Abstract
People who are more securely attached to close partners show health benefits, but the mechanisms underlying this link are not well specified. We focus on physiological pathways that are potential mediators of the connection between attachment in childhood and adulthood and health and disease outcomes. Growing evidence indicates that attachment insecurity (vs. security) is associated with distinctive physiological responses to stress, including responses involving the HPA, SAM and immune systems, but these responses vary with type of stressor (e.g., social/nonsocial) and contextual factors (e.g., partner’s attachment style). Taking this more nuanced perspective will be important for understanding the conditions under which attachment shapes health-related physiological processes as well as downstream health and disease consequences.
A wealth of evidence has established that individuals in high quality relationships and who are socially integrated have fewer health risks than individuals in low quality relationships or who have few social ties [1]. Attachment security, which provides a foundation for high quality relationships [2,3], also has been linked to a variety of health-related biological responses, behaviors and outcomes [4-6].
How might attachment in both childhood and adulthood shape later health outcomes? Physiological stress response systems offer likely pathways linking attachment to downstream health outcomes. Accordingly, we focus here on recent evidence examining links between attachment and primary stress response systems: the hypothalamic-pituitary-adrenal (HPA), sympathetic-adrenal medullary (SAM) and the immune systems [4,7].
Attachment Processes and Physiological Stress Responses
Attachment styles may shape physiological stress responses because they function as strategies for regulating distress [2,3]. Anxious attached individuals, who expect that partners will not be as available or as responsive as they desire, rely on hyperactivating strategies leading them to be vigilant in detecting potential threats, to persistently signal their distress, and to seek excessive reassurance/support. Avoidantly attached individuals, who expect that others will not be responsive, rely on deactivating strategies leading them to minimize distress and distance themselves from others. Securely attached individuals generally expect that partners will be responsive; they are typically able to regulate distress effectively and flexibly, and when needed, they will turn to partners for reassurance and support. Figure 1 illustrates a conceptual model, adapted from previous work [4], for considering how attachment orientations shape health-related physiological stress responses and health and disease outcomes. The model suggests that attachment styles promote strategies for regulating affect, the self, and behavior in close relationships. These strategies shape physiological stress response patterns, which in turn, may offer a pathway connecting attachment to downstream health and disease outcomes. Furthermore, each partner’s response occurs in the context of the relationship, and therefore both partners may influence each other’s responses and outcomes. In addition, features of the situational context (e.g., type of stressor or relationship) may moderate the link between attachment and physiological stress responses. We focus here on the link between two components of the model -- attachment style and physiological stress responses – and take into account the dyadic relationship context as well as other features of the situation.
Figure 1.
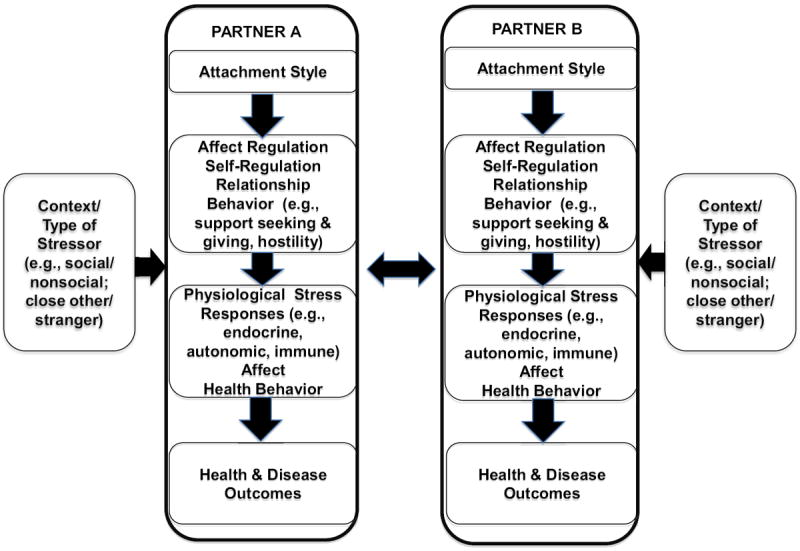
A conceptual model illustrating the links between attachment style and physiological stress responses as well as health and disease outcomes. Attachment styles promote particular strategies for regulating affect and the self as well as behavior patterns in close relationships. These regulatory processes and relationship behavior patterns, in turn, influence how individuals respond to stress at a physiological level (e.g., cortisol reactivity/recovery, cardiovascular reactivity, inflammation-related responses). Physiological stress responses (along with health behavior and affect) contribute to subsequent health outcomes over time, although these health behaviors and outcomes are not reviewed here. Importantly, the model is dyadic; attachment processes occur in the context of a relationship, and both partners may influence each other’s responses and outcomes reciprocally and/or interactively (e.g., Partner A’s attachment style in interaction with Partner B’s attachment style may produce distinctive physiological stress patterns for each partner). Also, other contextual factors (type of stressor, type of partner) can moderate associations between attachment and physiological stress responses.
Adapted from “Health and Attachment Processes” by P. R. Pietromonaco, C. C. DeVito, F. Ge, & J. Lembke, in press/2015. In J. A. Simpson & W. S. Rholes (Eds.) Attachment theory and research: New directions and emerging themes. NY: Guilford. Permission pending.
Attachment and HPA Regulation
The hypothalamic-pituitary-adrenal (HPA) axis is a major stress response system that controls the release of cortisol into the blood. Cortisol prepares the body for action and influences and interacts with multiple physiological systems (metabolic, immune, nervous). Cortisol responses may link attachment to later health and disease outcomes, given that dysregulated, atypical cortisol patterns have been associated with a variety of adverse physical and emotional health conditions [8].
Attachment in Childhood
A large body of indirect evidence has established that individuals who experienced early childhood interpersonal adversity or poor parenting (variables associated with attachment insecurity) evidence dysregulation in HPA axis responses [9-13], and a variety of health risks later in life, including metabolic syndrome, cardiovascular disease, and cancer [14,15]. Gunnar and colleagues were among the first to directly examine the relation of HPA functioning to assessments of attachment security in childhood [16], and this work was the catalyst for dozens of later studies, which clarified that insecure attachment in infants [17], school-age children [18] and adolescents [19] is associated with hyper- or hypo-responsiveness of the HPA system. Recent studies confirm the association of insecure attachment with both hyperactivated [20] and hypoactivated stress responses [21], and extend the earlier literature by clarifying the importance of the particular dyadic context of attachment (e.g. whether attachment is assessed with mother, father, or teacher) and the context of the type of stressor (e.g. whether HPA reactions are to stressors in close relationships or with strangers; see Figure 1). For example, toddlers who are insecurely attached to their child-care workers show greater HPA reactivity across the day; in contrast, toddlers’ attachment to their mothers predicts their HPA reactivity across the day only in high-quality child-care environments [20]. Adolescents who showed disorganized attachment as infants evidence different types of HPA dysregulation to different types of stressors: HPA hyper-responsiveness to a fear-inducing task with their mothers [22] and HPA hypo-responsiveness to a performance stressor (i.e., Trier Stress Test with strangers) [23]. In addition to underscoring the role of context for the relation of attachment to HPA functioning, newer research indicates that insecurely attached children underreport their psychological experience of distress (relative to their physiological reaction) [24]. If this discrepancy indicates a developing tendency to cope with stress through emotional suppression, then it may partly explain why insecure children experience greater health risks in later life [25, 26]. In fact, a recent groundbreaking study following individuals from infancy to age 32 found that infants classified as insecurely attached were more likely to experience an inflammation-related illness (e.g., heart disease, diabetes, stroke) as adults, even after other known risk factors (e.g., negative affect, BMI) were taken into account [26].
Attachment in Adulthood
In contrast to research on childhood attachment, research with adults has been able to examine whether HPA response patterns vary with attachment anxiety, avoidance, or both. Consistent with the expectation that anxiously attached individuals respond to stress with hyperactivation, most studies have found that anxiously attached individuals show elevated cortisol in response to a stressor and take longer to recover [27-29]. Similarly, anxiously attached married individuals produce higher daily cortisol [30]. In young dating couples, women’s attachment avoidance predicts cortisol patterns as well [27,31]; for example, more avoidant female dating partners evidenced elevated cortisol before and during a conflict discussion with their dating partner followed by a rapid drop in cortisol immediately after the discussion, perhaps providing physiological relief once they were able to disengage from the discussion [27].
Similar to findings for childhood attachment, the link between adult attachment and HPA responses depends on the situational context. Across a number of studies, attachment insecurity in adults has been associated with cortisol responses in situations involving attachment-related threats; however, the connection between attachment insecurity and cortisol responses is less clear in situations that do not involve an attachment-related threat (e.g., nonsocial contexts, tasks involving strangers) [7]. New findings point to the interplay between both relationship partners’ characteristics (e.g., their attachment styles) as a unique context that may influence cortisol responses. Specifically, more anxiously attached wives paired with more avoidantly attached husbands showed sharp increases in cortisol in anticipation of a conflict discussion followed by rapid declines, and their husbands showed corresponding patterns [32]. Furthermore, less constructive behavior during the conflict discussion accompanied these cortisol patterns among anxious wife/avoidant husband pairs: Anxiously attached wives had greater difficulty recognizing their avoidant husbands’ distress, and avoidantly attached husbands less effectively conveyed their needs to their anxious wives. The contribution of the dyadic context is further supported by recent work showing that one partner’s attachment style together with the other partner’s level of support predicts cortisol patterns. Among dating couples, anxiously attached women (but not anxiously attached men) faced with a stressful task (Trier Stress Test) benefited less from their partner’s positive support: their cortisol levels remained elevated longer compared to less anxiously attached women who also had received positive support from their partners [29]. Together, these findings suggest that connections between attachment and cortisol patterns depend on the interplay between characteristics of the individual and contextual factors such as their partner’s characteristics or behavior.
SAM Responses
Another physiological response system that may connect attachment to health is the sympathetic-adrenal-medullary (SAM) system. The SAM system triggers quick “fight-or-flight” responses through the sympathetic nervous system and the release of adrenaline from the adrenal medulla, and it initiates physiological responses (e.g., rapid increases in heart rate and breathing, pupil dilation, and nausea) to prepare the organism to respond quickly. SAM activity often is indexed through electrodermal responses, respiratory sinus arrhythmia (RSA), heart rate, or blood pressure. Similar to HPA axis responses, dysregulated SAM responses can alter immune function with potential long-term consequences for health [33,34].
Attachment in Childhood
As with research on the relation of childhood attachment to HPA functioning, indirect evidence of the relation of attachment to SAM functioning and later health outcomes shows that early family experiences (which are linked to children’s attachment styles) consistently predict SAM responses to stress [34-36]. More recent research that directly assesses childhood attachment focuses on identifying the interactive effects of the social and environmental context, child attachment, and SAM functioning. For example, mothers’ depressive symptoms interact with infant insecure attachment to predict infants’ dysregulated RSA [37], and infant RSA interacts with insecure attachment to predict increased problem behaviors [38]. As with recent research on child attachment and the HPA system, these studies underscore that fully understanding the relation of attachment to health outcomes will require models that take into account the complex interplay of attachment and physiological systems within varying socio-environmental contexts.
Attachment in Adulthood
Both attachment avoidance and anxiety have been associated with heightened SAM reactivity, although the patterns vary somewhat across studies. Individuals who were higher in avoidance (but not anxiety) in romantic relationships displayed greater electrodermal reactivity across stressful tasks [39]. Similarly, adults showing a deactivating pattern (reflecting attachment avoidance) with respect to their childhood caregiver also responded with greater electrodermal activity during a conflict discussion with their romantic partner; in addition, those showing a hyperactivating pattern (reflecting attachment anxiety) experienced an accelerated heart rate during the discussion [40]. Although a recent longitudinal study found that neither avoidance nor anxiety were associated concurrently with dating partners’ electrodermal activity during a relationship conflict, attachment anxiety at the earlier time point predicted greater electrodermal reactivity during a conflict discussion one year later [41]. One consistent finding across a number of studies is that when highly avoidant individuals show heightened autonomic nervous system activity, they are less likely to subjectively report greater distress, suggesting defensive or dissociated affect regulation among these individuals [3,42]. This finding echoes results mentioned earlier from the recent childhood literature showing insecure attachment associated with greater discrepancy between psychological and physiological reactions to stress.
Immune Responses
The immune system consists of a network of cells, tissues and organs that serve to protect the body from infection and disease. Although research examining attachment and immune responses is newly developing, sparse findings suggest that both childhood and adult attachment may impact immune functioning. This connection is especially important considering that the HPA and SAM axes modulate the immune system and vice versa [43].
Attachment in Childhood
Little work has directly examined childhood attachment and immune functioning, but research using related constructs (e.g., early childhood adversity) suggests that attachment insecurity is connected to dysregulated immune responses [44]. For example, children from lower income families have shown higher levels of C-reactive protein (indicating inflammation) [45] and higher levels of antibodies to a herpes virus (cytomegalovirus) [46].
Longitudinal research indicates that early life adversity may influence immune functioning years later [47,48]. For instance, adults who had experienced socioeconomic disadvantage or high levels of sexual or physical abuse at a young age showed elevated antibody titers to the Epstein-Barr virus, an indicator of cell-mediated immune functioning [48]. Attachment security may modulate the link between low SES and later immune functioning: Adults raised in a low SES family but who reported having mothers who were high in warmth were less likely to show detrimental inflammation responses than similar adults who reported that their mothers displayed low warmth [49]. Although additional work is needed that assesses the relation between attachment during early childhood (vs. retrospective reports of childhood experiences) and immune functioning, these findings suggest that secure attachment may protect individuals from the adverse effects associated with low SES early in life.
Attachment in Adults
Attachment insecurity has been associated with disruptions in immune functioning in adults. In one study, avoidantly attached husbands and wives showed heightened inflammatory (IL-6) responses to a marital conflict discussion [50]. In another study, more avoidantly attached women recovered more slowly from induced skin wounds over the course of discussions with their dating partner. In addition, more anxiously attached men showed slower wound recovery, but unexpectedly, more anxiously attached women showed faster recovery [51]. Other work further supports a link between anxious attachment and poorer immune function: Anxiously attached husbands and wives evidenced fewer T-cells over two days (together with higher cortisol levels) [30], and anxiously attached individuals showed elevated antibody titers to the Epstein-Barr virus on two tests one year apart [52]. Similarly, another recent study of adults (most males) found that individuals who were higher in attachment anxiety (but not those higher in avoidance) showed a greater increase in an inflammation marker (Il-6) after cardiac surgery [53]. (Attachment was unrelated to two other inflammation markers: TNF alpha and CRP.) Furthermore, poor sleep quality mediated the link between attachment anxiety and Il-6, possibly because anxious individuals’ hypervigilance interferes with their sleep quality and post-surgical healing. Nascent research suggests that attachment insecurity is related to poorer immune functioning, and goals for further work will be to discover which immune markers under which conditions (gender, type of stressor) are linked to avoidance or anxiety (or both).
Conclusion
Attachment insecurity (vs. security) in childhood and adulthood is associated with differential HPA, SAM and immune system responses. Recent work underscores that these connections depend on the context, including type of task and relationship and the interplay between partners’ characteristics. As researchers test more complex models involving physiological stress responses as mediators linking attachment to health, they also will need to take into account the complex interplay of attachment and physiological systems within different situational contexts.
Highlights.
Physiological stress responses may offer a pathway linking attachment and health.
Attachment insecurity predicts dysregulated HPA, SAM and immune responses.
These links have been demonstrated for both childhood and adult attachment.
These links vary importantly by context (e.g., type of stress or relationship).
Acknowledgments
Preparation of this article was supported by the National Cancer Institute at the National Institutes of Health, Grant R01 CA133908 to Paula R. Pietromonaco and Sally I. Powers.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
-
*
of special interest
-
**
of outstanding interest
- 1.Holt-Lunstad J, Smith TB, Layton JB. Social Relationships and Mortality Risk: A Meta-analytic Review. PLoS Med. 2010;7:1–20. doi: 10.1371/journal.pmed.1000316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mikulincer M, Shaver PR. Attachment in adulthood: Structure, dynamics, and change. Guilford Press; 2007. [Google Scholar]
- 3.Pietromonaco PR, Beck LA. Attachment processes in adult romantic relationships. In: Mikulincer M, Shaver PR, Simpson JA, Dovidio JF, editors. APA handbook of personality and social psychology, Interpersonal relations. Vol. 3. American Psychological Association; 2015. pp. 33–64. [Google Scholar]
- 4*.Pietromonaco PR, DeVito C, Ge F, Lembke J. Health and attachment processes. In: Simpson JA, Rholes WS, editors. Attachment theory and research: New directions and emerging themes. Guilford Press; in press. A comprehensive review of research examining attachment in childhood and adulthood and health-related physiological stress responses, health behavior, and health and disease outcomes. [Google Scholar]
- 5**.Pietromonaco PR, Uchino B, Dunkel Schetter C. Close relationship processes and health: Implications of attachment theory for health and disease. Health Psychol. 2013;32:499–513. doi: 10.1037/a0029349. This article examines the relevance of attachment theory for understanding a variety of health areas, including health behavior, pain, chronic disease, and aging, as well as implications for health-related interventions. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Maunder RG, Hunter JJ. Attachment relationships as determinants of physical health. J Am Acad Psychoanal Dyn Psychiatry. 2008;36:11–32. doi: 10.1521/jaap.2008.36.1.11. [DOI] [PubMed] [Google Scholar]
- 7*.Pietromonaco PR, DeBuse CJ, Powers SI. Does attachment get under the skin? Adult romantic attachment and cortisol responses to stress. Curr Dir Psychol Sci. 2013;22:63–68. doi: 10.1177/0963721412463229. An accessible review of many recent studies of attachment and HPA axis responses. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Miller GE, Chen E, Zhou ES. If It Goes Up, Must It Come Down? Chronic Stress and the Hypothalamic- Pituitary-Adrenocortical Axis in Humans. Psychol Bull. 2007;133:25–45. doi: 10.1037/0033-2909.133.1.25. [DOI] [PubMed] [Google Scholar]
- 9.Blair C, Raver CC. Child development in the context of adversity: Experiential canalization of brain and behavior. Am Psychol. 2012;67:309–318. doi: 10.1037/a0027493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Blair C, Raver CC, Granger D, Mills-Koonce R, Hibel L. Allostasis and allostatic load in the context of poverty in early childhood. Dev Psychopathol. 2011;23:845–857. doi: 10.1017/S0954579411000344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Blair C, Granger DA, Willoughby M, Mills-Koonce R, Cox M, Greenberg MT, Kivlighan KT, Fortunato CK. Salivary cortisol mediates effects of poverty and parenting on executive functions in early childhood. Child Dev. 2011;82:1970–1984. doi: 10.1111/j.1467-8624.2011.01643.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mills-Koonce WR, Garrett-Peters P, Barnett M, Granger DA, Blair C, Cox MJ. Father contributions to cortisol responses in infancy and toddlerhood. Dev Psychol. 2011;47:388–395. doi: 10.1037/a0021066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sturge-Apple ML, Davies PT, Cicchetti D, Manning LG. Interparental violence, maternal emotional unavailability and children’s cortisol functioning in family contexts. Dev Psychol. 2012;48:237–249. doi: 10.1037/a0025419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Miller GE, Chen E, Parker KJ. Psychological stress in childhood and susceptibility to the chronic diseases of aging: Moving toward a model of behavioral and biological mechanisms. Psychol Bull. 2011;137:959–997. doi: 10.1037/a0024768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Taylor SE, Way BM, Seeman TE. Early adversity and adult health outcomes. Dev Psychopathol. 2011;23:939–954. doi: 10.1017/S0954579411000411. [DOI] [PubMed] [Google Scholar]
- 16.Gunnar MR, Mangelsdorf S, Larson M, Hertsgaard L. Attachment, temperament, and adrenocortical activity in infancy: A study of psychoendocrine regulation. Dev Psychol. 1989;25:355–363. [Google Scholar]
- 17.Bernard K, Dozier M. Examining infants’ cortisol responses to laboratory tasks among children varying in attachment disorganization: Stress reactivity or return to baseline? Dev Psychol. 2010;46:1771–1778. doi: 10.1037/a0020660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Borelli JL, Crowley MJ, David DH, Sbarra DA, Anderson GM, Mayes LC. Attachment and emotion in school-aged children. Emotion. 2010;10:475–485. doi: 10.1037/a0018490. [DOI] [PubMed] [Google Scholar]
- 19.Oskis A, Loveday C, Hucklebridge F, Thorn L, Clow A. Anxious attachment style and salivary cortisol dysregulation in healthy female children and adolescents. J Child Psychol Psychiatry. 2011;52:111–118. doi: 10.1111/j.1469-7610.2010.02296.x. [DOI] [PubMed] [Google Scholar]
- 20*.Badanes LS, Dmitrieva J, Watamura SE. Understanding cortisol reactivity across the day at child care: The potential buffering role of secure attachments to caregivers. Early Child Res Q. 2012;27:156–165. doi: 10.1016/j.ecresq.2011.05.005. This study is notable because it investigated children’s cortisol patterns during day care in relation to their attachment to teachers and mothers. Secure attachment to teachers was related to declining cortisol over the day, but secure attachment to mothers was associated with declining cortisol only in high quality day care environments. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Roque L, Veríssimo M, Oliveira TF, Oliveira RF. Attachment security and HPA axis reactivity to positive and challenging emotional situations in child-mother dyads in naturalistic settings. Dev Psychobiol. 2012;54:401–411. doi: 10.1002/dev.20598. [DOI] [PubMed] [Google Scholar]
- 22.Spangler G, Zimmermann P. Emotional and adrenocortical regulation in early adolescence: Prediction by attachment security and disorganization in infancy. Int J Behav Dev. 2014;38:142–154. [Google Scholar]
- 23.Kelsay K, Leung DYM, Mrazek DA, Klinnert MD. Prospectively assessed early life experiences in relation to cortisol reactivity in adolescents at risk for asthma. Dev Psychobiol. 2013;55:133–144. doi: 10.1002/dev.21006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Borelli JL, West JL, Weekes NY, Crowley MJ. Dismissing child attachment and discordance for subjective and neuroendocrine responses to vulnerability. Dev Psychobiol. 2014;56:584–591. doi: 10.1002/dev.21107. [DOI] [PubMed] [Google Scholar]
- 25.Chapman BP, Fiscella K, Kawachi I, Duberstein P, Muennig P. Emotion suppression and mortality risk over a 12-year follow-up. J Psychosom Res. 2013;75:381–385. doi: 10.1016/j.jpsychores.2013.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26**.Puig J, Englund MM, Simpson JA, Collins WA. Predicting adult physical illness from infant attachment: A prospective longitudinal study. Health Psychol. 2013;32:409–417. doi: 10.1037/a0028889. Landmark study demonstrating that attachment in infancy predicts adult physical health 30 years later. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Powers SI, Pietromonaco PR, Gunlicks M, Sayer A. Dating couples’ attachment styles and patterns of cortisol reactivity and recovery in response to a relationship conflict. J Pers Soc Psychol. 2006;90:613–628. doi: 10.1037/0022-3514.90.4.613. [DOI] [PubMed] [Google Scholar]
- 28.Diamond LM, Hicks AM, Otter-Henderson KD. Every time you go away: Changes in affect, behavior, and physiology associated with travel-related separations from romantic partners. J Pers Soc Psychol. 2008;95:385–403. doi: 10.1037/0022-3514.95.2.385. [DOI] [PubMed] [Google Scholar]
- 29.Meuwly N, Bodenmann G, Germann J, Bradbury TN, Ditzen B, Heinrichs M. Dyadic coping, insecure attachment, and cortisol stress recovery following experimentally induced stress. J Fam Psychol. 2012;26:937–947. doi: 10.1037/a0030356. [DOI] [PubMed] [Google Scholar]
- 30**.Jaremka LM, Glaser R, Loving TJ, Malarkey WB, Stowell JR, Kiecolt-Glaser JK. Attachment anxiety is linked to alterations in cortisol production and cellular immunity. Psychol Sci. 2013;24:272–279. doi: 10.1177/0956797612452571. In the first study to examine attachment in relation to daily levels of both cortisol and immune responses, husbands and wives who were higher in attachment anxiety evidenced higher cortisol levels and lower levels of several forms of T-cells, reflecting lowered immune responding. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dewitte M, De Houwer J, Goubert L, Buysse A. A multi-modal approach to the study of attachment-related distress. Biol Psychol. 2010;85:149–162. doi: 10.1016/j.biopsycho.2010.06.006. [DOI] [PubMed] [Google Scholar]
- 32**.Beck LA, Pietromonaco PR, DeBuse CJ, Powers SI, Sayer AG. Spouses’ attachment pairings predict neuroendocrine, behavioral, and psychological responses to marital conflict. J Pers Soc Psychol. 2013;105:388–424. doi: 10.1037/a0033056. The first study to demonstrate that the interplay, or fit, between spouses’ attachment pairings is associated with distinctive cortisol patterns in anticipation of a conflict discussion, pointing to the importance of examining attachment effects within the dyadic relationship context. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Padgett DA, Glaser R. How stress influences the immune response. Trends Immunol. 2003;24:444. doi: 10.1016/s1471-4906(03)00173-x. [DOI] [PubMed] [Google Scholar]
- 34.Repetti RL, Taylor SE, Seeman TE. Risky Families: Family Social Environments and the Mental and Physical Health of Offspring. Psychol Bull. 2002;128:330. [PubMed] [Google Scholar]
- 35.Blair C, Berry D, Mills-Koonce R, Granger D. Cumulative effects of early poverty on cortisol in young children: Moderation by autonomic nervous system activity. Psychoneuroendocrinology. 2013;38:2666–2675. doi: 10.1016/j.psyneuen.2013.06.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mills-Koonce WR, Wagner NJ, Willoughby MT, Stifter C, Blair C, Granger DA. Greater fear reactivity and psychophysiological hyperactivity among infants with later conduct problems and callous-unemotional traits. J Child Psychol Psychiatry. 2014 doi: 10.1111/jcpp.12289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37*.Tharner A, Dierckx B, Luijk MPCM, van Ijzendoorn MH, Bakermans-Kranenburg MJ, van Ginkel JR, Moll HA, Jaddoe VWV, Hofman A, Hudziak JJ, et al. Attachment disorganization moderates the effect of maternal postnatal depressive symptoms on infant autonomic functioning. Psychophysiology. 2013;50:195–203. doi: 10.1111/psyp.12003. In a sample of over 400 mother-infant dyads, infants with a disorganized attachment pattern showed autonomic dysregulation only when their mothers had higher symptoms of depression, reinforcing the significance of the dyadic context. [DOI] [PubMed] [Google Scholar]
- 38.Conradt E, Measelle J, Ablow JC. Poverty, problem behavior, and promise: Differential susceptibility among infants reared in poverty. Psychol Sci. 2013;24:235–242. doi: 10.1177/0956797612457381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Diamond LM, Hicks AM, Otter-Henderson K. Physiological evidence for repressive coping among avoidantly attached adults. J Soc Pers Relatsh. 2006;23:205–229. [Google Scholar]
- 40.Roisman GI. The psychophysiology of adult attachment relationships: Autonomic reactivity in marital and premarital interactions. Dev Psychol. 2007;43:39–53. doi: 10.1037/0012-1649.43.1.39. [DOI] [PubMed] [Google Scholar]
- 41.Holland AS, Roisman GI. Adult attachment security and young adults’ dating relationships over time: Self-reported, observational, and physiological evidence. Dev Psychol. 2010;46:552–557. doi: 10.1037/a0018542. [DOI] [PubMed] [Google Scholar]
- 42.Diamond LM, Fagundes CP. Psychobiological research on attachment. J Soc Pers Relatsh. 2010;27:218–225. [Google Scholar]
- 43.Sapolsky RM, Romero LM, Munck AU. How do glucocorticoids influence stress responses? Integrating permissive, suppressive, stimulatory, and preparative actions. Endocr Rev. 2000;21:55–89. doi: 10.1210/edrv.21.1.0389. [DOI] [PubMed] [Google Scholar]
- 44.Fagundes CP, Glaser R, Kiecolt-Glaser JK. Stressful early life experiences and immune dysregulation across the lifespan. Brain Behav Immun. 2013;27:8–12. doi: 10.1016/j.bbi.2012.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Dowd JB, Zajacova A, Aiello AE. Predictors of Inflammation in U.S. Children Aged 3–16 Years. Am J Prev Med. 2010;39:314–320. doi: 10.1016/j.amepre.2010.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Dowd JB, Palermo TM, Aiello AE. Family poverty is associated with cytomegalovirus antibody titers in U.S. Children. Health Psychol. 2012;31:5–10. doi: 10.1037/a0025337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Miller GE, Chen E. Harsh Family Climate in Early Life Presages the Emergence of a Proinflammatory Phenotype in Adolescence. Psychol Sci Sage Publ Inc. 2010;21:848–856. doi: 10.1177/0956797610370161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Slopen N, Koenen KC, Kubzansky LD. Childhood adversity and immune and inflammatory biomarkers associated with cardiovascular risk in youth: A systematic review. Brain Behav Immun. 2012;26:239–250. doi: 10.1016/j.bbi.2011.11.003. [DOI] [PubMed] [Google Scholar]
- 49.Chen E, Miller GE, Kobor MS, Cole SW. Maternal warmth buffers the effects of low early-life socioeconomic status on pro-inflammatory signaling in adulthood. Mol Psychiatry. 2011;16:729–737. doi: 10.1038/mp.2010.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Gouin J-P, Glaser R, Loving TJ, Malarkey WB, Stowell J, Houts C, Kiecolt-Glaser JK. Attachment avoidance predicts inflammatory responses to marital conflict. Brain Behav Immun. 2009;23:898–904. doi: 10.1016/j.bbi.2008.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Robles TF, Brooks KP, Kane HS, Schetter CD. Attachment, skin deep? Relationships between adult attachment and skin barrier recovery. Int J Psychophysiol. 2013;88:241–252. doi: 10.1016/j.ijpsycho.2012.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Fagundes CP, Jaremka LM, Glaser R, Alfano CM, Povoski SP, Lipari AM, Agnese DM, Yee LD, Carson WE, III, Farrar WB, et al. Attachment anxiety is related to Epstein–Barr virus latency. Brain Behav Immun. 2014;41:232–238. doi: 10.1016/j.bbi.2014.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53*.Kidd T, Poole L, Leigh E, Ronaldson A, Jahangiri M, Steptoe A. Attachment anxiety predicts IL-6 and length of hospital stay in coronary artery bypass graft surgery (CABG) patients. J Psychosom Res. 2014;77:155–157. doi: 10.1016/j.jpsychores.2014.06.002. Patients with higher attachment anxiety showed greater inflammatory responses (IL-6) following coronary artery surgery, highlighting the importance of examining attachment within the context of significant health events. [DOI] [PMC free article] [PubMed] [Google Scholar]


