Abstract
Computed tomography-guided percutaneous transthoracic fine-needle aspiration biopsy of lung lesions is a well known diagnostic technique. Nevertheless, it has some complications; such as pneumothorax, intraparenchymal hemorrhage and hemoptysis, which are not rare. Air embolism is one of the rare but potentially fetal complications of this procedure. Herein, we report the case of a 69-year-old male, in which case of systemic air embolism developed after the performance of lung biopsy. Early diagnosis and prompt oxygen therapy is crucial for patient’s survival so careful reviewing of the obtained computed tomography images during the biopsy may prevent a missing systemic air embolism and provide an adequate therapy.
Keywords: Air embolism, complications, computerized tomography guided biopsy, lung biopsy
Özet
Akciğerden bilgisayarlı tomografi eşliğinde perkütan transtorasik iğne aspirasyon biyopsisi iyi bilinen bir tanı yöntemidir. Ancak bu yöntemin pnömotoraks, intraparenkimal kanama ve hemoptizi gibi nadir olmayan bazı komplikasyonları vardır. Hava embolisi bu prosedürün en nadir ancak potansiyel olarak fatal komplikasyonlardan biridir. Bu yazıda, akciğer biyopsisi sonrası sistemik hava embolisi gelişen 69 yaşındaki bir erkek olguyu sunacağız. Erken tanı ve hızlı oksijen tedavisi hayati önem taşıdığıdından biyopsi sırasında elde edilen bilgisayarlı tomografi görüntülerinin dikkatli incelenmesi olası bir sistemik hava embolisinin gözden kaçmasını önleyecek ve uygun tedaviye olanak sağlayacaktır.
Introduction
Computed tomography (CT)-guided percutaneous transthoracic lung needle biopsy is a widely used diagnostic procedure for evaluating pulmonary lesions. The most common symptom is having indeterminate pulmonary nodules or masses. Other well known symptoms are the perihilar masses after failed or negative bronchoscopy, confirming or refuting the presence of malignancy, and where malignancy is confirmed; to characterize the tumor further, mediastinal masses, pulmonary nodules in patients with known extrathoracic malignancy etc. Percutaneous transthoracic lung biopsy is generally associated with higher complication rates compared to solid organ biopsy. One of the least frequent, but the most severe complication is air embolism (0.07%) [1].
Case Report
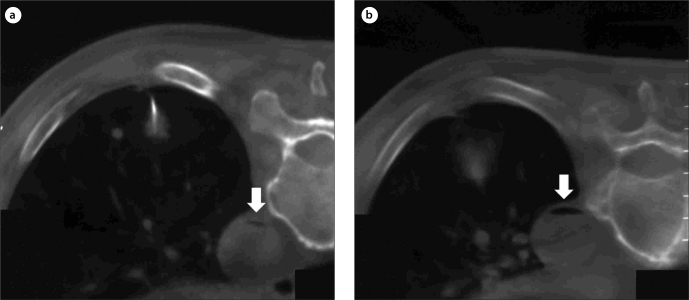
A 69-year-old man was referred to our radiology department with the history of fatigue, weight loss and weakness. Abnormal opacities were noted on conventional chest radiography, and therefore, he underwent chest computed tomography. On the chest CT scans, multiple nodules were detected in pulmonary parenchymal fields. Although a malignant process was suspected clinically, CT-guided percutaneous transthoracic needle biopsy of the lung lesions was planned for the definite diagnosis. After informed consent was obtained and a proper preparation in prone position; a single intervention using local anesthesia was performed with a 22-gauge spinal needle towards the peripherally seated nodule in the posterobasal segment of the left lung’s inferior lobe. The size of the nodule was 11×8 mm at a distance of 22 mm from the pleural surface. It was the largest and most accessible nodule in the subpleural region. Nevertheless; the patient maintained deep inspiration rather than holding his breath in spite of all the warnings made before and during the intervention. Upon the detection of air inside descending aorta in the CT sections taken to confirm the location of the needle, the procedure was aborted without delay (Figure 1a and b).
Figure 1. a, b.
Free air (arrow) in the aorta, at magnification control CT section for needle localization (a). Air within aorta (arrow) becomes more pronounced in a more distal CT section (b).
The anesthesiology team contacted our department promptly and performed the first medical intervention for the patient, who experienced a short duration of transient unconsciousness. The position of the patient, who was with stable vital signs, was changed to the Trendelenburg position and supportive oxygen therapy was applied. He was discharged from the intensive care unit without any sequela after two-days observation period.
Discussion
Percutaneous transthoracic lung biopsy is a widely used method of establishing the etiology of lung nodules. It is thought that Leyden developed the technique in 1883 to diagnose pneumonia and this technique was extended to the diagnosis of cancer from the 1930s onwards [2]. The biopsies were made under fluoroscopic guidance until the development of CT and they were performed under CT and CT-fluoroscopy guidance thereafter. Sonographic guidance is another technique utilized for large subpleural lesions.
The most commonly seen complications in percutaneous transthoracic lung biopsies are pneumothorax, intrapulmonary hemorrhage, and hemoptysis. Pneumothorax has a comparatively wide range of incidence that varies from 8 to 64% [3]. Although there is a higher frequency of fatality [4–6], the risks of hemorrhage (2–10%) and hemoptysis (7%) are low. Air embolism is a considerably uncommon complication; but it can lead to myocardial infarction, arrhythmia, and stroke; and can be fatal. It has a 0.02-to-0.007% incidence after percutaneous transthoracic biopsy [6–8]. Among the recently published articles; in the report of Hiraki et al. including 4 cases, none of the air embolisms ended fatally [1]. In fact, these types of studies show that air embolism is rarely reported because of the asymptomatic patients owing to the loss of air in the systemic circulation.
Several mechanisms can be defined to cause air embolism. First of them is the placement of the needle tip directly within the pulmonary vein and the contact of atmospheric air with the pulmonary vein when the stylet is taken out. Second is the formation of a bronchovenous fistula by the insertion of needle when passing through the parenchyma and entrance of intra-alveolar or intrabronchial air into the pulmonary venous circulation via this fistula.
Another factor that facilitates bronchovenous fistula formation is the inability of the vessel to perform its normal contraction because of its abnormal walls due to increased vascularity and post-inflammatory alterations invoked by the lesion.
Air embolism risk rises with the increase in the pressure within the air ways. Namely; the needle tip, which passes through a minor vein, leads to intraparenchymal hemorrhage, which in turn; causes hemoptysis with coughing and the intrapulmonary pressure that increases due to coughing facilitates entrance of intra-alveoar air into the venous circulation. Similarly; the pain, which is experienced during the passage of the pleura, leads to overt inspiration and this in turn; causes the air to easily enter the pulmonary vein by way of increased intra-alveolar pressure. In addition; a rigid lung parenchyma that governs cystic or cavitary lesions and vasculitides also increase the risk of air embolism. Recognition of air images in any of the arterial systems is both characteristic and diagnostic for an air embolism. Detection of free air images are noted in cerebral arteries, aorta and coronary arteries after lung biopsies [1, 7, 8]. Consequently; depending on the vulnerability of the end-organs to hypoxia, the volume of air and the extent of the involved area, clinical picture may range from a situation of mild temporary loss of consciousness to death, which is the most catastrophic complication [1, 7, 8].
Hyperbaric oxygen therapy is the primary treatment method. It diminishes the air volume, number of obstructive air bubbles and endothelial damage [9]. If this primary treatment modality is inaccessible at all times; the Trendelenburg position to reduce the cerebral embolisation risk and 100 % supportive oxygen therapy should be applied to the patient [7]. In any case; early diagnosis is very important for successful treatment. Once air embolism is suspected, the patient should be placed in the left lateral decubitus position or in Trendelenberg position to prevent residual air in the left atrium from entering the cerebral circulation. Supplemental 100% oxygen should be administered and general symptomatic support should be provided [10].
There are some precautions must be taken to prevent or minimize the risk of such a complication. These can be listed as; warning the patient not to cough or to maintain deep inspiration during the procedure, shortening the duration of the procedure, minimizing the communication with the atmospheric air during the procedure by digitally closing the needle tip after taking out the stylet, trying to keep the tract chosen for the procedure as remote as possible from the pulmonary vessels and bronchi, and finally trying to avoid performing a biopsy from a cystic, cavitary or bullous lung parenchyma as far as possible.
In conclusion; such a complication may occur even performed by a very experienced physician, an almost perfect technique and a very cooperative patient. The knowledge of the physician performing the biopsy about this complication and recognition of the associated signs and rapid therapeutic intervention he/she must perform are of prime importance.
Footnotes
Informed Consent: Informed consent was obtained from the patient who participated in this case.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept - D.C.O., C.S.; Design - D.C.O., C.S., A.S.E., C.A.; Supervision - D.C.O., C.A.; Funding - D.C.O., C.A.; Materials - C.S., A.S.E.; Data Collection and/or Processing - C.S., A.S.E., C.A; Analysis and/or Interpretation - D.C.O., C.S., A.S.E., C.A.; Literature Review - D.C.O., C.S., A.S.E.; Writing - D.C.O., C.S., A.S.E., C.A.; Critical Review - D.C.O., C.S., A.S.E., C.A.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Hiraki T, Fujiwara H, Sakurai J, et al. Systemic air embolism complicating percutaneous CT-guided transthoracic needle biopsy. Chest. 2007;132:684–90. doi: 10.1378/chest.06-3030. [DOI] [PubMed] [Google Scholar]
- 2.Manhire AR, Richardson CM, Gleeson FV. Lung biopsy guidelines for the obedience of fools and guidance wise men. Thorax. 2003;58:913–4. doi: 10.1136/thorax.58.11.913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Haramati LB, Austin JH. Complications after CT-guided needle biopsy through aerated versus nonaerated lung. Radiology. 1991;181:778. doi: 10.1148/radiology.181.3.1947096. [DOI] [PubMed] [Google Scholar]
- 4.Gohari A, Haramati LB. Complications of CT Scan-Guided Lung Biopsy: Lesion size and depth matter. Chest. 2004;126:666–8. doi: 10.1378/chest.126.3.666. [DOI] [PubMed] [Google Scholar]
- 5.Sinner WN. Complications of percutaneous transthoracic needle aspiration biopsy. Acta Radiol Diagn. 1976;17:813–28. doi: 10.1177/028418517601700609. [DOI] [PubMed] [Google Scholar]
- 6.Laurent F, Montaudon M, Latrabe V, et al. Percutaneous biopsy in lung cancer. Eur J Radiol. 2003;45:60–8. doi: 10.1016/s0720-048x(02)00286-3. [DOI] [PubMed] [Google Scholar]
- 7.Arnold BW, Zwiebel WJ. Percutaneous transthoracic needle biopsy complicated by air embolism. AJR Am J Roentgenol. 2002;178:1400–2. doi: 10.2214/ajr.178.6.1781400. [DOI] [PubMed] [Google Scholar]
- 8.Ghafoori M, Varedi P. Systemic air embolism after percutaneous transthoracic needle biopsy of the lung. Emerg Radiol. 2008;15:353–6. doi: 10.1007/s10140-007-0685-y. [DOI] [PubMed] [Google Scholar]
- 9.Ashizawa K, Watanabe H, Morooka H, Hayashi K. Hyperbaric oxygen therapy for air embolism complicating CT-guided needle biopsy of the lung. AJR Am J Roentgenol. 2004;182:1606–7. doi: 10.2214/ajr.182.6.1821606. [DOI] [PubMed] [Google Scholar]
- 10.Klein JS, Zarka MA. Transthoracic needle biopsy: an overview. J Thorac Imaging. 1997;12:232–49. doi: 10.1097/00005382-199710000-00002. [DOI] [PubMed] [Google Scholar]