Abstract
Globally, the solution-focused brief therapy is practiced in persons with depression. In India, fewer studies have documented about the treatment outcome of solution-focused therapy among persons with depression. The current study was carried out with a 19-year-old girl, studying SSLC (10th Standard) was diagnosed with moderate depression. She had difficulty in attention, concentration, memory, irritability and sad mood, poor academic performance, guilt feelings, lethargic, anhedonia, decreased sleep, and decreased appetite. The case worker has chosen provided 6 sessions of solution focused therapy for depression. There was considerable improvement in her symptoms and in scholastic performance. The current study supports the effectiveness of solution-focused therapy in persons with depression.
Keywords: Adolescent, depression, solution-focused therapy
INTRODUCTION
Solution-focused brief therapy (SFBT) was developed during the 1980s by de Shazer and Insoo Kim Berg. It proposes that the development of a solution is not necessarily related to the problem.[1]
A randomized experimental design study compared a single session of SFBT with a single session of Interpersonal Psychotherapy for depression in the treatment of 40 depressed female college students. This study demonstrated that single session SFBT was effective in reducing depressed mood.[2] In a study, SFBT with 10 clients with depression was applied. Nine of the subjects showed clinically significant improvement.[3] In addition, in a randomized controlled study, the SFBT was compared with cognitive behavior therapy (CBT) and was found that SFBT performed slightly worse than CBT.[4] Another study conducted in Finland showed similar positive results for brief psychodynamic therapy and SFBT, with SFBT clients improved earlier in therapy than client's in brief psychodynamic therapy.[5]
CASE REPORT
Ms. S, a 19-year-old girl, failed in SSLC, presented with pervasive sad mood, decreased interest in studies, poor academic performance, irritable over trivial issues, anger outbursts, crying spells, guilt feelings, feeling of worthlessness, disturbed sleep, reduced appetite, difficulty in attention and concentration.
In year 2007, Ms. S started complaining that she is unable to remember what was taught in class room as well as whatever she was reading. Gradually, her academic performance had come down significantly by 2008. Since 2008, mother reported that Ms. S gets irritable over trivial issues, anger out bursts and occasionally beats her sister. Subsequently, Ms. S became dull and lethargic later. In spite of these, there was a pressure from mother to perform better studies as she was performing very poor in her academics. So, the client started to think that she is a failure, she cannot clear her exams, better to die rather than living. However, client did not attempt for suicide. She also felt guilty that she was unable to fulfill the dreams of her parents with respect to academics.
Ms. S was not attending Bharatanatyam classes and meditation classes, which she used to before the onset of the symptoms. Client's sleep and food intake had come down gradually. Ms. S was given anti-depressant medication by the consultant psychiatrist for 2 months, and there was no adequate improvement in her depressive symptoms except her sleep.
The therapist followed single subject research design A-B outcome design with baseline and treatment phase to test the treatment gains. Hamilton Depression Rating Scale (HAM-D) was used to assess the severity of the depression. The scale has 21 items, and the total score 0-7 shows normal, 8-13 mild, 14-18 moderate, 19-22 severe, above 23 very severe. HAM - D demonstrated high levels of reliability (ra = .91 to .94, ra = .95 to .96). Extensive validity evidence was presented, including content, criterion related, construct, and clinical efficacy of the HDI cutoff score. The client had scored 21 on HAM – D (moderate depression) at baseline, and it had come down to 6 (normal) after providing solution-focused therapy [Figure 1].
Figure 1.
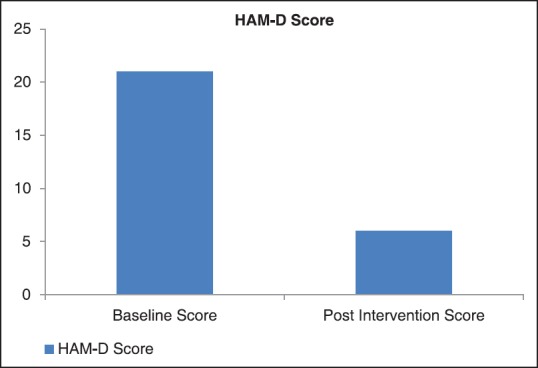
Depression levels at baseline and post-intervention
The case worker had listened to the client attentively and empathetically about her concerns. The client was anxious and worried about her academic difficulties and parents pressure to perform better in the academics. The detailed information was elicited from the client about her problems and experiences. This has increased client's understanding about her problem. The case worker has validated her feelings and concerns. This has brought some amount of positive change in the client as she felt that the case worker has understood her problem. The case worker and the client sat together and discussed about future goals. The goals were clear, simple, and attainable. Though the client felt hopeful, she did not have clarity about how to achieve her goals.
Identified goals were: 1. Managing academic stress, 2. Enhancing attention and concentration, and 3. Planned preparation for exams.
The miracle question
The miracle question devised by Steve de Shazer (1988) was asked to the client in each session.
Imagine when you go to sleep one night a miracle happens and the problems you have been talking about disappear. As you were asleep, you did not know that a miracle happened. When you woke up, what would be the first signs for you that a miracle had happened?
Scaling
On a 0 to 10 scale with 10 representing the best it could be and 0 as worst it has been. The aim of scaling was to measure the progress as sessions goes on. The client has mentioned her score as 2. As the sessions progressed, the scores have increased, which means Ms. S has improved significantly.
Discovering the client's resources
The case worker has discussed about the clients problems in the past and how they were managed. The case worker found that: The client was practicing Bharatanatyam and going for evening walk with friends. She also used to practice western dance with her sister. According to client, these activities were her main source of coping. Client reported that she used to feel free and active after doing Bharata Natyam. While she was in SSLC, the client stopped doing all these things due to academic pressure. The case worker has discussed about possibility to start doing these activities. The case worker also discussed with mother about the need for sending client for Bharata Natyam. The client started going to Bharata Natyam classes and evening walk with her friends. Gradually, her score on scaling has increased. The case worker has given positive feedback at the end of each session. Client efforts to change, regularity to sessions, honesty, and commitment were identified and reflected on her.
DISCUSSION
In developing and under developed countries, the cost of mental health care is high. The medication side-effects, costly medicine, lower socio-economic status, non-availability of drugs, irregular follow up may cause relapse of depression and depression indicated high percentage of relapse.[6] Hence, a brief solution-focused therapy would help the client in reducing health care cost and preventing relapse.
The results of current study support the previous study findings that solution-focused therapy for clients with mild to moderate depression can be successful with less number of sessions.[7] After undergoing the therapy, the client was not only improved from depression but her academic performance was also improved significantly. The solution-focused therapy can be tailored to meet specific symptoms and resources of the client. However, the therapist needs professional training before practicing solution-focused therapy.
CONCLUSION
Overall, the current study constructs on the existing empirical base supporting the use of solution-focused therapy in the treatment of mild to moderate depression. In this brief therapies era, where clients also do not have much time to come for more number of sessions, solution-focused therapy is very helpful. Intervention research studies on efficacy and cost-effectiveness of solution-focused therapy in clients having mild to moderate depression can be carried out.
Footnotes
Source of Support: Nil
Conflict of Interest: None.
REFERENCES
- 1.O’ Connell B. Solution focused therapy. In: Palmer S, editor. Brief Therapies Series. London: SAGE Publications; 2005. p. 1. [Google Scholar]
- 2.Sundstrom SM. Ames: Iowa State University; 1993. Single session psychotherapy for depression: Is it better to focus on problems or solutions? [Google Scholar]
- 3.Lee MY, Greene GJ, Mentzer RA, Pinnell S, Niles D. Solution focused brief therapy and the treatment of depression: A pilot study. J Brief Therapy. 2001;1:33–49. [Google Scholar]
- 4.Linssen F. Berlin, Germany: paper presented at the European brief therapy association conference; 2003. Solution focused therapy for anxiety and depression: A controlled study. [Google Scholar]
- 5.Knekt P, Lindfors O. Helsinki, Finland: The Social Insurance Institution; 2004. A randomized trial of the effect of four forms of psychotherapy on depressive and anxiety disorders: Design, methods and results on the effectiveness of short term psychodynamic psychotherapy and solution focused therapy during one year follow up, in Studies in Social Security and Health, No. 77. [Google Scholar]
- 6.Hollon SD, Beck AT. Cognitive and Cognitive behavior therapies. In: Lambert MJ, editor. Bergin's and Garfield's hand book of psychotherapy and behavior change. New York: Wiley; 2004. p. 447. [Google Scholar]
- 7.Estrada B, Beyebach M. Solution focused therapy with depressed deaf patients. Journal of Family Psychotherapy. 2007;18:45–63. [Google Scholar]


