Abstract
In cases where typical aspects are shown, the diagnosis of most frequent hepatic lesions can be made with some safety by means of several imaging methods; on the other hand, uncommon lesions generally represent a diagnostic challenge for the radiologist. In the present second part of the study, the authors describe four rare hepatic lesions, as follows: primary hepatic lymphoma, myofibroblastic tumor, primary hepatic neuroendocrine tumor and desmoplastic small round cell tumor, approaching their main characteristics and imaging findings with emphasis on computed tomography and magnetic resonance imaging.
Keywords: Neoplasms, Liver, Atypical, Computed tomography, Magnetic resonance imaging
Abstract
O diagnóstico das lesões hepáticas mais frequentes pode ser feito com alguma segurança quando exibem aspectos típicos, utilizandose os diversos métodos de imagem; ao contrário, as lesões incomuns são geralmente um desafio diagnóstico para o radiologista. Nesta segunda parte do estudo serão descritas quatro raras lesões hepáticas: o linfoma hepático primário, o tumor miofibroblástico, o carcinoma neuroendócrino primário do fígado e o tumor desmoplásico de pequenas células, abordando as suas principais características e achados de imagem, com foco na tomografia computadorizada e ressonância magnética.
INTRODUCTION
A wide variety of tumors affect the liver, and 90% of focal liver lesions are benign. Amongst benign liver lesions, hemangiomas and focal nodular hyperplasias (FNH) are the most common non-cystic lesions(1). Metastases are the most frequently found malignant neoplasms, hepatocellular carcinomas (HCC) being responsible for 80-85% of primary malignant tumors, followed by intrahepatic cholangiocarcinomas(2).
The diagnosis of typical liver lesions can be safely made with different imaging methods; by contrast, uncommon lesions generally represent a diagnostic challenge for radiologists.
Among tumors considered uncommon, one highlights epithelial tumors, such as cystadenomas and biliary cystadenocarcinomas, non epithelial tumors including angiomyolipomas, epithelioid hemangioendotheliomas and angiosarcomas, besides other tumors such as lymphomas, inflammatory pseudotumors (myofibroblastic tumors) and some sarcomas(3).
Few studies are available in the literature providing a comparative and comprehensive analysis of imaging findings of uncommon liver tumors.
The objective of the present study is, by means of a pictorial essay, to describe the main imaging findings of several uncommon benign and malignant liver tumors observed at computed tomography (CT) and magnetic resonance imaging (MRI). The following entities will be approached in this second part of the study: primary hepatic lymphoma; myofibroblastic tumor; primary hepatic neuroendocrine tumor; and desmoplastic small round cell.
PRIMARY HEPATIC LYMPHOMA
Primary hepatic lymphoma (PHL) is an extremely rare neoplasm, corresponding to less than 1% of extranodal lymphomas. It is defined as a primary liver tumor as there is no involvement of the spleen, lymph nodes or other distant sites at the moment of the diagnosis. There is a predilection for males (3 men:1 woman), usually at the fifth decade of life(4). At the moment of the diagnosis, the symptoms are nonspecific and the patients may present with abdominal discomfort and fever. There is a strong association with immunosuppression, hepatitis B and C, human immunodefficiency and Epstein-Barr viruses(5,6).
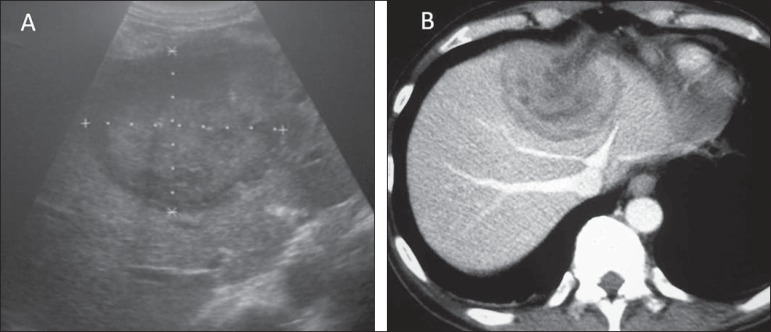
In about 60% of cases such tumors present as solitary, well defined masses (> 4 cm) which demonstrate peripheral lamellar enhancement after intravenous contrast media injection, and may rarely calcify, simulating hypovascular metastasis from the gastrointestinal tract, presenting with a target sign (Figures 1 and 2). Multinodular and infiltrative presentations are less frequently observed and are generally related to liver involvement by systemic lymphoma(5).
Figure 1.
Primary hepatic lymphoma. A: Ultrasonography demonstrating heterogeneous liver mass located in the confluence between the right and left lobes with target sign. B: Correlation with CT highlights peripheral, lamellar enhancement after intravenous contrast agent injection.
Figure 2.
MRI of a patient with primary hepatic lymphoma. Heterogeneous mass in the right liver lobe, with target sign and hyposignal on T1-weighted (A) and moderate to hypersignal on T2-weighted sequences (B).
Some findings suggest the diagnosis of PHL:
Absence of involvement of other extranodal sites.
Solitary mass presenting with peripheral lamellar enhancement.
Target sign without a known primary tumor.
Immunosuppressed patient.
INFLAMMATORY TUMOR (MYOFIBROBLASTIC TUMOR)
It is a rare liver lesion characterized by chronic inflammation, with fibroblasts proliferation which may compromise different organs but is most frequently is found in lungs and liver(7). It is also known as xanthogranuloma, histiocytoma, pseudolymphoma or fibroxanthoma. Currently it is known as inflammatory myofibroblastic tumor (IMT)(8).
This tumor is most frequently found in male young adults and in general presents a benign evolution. Its etiology still remains unknown and may be related to inflammatory-infectious processes (hepatitis and repetition cholangitis) and self-immune diseases(8).
Symptoms are nonspecific and include fever, abdominal pain, weight loss and jaundice. Generally, this tumor is a solitary mass and in 20% of cases develops as a multiple and synchronous mass, most frequently located in the right liver lobe, measuring 1-20 cm in its greater diameter(8). Laboratory analysis frequently demonstrates leukocytosis, eosinophilia and increased hemosedimentation velocity (HSV). Cases of patients presenting increased levels of tumor markers such as CA 19-9 have already been reported(7,9).
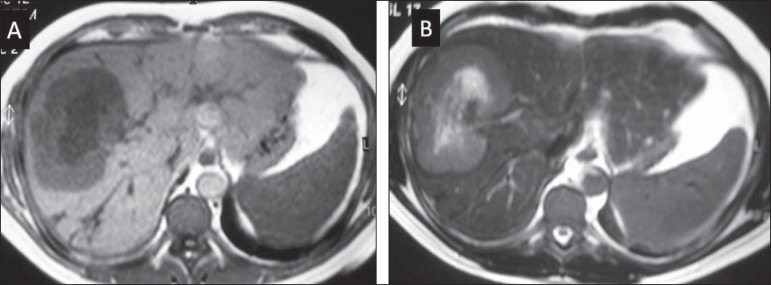
CT usually demonstrates a hypodense mass with peripheral, heterogeneous enhancement, with a poorly vascularized central area. Compressive effects of the mass may occur, determining dilatation of the biliary tract and portal hypertension (Figure 3). MRI is one of the best methods capable of better characterizing an inflammatory tumor. A focal, mass-type lesion is the most common appearance and presents with low signal intensity on T1-weighted images and slightly increased signal on T2-weighted images, sometimes with intermingled foci of marked hypersignal. After paramagnetic contrast media injection, intense and heterogeneous enhancement is observed, particularly in the periphery of the lesion(8).
Figure 3.
Inflammatory pseudotumor. A 66-year-old man with pain in the right hypochondrium associated with fever and leukocytosis. Non-contrast enhanced CT (A) and after intravenous contrast injection (B,C) demonstrates the presence of a hypodense and hypovascularized lesion in the segments II and IV, with permeative appearance, simulating infiltrating lesion. Follow-up CT three-month after antibiotic therapy demonstrates complete lesion regression (D).
Generally, histopathological correlation is required to establish a definitive diagnosis of inflammatory tumor that includes intrahepatic cholangiocarcinoma, liver abscess and HCC amongst its differential diagnoses(7).
Main findings suggestive of the diagnosis of IMT include:
Laboratory tests: leukocytosis and increased HSV.
Association with autoimmune diseases.
Solitary mass in the right liver lobe, with heterogeneous peripheral enhancement.
Resolution of the condition after either antibiotic therapy or corticotherapy.
PRIMARY HEPATIC NEUROENDOCRINE TUMOR
Primary hepatic neuroendocrine tumor (PHNT) represents less than 0.3% of all neuroendocrine tumors. It is most commonly found in women in seventh decade of life. Symptoms are nonspecific and include abdominal pain, palpable abdominal mass, fatigue and weight loss. More than 10% of cases are asymptomatic and only a small percentage of patients present with carcinoid syndrome (facial flush, abdominal pain and diarrhea)(10).
The diagnosis of primary hepatic carcinoid tumor is based on histological and immunohistochemical analysis and principally on exclusion of metastatic disease. Scintigraphy with somatostatin analog drug (OctreoScan) is a useful technique for the diagnosis of functional neuroendocrine tumors, with up to 90% sensitivity. On the other hand, PET/CT is an imaging modality reserved for the diagnosis of non functional tumors. Surgical resection is the treatment of choice and transcatheter arterial chemoembolization is an excellent palliative option in cases of recurrent lesions(11).
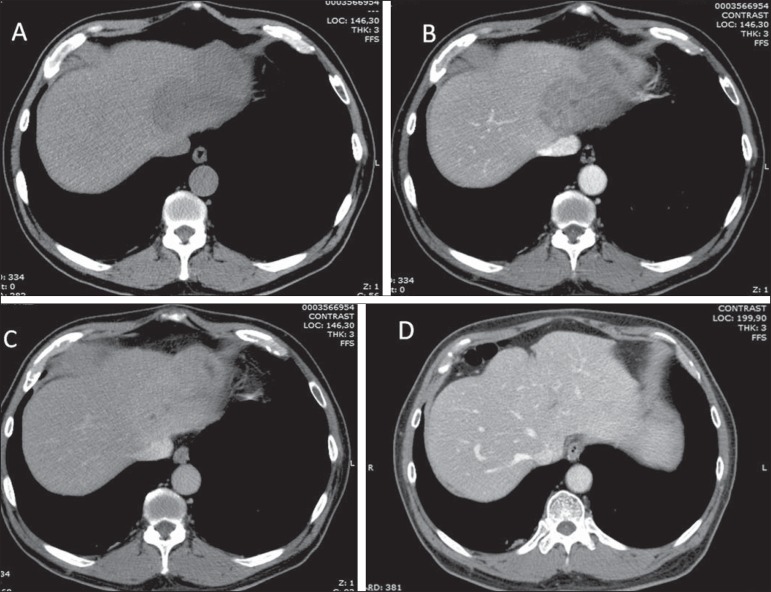
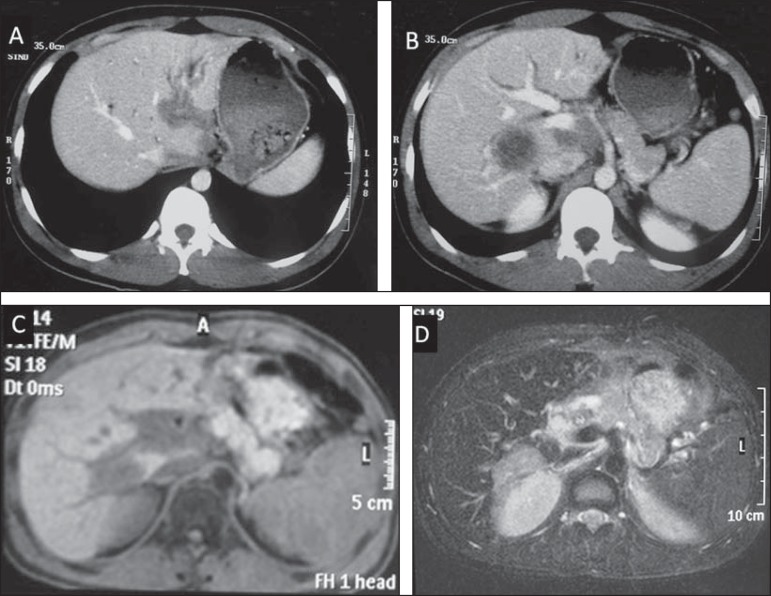
CT imaging findings include either single or multiple solid, hypervascularized lesions intermingled with areas of necrosis and calcifications (Figure 4). At MRI, the lesions present low signal intensity on T1-weighted and high signal intensity on T2-weighted sequences(10) (Figures 5 and 6).
Figure 4.
Primary hepatic neuroendocrine carcinoma. Computed tomography, non-contrast enhanced image (A) and after intravenous contrast media injection (B,C,D) demonstrate the presence of a heterogeneous, quite vascularized mass with some foci of calcification and intermingled cystic areas, occupying the left liver lobe.
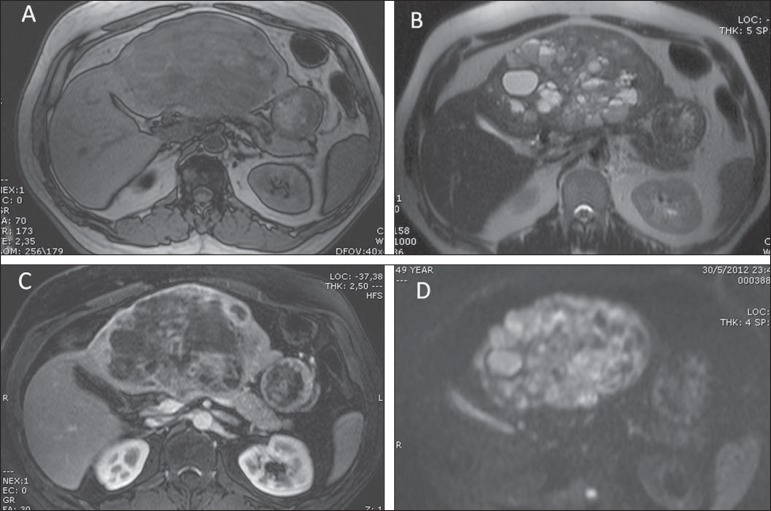
Figure 5.
Primary hepatic neuroendocrine carcinoma (same patient on Figure 4). MRI, T1--weighted (A), T2-weighted (B) and contrast-enhanced (C) sequences demonstrate heterogeneous mass with hyposignal on T1-weighted and hypersignal on T2-weighted images intermingled with multiple cystic areas (some of them with fluid-fluid level). The lesion presented restriction to water diffusion at the diffusion sequence (D).
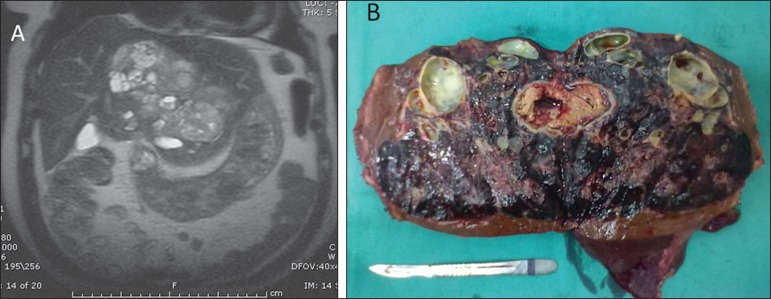
Figure 6.
Primary hepatic neuroendocrine carcinoma (same patient on Figures 4 and 5). MRI, coronal T2-weighted image (A) demonstrates heterogeneous mass occupying almost the whole left liver lobe, with hypersignal intermingled with multiple cystic areas, with excellent correspondence with the macroscopic aspect observed on the surgical specimen (B).
The differential diagnoses is broad, however, one should consider the possibility of hypervascular metastasis, HCC, cholangiocarcinoma with neuroendocrine differentiation and epithelioid variant of gastrointestinal stromal tumor(10).
Some findings may be useful to consider PHNT as a pertinent hypothesis among differential diagnoses:
Women between their sixth and seventh decades of life.
Presence of heterogeneous, hypervascular mass with no history of hepatopathy.
Eventual association with carcinoid syndrome.
DESMOPLASTIC SMALL ROUND CELL TUMOR
Desmoplastic small round cell tumor (DSCT) is a rare mesenchymal and highly aggressive tumor, with about 200 cases described in the literature. Its incidence is highest in adolescent and young adults (mean age, 22 years), preferentially in male individuals (4 men:1 woman)(12). The reported location is almost exclusively intra-abdominal, without a clearly identified visceral origin, affecting the omentum and peritoneal implants involving the diaphragm, splenic hilum, intestinal mesenterium and pelvic peritoneum(13).
Organs involvement is inconstant and secondary, and liver and lungs represent the main common sites for metastatic disease, besides the peritoneum(11).
Clinical manifestations of intra-abdominal DSCT are usually nonspecific and most frequently involve vague pelvic or abdominal symptoms and palpable masses(13).
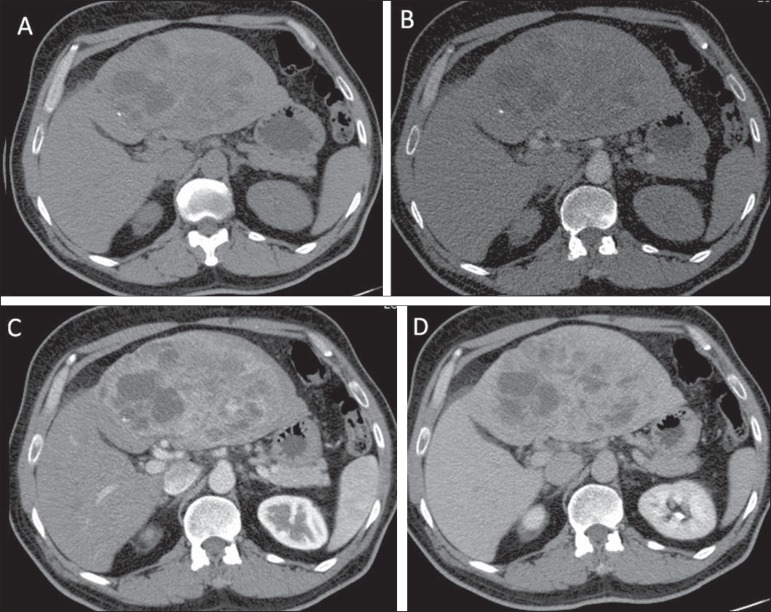
Imaging findings demonstrate intraperitoneal tumor mass without identifying the lesion site (organ) in association with multiple peritoneal implants and ascites. At CT and MRI, such tumors present as masses with soft tissue density, with central foci suggesting necrosis and hemorrhage, with moderate enhancement following intravenous contrast injection, and calcifications in 22% of cases(13)(Figure 7).
Figure 7.
Desmoplastic small round cell tumor. CT, portal phase (A,B) demonstrates hypodense, hypovascularized, expansile mass infiltrating the hepatic hilum in association with subtle segmental dilatation of left intrahepatic biliary tract. Also, an intraparenchymal component is observed. T1- and T2-weighted MRI images with fat suppression (D) demonstrates hyposignal from the lesion on T1- weighted and hypersignal on T2- weighted sequences extending toward the hepatic hilum.
DSCT may be considered in the presence of intraperitoneal masses with visceral extension, with no defined primary site occurring in young patients.
CONCLUSION
Despite their rarity, the tumors described in this second part of the study should be recognized and considered by radiologists as included in the differential diagnoses of liver lesions, assisting not only in the therapeutic planning and strategy, but also as a support in the definition of the anatomopathological diagnosis.
Footnotes
Study developed at Department of Imaging Diagnosis, Escola Paulista de Medicina da Universidade Federal de São Paulo (EPM-Unifesp), São Paulo, SP, Brazil.
REFERENCES
- 1.Tiferes DA, D'Ippolito G. Neoplasias hepáticas: caracterização por métodos de imagem. Radiol Bras. 2008;41:119–127. [Google Scholar]
- 2.Walther Z, Jain D. Molecular pathology of hepatic neoplasms: classification and clinical significance. Patholog Res Int. 2011;2011:403929. doi: 10.4061/2011/403929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hamilton SR, Aaltonen LA. World Health Organization Classification of Tumours. Pathology and genetics of tumours of the digestive system. Lyon, France: IARC Press; 2000. [Google Scholar]
- 4.Masood A, Kairouz S, Hudhud KH, et al. Primary non-Hodgkin lymphoma of the liver. Curr Oncol. 2009;16:74–77. doi: 10.3747/co.v16i4.443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Coenegrachts K, Vanbeckevoort D, Deraedt K, et al. MRI findings in primary non-Hodgkin's lymphoma of the liver. JBR-BTR. 2005;88:17–19. [PubMed] [Google Scholar]
- 6.Tan Y, Xiao EH. Rare hepatic malignant tumors: dynamic CT, MRI, and clinicopathologic features: with analysis of 54 cases and review of the literature. Abdom Imaging. 2013;38:511–526. doi: 10.1007/s00261-012-9918-y. [DOI] [PubMed] [Google Scholar]
- 7.Liu PS, Hussain HK. Uncommon hepatic tumors. In: Hussain HK, Francis IR, editors. Primary carcinomas of the liver. Series: Contemporary issues in cancer imaging. Cambridge: Cambridge University Press; 2010. pp. 214–229. [Google Scholar]
- 8.Venkataraman S, Semelka RC, Braga L, et al. Inflammatory myofibroblastic tumor of the hepatobiliary system: report of MR imaging appearance in four patients. Radiology. 2003;227:758–763. doi: 10.1148/radiol.2273020572. [DOI] [PubMed] [Google Scholar]
- 9.Fukuya T, Honda H, Matsumata T, et al. Diagnosis of inflammatory pseudotumor of the liver: value of CT. AJR Am J Roentgenol. 1994;163:1087–1091. doi: 10.2214/ajr.163.5.7976880. [DOI] [PubMed] [Google Scholar]
- 10.Gao J, Hu Z, Wu J, et al. Primary hepatic carcinoid tumor. World J Surg Oncol. 2011;9:151–151. doi: 10.1186/1477-7819-9-151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Park CH, Chung JW, Jang SJ, et al. Clinical features and outcomes of primary hepatic neuroendocrine carcinomas. J Gastroenterol Hepatol. 2012;27:1306–1311. doi: 10.1111/j.1440-1746.2012.07117.x. [DOI] [PubMed] [Google Scholar]
- 12.Dufresne A, Cassier P, Couraud L, et al. Desmoplastic small round cell tumor: current management and recent findings. Sarcoma. 2012;2012:714986–714986. doi: 10.1155/2012/714986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pickhardt PJ, Fisher AJ, Balfe DM, et al. Desmoplastic small round cell tumor of the abdomen: radiologic-histopathologic correlation. Radiology. 1999;210:633–638. doi: 10.1148/radiology.210.3.r99mr42633. [DOI] [PubMed] [Google Scholar]