Abstract
Background:
Polycystic ovary syndrome (PCOS) is one of the common endocrine disorders and is associated with reproductive, metabolic, and psychological disturbances affecting one in five women of reproductive age group.
Objective:
To investigate the prevalence of psychiatric disorders among women in ambulatory treatment with a diagnosis of PCOS.
Materials and Methods:
One hundred and ten patients of PCOS were evaluated using Diagnostic and Statistical Manual for Mental Disorders, Fourth Edition criteria by means of Mini International Neuropsychiatric Interview, English version 5.0.0. Diagnosis of PCOS was confirmed according to the National Institute of Health/National Institute of Child Health and Human Development, 1990 consensus conference criteria. Forty subjects without PCOS who were matched for age and body mass index were taken as a comparison group.
Results:
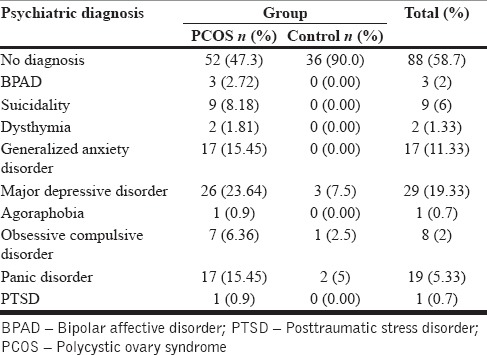
About 23% of cases had major depressive disorder as compared to 7.5% of controls, 1.8% had dysthymia, 15.45% had panic disorder compared to 5% of controls, 6.36% had obsessive compulsive disorder compared to 2.5% of controls, 8% cases had suicidality, 2.72% of cases were bipolar affective disorder, and 15.45% had generalized anxiety disorder (GAD).
Conclusion:
A high prevalence of mental disorders was observed, especially major depression, panic disorder, and GAD in patients with PCOS in our study. The results suggest that screening and appropriate management for psychiatric disorders should be part of the routine evaluation of these patients.
Keywords: Depression, polycystic ovary syndrome, prevalence, suicide
INTRODUCTION
Polycystic ovary syndrome (PCOS) is one of the common reproductive endocrine disorders, affecting 5-10% of women of reproductive age.[1] The classic features include menstrual irregularity, biochemical or clinical hyperandrogenism, and ultrasound appearance of polycystic ovaries.[2] The basic physiopathological features in patients with PCOS are obesity and insulin resistance. The resulting state of hyperinsulinemia stimulates the production of ovarian androgen by means of a cytochrome P450c17 enzyme complex, as well as the production of hypophyseal luteinizing hormone,[3,4] which leads to imbalance in sexual hormones. Endocrine and psychiatric disorders, especially mood disorders, seem to be interconnected and affecting each other.[5,6] The neuroendocrine systems are crucial not only in reproductive function, but also in mood regulation.[7] Women with PCOS are at increased risk of psychological problems. Some studies in the past have indicated a higher prevalence of psychiatric disorders especially mood disorders in patients with PCOS.[8] There are several reports linking specific PCOS features, such as infertility,[9] hirsutism,[10] and acne[11] to decreased mental well-being. Depression and anxiety symptoms are associated with higher body mass index and waist-to-hip ratio in women with PCOS.[12,13] Relationships may be further confounded by the use of psychotropic medications, which may induce weight gain.
We undertook this study to estimate the prevalence of psychiatric morbidity in woman with a diagnosis of PCOS presenting to the outpatients department at the Sher-e-Kashmir Institute of Medical Sciences (SKIMS). To our knowledge, this is the first study to look into the psychological issues in the female population with PCOS from Kashmir Valley.
MATERIALS AND METHODS
Sher-e-Kashmir Institute of Medical Sciences provides tertiary medical care to the whole of Kashmir region along with some adjoining areas of Jammu and Ladakh region, the population of about 6 million. One hundred and ten consecutive consenting patients diagnosed with PCOS were included in the study. The study was approved by the SKIMS Ethical Committee. Diagnosis of PCOS was made by consultant endocrinologist using clinical, biochemical, and ultrasonic parameters. The National Institute of Health/National Institute of Child Health and Human Development, 1990 consensus conference criteria were employed for the diagnosis of PCOS as per the criteria as follows:
Clinical and/or biochemical hyperandrogenism
Oligo-anovulation (oligomenorrhea/amenorrhea)
Exclusion of disorders such as nonclassical congenital adrenal hyperplasia, Cushing's syndrome, thyroid dysfunction, hyperprolactinemia, and androgen-producing tumors.
Forty subjects without PCOD who were matched for age were taken as a comparison group. All these subjects were interviewed for a detailed menstrual history including age of menarche, regularity, duration, and the number of menstrual cycles per year.
All consecutively diagnosed cases of PCOD who consented were included in our study. The subjects who had any history of systemic illness such as known diabetes, heart conditions, pregnancy, lactation, history of drug intakes such as steroids, androgens, oral contraceptives, anti-epileptics, or drugs known to interfere in glucose or lipid metabolism were excluded from the study.
Participants gave their verbal informed consent before entering in the study. Both the cases and comparison group were evaluated to investigate the lifetime and current psychiatric disorder for psychiatric morbidity using Diagnostic and Statistical Manual for Mental Disorders, Fourth Edition (DSM-IV) criteria by means of Mini International Neuropsychiatric Interview (MINI, English version 5.0.0) administered by qualified psychiatrist. The choice of MINI as an instrument was based on its high levels of reliability and validity, which have been reported in several studies.[14] The MINI is a structured interview tool, designed to evaluate the presence of psychiatric disorders according to Axis I, of the DSM-IV.
RESULTS
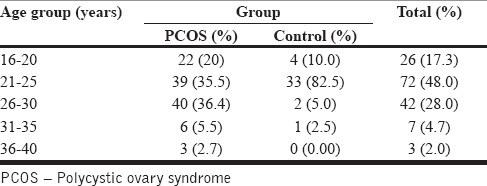
Sample comprised of 110 PCOS patients and 40 controls. The mean age of PCOS patients was 24.77 years, while the mean age of controls was 22.65 years.79 (71.9%) patients with PCOS were in the age group of 21-30 years while 22 (20%) were in the age group 16-20 years. 9 (8.2%) were in the age group 31-40 years. while 87.5% females of the comparison group belonged to 21-30 years group and 10% belonged to age group 16-20 years [Tables 1 and 2].
Table 1.
Mean age of subjects
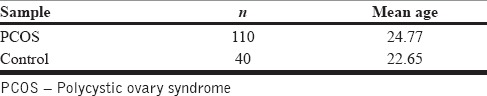
Table 2.
Age distribution
PSYCHIATRIC MORBIDITY
Table 3 shows 52.7% of patients in PCOS group were having a comorbid psychiatric illness as compared to only 10% of females in the comparison group.
Table 3.
Presence of psychiatric morbidity
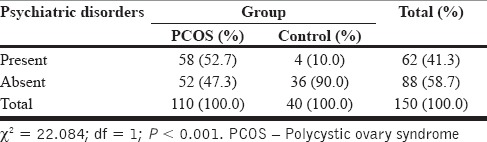
Table 4 shows 23.64% of PCOS patients had major depressive disorder compared to only 7.5% of females in the control group. Whereas, 15.45% of PCOS patients had generalized anxiety disorder (GAD), none of the controls had GAD. 6.36% of PCOS patients had obsessive compulsive disorder (OCD) while only 2.5% in the control group had OCD. 15.45% PCOS patients had panic disorder as compared to 5% of controls. Suicidality was seen in 8.18% of PCOS patients and 2.72% PCOS patients had bipolar affective disorder. 1.81% had dysthymia while agoraphobia was present in 0.9% of patients of PCOS.
Table 4.
Prevalence of different psychiatric morbidities
DISCUSSION
Polycystic ovary syndrome is a common endocrine disorder encountered by clinician in women of reproductive age. The syndrome is characterized by chronic anovulation and hyperadrogenism and is manifested by hirsutism, cystic acne, hair loss, insulin resistance, and weight gain and also one of the primary causes of infertility all of which leads to decrease in health-related quality of life.[15] Our patients with PCOS exhibited high rates of psychopathology, with 52.7% of the sample suffering from a psychiatric condition.
The main findings of our study were high rates of depression and anxiety disorders especially GAD, panic disorder, and OCD. There were also high rates of suicidality in patients of PCOS as compared to control group. The high rate of depression in women with PCOS corroborates earlier studies. Rassi et al. in 2010 found major depression in 26.4% of PCOS patients[16] Hollinrake et al. in 2007 found that 21% PCOS patients compared to 3% of controls had depression.[17] Whereas Månsson et al. in 2008 and Kerchner et al. in 2009 found 45% and 40% prevalence of depression in PCOS patients, respectively, which is higher than our study.[13,18] This variation in prevalence of depression between these studies can be explained by the fact that different methods and tools used for screening and diagnosing, influence of culture on epidemiology of depression, and lastly use of medication (like oestrogen).[19]
Several studies have shown that in women with PCOS, owing to the changes in physical features due to hyperandrogenism such as hirsutism, obesity, alopecia, or acne, that influence their feminine identity, and which are also culturally defined as unfeminine and undesirable, affects the social image of the patient.[20,21] These physical characteristics often lead to social withdrawal and isolation along with a negative image of self and lower self-esteem all of which are important risk factors for depression and anxiety disorders.
In addition, as major components of feminine role expectations, loss of regular menstruation, and infertility may also cause or contribute to emotional distress in women with PCOS.[22,23] Furthermore, the increased prevalence of depression can be explained by direct influence of high androgen levels on mood disturbances.[24]
Our study also showed high levels of suicidality in PCOS patients which was similar to study done by Månsson et al. in 2008.[13]
We found a high prevalence of anxiety disorder especially GAD, Panic Disorder, and OCD. Månsson et al. also found high rates of anxiety disorder in women with PCOS.[13] Similarly, Kerchner et al. found high levels of anxiety disorders in PCOS patients.[18] A high level of anxiety can be explained by the fact that there are persistent fears of loss of sexuality, loss of fertility, and anxiety of not being able to have children in the future. Moreover, most of the PCOS symptoms may also contribute to anxiety and in fact these symptoms have previously been related to anxiety in other patient population, including hirsutism,[25] acne,[26] obesity,[27] and involuntary childlessness (infertility).[28]
While recent research shows that approximately 50% of PCOS patients are overweight or obese.[29] Social phobia may be triggered by negative reactions from other people toward obesity and hirsutism. These anxiety-provoking situations are likely to elicit avoidance, that may in turn induce further anxiety and discomfort.[13] High anxiety symptoms in PCOS may be explained by increased arousal. High sympathetic nerve activity has been observed in women with PCOS compared with controls, observations explained by high testosterone concentrations.[30]
A depressed mood may have a profound influence on the quality of life and also reduce the motivation[31] and to ensure good compliance with medication and the dietary management of PCOS[32] good motivation is needed, so treatment of depression is likely to have a positive effect on other features of the disorder, including weight management.
CONCLUSION
Our study shows high prevalence of psychiatric morbidity in women with PCOS compared to the comparison group. The presence of psychiatric comorbidity has a negative influence on the outcome of PCOS and vice versa. Screening for mental health-related issues of such patients should be part of the initial evaluation. Both endocrinologist and gynecologist who commonly treat PCOS patients should be aware of the potential presence of psychiatric disorders and should have a proactive approach to not only medical but also treatment of psychiatric co-morbidity. Timely referral for the treatment of psychiatric co-morbidity can improve the outcome significantly and enhance the quality of life of the said patient group. In fact, a multidisciplinary team approach not only involving gynecologist and endocrinologist but also a psychiatrist would be ideal.
Limitations
There is no community data from Kashmir about the prevalence of psychiatric morbidity in the general population, hence, we were not able to compare and use the comparison group.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Knochenhauer ES, Key TJ, Kahsar-Miller M, Waggoner W, Boots LR, Azziz R. Prevalence of the polycystic ovary syndrome in unselected black and white women of the Southeastern United States: A prospective study. J Clin Endocrinol Metab. 1998;83:3078–82. doi: 10.1210/jcem.83.9.5090. [DOI] [PubMed] [Google Scholar]
- 2.Wild RA, Carmina E, Diamanti-Kandarakis E, Dokras A, Escobar-Morreale HF, Futterweit W, et al. Assessment of cardiovascular risk and prevention of cardiovascular disease in women with the polycystic ovary syndrome: A consensus statement by the Androgen Excess and Polycystic Ovary Syndrome (AE-PCOS) Society. J Clin Endocrinol Metab. 2010;95:2038–49. doi: 10.1210/jc.2009-2724. [DOI] [PubMed] [Google Scholar]
- 3.Franks S. Polycystic ovary syndrome. N Engl J Med. 1995;333:853–61. doi: 10.1056/NEJM199509283331307. [DOI] [PubMed] [Google Scholar]
- 4.Nestler JE, Jakubowicz DJ. Decreases in ovarian cytochrome P450c17 alpha activity and serum free testosterone after reduction of insulin secretion in polycystic ovary syndrome. N Engl J Med. 1996;335:617–23. doi: 10.1056/NEJM199608293350902. [DOI] [PubMed] [Google Scholar]
- 5.Weber B, Lewicka S, Deuschle M, Colla M, Heuser I. Testosterone, androstenedione and dihydrotestosterone concentrations are elevated in female patients with major depression. Psychoneuroendocrinology. 2000;25:765–71. doi: 10.1016/s0306-4530(00)00023-8. [DOI] [PubMed] [Google Scholar]
- 6.Rao RC, Rasgon NL, Hwang S, Altshuler LL, Zuckerbrow-Miller J, Korenman S. New Orleans, La: Annual Meeting American Psychiatric Association; 2001. Prevalence of depression in women with polycystic ovary syndrome. [Google Scholar]
- 7.Newberg AR, Catapano LA, Zarate CA, Manji HK. Neurobiology of bipolar disorder. Expert Rev Neurother. 2008;8:93–110. doi: 10.1586/14737175.8.1.93. [DOI] [PubMed] [Google Scholar]
- 8.Rasgon NL, Rao RC, Hwang S, Altshuler LL, Elman S, Zuckerbrow-Miller J, et al. Depression in women with polycystic ovary syndrome: Clinical and biochemical correlates. J Affect Disord. 2003;74:299–304. doi: 10.1016/s0165-0327(02)00117-9. [DOI] [PubMed] [Google Scholar]
- 9.Tan S, Hahn S, Benson S, Janssen OE, Dietz T, Kimmig R, et al. Psychological implications of infertility in women with polycystic ovary syndrome. Hum Reprod. 2008;23:2064–71. doi: 10.1093/humrep/den227. [DOI] [PubMed] [Google Scholar]
- 10.Hahn S, Janssen OE, Tan S, Pleger K, Mann K, Schedlowski M, et al. Clinical and psychological correlates of quality-of-life in polycystic ovary syndrome. Eur J Endocrinol. 2005;153:853–60. doi: 10.1530/eje.1.02024. [DOI] [PubMed] [Google Scholar]
- 11.Barnard L, Ferriday D, Guenther N, Strauss B, Balen AH, Dye L. Quality of life and psychological well-being in polycystic ovary syndrome. Hum Reprod. 2007;22:2279–86. doi: 10.1093/humrep/dem108. [DOI] [PubMed] [Google Scholar]
- 12.Adali E, Yildizhan R, Kurdoglu M, Kolusari A, Edirne T, Sahin HG, et al. The relationship between clinico-biochemical characteristics and psychiatric distress in young women with polycystic ovary syndrome. J Int Med Res. 2008;36:1188–96. doi: 10.1177/147323000803600604. [DOI] [PubMed] [Google Scholar]
- 13.Månsson M, Holte J, Landin-Wilhelmsen K, Dahlgren E, Johansson A, Landén M. Women with polycystic ovary syndrome are often depressed or anxious - A case control study. Psychoneuroendocrinology. 2008;33:1132–8. doi: 10.1016/j.psyneuen.2008.06.003. [DOI] [PubMed] [Google Scholar]
- 14.Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59(Suppl 20):22–33. [PubMed] [Google Scholar]
- 15.Elsenbruch S, Hahn S, Kowalsky D, Offner AH, Schedlowski M, Mann K, et al. Quality of life, psychosocial well-being, and sexual satisfaction in women with polycystic ovary syndrome. J Clin Endocrinol Metab. 2003;88:5801–7. doi: 10.1210/jc.2003-030562. [DOI] [PubMed] [Google Scholar]
- 16.Rassi A, Veras AB, dos Reis M, Pastore DL, Bruno LM, Bruno RV, et al. Prevalence of psychiatric disorders in patients with polycystic ovary syndrome. Compr Psychiatry. 2010;51:599–602. doi: 10.1016/j.comppsych.2010.02.009. [DOI] [PubMed] [Google Scholar]
- 17.Hollinrake E, Abreu A, Maifeld M, Van Voorhis BJ, Dokras A. Increased risk of depressive disorders in women with polycystic ovary syndrome. Fertil Steril. 2007;87:1369–76. doi: 10.1016/j.fertnstert.2006.11.039. [DOI] [PubMed] [Google Scholar]
- 18.Kerchner A, Lester W, Stuart SP, Dokras A. Risk of depression and other mental health disorders in women with polycystic ovary syndrome: A longitudinal study. Fertil Steril. 2009;91:207–12. doi: 10.1016/j.fertnstert.2007.11.022. [DOI] [PubMed] [Google Scholar]
- 19.Sen B, Mari JJ. Psychiatric research instruments in the transcultural setting: Experiences in India and Brazil. Soc Sci Med. 1986;23:277–81. doi: 10.1016/0277-9536(86)90348-5. [DOI] [PubMed] [Google Scholar]
- 20.Weiner CL, Primeau M, Ehrmann DA. Androgens and mood dysfunction in women: Comparison of women with polycystic ovarian syndrome to healthy controls. Psychosom Med. 2004;66:356–62. doi: 10.1097/01.psy.0000127871.46309.fe. [DOI] [PubMed] [Google Scholar]
- 21.Dixon JB, Dixon ME, O’Brien PE. Depression in association with severe obesity: Changes with weight loss. Arch Intern Med. 2003;163:2058–65. doi: 10.1001/archinte.163.17.2058. [DOI] [PubMed] [Google Scholar]
- 22.Domar AD, Broome A, Zuttermeister PC, Seibel M, Friedman R. The prevalence and predictability of depression in infertile women. Fertil Steril. 1992;58:1158–63. [PubMed] [Google Scholar]
- 23.Oddens BJ, den Tonkelaar I, Nieuwenhuyse H. Psychosocial experiences in women facing fertility problems — A comparative survey. Hum Reprod. 1999;14:255–61. doi: 10.1093/humrep/14.1.255. [DOI] [PubMed] [Google Scholar]
- 24.Tsilchorozidou T, Overton C, Conway GS. The pathophysiology of polycystic ovary syndrome. Clin Endocrinol (Oxf) 2004;60:1–17. doi: 10.1046/j.1365-2265.2003.01842.x. [DOI] [PubMed] [Google Scholar]
- 25.Lipton MG, Sherr L, Elford J, Rustin MH, Clayton WJ. Women living with facial hair: The psychological and behavioral burden. J Psychosom Res. 2006;61:161–8. doi: 10.1016/j.jpsychores.2006.01.016. [DOI] [PubMed] [Google Scholar]
- 26.Yazici K, Baz K, Yazici AE, Köktürk A, Tot S, Demirseren D, et al. Disease-specific quality of life is associated with anxiety and depression in patients with acne. J Eur Acad Dermatol Venereol. 2004;18:435–9. doi: 10.1111/j.1468-3083.2004.00946.x. [DOI] [PubMed] [Google Scholar]
- 27.Petry NM, Barry D, Pietrzak RH, Wagner JA. Overweight and obesity are associated with psychiatric disorders: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Psychosom Med. 2008;70:288–97. doi: 10.1097/PSY.0b013e3181651651. [DOI] [PubMed] [Google Scholar]
- 28.Lechner L, Bolman C, van Dalen A. Definite involuntary childlessness: Associations between coping, social support and psychological distress. Hum Reprod. 2007;22:288–94. doi: 10.1093/humrep/del327. [DOI] [PubMed] [Google Scholar]
- 29.Gambineri A, Pasquali R. Insulin resistance, obesity and metabolic syndrome in polycystic ovary syndrome. Endocrinol Nutr. 2006;53(Suppl 1):49–55. [Google Scholar]
- 30.Sverrisdóttir YB, Mogren T, Kataoka J, Janson PO, Stener-Victorin E. Is polycystic ovary syndrome associated with high sympathetic nerve activity and size at birth? Am J Physiol Endocrinol Metab. 2008;294:E576–81. doi: 10.1152/ajpendo.00725.2007. [DOI] [PubMed] [Google Scholar]
- 31.4th ed. Washington, DC, USA: APA; 1999. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. [Google Scholar]
- 32.Willmott J. The experiences of women with polycystic ovarian syndrome. Feminism Psychol. 2000;10:107–16. [Google Scholar]


