Abstract
The value of measuring ANCA during follow-up to predict a relapse is controversial. On the basis of recently obtained pathophysiologic insights, we postulated that measuring ANCA is useful in patients with renal involvement but is less valuable in patients with nonrenal disease. One hundred sixty-six consecutive patients with ANCA-associated vasculitis, positive for either proteinase 3 (PR3)-ANCA or myeloperoxidase (MPO)-ANCA, were included in our study, followed at regular intervals, and tested for PR3-ANCA and MPO-ANCA. In this cohort, 104 patients had renal involvement (72 with PR3-ANCA, 32 with MPO-ANCA) and 62 patients had nonrenal disease (36 with PR3-ANCA, 26 with MPO-ANCA). During an average (±SD) follow-up of 49±33 months and 18±14 ANCA measurements, 89 ANCA rises and 74 relapses were recorded. ANCA rises correlated with relapses in patients who presented with renal involvement (hazard ratio [HR], 11.09; 95% confidence interval [95% CI], 5.01 to 24.55), but in comparison, associated only weakly with relapses in patients who presented with nonrenal disease (HR, 2.79; 95% CI, 1.30 to 5.98). In conclusion, longitudinal ANCA measurements may be useful in patients with renal involvement but is less valuable in patients with nonrenal disease.
Keywords: ANCA, vasculitis, GN
ANCAs play an important role in the pathophysiology of ANCA-associated vasculitis (AAV).1 The value of measuring ANCA to predict disease activity, however, is controversial.2–5 A recent meta-analysis calculated a pooled positive likelihood ratio of 2.8 (95% confidence interval [95% CI], 1.7 to 4.9), concluding that serial ANCA measurements are of limited value.5 However, the interpretation of this meta-analysis is difficult because the published studies are very heterogeneous and prospective and retrospective studies are lumped together. On the basis of pathophysiologic insights,1 we hypothesize that serially measuring ANCA is useful in patients with renal involvement but is less valuable in patients with nonrenal disease. It was previously demonstrated that ANCAs induce GN but require more modification to induce granulomatous lesions in mouse models.6 Furthermore, ANCA is nearly always found in patients with renal involvement, whereas a subgroup of patients with nonrenal disease are clearly ANCA negative.3,7 Therefore, we investigated the relationship of an ANCA rise with a relapse in our cohort and divided our patients into those with and without renal involvement.
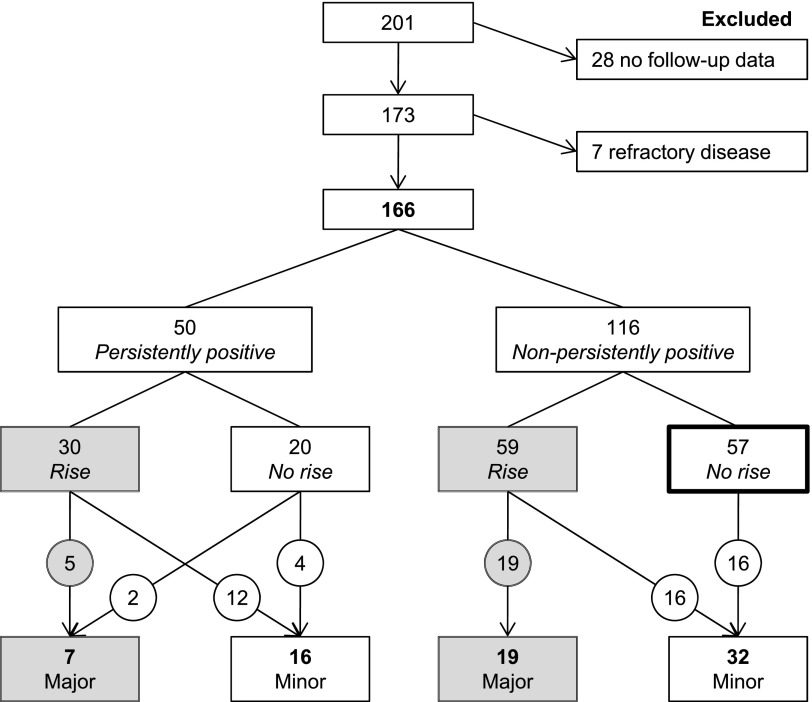
Between January 1, 2000, and November 1, 2011, 201 patients visited our university hospital with a diagnosis of AAV8 and were positive for either myeloperoxidase (MPO)-ANCA or proteinase 3 (PR3)-ANCA.9 Twenty-eight patients were excluded because we could not obtain follow-up data. Seven patients were refractory to treatment and did not reach stable clinical remission; these patients were also excluded. Of the remaining 166 patients, 74 patients (44.6%) did not experience a relapse during an average (±SD) follow-up of 7.5±5.9 years. All other patients had one or more relapses. There were 1, 2, 3, 4, or 5 relapses in 42 (25.3%), 31 (18.7%), 7 (4.2%), 4 (2.4%), and 8 (4.8%) patients, respectively. The relapse frequency was on average 0.17±0.21 per year for patients with PR3-ANCA and 0.11±0.18 for patients with MPO-ANCA (P=0.06).
To study the association of an ANCA rise with a relapse, the 166 patients were included when they entered their first remission after visiting our hospital. This study included 126 patients (75.9%) during remission after diagnosis and 40 patients during remission after a relapse. Table 1 presents baseline patient characteristics. During an average follow-up of 49±33 months and an average of 18±14 ANCA measurements, 74 patients relapsed (26 major relapses and 48 minor relapses). Eighteen patients included after a relapse and 74 patients included after diagnosis remained in remission. Seven patients died after a median follow-up of 3.3 years (interquartile range [IQR], 1.2–5.3), and causes of death were unknown (n=4), cardiovascular (n=2), malignancy (n=2), infection (n=1), or cerebral (n=1). Five patients were lost to follow-up after a median follow-up of 3.3 years (IQR, 1.8–4.1). During follow-up, 89 ANCA rises were identified. These rises were observed after an average of 20±17 months since the previous period of disease activity. After an ANCA rise, a relapse was diagnosed in 2 (2.2%), 26 (29.2%), 35 (39.3%), and 45 (50.6%) patients after <1, 6, 12, and 18 months since the rise, respectively. The median time elapsed between the ANCA rise and last follow-up visit in the patients that did not relapse was 41.5 months (IQR, 30.3–51.0).
Table 1.
Patient characteristics
| Characteristic | Total (n=166) | Renal (n=104) | Nonrenal (n=62) |
|---|---|---|---|
| At time of previous disease activity | |||
| Age (yr) | 56.7±14.5 | 56.2±14.8 | 57.5±13.9 |
| Men/women | 99/67 | 71/33 | 28/34 |
| PR3/MPO | 108/58 | 72/32 | 36/26 |
| GPA/MPA/EGPA | 126/23/17 | 83/19/2 | 43/4/15 |
| Birmingham Vasculitis Activity Score | 14 (8–20) | 18 (14–21) | 8 (6–11) |
| C-reactive protein | 60.5 (15–144) | 60 (17–144) | 64 (12–135) |
| Serum creatinine | 108 (85–195) | 148 (100–334) | 87 (77–95) |
| Organ involvement | |||
| Arthralgia | 76 | 49 | 27 |
| Cutaneous | 41 | 31 | 10 |
| Eyes | 30 | 20 | 10 |
| Ear, nose, throat | 122 | 75 | 47 |
| Lung | 124 | 74 | 50 |
| Cardiovascular | 12 | 9 | 3 |
| Renal | 104 | 104 | 0 |
| Dialysis | 15 | 15 | 0 |
| Abdominal | 11 | 10 | 1 |
| Central nervous system | 5 | 2 | 3 |
| Peripheral nervous system | 28 | 16 | 12 |
| Induction treatment resulting in remission | |||
| Cyclophosphamide+glucocorticoids | 111 | 77 | 34 |
| Rituximab+glucocorticoids | 7 | 7 | 0 |
| Methotrexate+glucocorticoids | 13 | 6 | 7 |
| Mofetil mycophenolate+glucocorticoids | 10 | 8 | 2 |
| Azathioprine+glucocorticoids | 4 | 0 | 4 |
| GC monotherapy | 16 | 3 | 13 |
| Other | 5 | 3 | 2 |
| Plasmapheresis | 30 | 29 | 1 |
| During follow-up | |||
| Time (mo) | 48.6±33.0 | 48.1±34.4 | 49.6±13.7 |
| Measurements | 17.9±14.0 | 19.0±14.7 | 16.1±12.7 |
| Nonpersistently ANCA positive | 116 | 73 | 43 |
| ANCA rise | 89 | 60 | 29 |
| Major relapse | 26 | 21 | 5 |
| Minor relapse | 48 | 23 | 25 |
Data are expressed as the mean±SD, median (IQR), or n. GPA, granulomatosis with polyangiitis; MPA, microscopic polyangiitis; EGPA, eosinophilic granulomatosis with polyangiitis.
At the time of relapse, all 26 patients with a major relapse were ANCA positive. In 24 patients (92%), the relapse was preceded by an ANCA rise. By contrast, only 32 of 48 patients (67%) with a minor relapse were ANCA positive at the time of relapse. In addition, the relapse was preceded by an ANCA rise in only 28 patients (58%). In patients who became ANCA negative during follow-up, all major relapses were preceded by an ANCA rise (Figure 1).
Figure 1.
Flowchart of the included patients. As shown, patients who become ANCA negative during follow-up do not experience a major relapse if an ANCA rise has not occurred.
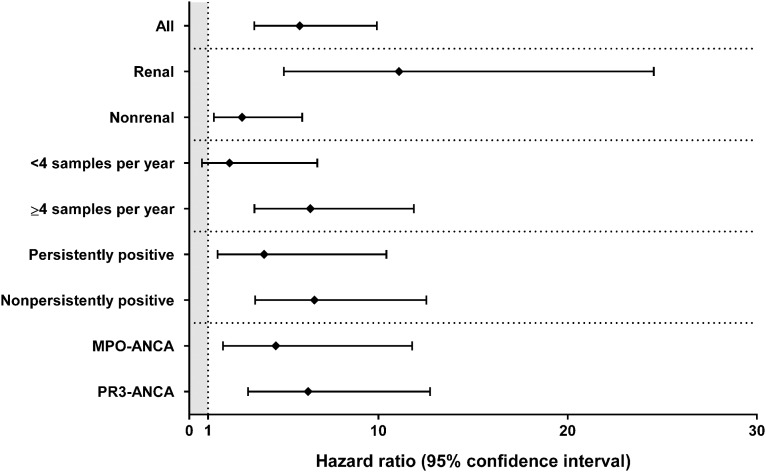
In the entire cohort, an ANCA rise is significantly associated with a relapse (hazard ratio [HR], 5.84; 95% CI, 3.44 to 9.92; P<0.001). A rise is strongly related to a relapse in patients with renal involvement (HR, 11.09; 95% CI, 5.01 to 24.55; P<0.001), whereas an ANCA rise is only weakly associated with a relapse in patients with nonrenal disease (HR, 2.79; 95% CI, 1.30 to 5.98; P=0.01). In addition, a rise is strongly associated with a relapse in patients with nonrenal severe10 disease (four relapses in 16 patients; HR, 13.08; 95% CI, 1.03 to 166.7; P=0.04), but not in patients with nonrenal limited10 disease (26 relapses in 46 patients; HR, 2.09; 95% CI, 0.92 to 4.78; P=0.08). Sampling interval (categorized as ≥4 measurements per year or fewer) and ANCA pattern (categorized as persistently ANCA positive or not) were additional factors that influenced the relationship of an ANCA rise with a relapse (Figure 2, Supplemental Material).
Figure 2.
The predictive value of an ANCA rise as determined by the antigen-specific solid-phase ANCA method in the entire cohort and subgroups of patients with AAV. A differentiation is made in renal involvement, sampling interval (<4 versus ≥4 per year), ANCA pattern (persistently positive or nonpersistently positive), and ANCA serotype (MPO-ANCA versus PR3-ANCA). HRs are shown with 95% CIs. The area up to a HR of 1 marks the border of significance.
How can our results be translated to daily practice? First, in patients who became ANCA negative during follow-up, the risk of developing a major relapse was extremely low as long as no rise in ANCA level occurred. Second, an ANCA rise in a patient with previous renal involvement should warn the clinician of a relapse because the probability of a relapse occurring after the rise is >11 times higher compared with the period before the rise. Third, measuring serial ANCA levels in patients without renal involvement, especially when severe vasculitic manifestations are lacking, is of limited value.11 However, an ANCA rise should not be used to preemptively treat the patient,12,13 because only less than one-half of the patients with an ANCA rise will experience a relapse within a year. Serial ANCA measurement is an important factor, but is not the only factor that should be considered during follow-up in patients with AAV.14,15
In 2006, a meta-analysis on the value of ANCA measurements to predict relapses concluded that no firm conclusions could be drawn because of considerable methodologic heterogeneity in the different studies.4 By contrast, another meta-analysis based on a more selected subgroup of these studies concluded that serial ANCA measurements have limited use.5 We found that the proportion of patients with renal involvement dictates the conclusion regarding whether ANCA measurements are of value during follow-up. Furthermore, we found that the association of an ANCA rise with a relapse was influenced by the ANCA method (Supplemental Material), sampling interval, and persistence of ANCA. Interestingly, we did not find a difference between MPO-ANCA and PR3-ANCA as previously suggested.5,14,16,17 We analyzed the articles that were in the latest meta-analysis and specified the study-level variables that may have influenced the results (Table 2).5 Studies with a high prevalence of renal or “severe” disease10 tended to have higher likelihood ratios, although variation in other study-level variables such as the ANCA method used or the definition of an ANCA rise may obscure this association. This suggests that spectrum bias is involved.18
Table 2.
An analysis of all the articles included in the Tomasson et al.5 meta-analysis in which all study-level variables that may influence the clinical usefulness of longitudinal ANCA measurements are presented
| Article | Cohort (N) | Severe (%) | Relapse (n) | Major (%) | Design | Method | Interval (mo) | Increase (%) | Slope (%/d) | LR+ |
|---|---|---|---|---|---|---|---|---|---|---|
| Finkielman34 | 101 | 71a | 46 | 19a | Prospective | Capture ELISA | 2–6 | 200 | 1.10 | 0.84 |
| Kerr35 | 72 | 59a | 45 | NR | Retrospective | IIF | 1–3 | 400 | 4.39 | 0.93 |
| Han13 | 48 | NR | 16 | NR | Retrospective | ELISA | 2.3 | 400 | 5.71 | 2.25 |
| Jayne36 | 60 | 65a | 23 | 43a | Retrospective | ELISA | 1 | 130 | 4.28 | 2.32 |
| Pettersson37 | 20 | 100 | 6 | 100 | Retrospective | IIF | 2 | Appearance | NR | 3.67 |
| Boomsma19 | 100 | NR | 37 | 73 | Prospective | IIF | 1.7 | 400 | 7.14 | 4.64 |
| ELISA | 175b | 3.13 | ||||||||
| Damoiseaux22 | 46 | 100 | 23 | NR | Retrospective | Capture ELISA | 3 | 200b | 2.19 | 12.5 |
| Hn ELISA | 200b | 2.19 | 4.3 | |||||||
| Hr ELISA | 250b | 2.74 | 5.6 | |||||||
| Hn-Hr ELISA | 175b | 1.92 | 8.9 | |||||||
| Terrier16 | 38 | 68a | 11 | 45a | Retrospective | ELISA | NR | Appearance | NR | 12.6 |
| Cohen Tervaert2 | 35 | 100 | 17 | 47 | Prospective | IIF | 1 | 400 | 13.16 | 15.38 |
LR+, positive likelihood ratio; NR, not reported; IIF, indirect immunofluorescence; Hn, human native; Hr, human recombinant.
The exact proportion of the severity of the included cohort and/or relapses was not described in the article, but an indication could be derived (e.g., from organ involvement).
The cut-off value was determined using a receiver operating characteristic curve.
The presence of ANCA is not the only factor required for disease reactivation, because many rises are not followed by a relapse.2,15,19 This suggests that other qualities, such as epitope specificity and the sialylation ratio, may determine the pathogenicity of ANCA.3,20,21 Otherwise, the association may be stronger when newer-generation ANCA methods are used.3,9,22 Finally, a second hit may be required after the occurrence of an ANCA rise before the patient truly develops a relapse. The importance of a second hit was previously demonstrated in a mouse model of MPO-ANCA,23 but remains elusive in humans. Possible candidates are microorganisms,24 environmental factors,25,26 and/or other autoantibodies.27
Our study has several limitations. In daily practice,2,19 the time between ANCA measurements varies, as was found in our study. We resolved this issue by using the slope of a rise, thereby taking into account the time between measurements. In this study, physicians were not blinded to ANCA results,2,19 which could have had an effect on diagnosing relapses. This may have influenced the association between an ANCA rise and a relapse in the entire cohort, but could not explain the marked difference between patients with and without renal involvement. A minority of patients suffered from microscopic polyangiitis or eosinophilic granulomatosis with polyangiitis, making any conclusion on ANCA testing in these diseases less valid. Renal involvement may be a proxy for severe vasculitic disease because we found that an ANCA rise in patients with severe nonrenal disease was also associated with a relapse in this small subgroup of patients. Finally, 5 of 62 patients who were initially diagnosed with nonrenal disease developed a renal relapse, suggesting that we should probably focus on markers of the biologic behavior of the disease in patients that initially present with nonrenal disease in order to predict the value of serial ANCA measurements in this patient subgroup.28
In summary, we have demonstrated in the largest published cohort with longitudinal ANCA measurements that an ANCA rise is related to a relapse in patients with renal involvement, but less in patients with nonrenal disease.
Concise Methods
Renal involvement was determined by a renal biopsy showing pauci-immune necrotizing GN.29 However, the presence of hematuria in combination with red cell casts, dysmorphic erythrocytes (>10), and/or proteinuria sufficed (a renal biopsy was not performed in 12 patients with renal involvement).30 Disease activity was scored using the Birmingham Vasculitis Activity Score (version 3).31 Patients were treated according to the European League Against Rheumatism guidelines as previously described.29 Maintenance therapy was given for at least 18 months and tapered within 24 months according to protocol in newly diagnosed patients.32 Patients who previously relapsed and/or relapsed during our study while using maintenance therapy were offered long-term maintenance therapy. Remission was defined as the absence of disease activity attributable to active disease during maintenance immunosuppressive therapy of a prednisone dose ≤7.5 mg.33 A relapse was defined as the reoccurrence or new onset of disease attributable to active disease combined with an increase or addition of immunosuppressive treatment.12,19,32,33 Relapses were further subdivided into minor or major relapses, depending on whether the relapse was potentially organ- or life-threatening.33 For a renal relapse, the (re)occurrence of hematuria in combination with a rise in serum creatinine of 25% was required to be characterized as a major relapse.
Solid-phase ANCA tests were used to detect and quantify PR3-ANCA and MPO-ANCA (Supplemental Material).3,9 For quantitation of MPO-ANCA and PR3-ANCA, the samples were diluted 1:50 in PBS as instructed by the manufacturer. Results were calculated in arbitrary units by a standard curve. Patient samples with results above the highest standard were further tested in 2-fold dilutions as appropriate. For the detection of an ANCA rise, the ANCA value was compared with the value measured in the samples obtained in the 6 months before the current sample. We defined a rise using the slope of an increase, for which a receiver operating characteristic curve was calculated to determine the optimal cut-off value (Supplemental Material).19 The association between an ANCA rise and relapse was investigated using a Cox regression model with an ANCA rise included as a time-dependent, binary, nonreversible predictor.19,34
Disclosures
None.
Supplementary Material
Footnotes
Published online ahead of print. Publication date available at www.jasn.org.
See related editorial, “Accurate Relapse Prediction in ANCA-Associated Vasculitis–the Search for the Holy Grail,” on pages 505–507.
This article contains supplemental material online at http://jasn.asnjournals.org/lookup/suppl/doi:10.1681/ASN.2013111233/-/DCSupplemental.
References
- 1.Wilde B, van Paassen P, Witzke O, Tervaert JWC: New pathophysiological insights and treatment of ANCA-associated vasculitis. Kidney Int 79: 599–612, 2011 [DOI] [PubMed] [Google Scholar]
- 2.Tervaert JWC, van der Woude FJ, Fauci AS, Ambrus JL, Velosa J, Keane WF, Meijer S, van der Giessen M, The TH, van der Hem GK, Kallenberg GM: Association between active Wegener’s granulomatosis and anticytoplasmic antibodies. Arch Intern Med 149: 2461–2465, 1989 [DOI] [PubMed] [Google Scholar]
- 3.Tervaert JWC, Damoiseaux J: Antineutrophil cytoplasmic autoantibodies: How are they detected and what is their use for diagnosis, classification and follow-up? Clin Rev Allergy Immunol 43: 211–219, 2012 [DOI] [PubMed] [Google Scholar]
- 4.Birck R, Schmitt WH, Kaelsch IA, van der Woude FJ: Serial ANCA determinations for monitoring disease activity in patients with ANCA-associated vasculitis: Systematic review. Am J Kidney Dis 47: 15–23, 2006 [DOI] [PubMed] [Google Scholar]
- 5.Tomasson G, Grayson PC, Mahr AD, Lavalley M, Merkel PA: Value of ANCA measurements during remission to predict a relapse of ANCA-associated vasculitis—A meta-analysis. Rheumatology (Oxford) 51: 100–109, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jennette JC, Falk RJ: L1. Pathogenesis of ANCA-associated vasculitis: Observations, theories and speculations. Presse Med 42: 493–498, 2013 [DOI] [PubMed] [Google Scholar]
- 7.Nölle B, Specks U, Lüdemann J, Rohrbach MS, DeRemee RA, Gross WL: Anticytoplasmic autoantibodies: Their immunodiagnostic value in Wegener granulomatosis. Ann Intern Med 111: 28–40, 1989 [DOI] [PubMed] [Google Scholar]
- 8.Jennette JC, Falk RJ, Bacon PA, Basu N, Cid MC, Ferrario F, Flores-Suarez LF, Gross WL, Guillevin L, Hagen EC, Hoffman GS, Jayne DR, Kallenberg CG, Lamprecht P, Langford CA, Luqmani RA, Mahr AD, Matteson EL, Merkel PA, Ozen S, Pusey CD, Rasmussen N, Rees AJ, Scott DG, Specks U, Stone JH, Takahashi K, Watts RA: 2012 revised International Chapel Hill Consensus Conference Nomenclature of Vasculitides. Arthritis Rheum 65: 1–11, 2013 [DOI] [PubMed] [Google Scholar]
- 9.Damoiseaux JGMC, Slot MC, Vaessen M, Stegeman CA, Van Paassen P, Tervaert JWC: Evaluation of a new fluorescent-enzyme immuno-assay for diagnosis and follow-up of ANCA-associated vasculitis. J Clin Immunol 25: 202–208, 2005 [DOI] [PubMed] [Google Scholar]
- 10.Stone JH, Wegener’s Granulomatosis Etanercept Trial Research Group : Limited versus severe Wegener’s granulomatosis: Baseline data on patients in the Wegener’s granulomatosis etanercept trial. Arthritis Rheum 48: 2299–2309, 2003 [DOI] [PubMed] [Google Scholar]
- 11.Rasmussen N, Salmela A, Ekstrand A, de Groot K, Gregorini G, Cohen Tervaert JW, Gross WL, Wiik A, Jayne DR, European Vasculitis Study Group (EUVAS) : Changes in proteinase 3 anti-neutrophil cytoplasm autoantibody levels in early systemic granulomatosis with polyangiitis (Wegener’s) may reflect treatment rather than disease activity. Clin Exp Rheumatol 31[Suppl 75]: S38–S44, 2013 [PubMed] [Google Scholar]
- 12.Tervaert JW, Huitema MG, Hené RJ, Sluiter WJ, The TH, van der Hem GK, Kallenberg CG: Prevention of relapses in Wegener’s granulomatosis by treatment based on antineutrophil cytoplasmic antibody titre. Lancet 336: 709–711, 1990 [DOI] [PubMed] [Google Scholar]
- 13.Han WK, Choi HK, Roth RM, McCluskey RT, Niles JL: Serial ANCA titers: Useful tool for prevention of relapses in ANCA-associated vasculitis. Kidney Int 63: 1079–1085, 2003 [DOI] [PubMed] [Google Scholar]
- 14.Jayne D: L27. Antibodies versus phenotypes: A clinician’s view. Presse Med 42: 579–582, 2013 [DOI] [PubMed] [Google Scholar]
- 15.Thai LH, Charles P, Resche-Rigon M, Desseaux K, Guillevin L: Are anti-proteinase-3 ANCA a useful marker of granulomatosis with polyangiitis (Wegener’s) relapses? Results of a retrospective study on 126 patients. Autoimmun Rev 13: 313–318, 2014 [DOI] [PubMed] [Google Scholar]
- 16.Terrier B, Saadoun D, Sène D, Ghillani P, Amoura Z, Deray G, Fautrel B, Piette JC, Cacoub P: Antimyeloperoxidase antibodies are a useful marker of disease activity in antineutrophil cytoplasmic antibody-associated vasculitides. Ann Rheum Dis 68: 1564–1571, 2009 [DOI] [PubMed] [Google Scholar]
- 17.Holle JU: L43. Seropositive and negative ANCA-associated vasculitis, anti-MPO and PR3-vasculitis: Different outcomes? Presse Med 42: 616–619, 2013 [DOI] [PubMed] [Google Scholar]
- 18.Ransohoff DF, Feinstein AR: Problems of spectrum and bias in evaluating the efficacy of diagnostic tests. N Engl J Med 299: 926–930, 1978 [DOI] [PubMed] [Google Scholar]
- 19.Boomsma MM, Stegeman CA, van der Leij MJ, Oost W, Hermans J, Kallenberg CG, Limburg PC, Tervaert JW: Prediction of relapses in Wegener’s granulomatosis by measurement of antineutrophil cytoplasmic antibody levels: A prospective study. Arthritis Rheum 43: 2025–2033, 2000 [DOI] [PubMed] [Google Scholar]
- 20.Roth AJ, Ooi JD, Hess JJ, van Timmeren MM, Berg EA, Poulton CE, McGregor J, Burkart M, Hogan SL, Hu Y, Winnik W, Nachman PH, Stegeman CA, Niles J, Heeringa P, Kitching AR, Holdsworth S, Jennette JC, Preston GA, Falk RJ: Epitope specificity determines pathogenicity and detectability in ANCA-associated vasculitis. J Clin Invest 123: 1773–1783, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Espy C, Morelle W, Kavian N, Grange P, Goulvestre C, Viallon V, Chéreau C, Pagnoux C, Michalski JC, Guillevin L, Weill B, Batteux F, Guilpain P: Sialylation levels of anti-proteinase 3 antibodies are associated with the activity of granulomatosis with polyangiitis (Wegener’s). Arthritis Rheum 63: 2105–2115, 2011 [DOI] [PubMed] [Google Scholar]
- 22.Damoiseaux J, Dähnrich C, Rosemann A, Probst C, Komorowski L, Stegeman CA, Egerer K, Hiepe F, van Paassen P, Stöcker W, Schlumberger W, Tervaert JW: A novel enzyme-linked immunosorbent assay using a mixture of human native and recombinant proteinase-3 significantly improves the diagnostic potential for antineutrophil cytoplasmic antibody-associated vasculitis. Ann Rheum Dis 68: 228–233, 2009 [DOI] [PubMed] [Google Scholar]
- 23.Huugen D, Xiao H, van Esch A, Falk RJ, Peutz-Kootstra CJ, Buurman WA, Tervaert JW, Jennette JC, Heeringa P: Aggravation of anti-myeloperoxidase antibody-induced glomerulonephritis by bacterial lipopolysaccharide: Role of tumor necrosis factor-α. Am J Pathol 167: 47–58, 2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Popa ER, Stegeman CA, Kallenberg CG, Tervaert JW: Staphylococcus aureus and Wegener’s granulomatosis. Arthritis Res 4: 77–79, 2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gatenby PA, Lucas RM, Engelsen O, Ponsonby A-L, Clements M: Antineutrophil cytoplasmic antibody-associated vasculitides: Could geographic patterns be explained by ambient ultraviolet radiation? Arthritis Rheum 61: 1417–1424, 2009 [DOI] [PubMed] [Google Scholar]
- 26.de Lind van Wijngaarden RAF, van Rijn L, Hagen EC, Watts RA, Gregorini G, Tervaert JW, Mahr AD, Niles JL, de Heer E, Bruijn JA, Bajema IM: Hypotheses on the etiology of antineutrophil cytoplasmic autoantibody associated vasculitis: The cause is hidden, but the result is known. Clin J Am Soc Nephrol 3: 237–252, 2008 [DOI] [PubMed] [Google Scholar]
- 27.Kain R, Tadema H, McKinney EF, Benharkou A, Brandes R, Peschel A, Hubert V, Feenstra T, Sengölge G, Stegeman C, Heeringa P, Lyons PA, Smith KG, Kallenberg C, Rees AJ: High prevalence of autoantibodies to hLAMP-2 in anti-neutrophil cytoplasmic antibody-associated vasculitis. J Am Soc Nephrol 23: 556–566, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kemna MJ, Tervaert JW: Does one size fit all? J Rheumatol 40: 1781–1784, 2013 [DOI] [PubMed] [Google Scholar]
- 29.Hilhorst M, Wilde B, van Breda Vriesman P, van Paassen P, Cohen Tervaert JW, Limburg Renal Registry : Estimating renal survival using the ANCA-associated GN classification. J Am Soc Nephrol 24: 1371–1375, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Watts R, Lane S, Hanslik T, Hauser T, Hellmich B, Koldingsnes W, Mahr A, Segelmark M, Tervaert JWC, Scott D: Development and validation of a consensus methodology for the classification of the ANCA-associated vasculitides and polyarteritis nodosa for epidemiological studies. Ann Rheum Dis 66: 222–227, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mukhtyar C, Lee R, Brown D, Carruthers D, Dasgupta B, Dubey S, Flossmann O, Hall C, Hollywood J, Jayne D, Jones R, Lanyon P, Muir A, Scott D, Young L, Luqmani RA: Modification and validation of the Birmingham Vasculitis Activity Score (version 3). Ann Rheum Dis 68: 1827–1832, 2009 [DOI] [PubMed] [Google Scholar]
- 32.Slot MC, Tervaert JW, Boomsma MM, Stegeman CA: Positive classic antineutrophil cytoplasmic antibody (C-ANCA) titer at switch to azathioprine therapy associated with relapse in proteinase 3-related vasculitis. Arthritis Rheum 51: 269–273, 2004 [DOI] [PubMed] [Google Scholar]
- 33.Hellmich B, Flossmann O, Gross WL, Bacon P, Tervaert JWC, Guillevin L, Jayne D, Mahr A, Merkel PA, Raspe H, Scott DG, Witter J, Yazici H, Luqmani RA: EULAR recommendations for conducting clinical studies and/or clinical trials in systemic vasculitis: Focus on anti-neutrophil cytoplasm antibody-associated vasculitis. Ann Rheum Dis 66: 605–617, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Finkielman JD, Merkel PA, Schroeder D, Hoffman GS, Spiera R, St Clair EW, Davis JC, Jr, McCune WJ, Lears AK, Ytterberg SR, Hummel AM, Viss MA, Peikert T, Stone JH, Specks U, WGET Research Group : Antiproteinase 3 antineutrophil cytoplasmic antibodies and disease activity in Wegener granulomatosis. Ann Intern Med 147: 611–619, 2007 [DOI] [PubMed] [Google Scholar]
- 35.Kerr GS, Fleisher TA, Hallahan CW, Leavitt RY, Fauci AS, Hoffman GS: Limited prognostic value of changes in antineutrophil cytoplasmic antibody titer in patients with Wegener's granulomatosis. Arthritis Rheum 36: 365–371, 1993 [DOI] [PubMed] [Google Scholar]
- 36.Jayne DR, Gaskin G, Pusey CD, Lockwood CM: ANCA and predicting relapse in systemic vasculitis. QJM 88: 127–133, 1995 [PubMed] [Google Scholar]
- 37.Pettersson E, Heigl Z: Antineutrophil cytoplasmic antibody (cANCA and pANCA) titers in relation to disease activity in patients with necrotizing vasculitis: a longitudinal study. Clinical Nephrol 37: 219–228, 1992 [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.