal pentobarbital sodium (50 mg/kg) and heparinized (1,000 U, i.p.). The heart was rapidly excised from guinea pigs and arrested in ice-cold oxygenated Locke's solution (154 mM NaCl, 5.6 mM KCl, 2.1 mM CaCl2, 5.9 mM NaHCO3, and 5.5 mM glucose 5.5 mM) before the aorta was cannulated on a Langendorff apparatus. Non-recirculating mode of retrograde perfusion with Locke's solution was carried out at a constant pressure (80 cmH2O) at 37°C. The isolated hearts were allowed to equilibrate for 30 min and followed by 30-min global and normothermic ischemia by halting perfusion35.
With three males and three females in each group, guinea pigs were randomly divided and reperfused without or with NPs for 30 min immediately after ischemia respectively. Through the mitral valve, a water-filled polyvinylchloride balloon was attached to a pressure transducer that was inserted into the left ventricular after having an incision in the left atrium. The end-diastolic pressure of the balloon inserted into the ventricle was adjusted to 25 mmHg, and the change of the pressure was recorded by a data recording system.
The LVDP and HR were measured at 5 min before ischemia, during ischemia and 10 min, 20 min, 30 min after ischemia. The values of these parameters after ischemia/reperfusion were expressed as a percentage of those obtained before ischemia.
Hypoxia and reoxygenation
Cardiomyocytes were cultured in 96-well plate under 5% CO2 atmosphere at 37°C. To each confluent well, 20 μl of Fe2O3@DMSA NPs solution was added to 180 μl of cell culture medium. After 24 h, the cells, except for the normal control group, were exposed to hypoxia (95% N2 and 5% CO2) for 6 h followed by 6 h of reoxygenation (95% O2 and 5% CO2). The medium was then replaced with high sugar DMEM, and the cells were continuously cultured for additional 6 h and then subjected to biochemical and cellular analyses.
Cell biology
To assess cytotoxicity, 20 μl MTT (5 g l−1) was added into each well of cell culture. After 4 h incubation at 37°C, the culture medium was removed, added with 150 μl of DMSO followed by shaking for 15 min. OD was measured with 960 automatic microplate reader at λ = 570 nm, and the value for each sample group (6 wells per group) were normalized to that of the normal group, which was set as 100%.
LDH, SOD, MDA, LD, ATP, NO and NOS in culture medium were measured by using 7550 spectrophotometer according to the manufacturer's instructions (NJBI, China). S-nitrosothiols was detected by DAN fluorometric method as described previously36.
To measure intracellular calcium, cells were loaded with Fluo-3/AM (5 μmol l−1) working solution containing 0.05% pluronic F-127 and incubated at 37°C for 45 min. After washing, the intracellular free-calcium was visualized and measured by confocal microscopy (TCS-SPII, Leica) excited at 488 nm and emitted at 530 nm. The change in Ca2+ was represented by changes in the percentage of relative fluorescent intensity.
Statistical analysis
Paired Student's t-test was used to compare the data among tested groups. All the values were expressed as the mean ± SD. Results were considered statistically significant if the p-value was less than 0.05.
Author Contributions
F.X., H.W., Y.L. and N.G. conceived and designed the experiments. F.X., Y.F., X.H., X.P. and S.Z. performed the experiments. L.S. and Y.Z. contributed reagents. F.X. and Y.F. wrote the paper. All authors discussed the results and commented on the manuscript.
Supplementary Material
Supplementary Information
Acknowledgments
We thank Professor Steven Zhan for helpful discussion. This work was financially supported by National Basic Research Program of China (No. 2011CB933503), Major National Science and Technology Projects (2013ZX09301-303-003), National Natural Science Foundation of China (No. 81473160, 81172955 and 81302773), the Fundamental Research Funds for the Central Universities (2242014R30013), and Jiangsu Provincial Special Program of Medical Science (BL2013029).
References
- Finegold J. A., Asaria P. & Francis D. P. Mortality from ischaemic heart disease by country, region, and age: statistics from World Health Organisation and United Nations. Int. J. Cardiol. 168, 934–945 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pu J. et al. Cardiomyocyte-expressed farnesoid-X-receptor is a novel apoptosis mediator and contributes to myocardial ischaemia/reperfusion injury. Eur. Heart J. 34, 1834–1845 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hausenloy D. J. & Yellon D. M. Myocardial ischemia-reperfusion injury: a neglected therapeutic target. J. Clin. Invest. 123, 92–100 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiong F. et al. Preparation, characterization of 2-deoxy-D-glucose functionalized dimercaptosuccinic acid-coated maghemite nanoparticles for targeting tumor cells. Pharm. Res. 29, 1087–1097 (2012). [DOI] [PubMed] [Google Scholar]
- Xiong F. et al. Rubik-like magnetic nanoassemblies as an efficient drug multifunctional carrier for cancer theranostics. J. Control Release. 172, 993–1001 (2013). [DOI] [PubMed] [Google Scholar]
- Hirsch L. R. et al. Nanoshell-mediated near-infrared thermal therapy of tumors under magnetic resonance guidance. Proc. Natl Acad. Sci. USA 100, 13549–13554 (2003). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bergemann C., Muller-Schulte D. & Oster J. Magnetic ion-exchange nano- and microparticles for medical, biochemical and molecular biological applications. Magn. Magn. Mater. 194, 45–52 (1999). [Google Scholar]
- Gao L. et al. Intrinsic peroxidase-like activity if ferromagnetic nanoparticles. Nature Nanotech 2, 577–583 (2007). [DOI] [PubMed] [Google Scholar]
- Chen Z. et al. Dual enzyme-like activities of iron oxide nanoparticles and their implication for diminishing cytotoxicity. ACS Nano. 6, 4001–4012 (2012). [DOI] [PubMed] [Google Scholar]
- Zhou R. et al. Cardioprotective effect of water and ethanol extract of Salvia miltiorrhiza in an experimental model of myocardial infarction. J. Ethnopharmacol. 139, 440–446 (2012). [DOI] [PubMed] [Google Scholar]
- Chang P. N. et al. Analysis of cardioprotective effects using purified Salvia miltiorrhiza extract on isolated rat hearts. J. Pharmacol. Sci. 101, 245–9 (2006). [DOI] [PubMed] [Google Scholar]
- Wu T., Ni J. & Wu J. Danshen (Chinese medicinal herb) preparations for acute myocardial infarction. Cochrane Database Syst. Rev. 16, CD004465 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asati A., Santra S., Kaittanis C. & Perez J. M. Surface-charge-dependent cell localization and cytotoxicity of cerium oxide nanoparticles. ACS Nano, 4, 5321–5331 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirsch V. et al. Surface charge of polymer coated SPIONs influences the serum protein adsorption, colloidal stability and subsequent cell interaction in vitro. Nanoscale 5, 3723–3732 (2013). [DOI] [PubMed] [Google Scholar]
- Fröhlich E. The role of surface charge in cellular uptake and cytotoxicity of medical nanoparticle. Int J Nanomedicine 7, 5577–5591 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Demortière A. et al. Size-dependent properties of magnetic iron oxide nanocrystals. Nanoscale 3, 225–332 (2011). [DOI] [PubMed] [Google Scholar]
- Chatterjee J., Haik Y. & Chen C. J. Size dependent magnetic properties of iron oxide nanoparticles. J Magn Magn Mater. 257, 113–118 (2003). [Google Scholar]
- Wang Q. D., Pernow J., Sjöquist P. O. & Rydén L. Pharmacological possibilities for protection against myocardial reperfusion injury. Cardiovasc. Res. 55, 25–37 (2002). [DOI] [PubMed] [Google Scholar]
- Sokhanenkova A. E., Sokhanenkov Miu., Afanas'eva Eiu. & Arzamastsev E. V. Characteristics of pharmacological and toxic effects of verapamil during cardiac arrhythmia in thyrotoxic and hypothyroid rats. Kardiologiia 48, 57–61 (2008). [PubMed] [Google Scholar]
- Bechtel L. K., Haverstick D. M. & Holstege C. P. Verapamil toxicity dysregulates the phosphatidylinositol 3-kinase pathway. Acad. Emerg. Med. 15, 368–374 (2008). [DOI] [PubMed] [Google Scholar]
- Wang L. D. & Nang B. S. The toxicity of Verapamil to cardiomyocytes. Chin. J. Clin. Pharmacol. Ther. 2, 178–179 (2000). [Google Scholar]
- Gawryszewski V. P. & Souza Mde. F. Mortality due to cardiovascular diseases in the Americas by region, 2000–2009. Sao Paulo Med J. 132, 105–10 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hausenloy D. J. & Yellon D. M. Myocardial ischemia-reperfusion injury: a neglected therapeutic target. J Clin Invest. 123, 92–100 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Q. D., Morcos E., Wiklund P. & Pernow J. L-arginine enhances functional recovery and Ca(2+)-dependent nitric oxide synthase activity after ischemia and reperfusion in the rat heart. J Cardiovasc Pharmacol. 29, 291–296 (1997). [DOI] [PubMed] [Google Scholar]
- Minhas K. M. et al. Xanthine oxidoreductase inhibition causes reverse remodeling in rats with dilated cardiomyopathy. Circ Res. 98, 271–279 (2006). [DOI] [PubMed] [Google Scholar]
- Johnson G. R., Tsao P. S., Mulloy D. & Lefer A. M. Cardioprotective effects of acidified sodium nitrite in myocardial ischemia with reperfusion. J Pharmacol Exp Ther. 252, 35–41 (1990). [PubMed] [Google Scholar]
- Williams M. W., Taft C. S., Ramnauth S., Zhao Z. Q. & Vinten-Johansen J. Endogenous nitric oxide (NO) protects against ischaemia-reperfusion injury in the rabbit. Cardiovasc Res. 30, 79–86 (1995). [PubMed] [Google Scholar]
- Prime T. A. et al. A mitochondria-targeted S-nitrosothiol modulates respiration, nitrosates thiols, and protects against ischemia-reperfusion injury. Proc Natl Acad Sci U S A 106, 10764–10769 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poteser M., Romanin C., Schreibmayer W., Mayer B. & Groschner K. S-nitrosation controls gating and conductance of the alpha 1 subunit of class C L-type Ca(2+) channels. J Biol Chem. 276, 14797–14803 (2001). [DOI] [PubMed] [Google Scholar]
- Gao L., Giglio K. M., Nelson J. L., Sondermann H. & Travis A. J. Ferromagnetic nanoparticles with peroxidase-like activity enhance the cleavage of biological macromolecules for biofilm elimination. Nanoscale 6, 2588–2593 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang G. et al. Superparamagnetic iron oxide nanoparticles: amplifying ROS stress to improve anticancer drug efficacy. Theranostics 3, 116–126 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang S. et al. The effect of iron oxide magnetic nanoparticles on smooth muscle cells. Nanoscale Res. Lett. 4, 70–77 (2009). [Google Scholar]
- Guo Q. et al. Protective effect of corocinnarine on ischemia-reperfusion myocardium of rats and its relation to anti-lipid peroxidation. Chin. Heart J. 14, 4–6 (2002). [Google Scholar]
- Hopkins T. A., Ouchi N., Shibata R. & Walsh K. Adiponectin actions in the cardiovascular system. Cardiovasc. Res. 74, 11–18 (2007). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skrzypiec-Spring M., Grotthus B., Szelag A. & Schulz R. Isolated heart perfusion according to Langendorff—still viable in the new millennium. J. Pharmacol. Toxicol. Methods 55, 113–126 (2007). [DOI] [PubMed] [Google Scholar]
- Park J. K. & Kostka P. Fluorometric detection of biological S-nitrosothiols. Anal. Biochem. 249, 61–66 (1997). [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Information