Abstract
Purpose
Asthma is a complex disease, with contributions from multiple genes, various genetic backgrounds, and environmental factors. Many human epidemiological studies have demonstrated that single nucleotide polymorphisms (SNPs) in Toll-like receptor (TLR) genes are inconsistently associated with asthma risk. Some have demonstrated differences concerning the study design and effect size, and conflicting results have been reported. A meta-analysis is necessary to determine the magnitude of this association.
Methods
Following the Preferred Reporting Items for Systematic Reviews and Meta-analyses guidelines, a systematic search and meta-analysis of the literature was conducted to estimate the association of SNPs in TLR genes with asthma risk. We screened the medical literature based on the following keyword searches in MEDLINE and EMBASE databases: 'TLR', 'polymorphism', 'asthma', and their combinations.
Results
Meta-analysis of eight studies on TLR4 Asp299Gly showed a marginal association of TLR4 with asthma risk (odds ratio [OR]=0.814 [95% confidence interval [CI], 0.652-1.016; P=0.069]) in the recessive model. TLR4 Thr399Ile was not associated with asthma risk under any genetic model. Meta-analysis of four studies on TLR2 Arg753Gln indicated that TLR2 might be significantly associated with asthma in the dominant and codominant models (P=0.029, P=0.030, and P=0.009, respectively). TLR9 -1237 was marginally associated with asthma risk (OR=0.408 [95% CI, 0.163-1.021; P=0.065]) in the codominant model. Analysis using the allele contrast model showed that the major TLR9 -1237 T allele tended to be a significant protective factor with OR=0.689 (95% CI, 0.471-1.007; P=0.055).
Conclusions
The results showed that TLR4 Asp299Gly, TLR2 Arg753Gln, and TLR9-1237 might contribute significantly to asthma susceptibility. Future genetic association studies would consolidate these findings.
Keywords: Asthma, TLR genes, SNPs, association, meta-analysis
INTRODUCTION
Asthma is a chronic and complex disorder of the respiratory system characterized by airway obstruction and inflammation,1 and its prevalence is increasing in both developed and developing countries.2,3 This increased prevalence may reflect increased exposure to environmental risk factors. Although environmental factors are important determinants of asthma, numerous studies have revealed that asthma has a strong genetic component. Susceptibility genes have been identified by candidate gene association studies, genome-wide linkage studies, and genome-wide association studies.4 Many genes have been shown to make small contributions to the overall phenotype.
Toll-like receptors are an essential family of innate immune pattern recognition receptors that play a pivotal role in host defense against microbes.5 TLRs can modulate the immune system through cellular activation, modulation of cytokine secretion6 and production of soluble factors to local dendritic networks.7 Human epidemiological studies have supported the common clinical perception that TLRs are associated with asthma. These studies have varied in design, population composition, asthma definition and size. Macrophages, one of the main immune cell types involved in asthma, express various TLRs, including TLR2, 4, 5, 6, 7, 8, and 9.8 Each TLR recognizes different classes of molecules expressed by pathogens and recognizes structurally conserved motifs.9
TLR1 and 6 recognize multiple diacyl peptides, and TLR1/2 dimers can recognize lipopeptides.10 TLR2, which has been found to be expressed by various cell types,11 is related to protection against allergies and allergic asthma by sensing pathogen-associated patterns in lipoproteins and lipopeptides. The TLR2/6 dimer is involved in the recognition of diacylated lipopeptides.12 Long-term stimulation of TLR3 upregulates the production of inflammatory cytokines and cellular recruitment to the airways.13 TLR4 encodes a macrophage cell-surface receptor, which is principally activated by bacterial endotoxin, also known as lipopolysaccharide (LPS). Few studies of the role of TLR5 in asthma have been reported. However, a significant decrease in the expression of TLR5 was observed in asthma patients,14 and TLR5 recognizes bacterial flagellin when complexed with TLR4.15 Similar to TLR5, few data exist on the role of TLR6 in allergic asthma.12 TLR6 is expressed on mast cells, which play important roles in allergy.16 TLR7 and TLR8, which are localized on the sex chromosome Xp22,17 recognize single-stranded RNA, and induce interferons (IFNs) to protect the host from viral infection.18 TLR9 detects bacterial or viral DNA with unmethylated cytosine and guanine.8 TLR10 is the most recently identified gene in the TLR family whose product recognizes pathogen-associated molecular patterns (PAMPs).19 TLRs are also involved in various signaling pathways of the immune system that protect from asthma or develop asthma phenotypes.20,21,22,23,24,25
Most studies published since 2004 have comprised genetic association investigations in various clinical settings, and have found positive associations of SNPs in TLR2,26,27,28 TLR4,29 TLR6,30 TLR7/8,31 TLR9,32 and TLR1019 with asthma. Recent insights into the complex mechanisms of human innate immunity have suggested that genetic variability in genes may play a role in the development of asthma and related diseases.34,35,36,37,38
Due to the important contribution of TLR genes to asthma, an updated meta-analysis was conducted to estimate the effect of SNPs in TLR genes on asthma susceptibility.
MATERIALS AND METHODS
Identification of eligible studies
The review process followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines.39 We performed a literature search using the MEDLINE and EMBASE databases to identify articles that examined associations between TLR polymorphisms and asthma. Combinations of keywords, such as 'TLR', 'polymorphism', and 'asthma' were entered as medical subject heading (MeSH) and text words. References in the identified studies were used to identify additional studies not indexed by MEDLINE or EMBASE databases. No language or date restrictions were applied.
Inclusion and exclusion criteria
Studies identified from the searches were screened and excluded from further analysis if one of the following reasons was satisfied: a review article, lack of information, animal research, not case-control or nested case-control study design, or unreported genotype frequencies.
For inclusion, the studies must have met the following criteria: (1) they evaluated TLR gene polymorphisms and asthma; (2) were case-control studies; (3) supplied the number of individual genotypes in asthmatic cases and in controls, respectively; or (4) they had an asthma outcome definition that followed accepted diagnostic guidelines.
Data extraction
Information was extracted carefully from all of the eligible publications independently by 2 authors, based on the inclusion criteria above. The following information was extracted from each study: author, year of study publication, ethnicity of the study population, demographics (age), asthma status, and number of cases and controls for each TLR polymorphism.
Statistical analysis
Data from the studies were combined to provide a summary odds ratio (OR). Summary ORs were represented as a point estimate with 95% confidence intervals (CIs) on a forest plot.40 The heterogeneity of the data was evaluated using the Q statistic.41 The stability of the summary risk estimate was evaluated using a sensitivity analysis in which each study was removed individually, and the OR was recalculated. Egger's regression test was used to identify publication bias.42
RESULTS
Study inclusion and characteristics
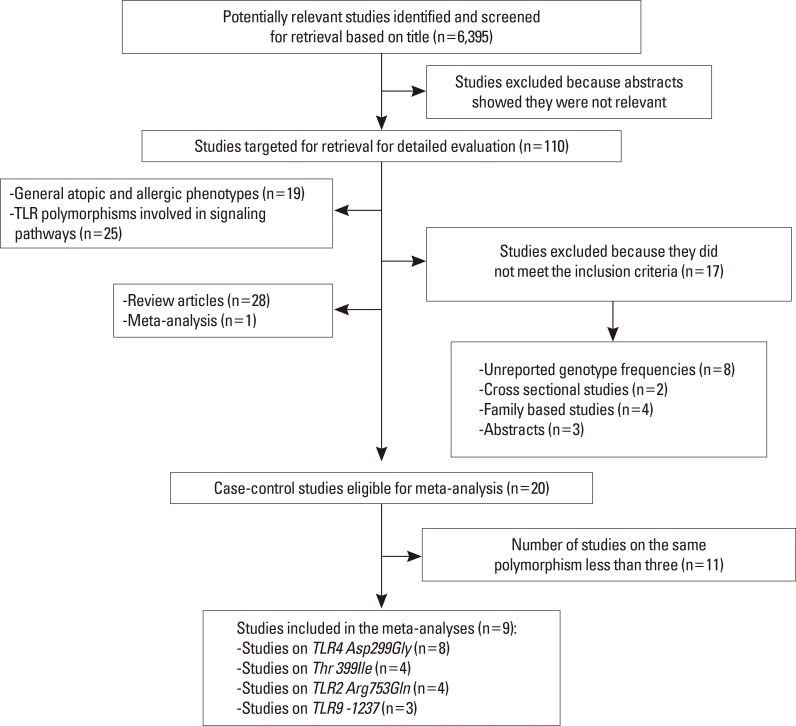
The initial search using the headings 'TLR', 'polymorphism' 'asthma', and their combinations resulted in approximately 6,395 journal articles. Based on the titles, 110 were potentially relevant. Nineteen studies investigating general atopic and allergic phenotypes were excluded. An additional 25 studies on TLR polymorphism involvement in signaling pathways were excluded. Review articles (n=28) were also excluded. Seventeen studies were excluded because they did not meet the inclusion criteria: eight did not report genotypic frequencies in cases and/or in controls24,25,38,43,44,45,46,47; two were cross-sectional studies48,49; four were family-based studies,50,51,52,53 and 3 were abstracts.54,55,56 Twenty case-control studies were eligible for meta-analysis,19,26,27,28,29,30,31,32,33,57,58,59,60,61,62,63,64,65,66,67 one study was in Portuguese,62 and another was in Chinese.64 Among the eligible studies, 11 were excluded because the number of studies of the same polymorphism was less than 3.
The controls for the studies by Lachheb et al.32 and Zhang et al.29 deviated from Hardy-Weinberg equilibrium (HWE) in the controls (P<0.01). The study by Caravalho et al.61 was small, and the definition of asthma was restricted to severe asthma with fungal sensitization. In the study by Palikhe et al.,65 the definition of asthma was limited to aspirin-tolerant asthma. In the study by Yang et al.,58 three sets of patients (first-affected sibling, second-affected sibling and asthmatic parents) were compared with hyper-normal controls. A meta-analysis was conducted when at least 3 studies on the same polymorphism were available. Fig. 1 provides a summary of the search results. Table 1 summarizes the characteristics of the case-control studies.
Fig. 1. Flow diagram of the systematic review and meta-analysis literature search results.
Table 1. Characteristics of the reviewed studies on SNPs in TLR genes and asthma risk.
| Reference | Ethnicity | Age: Case/control | Gender | Gene | Polymorphism | Case | Control | Results |
|---|---|---|---|---|---|---|---|---|
| Lazarus 2003 | European-American | Matched | Matched | TLR9 | rs5743836 T/C | 64 | 114 | SA |
| Noguchi 2004 | Japanese (Chinese) | Children/46.9 | Matched | TLR2 | c. -191 G>A | 133 | 186 | NS |
| c. 597 T>C | 133 | 188 | NS | |||||
| c. 1350 T>C | 134 | 190 | NS | |||||
| TLR3 | -7A | 135 | 189 | NS | ||||
| IVS3 +71 C>A | 134 | 188 | NS | |||||
| c. 1377 C>T | 133 | 189 | NS | |||||
| TLR9 | c. 1635 G>A | 132 | 189 | NS | ||||
| Tantisira 2004 | African-American | Matched | Matched | TLR6 | Ser249Pro C>T | 56 | 97 | SA |
| Lazarus 2004 | European-American | Matched | Matched | TLR10 | c.+1031 G>T | 506 | 514 | SA |
| c.+2322 A>G | 505 | 513 | SA | |||||
| Yang 2004 | English (Caucasian) | Matched | Matched | TLR4 | rs4986790 A>G | 320 | 184 | NS |
| Matched | Matched | TLR4 | rs4986790 A>G | 309 | 184 | NS | ||
| Matched | Matched | TLR4 | rs4986790 A>G | 185 | 184 | NS | ||
| Hoffjan 2005 | German (Caucasian) | 38/59 | Matched | TLR6 | Ser249Pro C>T | 68 | 212 | NS |
| 9.5/59 | Ser249Pro C>T | 132 | 212 | NS | ||||
| Smit 2007 | Danish (Caucasian) | 19.2/matched | Matched | TLR2 | rs4696480 A>T | 100 | 87 | NS |
| rs5743704 C>A | 100 | 87 | NS | |||||
| rs5743708 C>T | 100 | 87 | NS | |||||
| TLR4 | rs4986790 A>G | 100 | 87 | NS | ||||
| rs4986791 C>T | 100 | 87 | NS | |||||
| Caravalho 2008 | European (Caucasians) | 57.6±11.8/not mentioned | Matched | TLR2 | rs5743708 G>A | 14 | 80 | NS |
| TLR4 | rs4986790 A>G | 14 | 80 | NS | ||||
| TLR9 | rs5743836 T>C | 14 | 80 | NS | ||||
| Lachheb 2008 | African Caucasian | 10.5/8 | Matched | TLR2 | rs5743708 C>T | 210 | 224 | NS |
| TLR4 | rs4986790 A>G | 210 | 224 | NS | ||||
| rs4986791 C>T | 210 | 224 | NS | |||||
| TLR9 | rs5743836 T>C | 210 | 224 | SA | ||||
| rs187084 T>C | 210 | 224 | NS | |||||
| Larocca 2008 | Venezuelan (American) | 44.6±15.22/42.63±13.89 | Matched | T LR4 | rs4986790 A>G | 100 | 100 | NS |
| rs4986791 C>T | 100 | 100 | NS | |||||
| Bjørnvold 2009 | Norwegian (Caucasian) | Children | Matched | TLR2 | Rs3804100 T>C | 108 | 494 | SA |
| TLR2 | Rs3804099T>C | 108 | 494 | NS | ||||
| Hseih 2009 | Taiwanese (Asian) | 7.2±2.4/Children | Matched | TLR4 | rs10983755 A>G | 117 | 60 | NS |
| rs1927914 C>T | 117 | 60 | NS | |||||
| Zhang 2009 | Chinese (Asian) | 39.80±14.23/34.27±13.31 | Male | TLR7/8 | rs5935436 C>T | 135 | 200 | SA |
| rs3761623 A>G | 135 | 200 | NS | |||||
| rs3764880 G>A | 135 | 200 | NS | |||||
| 39.80±14.23/34.27±13.31 | Female | TLR7/8 | rs5935436 C>T | 183 | 152 | NS | ||
| rs3761623 A>G | 183 | 151 | SA | |||||
| rs3764880 G>A | 182 | 152 | SA | |||||
| Qian 2010 | Chinese (Asian) | 39.80/38.26 | Matched | TLR1 | rs4833095 C>T | 318 | 351 | NS |
| TLR2 | rs7656411 G>T | 317 | 351 | SA | ||||
| TLR6 | rs5743831 A>G | 318 | 352 | NS | ||||
| rs5743808 T>C | 318 | 351 | NS | |||||
| rs2381289 C>T | 318 | 352 | NS | |||||
| TLR10 | rs11466651 G>A | 318 | 352 | NS | ||||
| rs11466655 A>G | 318 | 351 | NS | |||||
| rs4504265 C>A | 317 | 349 | NS | |||||
| Zhang 2011 | Chinese (Asian) | 39.80/38.26 | Matched | TLR4 | rs1927914 T>C | 318 | 350 | SA* |
| rs10983755 G>A | 318 | 351 | ||||||
| rs11536879 A>G | 304 | 348 | ||||||
| rs1927907 G>A | 314 | 334 | ||||||
| Palikhe 2011 | Korean (Asian) | 43.1±15.2/32.1±12.7 | Matched | TLR3 | rs3775296 G>T | 254 | 274 | NS |
| rs3775291 G>A | 254 | 274 | NS | |||||
| Vorvonko 2011 | Russian (Caucasian) | Adults/38.5±10.4 | Matched | TLR4 | rs4986790 A>G | 283 | 227 | NS |
| Qian 2011 | Chinese (Asian) | 1.9-11.6/matched | Matched | TLR9 | rs187084 C/T | 312 | 339 | NS |
| Hussein 2012 | African Caucasian | 8.4±2.6/10.1±2.3 | Matched | TLR2 | rs5743708 G>A | 500 | 250 | SA* |
| TLR4 | rs4986790 A>G | 500 | 251 | |||||
| Şahin 2014 | Turkish (Caucasian) | 36±12.42/43±7.68 | Matched | TLR4 | rs4986790 A>G | 131 | 75 | NS |
| rs4986791 C>T | 131 | 75 | SA |
NS, non significant association; SA, significant association; SA*, significant association with asthma severity.
Data analysis
Association of TLR4 Asp299Gly with asthma risk
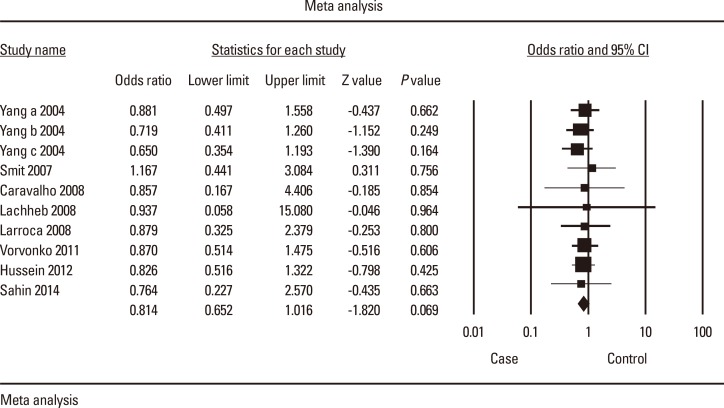
Analyses in the random effects model showed that the TLR4 Asp299Gly polymorphism was marginally associated with asthma under the recessive (0.069) (Fig. 2) and allele contrast (0.055) models. In the allele contrast model, sensitivity analysis by exclusion of any one particular study60 in the influence analysis significantly changed the results. The recalculated OR was 0.803 (95% CI, 0.647-0.997; P=0.047), indicating that the major A allele might protect against asthma (Table 2).
Fig. 2. Forest plot of the association between TLR4 Asp299Gly and asthma risk: AA vs AG+GG. The forest plot shows the odds ratios (ORs) and respective 95% confidence intervals (CIs) for the studies included in the meta-analysis. For each study in the forest plot, the area of the black square is proportional to the study weight, and the horizontal bar represents the 95% CI. Z score: the standardized expression of a value in terms of its relative position in the full distribution of values.
Table 2. Association of TLR4 Asp299Gly A/G, TLR4 Thr399Ile C>T, TLR2 Arg753Gln G/A and TLR9 -1237 T/C with asthma risk.
| TLRs | Genetic model | OR | P-value | I2 | Egger P | |
|---|---|---|---|---|---|---|
| TLR4 Asp299Gly A>G (n=8) | Recessive | AA vs AG+GG | 0.814 (0.652-1.016) | 0.069 | 0.000 | 0.25 |
| Homozygous | GG+AA vs AG | 0.835 (0.666-1.047) | 0.118 | 0.000 | 0.40 | |
| Dominant | AA+AG vs GG | 0.857 (0.297-2.477) | 0.776 | 0.000 | 0.42 | |
| Codominant* | AA vs GG | 0.897 (0.597-1.346) | 0.599 | 0.000 | 0.12 | |
| Codominant* | AG vs GG | 0.831 (0,663-1.042) | 0.110 | 0.000 | 0.40 | |
| Codominant* | AA vs AG | 0.972 (0.320-2.953) | 0.960 | 0.000 | 0.28 | |
| Allele contrast | A allele vs G allele | 0.814 (0.659-1.005) | 0.055 | 0.000 | 0.05 | |
| TLR4 Thr399Ile C>T (n=4) | Recessive | CC vs TC+TT | 0.784 (0.571-1.075) | 0.130 | 0.00 | 0.15 |
| Homozygous | CC+TT vs TC | 1.315 (0.688-2.513) | 0.408 | 0.00 | 0.45 | |
| Dominant | CC+TC vs TT | 0.708 (0.111-4522) | 0.715 | 0.00 | 0.05 | |
| Codominant | CC vs TT | 1.223 (0.655-2.286) | 0.527 | 0.00 | 0.34 | |
| Codominant | CT vs TT | 1.306 (0.683-2.497) | 0.419 | 0.00 | 0.45 | |
| Codominant | CC vs TC | 0.398 (0.053-3.006) | 0.372 | 0.00 | 0.03 | |
| Allele contrast | C allele vs T allele | 1.132 (0.623-2.056) | 0.684 | 0.00 | 0.34 | |
| TLR2 Arg753Gln G>A (n=4) | Recessive | GG vs GA+AA | 0.968 (0.441-2.123) | 0.935 | 18.71 | 0.37 |
| Homozygous | GG+AA vs GA | 2.476 (0.483-12.698) | 0.277 | 57.34 | 0.30 | |
| Dominant | GG+GA vs AA | 0.100 (0.013-0.789) | 0.029 | 0.00 | - | |
| Codominant | GG vs AA | 0.102 (0.013-0.803) | 0.030 | 0.00 | - | |
| Codominant | GA vs AA | 0.01 (0.001-0.312) | 0.009 | 24.25 | - | |
| Codominant | GG vs GA | 2.451 (0.483-12.441) | 0.279 | 56.82 | 0.30 | |
| Allele contrast | G allele vs A allele | 0.635 (0.228-1.771) | 0.385 | 52.24 | 0.47 | |
| TLR9-1237 T>C (n=3) | Recessive | TT vs TC+CC | 0.950 (0.570-1.583) | 0.223 | 33.33 | 0.41 |
| Homozygous | TT+CC vs TC | 1.267 (0.867-1.852) | 0.222 | 0.00 | 0.39 | |
| Dominant | TT+TC vs CC | 0.684 (0.090-5.192) | 0.714 | 85.96 | - | |
| Codominant* | TT vs CC | 0.408 (0.163-1.021) | 0.065 | 30.95 | - | |
| Codominant* | TC vs CC | 0.498 (0.206-1.202) | 0.121 | 16.83 | - | |
| Codominant* | TT vs TC | 0.876 (0.584-1.315) | 0.525 | 0.00 | 0.12 | |
| Allele contrast | T allele vs C allele | 0.689 (0.471-1.007) | 0.055 | 18.73 | 0.27 |
TLR4 Asp299Gly (rs 4986790); TLR4 Thr399Ile (rs4986791); TLR2 Arg753Gln (rs5743708); TLR9 -1237 (rs187084); Bold: significant P value (<0.05). TLR4 Asp299Gly polymorphism: one study removed,60 OR=0.803 (0.647-0.997); P=0.047 in the allele contrast model. TLR2 Arg753Gln polymorphism: one study removed,61 OR=4.460 (1.213-16.396); P=0.024 in the homozygous model; one study removed,61 OR=4.365 (1.2265-15.536); P=0.023 in the GG vs GA codominant model; one study removed,60 OR=0.402 (0.199-0.811); P=0.011 in the allele contrast model.
n, number of studies; OR, odds ratio; I2, heterogeneity test.
*best-fitted genetic model.
The estimated OR1 (AA vs GG), OR2 (AG vs GG) and OR3 (AA vs AG) were 0.897, 0.831, and 0.972, respectively. These estimates were likely to suggest a codominant genetic model. The pooled OR1 was 0.897 (95% CI, 0.597-1.346; P=0.599). Heterogeneity was absent (0.00%). No evidence of publication bias was detected by Egger's test (P=0.12). Sensitivity analysis by the removal of one study did not significantly change the results (Table 2).
Association of TLR4 Thr399Ile C>T with asthma risk
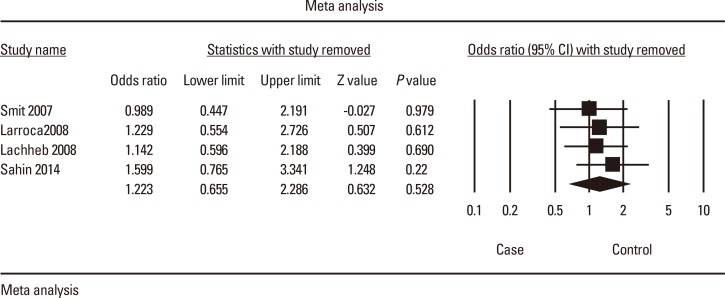
Analyses in the random-effects model showed that the TLR4 Thr399Ile polymorphism was not associated with asthma under any of the genetic models.
The estimated OR1 (CC vs TT), OR2 (CT vs TT) and OR3 (CC vs TC) were 1.223, 1.306, and 0.398, respectively. These estimates did not fit any genetic model. Analysis in the allele contrast model showed no significant association of the TLR4 Thr399Ile C allele with asthma risk (OR=1.223 [95% CI, 0.655-2.286; P=0.528]) (Fig. 3). Heterogeneity was absent in all of the models (0.00%). Sensitivity analysis by the removal of one study did not significantly change the results. Publication bias was detected by Egger's test in the dominant and CC vs TC codominant models (P=0.05 and P=0.03, respectively) (Table 2).
Fig. 3. Forest plot of the association between TLR4 Thr399Ile and asthma risk: C allele vs T allele. The forest plot shows the ORs and respective 95% CIs for the studies included in the meta-analysis. For each study in the forest plot, the area of the black square is proportional to the study weight, and the horizontal bar represents the 95% CI. Z score: the standardized expression of a value in terms of its relative position in the full distribution of values.
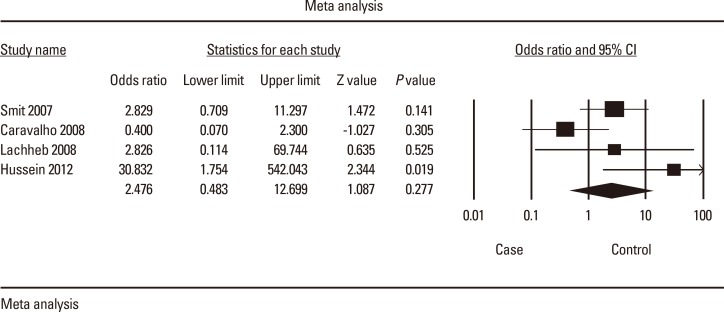
Association of TLR2 Arg753Gln G/A with asthma risk
Analyses showed that the TLR2 Arg753Gln polymorphism was not associated with asthma under the recessive, homozygous (Fig. 4) and allele contrast models. In the homozygous model, sensitivity analysis by the removal of one study61 significantly changed the results. The recalculated OR was 4.460 (95% CI, 1.213-16.396), indicating that the homozygous genotypes might be a significant risk factor (P=0.024). In the GG vs GA model, when one study was removed,61 the recalculated OR was 4.365 (95% CI, 1.227-15.536), suggesting that the homozygous genotype might be a significant risk factor (P=0.023). Sensitivity analysis by the removal of one study60 in the allele contrast model significantly changed the results. The recalculated OR was 0.402 (95% CI, 0.199-0.811), indicating that the major G allele might protect significantly against asthma (P=0.011).
Fig. 4. Forest plot of the association between TLR2 Arg753Gln and asthma: GG+AA vs GA. The forest plot shows the ORs and respective 95% CIs for the studies included in the meta-analysis. For each study in the forest plot, the area of the black square is proportional to the study weight, and the horizontal bar represents the 95% CI. Z score: the standardized expression of a value in terms of its relative position in the full distribution of values.
The estimated OR1 (GG vs AA), OR2 (GA vs AA) and OR3 (GG vs GA) were 0.102, 0.01, and 2.451, respectively. These estimates did not fit any genetic model. Only three studies were available; therefore, estimates were not sufficiently powerful. However, these estimates provided a first indication that genotypes with at least one copy of the major G allele might be protective. No evidence of publication bias was detected by Egger's test in all of the genetic models (Table 2).
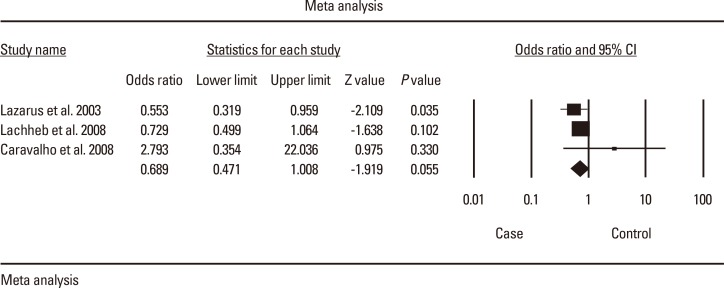
Association of TLR9 -1237 T/C with asthma risk
Analyses showed that the TLR9 -1237 T/C polymorphism was not associated with asthma under the recessive, homozygous and codominant models. In the allele contrast model, the major T allele was marginally associated with asthma with OR=0.689 (95% CI, 0.471-1.007; P=0.055), suggesting that the major T allele might be a significant protective factor (Table 2 and Fig. 5).
Fig. 5. Forest plot of the association between TLR9 -1237 and asthma: T allele vs C allele. The forest plot shows the (ORs and respective 95% CIs for the studies included in the meta-analysis. For each study in the forest plot, the area of the black square is proportional to the study weight, and the horizontal bar represents the 95% CI. Z score: the standardized expression of a value in terms of its relative position in the full distribution of values.
The estimated OR1 (TT vs CC), OR2 (TC vs CC) and OR3 (TT vs TC) were 0.408, 0.01, and 0.498, respectively. These estimates likely suggested a codominant genetic model. Only three studies on TLR9 -1237 T/C were available; therefore, estimates were not sufficiently powerful. However, these estimates indicated that the TT genotype tended to be a significant protective factor (P=0.065). No evidence of publication bias was detected by Egger's test in all of the genetic models (Table 2).
DISCUSSION
During the last decade, the function of TLRs in asthma pathogenesis has been investigated largely by comparing the incidence of disease among persons with different polymorphisms. The magnitude of the association of polymorphisms with asthma varies depending on genetics, demographics, environmental factors, and study methodologies. Many association studies have reported that TLR polymorphisms predispose to asthma.26,47,49,52,56,59,61,68 However, some polymorphisms might not be associated with asthma susceptibility, but rather with asthma severity, such as TLR4 polymorphisms.48,51,58 Conflicting results were also reported, demonstrating a protective effect of some polymorphisms.12,45,46 However, other studies reported no association between TLR polymorphisms and asthma risk.44,50,53,60,61,64,69,70 Given the conflicting results yielded by genetic association studies, a systematic review and meta-analysis is of great value. The current meta-analysis provides a comprehensive examination of the available evidence concerning the association of SNPs in TLR genes with asthma and refines their risk profiles. This analysis represents the first meta-analysis concerning the impact of some TLR polymorphisms on asthma and assesses their role as modifiers of asthma risk.
Estimates of combined effect sizes revealed that the major TLR9 -1237 T allele was significantly associated with a decreased asthma risk. Additionally, for TLR2 Arg753Gln G>A, sensitivity analysis in the allele contrast model revealed that the major G allele was significantly associated with a decreased asthma risk. For TLR4 Asp299Gly A>G, the AA homozygote genotype and A allele tended to be associated with a decreased asthma risk. These results implicate that the major allele in TLR polymorphisms might be generally associated with a protective effect. However, TLR4 Thr399Ile showed no significant association with asthma risk. In a previous meta-analysis, Chen71 reported no direct association between TLR4 Asp299Gly and asthma. This result is consistent with our findings in the dominant, homozygous and codominant models. In a recent systematic review, Klassen et al.72 reported that TLR 2, TLR6, TLR9, and TLR10 appear to have some association with childhood asthma in Caucasians. However, no convincing evidence for a role of TLRs in relation to childhood asthma exists. Polymorphisms in TLR3 seemed not to be associated with asthma.57,65 Results for TLR6 are conflicting. One study with a small sample size showed that TLR6 Ser249Pro C>T contributed to asthma susceptibility,30 but a larger study on the same polymorphism reported no association in both children and adults.59 However, other studies reported that polymorphisms in TLR6 were significantly associated with asthma phenotypes.44,45,56,73 Similarly, some polymorphisms in TLR7/8 have been shown to be associated with asthma disease,29,33 whereas other polymorphisms showed no association.29 For TLR10, some polymorphisms showed significant association with asthma23,33,45; however, other polymorphisms showed no significant association.27,45 Genetic association studies on TLR1 and TLR5 remain scarce or are lacking. Further investigations on TLR polymorphisms, including haplotype analysis along with gene-environment interaction, are needed.
SNPs, which occur at every 1.9 kb in the genome on average,73 could result in reduced or increased gene expression when they occur in promoter.74 This meta-analysis did not control for multiple known risk factors for asthma, such as age, gender, and ethnicity. These potential confounding factors may interact with TLR polymorphisms to moderate asthma susceptibility. Genetic associations were shown to be significantly influenced by age75,76,77,78 likely because some genes are expressed in adults and not expressed in children and vice versa. Observational studies showed that the prevalence of asthma has increased during the last decade due to environmental factors.3 Therefore, it is important to investigate other polymorphisms in TLRs, as well as gene-gene and gene-environment interactions. A possible gene-environment interaction has been reported,79 in which the SNPs act as modifiers of asthma risk in individuals with various degrees of environmental endotoxin exposure. Future studies should include haplotype analysis and stratification of the study population according to related environmental risk factors.
Asthma is a complex disease involving several genes that might be more relevant than TLR genes. Although statistically significant, the effect of the TLRs on asthma was modest. This result may reflect the important role of other confirmed candidate genes in asthma disease. It has been reported that many genes are involved and make small contributions to the overall asthma phenotype.
The findings of our meta-analyses are consistent with experimental studies demonstrating that TLR polymorphisms are important factors in asthma disease, and support the need for further research into the mechanisms underlying asthma susceptibility. The significant association between TLR polymorphisms and asthma risk may be of clinical and public health importance. Further meta-analyses and studies on the expression of related genes, environmental factors, and gene-gene and gene-environment interactions would provide useful information for the prevention and treatment of asthma.
The recent discovery of TLRs, with their role as initiators of the innate immune response and inflammation, suggests that modulating these receptors may be beneficial in the treatment of allergic disorders.7 TLRs are currently being exploited as possible targets for drug development.80 Recently, several patents aimed to modulate the innate immune reaction occurring in asthma through the use of novel synthetic TLR2 ligands8,11; these open new therapeutic perspectives for the prevention of these pathologies. Greater knowledge of risk factors will translate into improved diagnosis, prevention and therapeutic strategies for this chronic disease.
ACKNOWLEDGMENTS
This work was supported by a grant from the Ministry of Higher Education, Tunisia.
Footnotes
There are no financial or other issues that might lead to conflict of interest.
References
- 1.Corrigan CJ, Hartnell A, Kay AB. T lymphocyte activation in acute severe asthma. Lancet. 1988;1:1129–1132. doi: 10.1016/s0140-6736(88)91951-4. [DOI] [PubMed] [Google Scholar]
- 2.Devenny A, Wassall H, Ninan T, Omran M, Khan SD, Russell G. Respiratory symptoms and atopy in children in Aberdeen: questionnaire studies of a defined school population repeated over 35 years. BMJ. 2004;329:489–490. doi: 10.1136/bmj.38139.666447.F7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ho SM. Environmental epigenetics of asthma: an update. J Allergy Clin Immunol. 2010;126:453–465. doi: 10.1016/j.jaci.2010.07.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ober C, Yao TC. The genetics of asthma and allergic disease: a 21st century perspective. Immunol Rev. 2011;242:10–30. doi: 10.1111/j.1600-065X.2011.01029.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lee SH, Park JS, Park CS. The search for genetic variants and epigenetics related to asthma. Allergy Asthma Immunol Res. 2011;3:236–244. doi: 10.4168/aair.2011.3.4.236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sioud M. Induction of inflammatory cytokines and interferon responses by double-stranded and single-stranded siRNAs is sequence-dependent and requires endosomal localization. J Mol Biol. 2005;348:1079–1090. doi: 10.1016/j.jmb.2005.03.013. [DOI] [PubMed] [Google Scholar]
- 7.Phipps S, Lam CE, Foster PS, Matthaei KI. The contribution of toll-like receptors to the pathogenesis of asthma. Immunol Cell Biol. 2007;85:463–470. doi: 10.1038/sj.icb.7100104. [DOI] [PubMed] [Google Scholar]
- 8.Kanagaratham C, Camateros P, Flaczyk A, Radzioch D. Polymorphisms in toll-like receptor genes and their roles in allergic asthma and atopy. Recent Pat Inflamm Allergy Drug Discov. 2011;5:45–56. doi: 10.2174/187221311794474874. [DOI] [PubMed] [Google Scholar]
- 9.Takeda K, Akira S. Toll-like receptors in innate immunity. Int Immunol. 2005;17:1–14. doi: 10.1093/intimm/dxh186. [DOI] [PubMed] [Google Scholar]
- 10.Liang S, Hosur KB, Lu S, Nawar HF, Weber BR, Tapping RI, et al. Mapping of a microbial protein domain involved in binding and activation of the TLR2/TLR1 heterodimer. J Immunol. 2009;182:2978–2985. doi: 10.4049/jimmunol.0803737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fuchs B, Braun A. Modulation of asthma and allergy by addressing toll-like receptor 2. J Occup Med Toxicol. 2008;3(Suppl 1):S5. doi: 10.1186/1745-6673-3-S1-S5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Roponen M, Yerkovich ST, Hollams E, Sly PD, Holt PG, Upham JW. Toll-like receptor 7 function is reduced in adolescents with asthma. Eur Respir J. 2010;35:64–71. doi: 10.1183/09031936.00172008. [DOI] [PubMed] [Google Scholar]
- 13.Stowell NC, Seideman J, Raymond HA, Smalley KA, Lamb RJ, Egenolf DD, et al. Long-term activation of TLR3 by poly(I:C) induces inflammation and impairs lung function in mice. Respir Res. 2009;10:43. doi: 10.1186/1465-9921-10-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lun SW, Wong CK, Ko FW, Hui DS, Lam CW. Expression and functional analysis of toll-like receptors of peripheral blood cells in asthmatic patients: implication for immunopathological mechanism in asthma. J Clin Immunol. 2009;29:330–342. doi: 10.1007/s10875-008-9269-1. [DOI] [PubMed] [Google Scholar]
- 15.Mizel SB, Honko AN, Moors MA, Smith PS, West AP. Induction of macrophage nitric oxide production by Gram-negative flagellin involves signaling via heteromeric Toll-like receptor 5/Toll-like receptor 4 complexes. J Immunol. 2003;170:6217–6223. doi: 10.4049/jimmunol.170.12.6217. [DOI] [PubMed] [Google Scholar]
- 16.Chun E, Lee SH, Lee SY, Shim EJ, Cho SH, Min KU, et al. Toll-like receptor expression on peripheral blood mononuclear cells in asthmatics; implications for asthma management. J Clin Immunol. 2010;30:459–464. doi: 10.1007/s10875-009-9363-z. [DOI] [PubMed] [Google Scholar]
- 17.Chuang TH, Ulevitch RJ. Cloning and characterization of a sub-family of human toll-like receptors: hTLR7, hTLR8 and hTLR9. Eur Cytokine Netw. 2000;11:372–378. [PubMed] [Google Scholar]
- 18.Diebold SS, Kaisho T, Hemmi H, Akira S, Reis e Sousa C. Innate antiviral responses by means of TLR7-mediated recognition of single-stranded RNA. Science. 2004;303:1529–1531. doi: 10.1126/science.1093616. [DOI] [PubMed] [Google Scholar]
- 19.Lazarus R, Raby BA, Lange C, Silverman EK, Kwiatkowski DJ, Vercelli D, et al. Toll-like receptor 10 genetic variation is associated with asthma in two independent samples. Am J Respir Crit Care Med. 2004;170:594–600. doi: 10.1164/rccm.200404-491OC. [DOI] [PubMed] [Google Scholar]
- 20.Nakashima K, Hirota T, Suzuki Y, Akahoshi M, Shimizu M, Jodo A, et al. Association of the RIP2 gene with childhood atopic asthma. Allergol Int. 2006;55:77–83. doi: 10.2332/allergolint.55.77. [DOI] [PubMed] [Google Scholar]
- 21.Nakashima K, Hirota T, Obara K, Shimizu M, Jodo A, Kameda M, et al. An association study of asthma and related phenotypes with polymorphisms in negative regulator molecules of the TLR signaling pathway. J Hum Genet. 2006;51:284–291. doi: 10.1007/s10038-005-0358-1. [DOI] [PubMed] [Google Scholar]
- 22.Lee SW, Wang JY, Hsieh YC, Wu YJ, Ting HW, Wu LS. Association of single nucleotide polymorphisms of MD-1 gene with pediatric and adult asthma in the Taiwanese population. J Microbiol Immunol Infect. 2008;41:445–449. [PubMed] [Google Scholar]
- 23.Heinzmann A, Brugger M, Bierbaum S, Mailaparambil B, Kopp MV, Strauch K. Joint influences of Acidic-Mammalian-Chitinase with Interleukin-4 and Toll-like receptor-10 with Interleukin-13 in the genetics of asthma. Pediatr Allergy Immunol. 2010;21:e679–e686. doi: 10.1111/j.1399-3038.2010.01053.x. [DOI] [PubMed] [Google Scholar]
- 24.Sordillo JE, Sharma S, Poon A, Lasky-Su J, Belanger K, Milton DK, et al. Effects of endotoxin exposure on childhood asthma risk are modified by a genetic polymorphism in ACAA1. BMC Med Genet. 2011;12:158. doi: 10.1186/1471-2350-12-158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Smit LA, Bouzigon E, Bousquet J, Le Moual N, Nadif R, Pin I, et al. Mold allergen sensitization in adult asthma according to integrin β3 polymorphisms and Toll-like receptor 2/+596 genotype. J Allergy Clin Immunol. 2011;128:185–191.e7. doi: 10.1016/j.jaci.2011.04.007. [DOI] [PubMed] [Google Scholar]
- 26.Bjørnvold M, Munthe-Kaas MC, Egeland T, Joner G, Dahl-Jørgensen K, Njølstad PR, et al. A TLR2 polymorphism is associated with type 1 diabetes and allergic asthma. Genes Immun. 2009;10:181–187. doi: 10.1038/gene.2008.100. [DOI] [PubMed] [Google Scholar]
- 27.Qian FH, Zhang Q, Zhou LF, Jin GF, Bai JL, Yin KS. Polymorphisms in the toll-like receptor 2 subfamily and risk of asthma: a case-control analysis in a Chinese population. J Investig Allergol Clin Immunol. 2010;20:340–346. [PubMed] [Google Scholar]
- 28.Hussein YM, Awad HA, Shalaby SM, Ali AS, Alzahrani SS. Toll-like receptor 2 and Toll-like receptor 4 polymorphisms and susceptibility to asthma and allergic rhinitis: a case-control analysis. Cell Immunol. 2012;274:34–38. doi: 10.1016/j.cellimm.2012.02.006. [DOI] [PubMed] [Google Scholar]
- 29.Zhang Q, Qian FH, Zhou LF, Wei GZ, Jin GF, Bai JL, et al. Polymorphisms in toll-like receptor 4 gene are associated with asthma severity but not susceptibility in a Chinese Han population. J Investig Allergol Clin Immunol. 2011;21:370–377. [PubMed] [Google Scholar]
- 30.Tantisira K, Klimecki WT, Lazarus R, Palmer LJ, Raby BA, Kwiatkowski DJ, et al. Toll-like receptor 6 gene (TLR6): single-nucleotide polymorphism frequencies and preliminary association with the diagnosis of asthma. Genes Immun. 2004;5:343–346. doi: 10.1038/sj.gene.6364096. [DOI] [PubMed] [Google Scholar]
- 31.Zhang Q, Qian F, Zhou L, Wei G, Wang Y, Hu Z, et al. Polymorphisms of TLR7 and TLR8 associated with risk of asthma and asthma-related phenotypes in a southeastern Chinese Han population. J Nanjing Med Univ. 2009;23:25–32. [Google Scholar]
- 32.Lachheb J, Dhifallah IB, Chelbi H, Hamzaoui K, Hamzaoui A. Toll-like receptors and CD14 genes polymorphisms and susceptibility to asthma in Tunisian children. Tissue Antigens. 2008;71:417–425. doi: 10.1111/j.1399-0039.2008.01011.x. [DOI] [PubMed] [Google Scholar]
- 33.Lazarus R, Klimecki WT, Raby BA, Vercelli D, Palmer LJ, Kwiatkowski DJ, et al. Single-nucleotide polymorphisms in the Toll-like receptor 9 gene (TLR9): frequencies, pairwise linkage disequilibrium, and haplotypes in three U.S. ethnic groups and exploratory case-control disease association studies. Genomics. 2003;81:85–91. doi: 10.1016/s0888-7543(02)00022-8. [DOI] [PubMed] [Google Scholar]
- 34.Lazarus R, Vercelli D, Palmer LJ, Klimecki WJ, Silverman EK, Richter B, et al. Single nucleotide polymorphisms in innate immunity genes: abundant variation and potential role in complex human disease. Immunol Rev. 2002;190:9–25. doi: 10.1034/j.1600-065x.2002.19002.x. [DOI] [PubMed] [Google Scholar]
- 35.Leung TF, Tang NL, Wong GW, Fok TF. CD14 and toll-like receptors: potential contribution of genetic factors and mechanisms to inflammation and allergy. Curr Drug Targets Inflamm Allergy. 2005;4:169–175. doi: 10.2174/1568010053586336. [DOI] [PubMed] [Google Scholar]
- 36.Yang IA, Fong KM, Holgate ST, Holloway JW. The role of Toll-like receptors and related receptors of the innate immune system in asthma. Curr Opin Allergy Clin Immunol. 2006;6:23–28. doi: 10.1097/01.all.0000200503.77295.bb. [DOI] [PubMed] [Google Scholar]
- 37.Daley D, Park JE, He JQ, Yan J, Akhabir L, Stefanowicz D, et al. Associations and interactions of genetic polymorphisms in innate immunity genes with early viral infections and susceptibility to asthma and asthma-related phenotypes. J Allergy Clin Immunol. 2012;130:1284–1293. doi: 10.1016/j.jaci.2012.07.051. [DOI] [PubMed] [Google Scholar]
- 38.Miedema KG, Tissing WJ, Te Poele EM, Kamps WA, Alizadeh BZ, Kerkhof M, et al. Polymorphisms in the TLR6 gene associated with the inverse association between childhood acute lymphoblastic leukemia and atopic disease. Leukemia. 2012;26:1203–1210. doi: 10.1038/leu.2011.341. [DOI] [PubMed] [Google Scholar]
- 39.Moher D, Liberati A, Tetzlaff J, Altman DG PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. 2010;8:336–341. doi: 10.1016/j.ijsu.2010.02.007. [DOI] [PubMed] [Google Scholar]
- 40.Light RJ, Singer JD, Willett JB. The visual presentation and interpretation of meta-analyses. In: Cooper H, Hedges LV, editors. The handbook of research synthesis. New York (NY): Russell Sage Foundation; 1994. pp. 439–454. [Google Scholar]
- 41.Cochran WG. The combination of estimates from different experiments. Biometrics. 1954;10:101–129. [Google Scholar]
- 42.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Saçkesen C, Karaaslan C, Keskin O, Tokol N, Tahan F, Civelek E, et al. The effect of polymorphisms at the CD14 promoter and the TLR4 gene on asthma phenotypes in Turkish children with asthma. Allergy. 2005;60:1485–1492. doi: 10.1111/j.1398-9995.2005.00874.x. [DOI] [PubMed] [Google Scholar]
- 44.Puthothu B, Heinzmann A. Is toll-like receptor 6 or toll-like receptor 10 involved in asthma genetics--or both? Allergy. 2006;61:649–650. doi: 10.1111/j.1398-9995.2006.01098.x. [DOI] [PubMed] [Google Scholar]
- 45.Kormann MS, Depner M, Hartl D, Klopp N, Illig T, Adamski J, et al. Toll-like receptor heterodimer variants protect from childhood asthma. J Allergy Clin Immunol. 2008;122:86–92. 92.e1–92.e8. doi: 10.1016/j.jaci.2008.04.039. [DOI] [PubMed] [Google Scholar]
- 46.Smit LA, Siroux V, Bouzigon E, Oryszczyn MP, Lathrop M, Demenais F, et al. CD14 and toll-like receptor gene polymorphisms, country living, and asthma in adults. Am J Respir Crit Care Med. 2009;179:363–368. doi: 10.1164/rccm.200810-1533OC. [DOI] [PubMed] [Google Scholar]
- 47.Kerkhof M, Postma DS, Brunekreef B, Reijmerink NE, Wijga AH, de Jongste JC, et al. Toll-like receptor 2 and 4 genes influence susceptibility to adverse effects of traffic-related air pollution on childhood asthma. Thorax. 2010;65:690–697. doi: 10.1136/thx.2009.119636. [DOI] [PubMed] [Google Scholar]
- 48.Fagerås Böttcher M, Hmani-Aifa M, Lindström A, Jenmalm MC, Mai XM, Nilsson L, et al. A TLR4 polymorphism is associated with asthma and reduced lipopolysaccharide-induced interleukin-12(p70) responses in Swedish children. J Allergy Clin Immunol. 2004;114:561–567. doi: 10.1016/j.jaci.2004.04.050. [DOI] [PubMed] [Google Scholar]
- 49.Eder W, Klimecki W, Yu L, von Mutius E, Riedler J, Braun-Fahrländer C, et al. Toll-like receptor 2 as a major gene for asthma in children of European farmers. J Allergy Clin Immunol. 2004;113:482–488. doi: 10.1016/j.jaci.2003.12.374. [DOI] [PubMed] [Google Scholar]
- 50.Raby BA, Klimecki WT, Laprise C, Renaud Y, Faith J, Lemire M, et al. Polymorphisms in toll-like receptor 4 are not associated with asthma or atopy-related phenotypes. Am J Respir Crit Care Med. 2002;166:1449–1456. doi: 10.1164/rccm.200207-634OC. [DOI] [PubMed] [Google Scholar]
- 51.Werner M, Topp R, Wimmer K, Richter K, Bischof W, Wjst M, et al. TLR4 gene variants modify endotoxin effects on asthma. J Allergy Clin Immunol. 2003;112:323–330. doi: 10.1067/mai.2003.1648. [DOI] [PubMed] [Google Scholar]
- 52.Møller-Larsen S, Nyegaard M, Haagerup A, Vestbo J, Kruse TA, Børglum AD. Association analysis identifies TLR7 and TLR8 as novel risk genes in asthma and related disorders. Thorax. 2008;63:1064–1069. doi: 10.1136/thx.2007.094128. [DOI] [PubMed] [Google Scholar]
- 53.Lange NE, Zhou X, Lasky-Su J, Himes BE, Lazarus R, Soto-Quirós M, et al. Comprehensive genetic assessment of a functional TLR9 promoter polymorphism: no replicable association with asthma or asthma-related phenotypes. BMC Med Genet. 2011;12:26. doi: 10.1186/1471-2350-12-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Adjers K, Karjalainen J, Pessi T, Eklund C, Hurme M. Epistatic effect of TLR4 and IL4 genes on the risk of asthma in females. Int Arch Allergy Immunol. 2005;138:251–256. doi: 10.1159/000088726. [DOI] [PubMed] [Google Scholar]
- 55.He J, Bosse Y, Laprise C, Paré P, Sandford A, Kozyrskyj A, et al. Novel associations of genetic polymorphisms in the interleukin-1 receptor/Toll-like receptor signaling pathways with atopy and atopic asthma. J Allergy Clin Immunol. 2009;123:S167. [Google Scholar]
- 56.Koponen P, Vuononvirta J, Nuolivirta K, Helminen M, He Q, Korppi M. The association of genetic variants in toll-like receptor 2 subfamily with allergy and asthma after hospitalization for bronchiolitis in infancy. Pediatr Infect Dis J. 2014;33:463–466. doi: 10.1097/INF.0000000000000253. [DOI] [PubMed] [Google Scholar]
- 57.Noguchi E, Nishimura F, Fukai H, Kim J, Ichikawa K, Shibasaki M, et al. An association study of asthma and total serum immunoglobin E levels for Toll-like receptor polymorphisms in a Japanese population. Clin Exp Allergy. 2004;34:177–183. doi: 10.1111/j.1365-2222.2004.01839.x. [DOI] [PubMed] [Google Scholar]
- 58.Yang IA, Barton SJ, Rorke S, Cakebread JA, Keith TP, Clough JB, et al. Toll-like receptor 4 polymorphism and severity of atopy in asthmatics. Genes Immun. 2004;5:41–45. doi: 10.1038/sj.gene.6364037. [DOI] [PubMed] [Google Scholar]
- 59.Hoffjan S, Stemmler S, Parwez Q, Petrasch-Parwez E, Arinir U, Rohde G, et al. Evaluation of the toll-like receptor 6 Ser249Pro polymorphism in patients with asthma, atopic dermatitis and chronic obstructive pulmonary disease. BMC Med Genet. 2005;6:34. doi: 10.1186/1471-2350-6-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Smit LA, Bongers SI, Ruven HJ, Rijkers GT, Wouters IM, Heederik D, et al. Atopy and new-onset asthma in young Danish farmers and CD14, TLR2, and TLR4 genetic polymorphisms: a nested case-control study. Clin Exp Allergy. 2007;37:1602–1608. doi: 10.1111/j.1365-2222.2007.02831.x. [DOI] [PubMed] [Google Scholar]
- 61.Carvalho A, Pasqualotto AC, Pitzurra L, Romani L, Denning DW, Rodrigues F. Polymorphisms in toll-like receptor genes and susceptibility to pulmonary aspergillosis. J Infect Dis. 2008;197:618–621. doi: 10.1086/526500. [DOI] [PubMed] [Google Scholar]
- 62.Larocca N, DeSanctis J, Toro F, Moreno D. F.23. Polymorphisms of Toll-like receptor 2 and 4 genes in asthma and COPD. Clin Immunol. 2006;119(Suppl):S58–S59. [Google Scholar]
- 63.Hsieh YY, Wan L, Chang CC, Tsai CH, Tsai FJ. STAT2*C related genotypes and allele but not TLR4 and CD40 gene polymorphisms are associated with higher susceptibility for asthma. Int J Biol Sci. 2009;5:74–81. doi: 10.7150/ijbs.5.74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Qian XB, Wu Y, Cao SY, Cai XH, Yu CY, Xuan MY, et al. Association of single nucleotide polymorphisms in the promoter region of the TLR9 gene with childhood atopic asthma. Zhonghua Yi Xue Yi Chuan Xue Za Zhi. 2011;28:185–189. doi: 10.3760/cma.j.issn.1003-9406.2011.02.014. [DOI] [PubMed] [Google Scholar]
- 65.Palikhe NS, Kim SH, Kim JH, Losol P, Ye YM, Park HS. Role of toll-like receptor 3 variants in aspirin-exacerbated respiratory disease. Allergy Asthma Immunol Res. 2011;3:123–127. doi: 10.4168/aair.2011.3.2.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Voron'ko OE, Dmitrieva-Zdorova EV, Latysheva EA, Aksenova MG, Storozhakov GI, Bodoev NV, et al. CARD15 and TLR4 genes polymorphisms in atopic bronchial asthma. Mol Biol (Mosk) 2011;45:831–839. [PubMed] [Google Scholar]
- 67.Sahin F, Yıldız P, Kuskucu A, Kuskucu MA, Karaca N, Midilli K. The effect of CD14 and TLR4 gene polimorphisms on asthma phenotypes in adult Turkish asthma patients: a genetic study. BMC Pulm Med. 2014;14:20. doi: 10.1186/1471-2466-14-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Pacheco-Martínez MM, Saucedo-Ramírez O, Del Rio Navarro B, Del Rio-Chivardi J, Cruz M, Pérez-Figueroa GE, et al. Toll-like receptor 4 expression in obese asthmatic children with allergic inflammation. Bol Med Hosp Infant Mex. 2011;68:257–261. [Google Scholar]
- 69.Liang XH, Cheung W, Heng CK, Wang DY. Absence of the toll-like receptor 4 gene polymorphisms Asp299Gly and Thr399Ile in Singaporean Chinese. Ther Clin Risk Manag. 2005;1:243–246. [PMC free article] [PubMed] [Google Scholar]
- 70.Douville RN, Lissitsyn Y, Hirschfeld AF, Becker AB, Kozyrskyj AL, Liem J, et al. TLR4 Asp299Gly and Thr399Ile polymorphisms: no impact on human immune responsiveness to LPS or respiratory syncytial virus. PLoS One. 2010;5:e12087. doi: 10.1371/journal.pone.0012087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Chen S. Association between the TLR4 +896A>G (Asp299Gly) polymorphism and asthma: a systematic review and meta-analysis. J Asthma. 2012;49:999–1003. doi: 10.3109/02770903.2012.738270. [DOI] [PubMed] [Google Scholar]
- 72.Klaassen EM, Thönissen BE, van Eys G, Dompeling E, Jöbsis Q. A systematic review of CD14 and toll-like receptors in relation to asthma in Caucasian children. Allergy Asthma Clin Immunol. 2013;9:10. doi: 10.1186/1710-1492-9-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Marth G, Yeh R, Minton M, Donaldson R, Li Q, Duan S, et al. Single-nucleotide polymorphisms in the public domain: how useful are they? Nat Genet. 2001;27:371–372. doi: 10.1038/86864. [DOI] [PubMed] [Google Scholar]
- 74.Trajkov D, Mirkovska-Stojkovikj J, Arsov T, Petlichkovski A, Strezova A, Efinska-Mladenovska O, et al. Association of cytokine gene polymorphisms with bronchial asthma in Macedonians. Iran J Allergy Asthma Immunol. 2008;7:143–156. [PubMed] [Google Scholar]
- 75.Saadat M, Ansari-Lari M. Genetic polymorphism of glutathione S-transferase T1, M1 and asthma, a meta-analysis of the literature. Pak J Biol Sci. 2007;10:4183–4189. doi: 10.3923/pjbs.2007.4183.4189. [DOI] [PubMed] [Google Scholar]
- 76.Cui L, Jia J, Ma CF, Li SY, Wang YP, Guo XM, et al. IL-13 polymorphisms contribute to the risk of asthma: a meta-analysis. Clin Biochem. 2012;45:285–288. doi: 10.1016/j.clinbiochem.2011.12.012. [DOI] [PubMed] [Google Scholar]
- 77.Piacentini S, Polimanti R, Simonelli I, Donno S, Pasqualetti P, Manfellotto D, et al. Glutathione S-transferase polymorphisms, asthma susceptibility and confounding variables: a meta-analysis. Mol Biol Rep. 2013;40:3299–3313. doi: 10.1007/s11033-012-2405-2. [DOI] [PubMed] [Google Scholar]
- 78.Lee YH, Choi SJ, Ji JD, Song GG. The CTLA-4 +49 A/G and -318 C/T polymorphisms and susceptibility to asthma: a meta-analysis. Mol Biol Rep. 2012;39:8525–8532. doi: 10.1007/s11033-012-1707-8. [DOI] [PubMed] [Google Scholar]
- 79.von Mutius E. Gene-environment interactions in asthma. J Allergy Clin Immunol. 2009;123:3–11. doi: 10.1016/j.jaci.2008.10.046. [DOI] [PubMed] [Google Scholar]
- 80.Bezemer GF, Sagar S, van Bergenhenegouwen J, Georgiou NA, Garssen J, Kraneveld AD, et al. Dual role of toll-like receptors in asthma and chronic obstructive pulmonary disease. Pharmacol Rev. 2012;64:337–358. doi: 10.1124/pr.111.004622. [DOI] [PubMed] [Google Scholar]