Abstract
Background:
Primary care has been identified as a key setting for the reduction of alcohol-related harm, while general practitioners are expected to play a significant role. The study aimed at identifying pattern of, and factors that are associated with alcohol use disorders (AUDs) among patients attending Family Medicine unit of State University Teaching Hospital.
Materials and Methods:
Sample was selected through a random sampling from a population of patients, aged 18-65 years, attending the general medical out-patients unit of the hospital from January to April 2013. A pretested, semi-structured questionnaire was administered, incorporating sociodemographics and the diagnoses made by the attending Physician. The participants also completed the alcohol use disorders identification test (AUDIT) questionnaire and the patient health questionnaire-9.
Results:
The prevalence of AUDs among the population of general out-patients was 9.7%. The AUDIT scores of the participants range from 0 to 29 with a mean of 1.3 (standard deviation = 4.08). AUDs were significantly associated with gender, level of education, occupational class, and the presence of significant depressive symptoms (P < 0.05). There was no statistically significant association found for age, employment status, marital status, and religion.
Conclusion:
The prevalence of AUDs among population studied was lower compared with a similar study in similar setting, but however, significant. AUDs were predicted by gender, lower education level, occupational group, and the presence of significant depressive symptoms mostly in the mild to moderate form. Identifying the group at risk in clinical setting may go a long way in reducing the adverse effect of AUDs in our society.
Keywords: Alcohol use disorders, alcohol use disorders identification test questionnaire, family practice, predictors
INTRODUCTION
Alcohol-related harm is a global problem. Globally, alcohol consumption has increased in recent decades, more significantly in developing countries. Prevalence estimates range from 4% to 29% for hazardous drinking and from <1% to 10% for harmful drinking globally.[1] Similar rates of hazardous or harmful alcohol use in health care settings have been reported from different African countries.[2,3,4,5,6,7] Recent estimates suggest that about 2.5 million deaths each year are directly attributable to alcohol, with the highest percentage of alcohol-related deaths occurring among people between 15 and 29 years old; with nearly 1 out of 10 deaths in this age group worldwide attributable to alcohol.[8] This makes alcohol the world's third largest risk factor for disease. Alcohol use contributes to traumatic outcomes; killing or disabling many at a relatively young age, and resulting in the loss of many years of life to death or disability.[9] Researchers have established a strong association between alcohol use and road traffic accidents in Nigeria.[10,11,12] In fact, Welcome and Pereverzev[12] reported that approximately 50% of accidents on Nigerian roads are related to alcohol use.
There has been an increasing emphasis on the role of primary health care and family physician in the prevention and management of alcohol-related harm.[13,14] The health professionals at these primary care settings are readily accessible to the general population and have a significant role in the delivery of advice about alcohol consumption. In addition, there is good evidence that brief interventions delivered by general practitioners have a positive impact on patients’ alcohol consumption.
This study is aimed at determining the pattern and the predictors of alcohol use disorders (AUDs) among patients attending the family practice unit of our teaching hospital which provides essentially primary care services.
MATERIALS AND METHODS
Study population
The study population consists of patients attending Family practice units of the Ekiti State University Teaching Hospital, Ado-Ekiti, in South-western Nigeria. It is a State University Teaching Hospital providing primary, secondary and tertiary care. The family Physician clinic provides essentially primary care services and makes referrals to other specialist clinics.
Sampling technique
Sample was selected through a random sampling from a population of patients, aged 18-65 years, attending the general medical unit of the hospital from January to April, 2013. Patients with debilitating physical illnesses and those that came for routine medical check-up were not included in the study.
Procedures
The Ethics and Research Committee of the University Teaching Hospital approved the study protocol and informed consents were obtained from the participants after the aims and objectives of the study had been explained to them. Previously trained research assistants who are of Psychology students and clinical Psychologists explained the size of a standard drink to those agreeing to participate. A standard drink was defined as equivalent volumes containing an average of 13.5 g ethanol.
Data were collected using a pretested, semi-structured questionnaire incorporating sociodemographics, and the diagnoses made by the attending physicians. The participants also completed the alcohol use disorders identification test (AUDIT) questionnaire and the patient health questionnaire (PHQ-9). The AUDIT is a self-administered questionnaire including three items on the amount and frequency of drinking, three on alcohol dependence, and four on common problems caused by alcohol. Each item is scored 0-4, giving a total score of 40. Several studies have shown its validity and reliability in the detection of hazardous drinking, alcohol misuse, and alcohol dependence.[15] While this study, a score of 8 and above for men; and score 7 and above for female indicated AUDs. Subjects’ occupation was classified according to the system of Boroffka and Olatawura[16] which is well-operationalized and is comparable to other systems like the International Labor Organization classificatory system.[17] It has also been widely used in previous studies in this environment.[18,19] The categories are as follows: Group I consists of professionals with university degrees, e.g., doctors, lawyers, scientists, etc.; group II consists of professionals without university degrees and include teachers, administrators, large scale farmers, and armed forces officers; group III consists of clerks, motor vehicle drivers, mechanics, etc.; group IV consists of cooks, small-scale farmers, barbers, etc.; group V includes laborers and petty traders; group VI includes full-time housewives, students, and unemployed educated youths.
The PHQ-9 consists of nine items, each of which is scored 0-3, providing a 0-27 severity score. PHQ-9 severity is calculated by assigning scores of 0, 1, 2, and 3, to the response categories of - not at all, — several days, — more than half the days, and nearly every day, respectively. PHQ-9 total score for the nine items ranges from 0 to 27.[20] It consists of the nine criteria for depression from the Diagnostic and Statistical Manual of Mental Disorders, fourth edition.
Data analysis
The Statistical Package for the Social Sciences version 16 (SPSS.16) program was used for statistical analysis. Results were calculated as frequencies (%), means, and standard deviations (SD). T-test for continuous data and Chi-square for categorical data were used to examine differences between groups. The level of significance was set at P < 0.05.
RESULTS
General measures
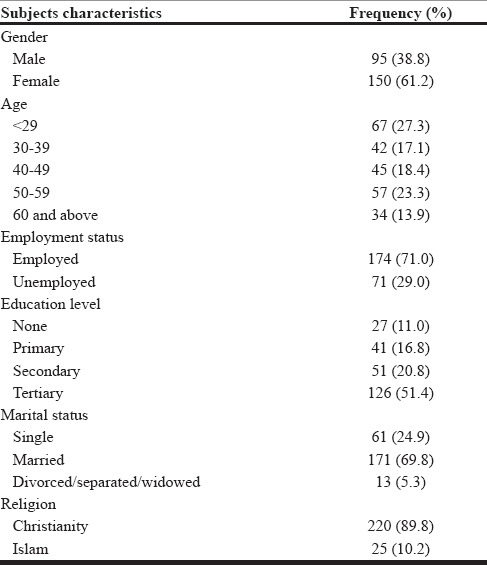
A total of 245 participants completed both the PHQ-9 and the AUDIT questionnaires. The age of the participants ranges from 18 to 65 years with a mean of 42.07 (SD = 13.93) 23 (9.4%) had AUDIT score indicating AUDs. The AUDIT scores of the participants ranges from 0 to 29 with a mean of 1.3 (SD = 4.08). The group includes 150 (61.2%) females. The mean AUDIT score for male is 2.68 SD = 5.875 and for female is 0.48 (SD = 1.889, P = 0.000). The PHQ score ranges from 0 to 23 with a mean of 5.99 (SD = 5.17). Most (69.8%) were married to only 13 (5.3%) constituting either separated or divorced or widowed. Other sociodemographic characteristics are as shown in Table 1.
Table 1.
Sociodemographic characteristics of the respondents
Sociodemographic characteristics and alcohol use disorders [Table 2]
Table 2.
Sociodemographic characteristics and AUDs
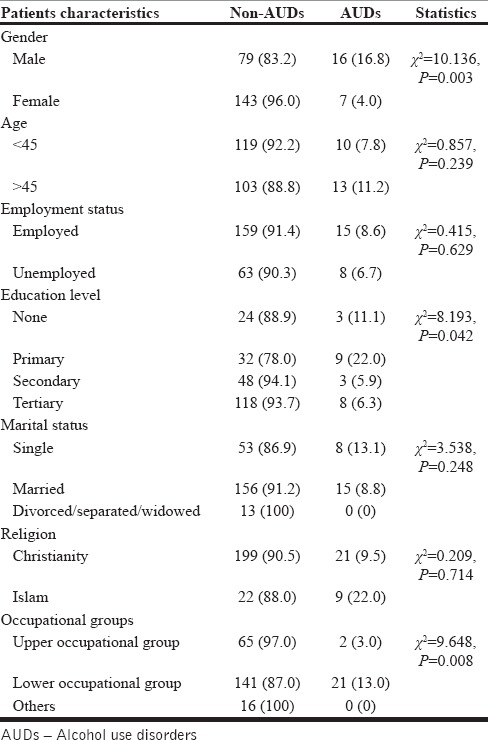
Of the 23 who had AUDIT score indicating AUDs, 18 (18.9%) of males and the remaining 5 (4.0%) of women had AUDs. The association between gender and AUDs was statistically significant (χ2 = 10.136, P = 0.003). Higher proportion (11.2%) of those aged 45 and above had AUDs compared to 7.8% of those aged below 45 years, however, this was not statistically significant (χ2 = 0.857, P = 0.239). A greater proportion of those with primary education (22.0%); compared to secondary (5.9%) or tertiary education (6.3%) had AUDs. The association between level of education and AUDs was statistically significant (χ2 = 8.198, P = 0.042). No statistically significant association was found between marital status (P = 0.170), average income per month (P = 0.463), religion (P = 0.714), and employment status (P = 0.629).
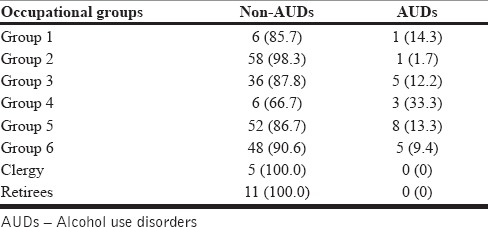
As shown in Table 3, analysis of occupational group in relation to AUDs shows that higher proportion of participants in occupational group IV had AUDs. Categorizing occupational groups into upper, lower, and others shown that majority of those in the lower occupational group compared to other groups had AUD, and this was statistically significant (P = 0.008).
Table 3.
Occupational group and AUDs
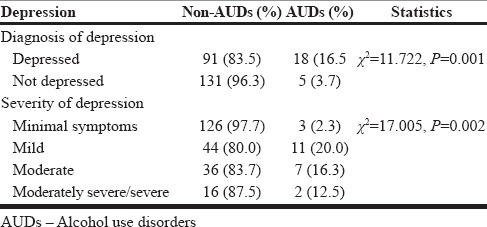
Depression and alcohol use disorders
Table 4 shows that 18 (16.5%) of those who had significant depressive symptoms compared with 5 (3.7%) of those without significant depressive symptoms had AUDs. Significant depressive symptoms was significantly associated with AUDs (χ2 = 11.722, df = 1, P = 0.001). Most of the participants with AUDs presented with mild to moderate depression.
Table 4.
Relationship between depression and AUDs
DISCUSSIONS
Most alcohol-related harm is attributable to hazardous/harmful drinking.[21,22] This study looked at the pattern and the predictors of harmful alcohol drinking among patients visiting the Family physician at the general out-patient clinic. Twenty-three (9.3%) of the population studied have AUDs. This prevalence is relatively similar to what was reported by Gureje et al.,[5] however, it is lower compared with that reported by Abiodun et al.[18] both in Nigeria and likewise lower when compared with other studies in Africa; by Kullgren et al.[23] in Uganda and Peltzer[3] in South Africa. The difference observed in the prevalence rates may not be too surprising as difference sociocultural practices and cultural view of AUDs are influenced by prevalent norm in the society. It has been suggested, even though some similarities exist with respect to the definition of problematic alcohol use in ethnically diverse societies, very substantial differences also exist.[24] The variations in the study methods used, including how alcohol use and various disorders are defined and the sensitivity of the instruments used, is another major factor. The variability in the response of the respondents to alcohol use may also be a factor.
Like in most studies,[3,6,18,23,25,26] our study found a significant association between AUDs with some sociodemographic variables. There was male dominance among patients with AUDs. Similar findings had been reported in this environment. Indeed, in a study by Abiodun et al.[18] all the participants with AUDs were males. The cultural practices and perception which is permissive to men drinking alcohol and the occupational engagement of men are possible reasons for this observation. Besides, men also take alcohol to enhance sexual performance, for social acceptance and to overcome societal stresses.[27] A higher prevalence of AUDs is seen among those age 45 years and above compared to those below 45 years. Though our study did not find a significant association between age group and AUDs, the study by Abiodun et al. reported a significant association between older age group and AUDs. Nonetheless, there is a considerable variation in the pattern and prevalence of AUDs in different age groups. Some authors have reported higher prevalence among younger age group[26,28] while some have reported higher prevalence among older age group.[18,29,30] The possible explanation for the pattern observed in this study may due to the fact that the study is based in the hospital; and many young people with alcohol problems may not patronize the hospital but rather engage self-medication.[31] Studies have shown that young people tend to find it difficult to ask for help especially when it comes to health issues.[29,30,31,32,33,34,35] Thus, whenever young people face health concerns, they often seek health care informally; in other words, they do not refer to health professionals or to formal health services first.
There is a significant association between educational level and AUDs. Even though, majority of patients in our study had tertiary education, however, a larger proportion of those with primary education compared with other groups had AUDs. This observation may also explain the higher prevalence of AUDs among those in lower occupational group. Similarly, other authors[18,26] have reported an association between low educational level and AUDs. The fact that those with lower education engaged more in manual works such as driving, bricklaying, laborers and other occupation that expose them to the risk, and encourage use of drugs as an “enhancer” may possibly explain this observation. Besides, this group is more likely to take more of local gin that contains a higher concentration of alcohol.
In this study, AUDs is significantly associated with the presence of significant depressive symptoms. About a quarter of those with significant depressive symptoms compared to barely 4% of those without significant symptoms had AUDs, and most of these are likely to present with mild to moderate form of depression. Previous studies[36,37] have found that anxiety and depression were associated with AUDs and identifying alcohol use in these groups of people may be particularly important. People with AUDs often have co-occurring psychiatric disorders, most importantly depression; furthermore, they experienced an adverse health outcome, and repeated hospital admissions.[38] The association between AUDs and depression also increases the possibility of suicide because alcohol abuse can exaggerate depression and increases impulsiveness and impairs judgment.
CONCLUSIONS
Alcohol use disorders are relative lower in this population compared with other studies, but however significant. AUDs are associated with gender, low educational, low occupational group, and the presence of significant depressive symptoms mostly in the mild or moderate severity. Identifying the group at risk in clinical setting may go a long way in reducing the adverse effect of AUDs in our society.
ACKNOWLEDGMENTS
The authors want to thank the Residents in the Family medicine department for their assistance during the period of data collection.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.Reid MC, Fiellin DA, O’Connor PG. Hazardous and harmful alcohol consumption in primary care. Arch Intern Med. 1999;159:1681–9. doi: 10.1001/archinte.159.15.1681. [DOI] [PubMed] [Google Scholar]
- 2.Abiodun OA. Alcohol-related problems in primary care patients in Nigeria. Acta Psychiatr Scand. 1996;93:235–9. doi: 10.1111/j.1600-0447.1996.tb10640.x. [DOI] [PubMed] [Google Scholar]
- 3.Peltzer K. Prevalence of alcohol use by rural primary care outpatients in South Africa. Psychol Rep. 2006;99:176–8. doi: 10.2466/pr0.99.1.176-178. [DOI] [PubMed] [Google Scholar]
- 4.Ward CL, Mertens JR, Flisher AJ, Bresick GF, Sterling SA, Little F, et al. Prevalence and correlates of substance use among South African primary care clinic patients. Subst Use Misuse. 2008;43:1395–410. doi: 10.1080/10826080801922744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gureje O, Obikoya B, Ikuesan BA. Alcohol abuse and dependence in an urban primary care clinic in Nigeria. Drug Alcohol Depend. 1992;30:163–7. doi: 10.1016/0376-8716(92)90021-4. [DOI] [PubMed] [Google Scholar]
- 6.Pengpid S, Peltzer K, Van der Heever H. Prevalence of alcohol and associated factors in urban hospital out-patient clinic in South Africa. Int J Environ Res Public Health. 2011;8:2629–39. doi: 10.3390/ijerph8072629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Peltzer K, Matseke G, Azwihangwisi M. Evaluation of alcohol screening and brief intervention in routine practice of primary care nurses in Vhembe district, South Africa. Croat Med J. 2008;49:392–401. doi: 10.3325/cmj.2008.3.392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.WHO. Alcohol Fact Sheet, February. 2011. Available from http://www.who.int/mediacentre/factsheets/fs349/en .
- 9.WHO. 2003. [Last accessed 14th Oct, 2014]. Available from: http://www.who.int/substance_abuse/publications/en/SBIFactSheet.pdf .
- 10.Omolase CO, Afolabi OT, Omolase BO, Ihemedu CO. Drink-driving among commercial drivers in a Nigerian community. Middle East J Psychiatry Alzheimer's. 2011;2:15–9. [Google Scholar]
- 11.Owoaje ET, Amoran OE, Osemeikhain O, Ohnoferi OE. Incidence of road traffic accidents and pattern of injury among commercial motorcyclists in a rural community in South Western Nigeria. J Community Med Prim Health Care. 2005;17:7–12. [Google Scholar]
- 12.Welcome MO, Pereverzev VA. Limit of blood alcohol concentration: A major problem to solve in Nigeria. Eur Psychiatry. 2010;25(Suppl 1):544. [Google Scholar]
- 13.Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG. Guidelines for Use in Primary Care. Switzerland, Geneva: World Health Organization; 2001. AUDIT: The Alcohol Use Disorders Identification Test. [Google Scholar]
- 14.Anderson P. Management of alcohol problems: The role of the general practitioner. Alcohol Alcohol. 1993;28:263–72. [PubMed] [Google Scholar]
- 15.Piccinelli M, Tessari E, Bortolomasi M, Piasere O, Semenzin M, Garzotto N, et al. Efficacy of the alcohol use disorders identification test as a screening tool for hazardous alcohol intake and related disorders in primary care: A validity study. BMJ. 1997;314:420–4. doi: 10.1136/bmj.314.7078.420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Boroffka A, Olatawura MO. Community psyciatry in Nigeria — the current status. Int J Soc Psychiatry. 1977;23:275–81. doi: 10.1177/002076407702300406. [DOI] [PubMed] [Google Scholar]
- 17.Yearbook of Labour Statistics. Vol. 53. Geneva: International Labour Office; 1994. International Labour Organization (ILO). The Revised International Standard Classification of Occupation (ISCO-88) pp. 1122–3. [Google Scholar]
- 18.Abiodun OA, Ajiboye PO, Buhari ON, Ayanda KA, Adefalu OM, Adegboye LO. Alcohol-related disorders among medical and surgical in-patients in a Nigerian teaching hospital. Ann Afr Med. 2013;12:120–6. doi: 10.4103/1596-3519.112407. [DOI] [PubMed] [Google Scholar]
- 19.Eze GO, James BO, Omoaregba JO, Osahan RO. Psychosocial characteristics of patients admitted to a drug rehabilitation unit in Nigeria. Int J Health Res. 2009;2:333–8. [Google Scholar]
- 20.Cameron IM, Crawford JR, Lawton K, Reid IC. Psychometric comparison of PHQ-9 and HADS for measuring depression severity in primary care. Br J Gen Pract. 2008;58:32–6. doi: 10.3399/bjgp08X263794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gururaj G, Girish N, Benegal V. New Delhi: World health Organization, Regional Office for South East Asia; 2006. Alcohol Control Series 1: Burden and Socio-Economic Impact of Alcohol — The Bangalore Study. [Google Scholar]
- 22.Anderson P. Alcohol as a key area. BMJ. 1991;303:766–9. doi: 10.1136/bmj.303.6805.766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kullgren G, Alibusa S, Birabwa-Oketcho H. Problem drinking among patients attending primary healthcare units in Kampala, Uganda. Afr J Psychiatry (Johannesbg) 2009;12:52–8. doi: 10.4314/ajpsy.v12i1.30279. [DOI] [PubMed] [Google Scholar]
- 24.Gureje O, Mavreas V, Vazquez-Barquero JL, Janca A. Problems related to alcohol use: A cross-cultural perspective. Cult Med Psychiatry. 1997;21:199–211. doi: 10.1023/a:1005397700193. [DOI] [PubMed] [Google Scholar]
- 25.Mbatia J, Jenkins R, Singleton N, White B. Prevalence of alcohol consumption and hazardous drinking, tobacco and drug use in urban Tanzania, and their associated risk factors. Int J Environ Res Public Health. 2009;6:1991–2006. doi: 10.3390/ijerph6071991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Brisibe S, Ordinioha B. Socio-demographic characteristics of alcohol abusers in a rural Ijaw community in Bayelsa State, South-South Nigeria. Ann Afr Med. 2011;10:97–102. doi: 10.4103/1596-3519.82066. [DOI] [PubMed] [Google Scholar]
- 27.Demel R, Hagen J. The structure of positive alcohol experiences in alcohol dependent in-patients. Addict Res. 2004;12:125–40. [Google Scholar]
- 28.Wu SI, Liu SI, Fang CK, Hsu CC, Sun YW. Prevalence and detection of alcohol use disorders among general hospital inpatients in eastern Taiwan. Gen Hosp Psychiatry. 2006;28:48–54. doi: 10.1016/j.genhosppsych.2005.08.002. [DOI] [PubMed] [Google Scholar]
- 29.Nair MG, Pillay SS. Psychiatric disorder in a South African general hospital. Prevalence in medical, surgical, and gynecological wards. Gen Hosp Psychiatry. 1997;19:144–8. doi: 10.1016/s0163-8343(97)00147-3. [DOI] [PubMed] [Google Scholar]
- 30.Coder B, Freyer-Adam J, Bischof G, Pockrandt C, Hartmann B, Rumpf HJ, et al. Alcohol problem drinking among general hospital inpatients in Northeastern Germany. Gen Hosp Psychiatry. 2008;30:147–54. doi: 10.1016/j.genhosppsych.2007.10.007. [DOI] [PubMed] [Google Scholar]
- 31.Zimmer-Gembeck MJ, Alexander T, Nystrom RJ. Adolescents report their need for and use of health care services. J Adolesc Health. 1997;21:388–99. doi: 10.1016/S1054-139X(97)00167-5. [DOI] [PubMed] [Google Scholar]
- 32.El Kahi HA, Abi Rizk GY, Hlais SA, Adib SM. Health-care-seeking behaviour among university students in Lebanon. East Mediterr Health J. 2012;18:598–606. doi: 10.26719/2012.18.6.598. [DOI] [PubMed] [Google Scholar]
- 33.Pommier J, Mounchtouris A, Billot L, Romero MI, Zubarew T, Deschamps JP. Self-reported determinants of health service use by French adolescents. Int J Adolesc Med Health. 2011;13:115–30. doi: 10.1515/IJAMH.2001.13.2.115. [DOI] [PubMed] [Google Scholar]
- 34.Gould MS, Munfakh JL, Lubell K, Kleinman M, Parker S. Seeking help from the internet during adolescence. J Am Acad Child Adolesc Psychiatry. 2002;41:1182–9. doi: 10.1097/00004583-200210000-00007. [DOI] [PubMed] [Google Scholar]
- 35.Elliott BA, Larson JT. Adolescents in mid-sized and rural communities: Foregone care, perceived barriers, and risk factors. J Adolesc Health. 2004;35:303–9. doi: 10.1016/j.jadohealth.2003.09.015. [DOI] [PubMed] [Google Scholar]
- 36.Swendsen JD, Merikangas KR. The comorbidity of depression and substance use disorders. Clin Psychol Rev. 2000;20:173–89. doi: 10.1016/s0272-7358(99)00026-4. [DOI] [PubMed] [Google Scholar]
- 37.Arch JJ, Craske MG, Stein MB, Sherbourne CD, Roy-Byrne PP. Correlates of alcohol use among anxious and depressed primary care patients. Gen Hosp Psychiatry. 2006;28:37–42. doi: 10.1016/j.genhosppsych.2005.08.007. [DOI] [PubMed] [Google Scholar]
- 38.Vikram P. Alcohol use and mental health in developing countries. Ann Epidermiol. 2007;17:87–92. [Google Scholar]


