Abstract
Objective
To determine the relative contributions of tinnitus, asymmetrical hearing loss, low frequency hearing loss (pure tone average of .5, 1, 2, 3 kHz, PTA.5123), or high frequency hearing loss (pure tone average of 4, 6 kHz, PTA46), to acute injury risk among a cohort of production and maintenance workers at six aluminum manufacturing plants, adjusting for ambient noise exposure and other recognized predictors of injury risk.
Design and Study Sample
This retrospective analysis considered 9,920 workers employed during 2003 to 2008. The cohort consisted of 8,818 workers (89%) whose complete records were available.
Results
Adjusting for noise exposure and other recognized injury predictors, a 25% increased acute injury risk was observed among workers with a history of tinnitus in conjunction with high-frequency hearing loss (PTA46). Low frequency hearing loss may be associated with minor, yet less serious, injury risk. We did not find evidence that asymmetry contributes to injury risk.
Conclusion
These results provide evidence that tinnitus, combined with high-frequency hearing loss, may pose an important safety threat to workers, especially those who work in high-noise exposed environments. These at risk workers may require careful examination of their communication and hearing protection needs.
Keywords: tinnitus, hearing asymmetry, hearing loss, workplace health and safety
Introduction
Hearing loss and tinnitus are global public health concerns (Yankaskas, 2013) with noise-induced hearing loss (NIHL) recognized as one of the most common occupational diseases in the United States (US) (Sataloff and Sataloff, 1996). An estimated 10 million US workers have hearing threshold levels (HTLs) ≥ 25 dB (Ward et al, 2000) and approximately 3.7 million working aged adults in the United Kingdom have some form of hearing loss (2011 Hearing Matters). Tinnitus, the perception of phantom sound not present in the environment, affects an estimated 12–15% of the general population in the US and Europe (Allman et al, 2013) and more than a third of the population over age 65 (Mattox, 2006). While as many as 80% of those with NIHL also suffer from tinnitus, either tinnitus or hearing loss can exist in the absence of the other (Mazurek et al, 2010).
Globally, approximately 100 million occupational injuries are reported each year although the true number of injuries occurring on the job may be much higher because of under-reporting (Leigh, 2011; Nelson et al, 2005). These injuries place an immense burden on workers and employers. Almost 8.6 million nonfatal occupational injuries occurred in the United States (US) in 2007 with costs reaching $186 billion (Leigh, 2011)
Many factors are recognized as contributing to occupational injury risk, including work demands, age, lifestyle and job stress (Chau et al, 2009; Pollack et al, 2007; Taiwo et al, 2009; Souza et al, 2014). Mounting evidence links ambient noise exposure to injury risk although the causal pathway for this association remains unclear (Amjad-Sardrudi et al, 2012; Moll van Charante and Mulder, 1990; Wilkins and Action, 1982; Picard et al, 2008; Girard et al, 2014). Additionally, hearing loss, which may impair both the perception of speech and the ability to hear warning signals, has been linked to increased injury risk in a number of previous reports, several of which used different frequencies and thresholds to determine hearing loss (Moll van Charante and Mulder, 1990; Wilkins and Action, 1982; Girard et al, 2014; Choi et al, 2005; Zwerling et al, 1996; Yung, 2014).
Hearing loss of >20 dBHL measured at 4 kHz has been associated with increased injury risk among male shipyard workers (Moll van Charante and Mulder, 1990) while hearing thresholds >25 dBHL at 1, 2, 3, and 4 kHz have been associated with increased injury risk among farmers (Choi et al, 2005). Additionally, bilateral hearing decrements at 3, 4, and 6 kHz have been associated with increased injury risk, with injury risk further elevated among hearing impaired workers exposed to high levels of occupational noise (Picard et al, 2008; Girard et al, 2009).
Tinnitus has been linked to sleep disturbance, depression, fatigue and decreased ability to concentrate (Hallam et al, 2004; Rossiter et al, 2006; Folmer and Griest, 2000; Folmer et al, 1999; Langguth et al, 2007) each of which may also increase injury risk (Vetter and Symonds, 2010; Arlinghaus et al, 2012). By producing irrelevant and/or confusing sounds that might compete with important workplace auditory cues, tinnitus may pose a workplace safety threat (Hallam et al, 2004).
Asymmetrical hearing loss has also been associated with injury risk (Choi et al, 2005), as it may interfere with components of sound localization, such as direction, distance and movement, and may impair speech perception in noisy environments (Nia and Bance, 2001). The prevalence of asymmetrical hearing loss varies depending on the criteria used, and differs for different populations (Margolis and Saly, 2008) so the true prevalence remains unclear.
Understanding the relative contribution of each of these attributes of hearing is critical to the development of meaningful interventions to reduce associated injury risks.
A previous report on a cohort from the company studied here revealed a positive exposure response association between ambient noise exposure and risk for both minor and serious injury, and a monotonic increase in minor injury risk with increasing hearing threshold at .5, 1, 2, and 3 kHz (Cantley et al, 2014). These findings raised additional questions regarding associations between hearing loss across higher frequencies, hearing asymmetry, tinnitus, and acute injury risk.
Building on our earlier work, the objective of this study is to examine the contribution of tinnitus, hearing asymmetry, and hearing across a range of frequencies to acute injury risk, adjusting for ambient noise exposure, reported use of hearing protection, and other job and individual level confounders previously associated with injury risk in this population of aluminum workers (Pollack et al, 2007; Taiwo et al, 2009; Kubo et al, 2013).
Methods
This study used data available through a longstanding partnership between the company and Yale University and Stanford University established to improve worker health and safety outcomes. Study protocols have been reviewed and approved by the human subjects committees at Yale University School of Medicine and Stanford University.
The study cohort was derived from the population of production and maintenance workers who were active any time between January 1, 2003 and December 31, 2008, at the six study plants. We determined job histories and calculated active person-time per year in each job held during the six year study period (2003–2008) using the human resources database, described in earlier reports (Pollack et al, 2007; Taiwo et al, 2009). The company’s real-time incident surveillance database, which contains detailed information for all work-related injuries and illnesses including those that result in first aid treatment only, was used to create yearly injury histories for each worker in each job held. Acute injuries were identified through the “nature of injury” variable, which describes each incident. Acute injury types included for analysis comprised lacerations, contusions, instantaneous strains/sprains, burns, dislocations, amputations, and other acute injuries. All acute injuries, sustained by the study cohort in jobs held between January 1, 2003, and December 31, 2008, were included for analysis. A separate analysis was conducted for the subset of more serious injuries that required medical treatment, work restrictions or lost work time, which were distinguished from the minor injuries using the “case type” variable.
The company’s industrial hygiene policies require regular noise sampling for all jobs where exposures are equal to or exceed an 8-hour time-weighted average of 82 dBA; therefore, multiple personal noise samples are available in the industrial hygiene database for distinct jobs. We calculated the arithmetic mean of all full shift personal noise samples (collected for at least 70% of shift length) for each job and assigned the average noise exposure by job for each job held to the individual workers exposed by means of a previously described linkage process (Pollack et al, 2007). Mean noise exposure was explored as a continuous as well as a categorical variable with the following noise exposure categories designated for analysis: less than 82 dBA (i.e., effectively non-noise exposed and used as the reference category); 82 to < 85 dBA (i.e., low noise exposure), 85 to < 88 dBA (i.e., moderate overexposure) and ≥ 88 dBA (i.e., high overexposure).
Individuals who work in jobs where at least 5% of the noise measurement samples equal or exceed an 8-hour time-weighted average of 82 dBA are enrolled in hearing conservation programs and undergo periodic audiometric testing, per company policy. Hearing tests are performed by certified audiometric technicians in test environments designed to meet ANSI standards. From this audiometric surveillance data, we used HTLs at a variety of single and combined frequencies for each study year for each member of the cohort, from the audiometric test performed prior to or up to 30 days after the beginning of each person-year contributed to the study period. Low frequency PTA.5123 was calculated by taking the binaural average of hearing thresholds for the frequencies of .5, 1, 2, and 3 kHz. Frequency specific HTLs were calculated for 4 kHz as well as 6 kHz by taking the binaural average of hearing thresholds for the frequencies of 4 kHz or 6 kHz, respectively. In addition, PTA46 was calculated as the binaural average at the combined frequencies of 4 kHz and 6 kHz. HTLs and PTAs were explored as continuous variables, and also dichotomized as < 25 dBHL (i.e. normal hearing which was used as the referent) and ≥ 25 dBHL (i.e., hearing loss).
Hearing asymmetry was calculated in two ways. First, using the American College of Otolaryngology criteria, we calculated hearing asymmetry as an average difference of ≥15 dB at 0.5, 1, 2 kHz or ≥ 30 dB at 3, 4, 6 kHz between ears (May, 2000). Second, using the less stringent criteria employed by Choi, et al (2005), hearing asymmetry was defined as an average difference ≥5 dB at 0.5, 1, 2 kHz between ears.
Self-reported hearing protection device (HPD) use among workers undergoing audiometric testing is frequently included in the company’s audiometric surveillance database. Frequency or consistency of HPD use, however, is not captured. To determine whether known use of hearing protection was a significant predictor of injury risk for the cohort, we dichotomized reported HPD use as known or unknown, with unknown used as the referent.
A history of tinnitus was determined by a positive response to the question, “Have you ever had noises in the ear?” on the audiometric questionnaire completed prior to each audiogram.
The job demand database, described in a previous report (Pollack et al, 2007) includes an overall rating of physical job demand for each job at the 6 study plants. Physical demand was dichotomized as heavy/very heavy versus light/medium for this study.
Subject Selection Criteria
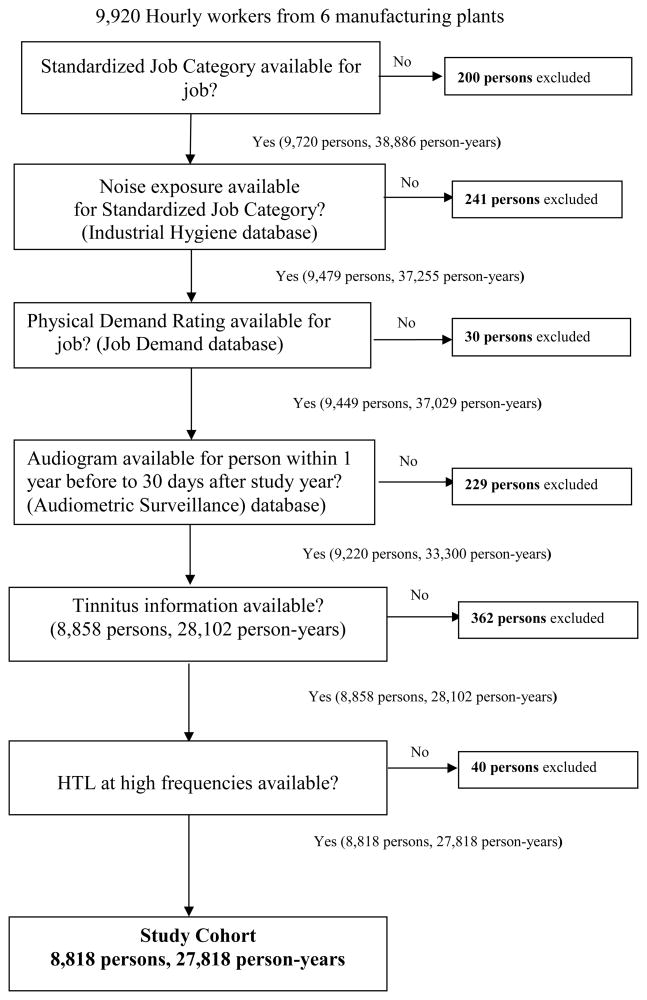
The study cohort was comprised of production and maintenance workers who worked any time between January 1, 2003 - December 31, 2008, in a job for which occupational noise exposure was sampled and physical demand was rated, answered the question regarding tinnitus on the audiometric questionnaire, and had an audiogram performed between the time period of 1 year before, to 30 days after, the start of each person-year contributed. Data was linked using an encrypted, uniform, unique identifier created for each person, to ensure human subject privacy. Construction of the study cohort is displayed in Figure 1.
Figure 1.
Construction of Study Cohort
Statistical Analysis
Descriptive analysis of baseline demographic characteristics for the cohort, and distribution at baseline of tinnitus, hearing asymmetry, low frequency PTA.5123 (binaural average at .5, 1, 2, 3 kHz), high-frequency PTA46 (binaural average at 4, 6 kHz), and frequency specific binaural HTLs at 4 kHz and 6 kHz was performed. The distribution of injury and serious injury by noise exposure category, HTL or PTA, hearing asymmetry, and history of tinnitus was calculated, as were unadjusted injury rates. We used generalized linear mixed models (GLMMs) to estimate relative risks (RRs) for injury, along with corresponding 95% CIs for frequency-specific HTL and combined frequency PTAs, modeled as both continuous and categorical variables (< 25 dBHL, ≥25 dBHL), tinnitus, and asymmetrical hearing loss in bivariate and multivariate models adjusted for ambient noise exposure. Multivariate models were additionally adjusted for sex, age, race/ethnicity, tenure < 1 year, physical job demand, reported hearing protection use, and calendar year, to account for any temporal trend in injury risk during the study period. Because of the non-linear effect of calendar year, year was included as a categorical variable. Finally, random effects for person within job, job within plant, and plant were incorporated to allow for between and within person, job and plant variation and account for correlation resulting from clustering. An unstructured covariance structure was specified (Stroup, 2012). Separate analyses were conducted for all acute injuries, as well as the subset of more serious acute injuries. A Poisson distribution with a log link and offset of the log person-days contributed to each job for each year of the study was chosen for the acute injury outcome that included minor injuries requiring first aid only. For models using serious acute injury as the outcome, a binomial distribution was selected to better fit the distribution of serious injury among the study cohort. All p values were two sided and a value of less than α = 0.05 was considered statistically significant. Interactions between ambient noise exposure, HTLs, PTAs, tinnitus, hearing asymmetry, and age were explored for significance.
All statistical analyses were performed using SAS version 9.3.
Results
During the 6-year study period at the six study plants, 8,818 workers contributing 27,818 person-years met the inclusion criteria (Figure 1). Table 1 displays descriptive statistics for the study cohort at baseline. Of these 8,818 workers (90% male, 88% white), 1,373 workers (16%) had a history of tinnitus, 466 (5%) had hearing asymmetry (defined as ≥15 dB difference at .5, 1, 2 kHz or ≥30 dB difference at 3, 4, 6 kHz), 904 workers (10%) had impaired hearing at combined frequencies of .5, 1, 2, 3 kHz, 3,943 workers (45%) had hearing loss ≥25 dB at combined frequencies of 4 and 6 kHz and 1,083 workers (12%) had a history of tinnitus in conjunction with hearing loss ≥25 dB at combined frequencies of 4 and 6 kHz at baseline. During the six-year study period, 2,999 workers in 3,296 person-jobs sustained 4,897 acute injuries, including minor injuries requiring first aid treatment only while 1,005 workers in 1,026 person-jobs sustained 1,104 serious injuries (Table 2). Table 2 also displays the distribution of injury and serious injury by audiometric measures of hearing sensitivity, hearing asymmetry, tinnitus, and noise exposure category throughout the study period.
Table 1.
Cohort Demographics at Baseline
| N | % | |
|---|---|---|
| Total | 8818 | 100 |
| Male | 7895 | 90 |
| Age (mean, SD) | 44.3, 10.5 | |
| White | 7736 | 88 |
| Mean Noise Exposure | ||
| < 82 dBA | 4068 | 46 |
| 82 to < 85 dBA | 2015 | 23 |
| 85 to < 88 dBA | 2104 | 24 |
| ≥ 88 dBA | 631 | 7 |
| PTA.5123 (binaural average at .5, 1, 2, 3 kHz) | ||
| < 25 dBHL | 7914 | 90 |
| ≥25 dBHL | 904 | 10 |
| Heavy/Very heavy physical demand | 1618 | 18 |
| HTL at 4 kHz (binaural average at 4 kHz) | ||
| < 25 dB | 5112 | 58 |
| ≥25 dB | 3706 | 42 |
| HTL at 6 kHz (binaural average at 6 kHz) | ||
| < 25 dBHL | 4687 | 53 |
| ≥25 dBHL | 4131 | 47 |
| PTA46 (binaural average of 4, 6 kHz) | ||
| < 25 dBHL | 4875 | 55 |
| ≥25 dBHL | 3943 | 45 |
| Tinnitus | 1373 | 16 |
| Hearing Asymmetry (≥5 dB difference at .5, 1, 2 kHz) | 1570 | 18 |
| Hearing Asymmetry (≥15 dB difference at .5, 1, 2 kHz or > 30 dB difference at 3, 4, 6 kHz) | 466 | 5 |
| Tinnitus plus PTA46 < 25 dBHL | 290 | 3 |
| Tinnitus and PTA46 > 25 dBHL | 1083 | 12 |
| No tinnitus and PTA46 < 25 dBHL | 4585 | 52 |
| No tinnitus and PTA46 > 25 dBHL | 2860 | 33 |
Abbreviations: dBA, A-weighted decibels; HTL, hearing threshold level; PTA, pure tone average; dB, decibels, dBHL, decibels hearing level
Table 2.
Distribution of acute injury and serious acute injury by noise exposure and hearing categories, tinnitus and hearing asymmetry
| All Acute Injury | Serious* Acute Injury | |||
|---|---|---|---|---|
| N | % | N | % | |
| Total Injuries | 4897 | 100 | 1,104 | 100 |
| Person-jobs in which injuries occurred | 3296 | 100 | 1,026 | 100 |
| Noise Exposure | ||||
| < 82 dBA | 2465 | 50 | 501 | 45 |
| 82 < 84.99 dBA | 939 | 19 | 221 | 20 |
| 85 < 87.99 dBA | 1127 | 23 | 252 | 23 |
| ≥ 88 dBA | 366 | 8 | 130 | 12 |
| PTA.5123 (binaural average at.5, 1, 2, 3 kHz) | ||||
| < 25 dBHL | 4359 | 89 | 982 | 89 |
| ≥ 25 dBHL | 538 | 11 | 122 | 11 |
| HTL at 4 kHz (binaural average at 4 kHz) | ||||
| < 25 dBHL | 2857 | 58 | 625 | 57 |
| ≥ 25 dB | 2040 | 42 | 479 | 43 |
| HTL at 6 kHz (binaural average at 6 kHz) | ||||
| < 25 dBHL | 2557 | 52 | 562 | 51 |
| ≥ 25 dBHL | 2340 | 48 | 542 | 49 |
| PTA46 (binaural average at 4, 6 kHz) | ||||
| < 25 dBHL | 2681 | 55 | 595 | 54 |
| ≥ 25 dBHL | 2216 | 45 | 509 | 46 |
| Tinnitus | 985 | 20 | 203 | 18 |
| Hearing Asymmetry** | 270 | 5 | 66 | 6 |
Abbreviations: dBA, A-weighted decibels; HTL, hearing threshold level; PTA, pure tone average; dB, decibels, dBHL, decibels hearing level
requiring medical treatment, work restrictions or lost work time
≥15 dB difference at .5,1,2 kHz or ≥ 30 dB difference at 3, 4, 6 kHz
The unadjusted injury rates by noise exposure category, audiometric results (single frequency and pure tone averages), tinnitus, and asymmetrical hearing loss are shown in Table 3.
Table 3.
Unadjusted All Injury and Serious Injury Rates per 100 Person-Years by Noise Exposure and Audiometric Status, Tinnitus, and Hearing Asymmetry 2003–2008
| All Acute Injury n (rate) | Serious* Acute Injury n (rate) | |
|---|---|---|
| Total | 4897 | 1104 |
| Mean Noise Exposure | ||
| < 82 dBA | 2465 (16.62) | 501 (3.38) |
| 82 to < 85 dBA | 939 (16.57) | 221 (3.90) |
| 85 to < 88 dBA | 1127 (21.85) | 252 (4.89) |
| ≥ 88 dBA | 366 (16.90) | 130 (6.00) |
| PTA.5123 (binaural average at .5,1,2,3 kHz) | ||
| <25 dBHL | 4359 (17.56) | 982 (3.96) |
| ≥25 dBHL | 538 (17.95) | 122 (4.07). |
| HTL at 4 kHz (binaural average at 4 kHz) | ||
| < 25 dBHL | 2857 (18.88) | 625 (4.13) |
| ≥ 25 dBHL | 2040 (16.08) | 479 (3.77) |
| HTL at 6 kHz (binaural average at 6 kHz) | ||
| < 25 dBHL | 2557 (18.85) | 562 (4.14) |
| ≥ 25 dBHL | 2340 (16.42) | 542 (3.80) |
| PTA46 (binaural average at 4, 6 kHz) | ||
| < 25 dBHL | 2681 (18.97) | 595 (4.21) |
| ≥ 25 dBHL | 2213 (16.19) | 509 (3.72) |
| Tinnitus | ||
| Yes | 985 (19.80) | 203 (4.08) |
| No | 3912 (17.13) | 901 (3.94) |
| Asymmetrical Hearing loss | ||
| Yes | 270 (17.58) | 66 (4.30) |
| No | 4627 (17.61) | 1038 (3.95) |
Abbreviations: dBA, A-weighted decibels; HTL, hearing threshold level; PTA, pure tone average; dB, decibels, dBHL, decibels hearing level
requiring medical treatment, work restrictions, or lost work time
The results of GLMM modeling indicated statistically significant interactions between tinnitus and HTL for the frequency specific HTLs at 4 kHz and 6 kHz and combined frequency PTAs at 4, 6 kHz (PTA46) for the acute injury outcome that included minor injuries. For the serious injury outcome, a significant interaction was found between tinnitus and frequency-specific HTL at 4 kHz and well as the combined frequency PTA at 4, 6 kHz (PTA46). Further exploration of these interactions revealed that hearing thresholds ≥25 dB at higher frequencies appeared to increase injury risk only among the group of workers with a history of tinnitus. Additionally, the binaural average at 4 and 6 kHz (PTA46) was the most sensitive high-frequency predictor of risk for both minor and serious injury outcomes among this cohort. Consequently, to increase ease of interpretation, tinnitus and PTA46 were combined into a single categorical variable with four levels:
) history of tinnitus plus PTA46 ≥25 dBHL (impaired high-frequency hearing);
) history of tinnitus and PTA46 < 25 dBHL (normal high-frequency hearing);
) no history of tinnitus but PTA46 ≥25 dBHL (impaired high-frequency hearing) and
) no history of tinnitus and PTA46 < 25 dBHL (normal high-frequency hearing), which was used as the reference category.
The results of the fully adjusted multivariate mixed effects models are shown in Table 4 for all acute injury and the subset of serious acute injury outcomes, with PTA.5123 (binaural average at .5, 1, 2, 3 kHz) modeled dichotomously (< 25 dBHL, ≥25 dBHL) and the high-frequency PTA46 (binaural average at 4, 6 kHz) and tinnitus variable modeled categorically, as described above. These multivariate models were simultaneously adjusted for noise exposure category, PTA.5123 category, sex, race/ethnicity, physical demand, tenure < 1 year, age, calendar year, reported hearing protection use, and the combined tinnitus-high-frequency PTA46 variable. Mean ambient noise exposure showed a monotonic and statistically significant exposure response association with injury risk for both injury outcomes examined. Compared to workers exposed to mean ambient noise of < 82 dBA, those exposed to average noise levels ≥88 dBA showed a 57% elevated injury risk (RR 1.57, CI: 1.09, 2.25) and nearly double the risk of serious injury (RR 1.99, CI: 1.28, 3.10). Low frequency hearing loss ≥25dBHL was associated with increased risk of minor (RR 1.11, CI: 1.00, 1.23) but not serious injury risk, although this association did not quite attain statistical significance (p=0.0553). Asymmetrical hearing loss was not associated with injury risk, while workers with a history of tinnitus who also displayed high-frequency hearing loss were at 25% greater risk for acute injury (RR 1.25, CI: 1.13, 1.38), as well as the subset of serious acute injuries (RR 1.25, CI: 1.02, 1.54). Reported HPD use versus unknown HPD use was protective for the injury outcome that included minor injuries (RR 0.87, CI: 0.78, 0.97) but did not predict more serious injury risk.
Table 4.
Fully adjusted multivariate mixed model results* with random intercepts for plant, job and person within plant-job Tinnitus and PTA46 (binaural average at 4, 6 kHz) combined into a categorical variable with 4 levels
| Outcome | All Injury | Serious Injury | ||||
|---|---|---|---|---|---|---|
| Relative Risk | 95% CI | Pr > F | Relative Risk | 95% CI | Pr > F | |
| Mean Noise Exposure | 0.0144 | 0.0091 | ||||
| 82 to < 85 dBA | 1.00 | Reference | 1.31 | 0.99, 1.73 | ||
| 82 to < 85 dBA | 1.17 | 0.95, 1.44 | 1.31 | 0.99, 1.73 | ||
| 85 to < 88 dBA | 1.37 | 1.08, 1.74 | 1.34 | 0.98, 1.82 | ||
| ≥ 88 dBA | 1.57 | 1.09, 2.25 | 1.99 | 1.28, 3.10 | ||
| PTA.5123 (binaural average at .5,1,2,3 kHz) | 0.0553 | 0.4750 | ||||
| <25 dBHL | 1.00 | Reference | 1.00 | Reference | ||
| ≥25 dBHL | 1.11 | 1.00, 1.23 | 1.08 | 0.87, 1.33 | ||
| Asymmetrical hearing loss | 0.97 | 0.85, 1.11 | 0.6393 | 1.09 | 0.84, 1.42 | 0.4991 |
| HPD use reported | 0.87 | 0.78, 0.97 | 0.0140 | 1.16 | 0.92, 1.45 | 0.2127 |
| Combined Tinnitus and PTA46 variable | <.0001 | 0.0259 | ||||
| No Tinnitus & PTA46 (binaural average at 4, 6 kHz) <25 dBHL | 1.00 | Reference | 1.00 | Reference | ||
| No Tinnitus & PTA46 (binaural average at 4, 6 kHz) ≥25 dBHL | 0.99 | 0.91, 1.07 | 0.97 | 0.83, 1.14 | ||
| Tinnitus & PTA46 (binaural average at 4, 6 kHz) <25 dBHL | 1.03 | 0.89. 1.20 | 0.79 | 0.55, 1.14 | ||
| Tinnitus & PTA46 (binaural average at 4, 6 kHz) ≥25 dBHL | 1.25 | 1.13, 1.38 | 1.25 | 1.02, 1.54 | ||
Simultaneously adjusted for noise, PTA.5123 (.5123 kHz), tinnitus (Y/N) and PTA46 at 4, 6 kHz (<25dB, ≥25dB) category, age, sex, race/ethnicity, high physical demand, tenure< 1 year, asymmetrical hearing loss, reported HPD use, and calendar year
Discussion
The results of this study suggest that tinnitus, in conjunction with hearing loss at high frequencies, may be an important predictor of acute occupational injury risk. At the same time, this current analysis, in contrast to our earlier findings, provides less evidence for an association between low-frequency hearing loss and risk of minor injuries. Certainly, further study is warranted to better discern associations between hearing impairment at low frequencies and acute injury risk. Asymmetrical hearing loss, associated with increased risk for injury in a previous report (Choi et al, 2005), did not elevate injury risk among the cohort studied here. However, the number of subjects in our study cohort with asymmetrical hearing loss was small, which may have resulted in insufficient statistical power to discern meaningful associations. Compared to those for whom HPD use was unknown, reported HPD use appeared protective for the all injury outcome that included minor events, but did not predict more serious injury risk for this cohort. Undoubtedly, the impact of HPD fit and usage patterns on injury risk merits future examination.
Using generalized linear mixed models with random effects for plant, job, and person within plant-job, and adjusting for other known injury risk predictors and potential confounders, we show that tinnitus, in combination with high-frequency PTA46 ≥25 dBHL, may elevate acute injury risk. This finding is of importance given that over-exposure to noise first causes hearing loss at these high frequencies. Tinnitus impacts a large portion of the general population and often, though not always, occurs in conjunction with NIHL. Although reports documenting evidence for an association between acute bodily injury risk and tinnitus are extremely scarce in the extant literature, myriad evidence suggests linkages between tinnitus and sleep disturbance, fatigue, and distraction, findings which make an association between tinnitus and acute occupational injury risk quite plausible. Notably, mean PTA46 was 43.8 (SD 20.7) for the subset of the cohort reporting any history of tinnitus compared to a mean PTA46 of 24.2 (SD 17.3) for those never reporting tinnitus (data not shown) suggesting that tinnitus may be a marker of greater high-frequency hearing loss among this cohort.
Anecdotal reports from tinnitus sufferers indicate that use of hearing protection may increase the magnitude of tinnitus annoyance. While we have insufficient information regarding the impact of hearing protection on tinnitus-related annoyance, the severity or frequency of tinnitus, or degree of tinnitus-related annoyance among our study cohort, further and more detailed examination of this suggested association between tinnitus and injury risk is warranted.
This study has some limitations. We have no information regarding degree or severity of tinnitus for this cohort. Availability of such information could provide additional insight into the observed associations between tinnitus, high-frequency hearing loss, and injury risk. Second, although we have reported hearing protection device (HPD) use for a large portion of our cohort, we have no ability to discern HPD fit or usage patterns, which could impact the associations we report here. Finally, although we adjusted for physical job demand and included a random term for plant, and job within plant, to control for differences in plant-level and job-related injury risk unrelated to physical demand or noise exposure, unrecognized plant or job-level factors could influence the outcome reported here.
Despite the aforementioned limitations, this study has several important strengths. The large study cohort and breadth of available data precluded introduction of potential biases related to use of self-reported data. In addition, these data allowed us to adjust for several individual and job-level covariates known to increase injury risk in similar cohorts (Pollack et al, 2007; Taiwo et al, 2009; Kubo et al, 2013; Tessier-Sherman, 2014). Furthermore, use of generalized linear mixed modeling with random effects for plant, job within plant, and person within job, which allowed us to account for correlation resulting from clustering and repeated measures on persons, provides increased confidence in these reported results.
Conclusions
This study, in conjunction with previous reports, highlights the importance of reducing noise exposure through engineering controls regardless of the precise mechanism(s) through which noise exposure impacts injury risk. Moreover, these results underscore the importance of carefully examining the communication needs of hearing impaired workers and workers with tinnitus who are exposed to workplace noise. Finally, this work suggests that the relationship between tinnitus, hearing loss, and injury risk is deserving of further investigation.
Acknowledgments
This research was funded by grants from the National Institute on Aging (Disease, Disability and Death in an Aging Workforce, NIH/NIA, 1 R01 AG026291-06), National Institute for Occupational Safety and Health, (Assessing hearing conservation effectiveness, 1 R01 OH010132-01) and a contract with Alcoa Inc.
Footnotes
Competing Interests
Cantley, Galusha, Tessier-Sherman, Slade and Cullen receive a portion of their compensation at Yale and Stanford through a long-standing contractual agreement with Alcoa Inc. Dixon-Ernst was employed by Alcoa Inc. during the time this work was conducted.
Data Sharing
As an alternative to providing a de-identified data set to the public domain, we allow access for the purpose of re-analyses or appropriate “follow-on” analyses by any qualified investigator willing to sign a contractual covenant with the host institution, limiting use of data to a specific agreed upon purpose and observing the same restrictions as are limited in our contract with Alcoa, such as 60-day manuscript review for compliance purposes.
References
- Action on Hearing Loss – 2011 Report: Hearing Matters. http://www.actiononhearingloss.org.uk.
- Allman BL, Baizer JS, Salvi RJ, Lobarinas E. Special issue in Hearing Research: Neuroscience of tinnitus. Hearing Research. 2013;295(0):1–2. doi: 10.1016/j.heares.2012.11.012. [DOI] [PubMed] [Google Scholar]
- Amjad-Sardrudi H, Dormohammadi A, Golmohammadi R, Poorolajal J. Effect of Noise Exposure on Occupational Injuries: A Cross-sectional Study. J Res Health Sci. 2012;12(2):101–4. [PubMed] [Google Scholar]
- Arlinghaus A, Lombardi DA, Willetts JL, Folkard S, Christiani DC. A structural equation modeling approach to fatigue-related risk factors for occupational injury. Am J Epidemiol. 2012;176(7):597–607. doi: 10.1093/aje/kws219. [DOI] [PubMed] [Google Scholar]
- Cantley LF, Galusha D, Cullen MR, Dixon-Ernst C, Rabinowitz PM, Neitzel RL. Association between ambient noise exposure, hearing acuity and risk of acute occupational injury. Scand J Work Environ Health. 2014 doi: 10.5271/sjweh.3450. online first. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chau N, Bhattacherjee A, Kunar BM. Relationship between job, lifestyle, age and occupational injuries. Occupational Medicine. 2009;59(2):114–9. doi: 10.1093/occmed/kqp002. [DOI] [PubMed] [Google Scholar]
- Choi S-W, Peek-Asa C, Sprince NL, Rautiainen RH, Donham KJ, Flamme GA, et al. Hearing loss as a risk factor for agricultural injuries. Am J Ind Med. 2005;48(4):293–301. doi: 10.1002/ajim.20214. [DOI] [PubMed] [Google Scholar]
- Folmer RL, Griest SE. Tinnitus and insomnia. Am J Otolaryngol. 2000;21(5):287–93. doi: 10.1053/ajot.2000.9871. [DOI] [PubMed] [Google Scholar]
- Folmer RL, Griest SE, Meikle MB, Martin WH. Tinnitus severity, loudness, and depression. Otolaryngol Head Neck Surg. 1999;121(1):48–51. doi: 10.1016/S0194-5998(99)70123-3. [DOI] [PubMed] [Google Scholar]
- Girard SA, Leroux T, Courteau M, Picard M, Turcotte F, Richer O. Occupational noise exposure and noise-induced hearing loss are associated with work-related injuries leading to admission to hospital. Inj Prev. 2014 doi: 10.1136/injuryprev-2013-040828. Published Online First 17 March 2014. [DOI] [PubMed] [Google Scholar]
- Girard SA, Picard M, Davis AC, Simard M, Larocque R, Leroux T, et al. Multiple work-related accidents: tracing the role of hearing status and noise exposure. Occup Environ Med. 2009;66(5):319–24. doi: 10.1136/oem.2007.037713. [DOI] [PubMed] [Google Scholar]
- Hallam RS, McKenna L, Shurlock L. Tinnitus impairs cognitive efficiency. Int J Audiol. 2004;43(4):218–26. doi: 10.1080/14992020400050030. [DOI] [PubMed] [Google Scholar]
- Kubo J, Cullen MR, Cantley L, Slade M, Tessier-Sherman B, Taiwo O, et al. Piecewise exponential models to assess the influence of job-specific experience on the hazard of acute injury for hourly factory workers. BMC Med Res Methodol. 2013;13:89. doi: 10.1186/1471-2288-13-89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langguth B, Kleinjung T, Fischer B, Hajak G, Eichhammer P, Sand PG. Tinnitus severity, depression, and the big five personality traits. Prog Brain Res. 2007;166:221–5. doi: 10.1016/S0079-6123(07)66020-8. [DOI] [PubMed] [Google Scholar]
- Leigh JP. Economic burden of occupational injury and illness in the United States. Milbank Q. 2011;89(4):728–72. doi: 10.1111/j.1468-0009.2011.00648.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Margolis RH, Saly GL. Asymmetric hearing loss: definition, validation, and prevalence. Otol Neurotol. 2008;29(4):422–31. doi: 10.1097/MAO.0b013e31816c7c09. [DOI] [PubMed] [Google Scholar]
- Mattox DE. Assessment and Management of Tinnitus and Hearing Loss Continuum: Lifelong Learning in Neurology. Neuro-Otology. 2006;12(4):135–50. [Google Scholar]
- May JJ. Occupational hearing loss. Am J Ind Med. 2000;37(1):112–20. doi: 10.1002/(sici)1097-0274(200001)37:1<112::aid-ajim9>3.0.co;2-#. [DOI] [PubMed] [Google Scholar]
- Mazurek B, Olze H, Haupt H, Szczepek AJ. The more the worse: the grade of noise-induced hearing loss associates with the severity of tinnitus. Int J Environ Res Public Health. 2010;7(8):3071–9. doi: 10.3390/ijerph7083071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moll van Charante AW, Mulder PGH. Perceptual Acuity and the Risk of Industrial Accidents. Am J Epidemiol. 1990;131(4):652–63. doi: 10.1093/oxfordjournals.aje.a115549. [DOI] [PubMed] [Google Scholar]
- Nelson DI, Concha-Barrientos M, Driscoll T, Steenland K, Fingerhut M, Punnett L, et al. The global burden of selected occupational diseases and injury risks: Methodology and summary. Am J Ind Med. 2005;48(6):400–18. doi: 10.1002/ajim.20211. [DOI] [PubMed] [Google Scholar]
- Nia J, Bance M. Effects of varying unilateral conductive hearing losses on speech-in-noise discrimination: an experimental study with implications for surgical correction. Otol Neurotol. 2001;22(6):737–44. doi: 10.1097/00129492-200111000-00005. [DOI] [PubMed] [Google Scholar]
- Picard M, Girard SA, Simard M, Larocque R, Leroux T, Turcotte F. Association of work-related accidents with noise exposure in the workplace and noise-induced hearing loss based on the experience of some 240,000 person-years of observation. Accid Anal Prev. 2008;40(5):1644–52. doi: 10.1016/j.aap.2008.05.013. [DOI] [PubMed] [Google Scholar]
- Pollack KM, Agnew J, Slade MD, Cantley L, Taiwo O, Vegso S, et al. Use of employer administrative databases to identify systematic causes of injury in aluminum manufacturing. Am J Ind Med. 2007;50(9):676–86. doi: 10.1002/ajim.20493. [DOI] [PubMed] [Google Scholar]
- Rossiter S, Stevens C, Walker G. Tinnitus and its effect on working memory and attention. J Speech Lang Hear Res. 2006;49(1):150–60. doi: 10.1044/1092-4388(2006/012). [DOI] [PubMed] [Google Scholar]
- Sataloff RT, Sataloff J. Occupational Hearing Loss. 3. New York: Taylor and Francis; 1996. [Google Scholar]
- Souza K, Cantley LF, Slade MD, Eisen EA, Christiani D, Cullen MR. Individual and Plant Level Predictors of Acute, Traumatic Occupational Injuries in a Manufacturing Cohort. Occup Environ Med. doi: 10.1136/oemed-2013-101827. Published Online First: 12 April 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stroup W. Generalized Linear Mixed Models: Modern Concepts, Methods and Applications. Chapman and Hall/CRC Texts in Statistical Science. 2012 [Google Scholar]
- Taiwo OA, Cantley LF, Slade MD, Pollack KM, Vegso S, Fiellin MG, et al. Sex differences in injury patterns among workers in heavy manufacturing. Am J Epidemiol. 2009;169(2):161–6. doi: 10.1093/aje/kwn304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tessier-Sherman B, Cantley LF, Galusha D, Slade MD, Taiwo OA, Cullen MR. Occupational Injury by Sex in a Manufacturing Cohort. Occup Environ Med. 2014;71:605–610. doi: 10.1136/oemed-2014-102083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vetter RE, Symonds ML. Correlations between injury, training intensity, and physical and mental exhaustion among college athletes. J Strength Cond Res. 2010;24(3):587–96. doi: 10.1519/JSC.0b013e3181c7c2eb. [DOI] [PubMed] [Google Scholar]
- Ward W, Royster J, Royster L. Auditory and Non-Auditory Effects of Noise. In: Berger E, Royster L, Royster J, Driscoll D, Layne M, editors. The Noise Manual. 5. Fairfax, VA: American Industrial Hygiene Association; 2000. pp. 123–47. [Google Scholar]
- Wilkins PA, Action WI. Noise and accidents - a review. Ann Occup Hyg. 1982;25(3):249–60. doi: 10.1093/annhyg/25.3.249. [DOI] [PubMed] [Google Scholar]
- Yankaskas K. Prelude: Noise-induced tinnitus and hearing loss in the military. Hear Res. 2013;295:3–8. doi: 10.1016/j.heares.2012.04.016. [DOI] [PubMed] [Google Scholar]
- Yung A, Haagsma JA, Polinder S. A systematic review on the influence of pre-existing disability on sustaining injury. Accid Anal Prev. 2014;62(0):199–208. doi: 10.1016/j.aap.2013.09.024. [DOI] [PubMed] [Google Scholar]
- Zwerling C, Sprince NL, Wallace RB, Davis CS, Whitten PS, Heeringa SG. Risk factors for occupational injuries among older workers: an analysis of the health and retirement study. Am J Public Health. 1996;86(9):1306–9. doi: 10.2105/ajph.86.9.1306. [DOI] [PMC free article] [PubMed] [Google Scholar]