Abstract
Multidrug resistance (MDR) in Enterobacter aerogenes can be mediated by induction of MarA, which is triggered by certain antibiotics and phenolic compounds. In this study, we identified the gene encoding RamA, a 113-amino-acid regulatory protein belonging to the AraC-XylS transcriptional activator family, in the Enterobacter aerogenes ATCC 13048 type strain and in a clinical multiresistant isolate. Overexpression of RamA induced an MDR phenotype in drug-susceptible Escherichia coli JM109 and E. aerogenes ATCC 13048, as demonstrated by 2- to 16-fold-increased resistance to β-lactams, tetracycline, chloramphenicol, and quinolones, a decrease in porin production, and increased production of AcrA, a component of the AcrAB-TolC drug efflux pump. We show that RamA enhances the transcription of the marRAB operon but is also able to induce an MDR phenotype in a mar-deleted strain. We demonstrate here that RamA is a transcriptional activator of the Mar regulon and is also a self-governing activator of the MDR cascade.
Multidrug resistance (MDR) relates to all bacterial species but has been studied mostly in members of the Enterobacteriaceae, particularly in E. coli with the study of the mar operon (1, 17, 18, 32). The MDR phenotype often associates a decrease in porin synthesis with an increased activity of efflux pumps to restrict the intracellular concentration of various antibiotics, including β-lactams, tetracyclines, chloramphenicol, and quinolones. Resistance results from activation of the chromosomal genes by induction or mutation and by DNA transfer (21). A single drug treatment can lead to cross-resistance to other unrelated antibiotics (16). In clinical isolates which exhibit high resistance to broad-spectrum antibiotics, MDR is the result of enzymatic responses, mutations in the antibiotic target, and modifications in envelope permeability, including porin alteration and induction of drug efflux (7, 20, 23). In such a case, the existence of clinical strains resistant to several structurally unrelated antibiotics contributes to treatment failures in human infections, bacterial dissemination, outbreaks, and changes in patients' flora due to the selective advantage of the microorganism.
The mar regulon identified in E. coli plays a key role in the expression of the multidrug resistance phenotype. MarA expression induces the synthesis of the micF antisense RNA that downregulates the OmpF outer membrane porin, on one hand, and, on the other hand, overproduction of the AcrAB-TolC drug efflux pump (1, 3, 17). Mutations located in the MarR repressor leading to constitutive expression of the marRAB operon have been described in fluoroquinolone-resistant isolates of E. coli and Enterobacter cloacae (20, 25). The Rob and SoxS regulatory proteins are MarA homologues and participate in E. coli MDR regulation (1, 16, 28).
Among the emerging resistant bacteria, E. aerogenes is now the third leading cause of nosocomial respiratory tract infections (6, 11). A TEM-24-producing clone was the agent of a hospital pandemic (6, 13). Moreover, a concomitant decrease in porin synthesis and quinolone efflux has been reported in several clinical strains (4, 14). In a previous study, rapid modulation of porin synthesis during the course of patient therapy was observed in E. aerogenes, suggesting that resistance is mediated by a regulation event rather than a mutation (4). Recently, we described the functional role played in MDR in E. aerogenes by the marRAB operon, overexpression of which results in major porin decrease and norfloxacin active efflux (9).
In a single-step Klebsiella pneumoniae MDR mutant, George et al. characterized a novel genetic system, named ramA for “resistance antibiotic multiple” (15). The K. pneumoniae ramA locus cloned in E. coli elicited a high level of resistance to diverse antibiotics, including chloramphenicol, tetracycline, nalidixic acid, ampicillin, norfloxacin, trimethoprim, and puromycin, a decreased expression of OmpF porin, and the active efflux of chloramphenicol and tetracycline. ramA overexpression has been associated with fluoroquinolone resistance in K. pneumoniae isolates (30). The ramA locus was identified in Salmonella enterica serovar Paratyphi B and given the name rma, sharing a high percentage of identity (32). Rma was demonstrated to bind to the mar operator (32). Surprisingly, an alignment of K. pneumoniae ramA with the genome of E. coli indicates no homologue of the ramA locus.
In the present study, we identified the ramA gene of E. aerogenes. We demonstrate its involvement in the regulation of outer membrane impermeability and in the active extrusion of intracellular antibiotics. We show that E. aerogenes RamA is able to enhance the transcription of the E. coli marRAB operon but is also able to induce an MDR genetic cascade in an E. coli marRAB deletion background.
MATERIALS AND METHODS
Bacterial strains, plasmids, and growth media.
The bacterial strains and plasmids used in this study are listed in Table 1. All bacterial strains were grown in Luria-Bertani (LB) or Mueller-Hinton (MH) broth. Transformed strains were selected on LB agar containing ampicillin at 100 μg/ml, chloramphenicol at 50 μg/ml, or kanamycin at 50 μg/ml.
TABLE 1.
Bacterial strains and plasmids used in this study
| Strain or plasmid | Relevant featuresa | Source or reference |
|---|---|---|
| E. coli | ||
| JM109 | recA1 supE44 endA1 hsdR17 gyrA96 relA1 thi Δ(lac-proAB) | Laboratory collection |
| CH164 | AG100 ΔmarA zdd-230::Tn9 | 17 |
| SPC105 | MC4100 containing a chromosomal Pmarn::lacZ fusion at the λ attachment site and a wild-type mar locus | 10 |
| BW5104 | Mu-1 Δlac169 creB510 hsdR514 | 19 |
| EP663 | BW5104 tolC::Tn10, Tcr | 29 |
| E. aerogenes | ||
| ATCC 13048 | Susceptible strain | ATCC |
| EA27 | MDR clinical isolate | 29 |
| Plasmids | ||
| pDrive | High-copy-number PCR cloning vector, Ampr Knr | Qiagen |
| pRC2 | pDrive bearing the RaRBS and RaId PCR product to express ramA from Plac | This study |
| pBCSK+ | High-copy-number vector; Cmr | Stratagene |
| pRC3 | EcoRI fragment of pRC2 subcloned into pBCSK+ | This study |
| pmicB21 | pICIII bearing a micF::lacZ fusion | 27 |
Ampr, ampicillin resistant; Knr, kanamycin resistant; Cmr, chloramphenicol resistant, Tcr, tetracycline resistant.
Antibiotic susceptibility tests.
MICs were determined by a standard broth dilution method, as previously described (23). Approximately 106 cells were inoculated into 1 ml of MH broth containing twofold serial dilutions of each antibiotic: tetracycline, norfloxacin, cefepime, nalidixic acid, ceftazidime, and chloramphenicol. For the chloramphenicol MIC, phenylalanine arginine β-naphthylamide (PAβN) (Sigma-Aldrich) was added at 26.3 μg/ml; that concentration does not inhibit bacterial growth (22, 24). The results of triplicate tests were read after 18 h at 37°C and correspond to the highest dilution showing complete growth inhibition.
DNA preparation, Genome Walker, primers, and PCR.
DNA was prepared with the hexadecyltrimethylammonium bromide (CTAB) method (2). Primers were designed from the sequence of the E. aerogenes (RaId and RaRBS) and K. pneumoniae (A1, A2, and R2) ramA genes with primers A1 (forward; 5′-CCGCTCAGGTGATTGACACT-3′), A2 (reverse; 5′-GGTCTGCTGCGAATCAAGC-3′), R2 (reverse; 5′-GAAGTGGGCAAGAAAACGC-3′), RaId (reverse 5′-CAGATTAAGCCGCAAGAGAGC-3′), and RaRBS (forward; 5′-CGCTAACCGCCAGAGTGGT-3′).
PCR amplifications were performed in a GeneAmp PCR System 2400 thermocycler (Perkin Elmer), with an initial 5-min denaturation at 94°C followed by 30 cycles of denaturation at 94°C for 30 s, a 30-s annealing at 54°C, and a 2-min extension at 72°C. The 30 cycles were followed by a 7-min extension at 72°C. After determination of the partial sequence of the putative ramA gene with primers A1 and A2, the unknown 5′-end sequence was amplified with the Universal Genome Walker kit (Clontech Laboratories, Palo Alto, Calif.). Briefly, genomic DNA was digested with EcoRV, DraI, PvuII, StuI, and ScaI. DNA fragments were ligated with a Genome Walker adapter, which had one blunt end and one end with a 5′ overhang. The ligation mixture of the adapter was used as a template for PCR. This PCR was performed with an adapter primer supplied by the manufacturer and the reverse A2 primer to walk along the DNA sequence. The amplification was carried out according to the manufacturer's instructions.
DNA sequencing and data analysis.
The sequences of the PCR products were determined with an ABI Prism 377 DNA sequencer with dye fluorescent terminators and the primers used in the initial PCR amplification. Sequence analysis comparison was performed with the lalign program (http://www.ch.embnet.org/software/LALIGN_form.html).
β-Galactosidase assay.
The activity of the E. coli marRAB and micF promoters was measured by assaying the β-galactosidase activity of a chromosomal mar::lacZ operon fusion and a plasmid micF::lacZ fusion as described by Miller (26a).
Measurement of chloramphenicol accumulation.
Exponential-phase bacteria grown in LB broth were removed by centrifugation and washed once in 50 mM sodium phosphate buffer (SPB), pH 7. Pellets were suspended in the same buffer to a density of 2 × 1010 CFU ml−1 and kept at 37°C for no more than 30 min before use. To deenergize the bacteria, 50 μM carbonyl cyanide m-chlorophenyl hydrazone (CCCP) (Sigma-Aldrich) was added 10 min before the radiolabeled chloramphenicol. Assays were initiated by adding [14C]chloramphenicol (10 μg/ml, 1010 cpm/ml; a gift from Aventis Hoescht Marrion Roussel Laboratories). Samples (100 μl) were removed at set intervals and immediately filtered through 0.45-μm Whatman GF/C filters presoaked in SPB and then washed twice with 5 ml of cold SPB. The filters were dried, and the radioactivity was determined in a Beckman scintillation spectrophotometer. Positive and negative control samples were run under identical conditions (23, 24). The accumulation experiments were performed in duplicate.
SDS-PAGE and immunodetection of porins and AcrA.
Exponential-phase bacteria grown in LB broth were pelleted and solubilized in boiling buffer at 96°C. Samples (an amount corresponding to 0.02 optical density units at 600 nm) were loaded on sodium dodecyl sulfate (SDS)-polyacrylamide gels (10% polyacrylamide, 0.1% SDS) for SDS-polyacrylamide gel electrophoresis (PAGE) as previously described (8) and then electrotransferred to nitrocellulose membranes. An initial saturating step with Tris-buffered sodium (TBS; 50 mM Tris-HCl, 150 mM NaCl, pH 8) containing 10% skim milk powder was carried out overnight at 4°C. The nitrocellulose membranes were then incubated in TBS containing 10% skim milk powder and 0.2% Triton X-100 for 2 h at room temperature in the presence of polyclonal antibodies directed against the internal porin L3 loop or against AcrA. The polyclonal antibody F4 was prepared against a peptide located within the internal porin L3 loop and recognized enterobacterial porins as previously described (12). The polyclonal anti-AcrA antibody has been previously described (29). After four washes in the same buffer, detection was performed with alkaline phosphatase-conjugated AffinitiPure goat anti-rabbit immunoglobulin G antibodies (Jackson ImmunoResearch).
Nucleotide sequence accession number.
The nucleotide sequence determined in this study has been submitted to the EMBL database and given accession no AJ404625.
RESULTS
Identification of ramA in E. aerogenes.
The E. aerogenes ramA gene was PCR amplified with primers A1 and A2, chosen from the K. pneumoniae ramA sequence, and the reverse R2 primer, chosen in the 3′ flanking region surrounding the K. pneumoniae ramA gene. PCR assays were performed on the genomic DNA of E. aerogenes ATCC 13048 (type strain) and on the MDR clinical isolate EA27 (23, 29). For both strains with primers A1 and A2, an identical 339-bp sequence encoding a 113-amino-acid putative protein was obtained. The sequence of the promoter region was obtained by the genome walker method on E. aerogenes ATCC 13048 DNA restricted by ScaI and amplified with the A2 primer and the Ap2 primer supplied by the manufacturer. An identical ramA product was also PCR amplified with primers A1 and A2 in all 39 E. aerogenes clinical isolates tested (data not shown). Alignment of the predicted amino acid sequence of RamA from E. aerogenes with those of the two known homologues in S. enterica and K. pneumoniae exhibited high interspecific conservation. The putative sequence of RamA of E. aerogenes showed greater amino acid similarity with RamA of K. pneumoniae (98%) than with Rma of S. enterica (92%) (lalign program).
RamA sequence analysis and putative marbox.
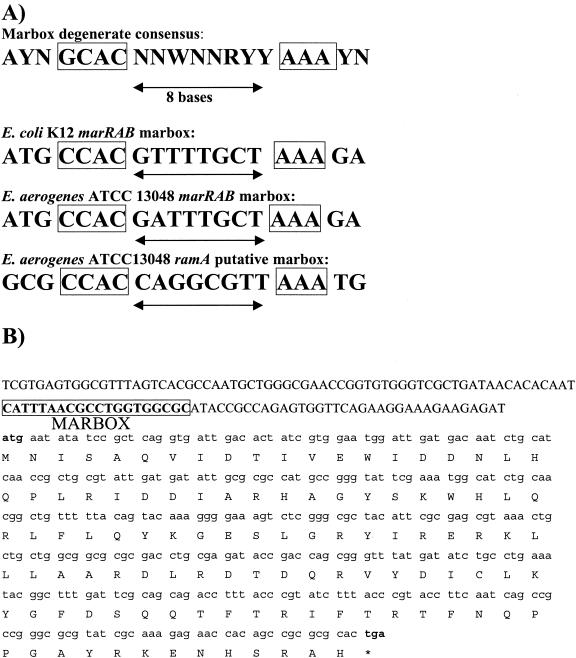
The RamA and MarA alignment shows that amino acids in their helix-turn-helix DNA binding motif are mostly conserved, suggesting that the two proteins could regulate the same target genes (Fig. 1). The transcriptional activator MarA binds as a monomer to a 20-bp degenerate asymmetric recognition sequence named the marbox (Fig. 2) (26). As MarA is able to autoregulate its expression, we looked for the presence of a marbox in the promoter region of ramA. From the consensus sequence of the E. coli marbox and the putative MarA binding site of the E. aerogenes mar operon, we identified a putative marbox in the ramA promoter region (Fig. 2). This putative marbox is in a backward orientation and would belong to class I of the MarA-activated promoters (26).
FIG. 1.
Multiple-sequence alignment of RamA and MarA of E. aerogenes. Sequences were aligned by use of the Lalign program. The locations of the two helix-turn-helix motifs are marked by overlining, identical residues are shaded, and conservative replacements are underlined.
FIG. 2.
(A) Alignment of the marboxes of the E. coli and E. aerogenes mar operons and of E. aerogenes ramA with the consensus (N, any base; W, A or T; R, A or G; Y, C or T). (B) Position of the E. aerogenes putative ramA marbox on the nucleotide sequence of ramA; the start and stop codons are in bold.
ramA overexpression induces multidrug resistance in E. coli and in E. aerogenes.
The 447-bp PCR product obtained by ramA amplification with the RaRBS and RaId primers, including the whole open reading frame and the ribosome binding site, was cloned into plasmid pDRIVE to generate pRC2. To test the hypothesis that RamA acts as an MDR activator, we introduced pRC2 into E. coli JM109 and into E. aerogenes ATCC 13048. Both transformants presented a 2- to 16-fold increase in MICs of the antibiotics tested (Table 2). Thus, ramA overexpression confers an MDR phenotype on E. coli and E. aerogenes. The MICs for chloramphenicol were evaluated in the presence of PAβN, a nonspecific efflux pump inhibitor (22, 24). In the presence of PAβN (26.3 μg/ml), the MIC of chloramphenicol for JM109(pRC2) decreased eightfold, from 64 to 8 μg/ml, indicating the activity of an efflux system in the transformed strains.
TABLE 2.
Effect of RamA expression
| Strain | MICa (μg/ml)
|
|||||
|---|---|---|---|---|---|---|
| CHL | TET | NAL | NOR | CAZ | FEP | |
| E. coli | ||||||
| JM109 | 8 | 1 | 64 | 0.5 | 0.5 | 0.047 |
| JM109(pRC2) | 64 | 16 | 128 | 2 | 0.5 | 0.38 |
| CH164 | 8 | 4 | 8 | 0.5 | 2 | 0.25 |
| CH164(pRC2) | 32 | 16 | 32 | 1 | 4 | 2 |
| BW5104 | 16 | 4 | 4 | 0.25 | 0.25 | 0.016 |
| BW5104(pRC2) | 64 | 16 | 16 | 0.5 | 1 | 0.094 |
| EP663 | 2 | R | 0.25 | 0.5 | 0.125 | 0.016 |
| EP663 (pRC2) | 2 | R | 0.25 | 0.06 | 1 | 0.094 |
| E. aerogenes | ||||||
| ATCC 13048 | 8 | 4 | 8 | 0.5 | 2 | 0.25 |
| ATCC 13048(pRC2) | 32 | 16 | 32 | 1 | 4 | 2 |
CHL, chloramphenicol; TET, tetracycline; NAL, nalidixic acid; NOR, norfloxacin; CAZ, ceftazidime; FEP, cefepime; R, resistant.
Consequently, to evaluate the importance of the efflux mechanism in the resistance mediated by RamA, pRC2 was introduced into an E. coli tolC null mutant strain. Compared to the BW5104 parental strain, a decrease in the MICs for chloramphenicol (eightfold) and nalidixic acid (16-fold) was observed in the tolC mutant (EP663), showing that efflux mediated by TolC is involved in the resistance to these antibiotics (Table 2). In the absence of TolC, RamA overproduction did not increase chloramphenicol and nalidixic acid resistance levels, indicating that ramA-mediated efflux requires TolC. For β-lactams such as cefepime and ceftazidime, which work by decreasing permeability, inactivation of tolC had no effect on the resistance level even when ramA was overexpressed.
Evidence of active efflux of chloramphenicol in E. coli expressing ramA.
The increase in the MICs for chloramphenicol and tetracycline in the strain containing pRC2 suggested the presence of an efflux pump (Table 2). To examine this mechanism, the intracellular accumulation of radiolabeled chloramphenicol was studied in E. coli JM109(pRC2). A severe decrease in the intracellular accumulation of [14C]chloramphenicol was measured in the presence of pRC2, with a reduction of about fivefold compared to JM109 (Fig. 3). The addition of CCCP, which collapses the membrane energy and blocks the energy-dependent efflux pump, induced a noticeable increase in the intracellular level of [14C]chloramphenicol in JM109(pRC2) (23, 24). CCCP partially restored a level of intracellular chloramphenicol similar to that in the wild-type strain. These results suggest that RamA production from pRC2 is able to induce the expression of an active efflux pump.
FIG. 3.
Accumulation of [14C]chloramphenicol in E. coli JM109 (▴), JM109(pRC2) (♦), and JM109(pRC2) in the presence of CCCP (▪).
ramA overexpression in E. coli and in E. aerogenes causes AcrA increase and porin decrease.
Rma was shown to induce MDR by porin downregulation associated with a TolC increase, evidenced by Western blotting, suggesting the presence of efflux (32). In order to characterize the ramA MDR activation pathway, immunodetection of porins and AcrA was performed with the F4 antipeptide, directed against the porin L3 loop on E. coli JM109(pRC2) and E. aerogenes ATCC 13048(pRC2) and with AcrA antibodies on E. aerogenes ATCC 13048(pRC2). RamA overexpression in E. coli JM109 and in E. aerogenes ATCC 13048 harboring pRC2 induced a noticeable decrease in production of the major porin. Conjointly, we observed overexpression of AcrA, the periplasmic component of the AcrAB-TolC efflux pump in E. aerogenes ATCC 13048(pRC2) (Fig. 4).
FIG. 4.
Immunoblots of whole-membrane extracts with antibodies raised against E. aerogenes AcrA (A) and against porins (F4 antibodies) (B). (A) Lane 1, E. aerogenes ATCC 13048; lane 2, E. aerogenes ATCC 13048(pRC2); lane 3, E. coli CH164; lane 4, E. coli CH164(pRC2). Lane 1, E. coli JM109; lane 2, E. coli JM109(pRC2); lane 3, E. aerogenes ATCC 13048; lane 4, E. aerogenes ATCC 13048(pRC2); lane 5, E. coli CH164; lane 6, E. coli CH164(pRC2).
RamA induces an MDR phenotype in a marRAB deletion background.
The precise role of RamA in the MDR regulation cascade remains quite obscure. In order to define whether RamA is able to induce an MDR response by a marRAB operon independent pathway, the E. coli CH164 Δmar strain was transformed with pRC2. Measures of antibiotics susceptibility and immunodetection of porins and AcrA were performed. The transformed strain exhibited increased MICs to structurally unrelated antibiotics (Table 2) and a porin production decrease associated with an increase in AcrA synthesis (Fig. 4).
The MDR phenotype in CH164(pRC2) was similar to that observed in JM109(pRC2). Thus, RamA is able to induce an MDR cascade independently of the mar operon.
RamA effect on marRAB operon and micF RNA.
Yassien et al. previously reported that a MalE-Rma hybrid is able to bind to the E. coli mar operator (32). To determine whether RamA can regulate mar operon transcription, we investigated the effect of RamA on a mar::lacZ chromosomal fusion in E. coli. E. coli SPC105 was transformed with pRC3 bearing ramA, and β-galactosidase assays were performed. Since pRC3 encodes chloramphenicol resistance and chloramphenicol is an inducer of the mar operon expression (1), experiments were carried out in the absence of chloramphenicol, and the presence of pRC3 was verified after each assay. The results indicate that in the presence of pRC3, the β-galactosidase activity of the mar::lacZ strain was increased fourfold. The β-galactosidase activities of E. coli strains SPC105 mar::lacZ, SPC105(pRC3), JM109, JM109(pmicB21), and JM109(pmicB21, pRC3) were 480 ± 57, 1,950 ± 132, 80 ± 6, 530 ± 50, and 1,880 ± 73 Miller units, respectively (mean ± standard deviation).
To assay whether RamA affected micF transcription, JM109 was cotransformed with pmicB21 bearing a micF::lacZ fusion and with pRC3. The β-galactosidase activity in JM109(pmicB21) was increased 3.5-fold in presence of pRC3 (see above). micF activation may be due to direct activation by RamA and/or indirect activation through the mar operon. These results suggest that RamA is able to induce transcription of both the mar operon and the anti-sense micF RNA in E. coli.
DISCUSSION
In this study, we characterized the E. aerogenes ramA gene and its role in the induction of the MDR response. RamA overexpression in the susceptible E. coli JM109 and in E. aerogenes ATCC 13048 strains induces an MDR phenotype, as evidenced by increases in the MICs of structurally unrelated antibiotics. We showed that RamA induces a significant reduction in the amount of intracellular radiolabeled chloramphenicol. Strains expressing RamA are less permeable due to a loss of the major porins, and in addition they produce larger amounts of the AcrA periplasmic linker protein, involved in the AcrAB-TolC efflux pump.
RamA belongs to the AraC-XylS regulator family. In this broad family, RamA is very close to a group of MDR regulators, including MarA, SoxS, and Rob. RamA and MarA from E. aerogenes share 45% identity, and the amino acids of the two DNA binding motifs essential to the regulatory function of MarA are well conserved in RamA. It is tempting to speculate that RamA and MarA recognize an overlapping set of operator sequences. This idea is supported by the ability of strains expressing RamA to overexpress acrA and micF, two target genes of MarA. Moreover, the presence of a putative marbox in the ramA promoter has been detected. This putative marbox is very well conserved, according to the consensus (26). MarA and also RamA could therefore regulate the transcription of ramA.
The transcriptional activator MarA autoregulates the expression of the marRAB operon via its binding to a marbox on its own operator (1). Using a lac reporter gene fused to the mar promoter, we showed that RamA overproduction is able to enhance expression of the E. coli mar operon. As the marRAB operons of E. coli and E. aerogenes share a high percentage of identity (9), we propose that RamA is able to modulate E. aerogenes marRAB operon transcription. In contrast to E. coli, in which no ramA homologue have been found in the two genomes sequenced (strains K-12 and O157:H7), E. aerogenes possesses two MDR transcriptional activators, MarA and RamA.
The major finding of this study is that constitutive expression of RamA results in an MDR phenotype even in the absence of the mar locus. Indeed, E. coli CH164 Δmar transformed with pRC2 exhibited an increase in the MICs of unrelated antibiotics, a loss of porins, and an increase in AcrA expression. The RamA-induced phenotype is very similar to that induced by MarA, but RamA is able to activate the MDR cascade independently of MarA. It is important to notice that these results indicate that E. aerogenes is able to regulate the marRAB operon by two processes: the chemical effector way with salicylate (9) and the genetic regulator way with RamA, described here. Thus, RamA can promote MDR by direct activation of acrAB and micF and indirect activation through MarA. The duplication of MDR activation pathways may explain the rapid and efficient adaptive response of E. aerogenes during antibiotic treatment and the emergence of MDR strains in vivo (4, 5, 14). It is now important to define the conditions of ramA expression and the benefit to bacteria of possessing two genes, ramA and marA, with a similar function. Therefore, we need to study the relationship between the MarA and RamA genetic systems to decipher their individual involvement in MDR.
Acknowledgments
We thank E. Pradel, S. B. Levy, and J. L. Rosner for the generous gift of bacterial strains and Aventis Pharma (Romainville, France) for the radiolabeled chloramphenicol.
R. Chollet is a recipient of a grant from the Fondation pour la Recherche Médicale. This work was supported by the Université de la Méditerranée and the Assistance Publique à Marseille.
REFERENCES
- 1.Alekshun, M. N., and S. B. Levy. 1997. Regulation of chromosomally mediated multiple antibiotic resistance: the mar regulon. Antimicrob. Agents Chemother. 41:2067-2075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ausubel, F. M., R. E. Brent, D. D. Kingston, J. G. Moor, J. A. Seidman, and K. Struhl (ed.). 1995. Current protocols in molecular biology. John Wiley & Sons, New York, N.Y.
- 3.Barbosa, T. M., and S. B. Levy. 2000. Differential expression of over 60 chromosomal genes in Escherichia coli by constitutive expression of MarA. J. Bacteriol. 182:3467-3474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bornet, C., A. Davin-Regli, C. Bosi, J. M. Pagès, and C. Bollet. 2000. Imipenem resistance of Enterobacter aerogenes mediated by outer membrane permeability. J. Clin. Microbiol. 38:1048-1052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bornet, C., R. Chollet, M. Mallea, J. Chevalier, A. Davin-Regli, J. M. Pages, and C. Bollet. 2003. Imipenem and expression of multidrug efflux pump in Enterobacter aerogenes. Biochem. Biophys. Res. Commun. 301:985-990. [DOI] [PubMed] [Google Scholar]
- 6.Bosi, C., A. Davin-Regli, C. Bornet, M. Malléa, J. M. Pagès, and C. Bollet. 1999. Most Enterobacter aerogenes strains in France belong to a prevalent clone. J. Clin. Microbiol. 37:2165-2169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Charrel, R. N., J.-M. Pages, P. De Micco, and M. Mallea. 1996. Prevalence of outer membrane porin alteration in β-lactam-antibiotic-resistant Enterobacter aerogenes. Antimicrob. Agents Chemother. 40:2854-2858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chevalier, J., J. M. Pagès, and M. Malléa. 1999. In vivo modification of porin activity conferring antibiotic resistance to Enterobacter aerogenes. Biochem. Biophys. Res. Commun. 266:248-251. [DOI] [PubMed] [Google Scholar]
- 9.Chollet, R., C. Bollet, J. Chevalier, M. Mallea, J.-M. Pagès, and A. Davin-Regli. 2002. Characterization of a mar operon involved in the multidrug resistance of Enterobacter aerogenes. Antimicrob. Agents Chemother. 46:1093-1097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cohen, S. P., S. B. Levy, J. Foulds, and J. L. Rosner. 1993. Salicylate induction of antibiotic resistance in Escherichia coli: activation of the mar operon and a mar-independent pathway. J. Bacteriol. 175:7856-7862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Davin-Regli, A., D. Monnet, P. Saux, C. Bosi, R. N. Charrel, A. Barthelemy, and C. Bollet. 1996. Molecular epidemiology of Enterobacter aerogenes acquisition: one-year prospective study in two intensive care units. J. Clin. Microbiol. 34:1474-1480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.De, E., A. Basle, M. Jaquinod, N. Saint, M. Mallea, G. Molle, and J. M. Pages. 2001. A new mechanism of antibiotic resistance in Enterobacteriaceae induced by a structural modification of the major porin. Mol. Microbiol. 41:189-198. [DOI] [PubMed] [Google Scholar]
- 13.Dumarche, P., C. De Champs, D. Sirot, C. Chanal, R. Bonnet, and J. Sirot. 2002. TEM derivative-producing Enterobacter aerogenes strains: dissemination of a prevalent clone. Antimicrob. Agents Chemother. 46:1128-1131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gayet, S., R. Chollet, G. Molle, J. M. Pages, and J. Chevalier. 2003. Modification of outer membrane protein profile and evidence suggesting an active drug pump in Enterobacter aerogenes clinical strains. Antimicrob. Agents Chemother. 47:1555-1559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.George, A. M., R. M. Hall, and H. W. Stokes. 1995. Multidrug resistance in Klebsiella pneumoniae: a novel gene, ramA, confers a multidrug resistance phenotype in Escherichia coli. Microbiology 141:1909-1920. [DOI] [PubMed] [Google Scholar]
- 16.George, A. M. 1996. Multidrug resistance in enteric and other Gram-negative bacteria. FEMS Microbiol. Lett. 139:1-10. [DOI] [PubMed] [Google Scholar]
- 17.Hächler, H., S. P. Cohen, and S. B. Levy. 1991. marA, a regulated locus which controls expression of chromosomal multiple antibiotic resistance in Escherichia coli. J. Bacteriol. 173:5532-5538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kunonga, N. I., R. J. Sobieski, and S. S. Crupper. 2000. Prevalence of the multiple antibiotic resistance operon (marRAB) in the genus Salmonella. FEMS. Microbiol. Lett. 187:155-160. [DOI] [PubMed] [Google Scholar]
- 19.Lee, K. S., W. W. Metcalf, and B. L. Wanner. 1992. Evidence for two phosphonate degradative pathways in Enterobacter aerogenes. J. Bacteriol. 174:2501-2510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Linde, H. J., F. Notka, C. Irtenkauf, J. Decker, J. Wild, H.-H. Niller, P. Heisig, and N. Lehn. 2002. Increase in MICs of ciprofloxacin in vivo in two closely related clinical isolates of Enterobacter cloacae. Antimicrob. Agents Chemother. 44:1865-1868. [DOI] [PubMed] [Google Scholar]
- 21.Livermore, D. M. 2003. Bacterial resistance: origins, epidemiology, and impact. Clin. Infect. Dis. 36:S11-S23. [DOI] [PubMed] [Google Scholar]
- 22.Lomovskaya, O., M. S. Warren, A. Lee, J. Galazzo, R. Fronko, M. Lee, J. Blais, D. Cho, S. Chamberland, T. Renau, R. Leger, S. Hecker, W. Watkins, K. Hoshino, H. Ishida, and V. J. Lee. 2001. Identification and characterization of inhibitors of multidrug resistance efflux pumps in Pseudomonas aeruginosa: novel agents for combination therapy. Antimicrob. Agents Chemother. 45:105-116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Malléa, M., J. Chevalier, C. Bornet, A. Eyraud, A. Davin-Regli, C. Bollet, and J. M. Pagès. 1998. Porin alteration and active efflux: two in vivo drug resistance strategies used by Enterobacter aerogenes. Microbiology 144:3003-3009. [DOI] [PubMed] [Google Scholar]
- 24.Malléa, M., J. Chevalier, A. Eyraud, and J. M. Pagès. 2002. Inhibitors of antibiotics efflux pumps in resistant Enterobacter aerogenes strains. Biochem. Biophys. Res. Commun. 293:1370-1373. [DOI] [PubMed] [Google Scholar]
- 25.Maneewannakul, K., and S. B. Levy. 1996. Identification of mar mutants among quinolone resistant clinical isolates of Escherichia coli. Antimicrob. Agents Chemother. 40:1695-1698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Martin, R. G., and J. L. Rosner. 2002. Genomics of the marA/soxS/rob regulon of Escherichia coli: identification of directly activated promoters by application of molecular genetics and informatics to microarray data. Mol. Microbiol. 44:1611-1624. [DOI] [PubMed] [Google Scholar]
- 26a.Miller, J. H. 1972. Experiments in molecular genetics. Cold Spring Harbor Laboratory, Cold Spring Harbor, N.Y.
- 27.Mizuno, T., M.-Y. Chou, and M. Inouye. 1984. A unique mechanism regulating gene expression: translational inhibition by a complementary RNA transcript (micRNA). Proc. Natl. Acad. Sci. USA 81:1966-1970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Oethinger, M., L. Podglajen, W. V. Kern, and S. B. Levy. 1998. Overexpression of the marA or soxS regulatory gene in clinical topoisomerase mutants of Escherichia coli. Antimicrob. Agents Chemother. 42:2089-2094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pradel, E., and J. M. Pagès. 2002. The AcrAB-TolC efflux pump contributes to multidrug resistance in the nosocomial pathogen E. aerogenes. Antimicrob. Agents Chemother. 46:2640-2643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Schneiders, T., S. G. B. Amyes, and S. B. Levy. 2003. Role of AcrR and RamA in fluoroquinolone resistance in clinical Klebsiella pneumoniae isolates from Singapore. Antimicrob. Agents Chemother. 47:2831-2837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sulavik, M. C., M. Dazer, and P. F. Miller. 1997. The Salmonella typhimurium mar locus: molecular and genetic analyses and assessment of its role in virulence. J. Bacteriol. 179:1857-1866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Yassien, M. A., H. E. Ewis, C-D. Lu, and A. T. Abdelal. 2002. Molecular cloning and characterization of the Salmonella enterica serovar Paratyphi B rma gene, which confers multiple drug resistance in Escherichia coli. Antimicrob. Agents Chemother. 44:10-13. [DOI] [PMC free article] [PubMed] [Google Scholar]