Abstract
Purpose
Postoperative nausea and vomiting (PONV) after spinal anesthesia for cesarean delivery are distressing to both patients and surgeons. This study was designed to evaluate the efficacy and safety of palonosetron and ramosetron (both newer and highly potent 5HT3 receptor antagonists) in nausea and vomiting in cesarean delivery after spinal anesthesia.
Methods
In this randomized, double-blind study, 109 women received either palonosetron (0.075 mg) or ramosetron (0.3 mg) intravenously immediately after clamping of the fetal umbilical cord. Nausea, vomiting, adverse events, and overall satisfaction were then observed for 48 h after administration of spinal anesthesia.
Results
A complete response (defined as no postoperative nausea and vomiting) during first 0–2 h postoperative after administration of spinal anesthesia was achieved in 85.5 % of patients with palonosetron and in 83.3 % of patients with ramosetron (p > 0.05). However, the corresponding incidence during 2 to 24 h was 70.9 and 53.7 %, respectively (p < 0.05), while it was 63.3 and 44.4 % at 24–48 h after anesthesia (p < 0.05). Along with a more complete response, the severity of nausea was also lesser with palonosetron during the corresponding study periods (2–24 and 24–48 h, respectively; p < 0.05). Patients who received palonosetron were also more satisfied than those who received ramosetron (p < 0.05). No difference in adverse events was observed in any of the groups.
Conclusion
To conclude, prophylactic therapy with palonosetron is more effective than prophylactic therapy with ramosetron for the long-term prevention of PONV after cesarean section.
Keywords: Anesthesia, Cesarean section, Palonosetron, Postoperative nausea and vomiting, Ramosetron, Spinal
Introduction
Postoperative nausea and vomiting (PONV) after spinal anesthesia in cesarean delivery are common [1] and the reported incidence is quite high [1, 2]. Furthermore, post-delivery PONV can complicate postoperative care in several ways like aspiration of vomitus, electrolyte disturbance and dehydration, delay of nutrition, fluid intake and oral drug therapy, and wound dehiscence due to frequent expulsive efforts, associated with delayed recovery and prolonged hospital stay [3]. For the prevention of PONV, selective serotonin 5-hydroxytryptamine type 3 (5-HT3) receptor antagonists are considered one of the first-line therapy because of their efficacy and fewer side-effects compared with other antiemetics [4], but most research has been on ondansetron [5].
Ramosetron is a recently developed selective 5-HT3 receptor antagonist. It exhibits significantly greater binding affinity for 5-HT3 receptors with a slower dissociation rate from receptor binding, resulting in more potent and longer receptor antagonizing effects compared with older 5-HT3 receptor antagonists [6].
Palonosetron is the first of “second-generation” 5-HT3 receptor antagonists and is superior to the “first generation” in respect of high receptor-binding affinity, and it may also bind to the receptor at an allosteric site different from those that bind ondansetron and granisetron [7, 8]. It has a prolonged mean elimination half-life of about 40 h.
Till date most of the studies have found palanosetron to be superior to than ramosetron for prevention of PONV, particularly long-term PONV (at 24 and 48 h after operation) [9–11]. However, a few studies have found ramosetron to be more effective for prevention of PONV compared to palonosetron [12, 13]. The latest 2014 consensus guidelines on PONV have concluded that though there are multiple randomized controlled trials on both these drugs, however these numbers are insufficient to conduct a viable meta-analysis comparison of these drugs (evidence category A, level 2) [4]. Furthermore, there are no data on either palonosetron or ramosetron regarding their use for preventing PONV in cesarean delivery in the Indian context, or from any other part of the world. This lacuna in knowledge compelled us to conduct the current study.
The primary objective of this prospective, randomized, double-blinded trial was to assess the relative efficacy of palonosetron and ramosetron for preventing PONV in patients undergoing spinal anesthesia for cesarean delivery. The secondary objectives were to assess the effects of the drugs both introperatively and postoperatively, including any adverse effects.
Methods
After ethical committee approval, 120 women (ASA 1 and 2) aged between 18 and 35 years undergoing elective cesarean delivery in the department of Obstetrics and Gynaecology, Medical College and Hospital, Kolkata were included in this study from June 2012 to January 2013. Women with history of motion sickness, history of emesis in post-delivery period, history of acid peptic diseases, body mass index >30 kg−1 m2 and those who had received antiemetic, steroid meditation 24 h before surgery, or having any contraindication to regional anesthesia were excluded from this study. Other exclusion criteria were any history of organic disease, patients on antihypertensives, insulin or antipsychotic, allergic to any of the drugs under study or 5-HT3 receptor antagonists in the past, any recent history of alcohol or drug abuse or any history of nausea/vomiting prior to administration drug (s) inside OT. All patients were clearly explained regarding the proposed study procedure and any queries they had regarding drugs, procedures or otherwise were answered, and thereafter informed verbal and written consent was obtained. All patients posted for operation fasted for 6 to 8 h, but were allowed sips of water till 2 h before operation.
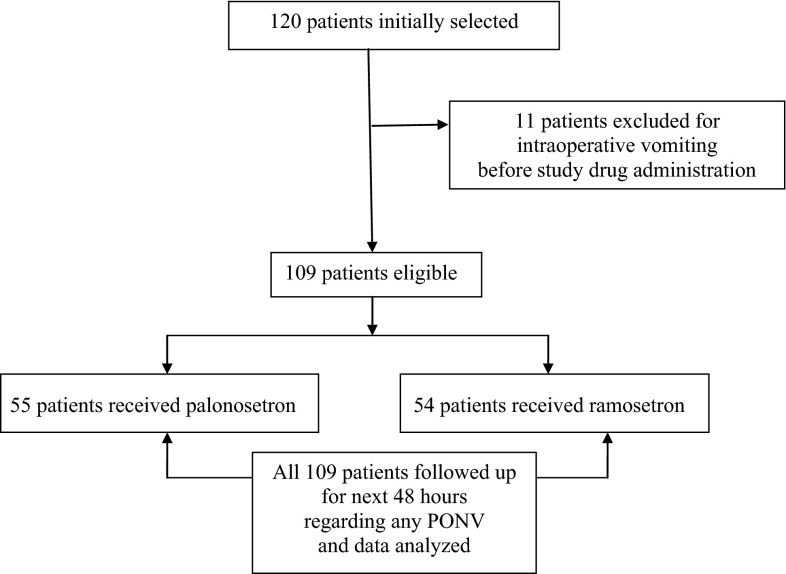
Of the 120 women initially selected, 11 patients were excluded as they vomited intraoperatively before drug administration. To limit fetal exposure, study drugs were given intravenously immediately after clamping of the umbilical cord. The 109 eligible women were randomly allocated, using a computer-generated random number table, followed by the allocation of these numbers in sealed envelope technique to receive intravenously one of two treatment regimens: Group P (no. = 55) received palonosetron 2 ml (0.075 mg, 1.5 ml, ThemisetTM; made 2 ml with 0.5 ml normal saline), while Group R (no. = 54) received ramosetron (0.3 mg, NoziaTM) in 2 ml solution. Study medications were prepared by personnel not involved in this study in individual 2 ml covered and coded syringes to ensure blinding to the anesthetists. All participating patients and investigators (trained nurses and anaesthesiologists) who collected post-delivery data were blinded to the study drug administered (Fig. 1).
Fig. 1.
Flowchart showing recruitment of study population and subsequent follow-up
Each woman was pre-loaded with 15 ml kg−1 of lactated Ringer’s solution before induction of spinal anesthesia. Baseline pulse rate, blood pressure, oxygen saturation of each women, and fetal heart rate were recorded before spinal anesthesia. Under all aseptic precaution, lumbar puncture was performed in sitting position using 25 gauge Whitacre type lumber puncture needle and 0.5 % hyperbaric bupivacaine 2 ml (10 mg) was injected intrathecally. Women were then placed supine for 5 min, thereafter a wedge was placed under right hip for left uterine displacement. Oxygen 3 L min−1 was administered via face mask. Patients were monitored during procedure by continuous ECG, NIBP and pulse oximetry. A decrease in systolic blood pressure >25 % of baseline values and/or less than 90 mm Hg after spinal injection was treated with additional intravenous fluids and/or phenylephrine 0.1 to 0.2 mg boluses intravenously, as indicated. Following confirmation of spinal block by loss of sensation to cold and pinprick at T4–5 level, surgery was started. Oxytocin 10 units was administered intramuscularly at the time of umbilical cord clamping, followed by 10 units in each running infusion bottle till end of operation. Patients in each group were allowed to receive fentanyl 1.5 mcg kg−1 intravenously, if required, for pain relief after delivery of the baby due to uterus exteriorization and/or peritoneum manipulation [14].
Nausea was defined as a subjectively unpleasant sensation associated with awareness of the urge to vomit; retching was defined as the labored, spasmodic rhythmic contraction of the respiratory muscles without the expulsion of gastric contents. Vomiting was defined as the forceful expulsion of gastric contents from mouth [1, 2, 4]. If two or more episodes of emesis occurred in each observation period, another rescue antiemetic (not belonging to the 5-HT3 receptor antagonist group, i.e., metoclopramide 10 mg) was given intravenously. We made no distinction between vomiting and retching for treatment purpose. All episodes of PONV (nausea, retching, and vomiting) were recorded by direct questioning by trained nurses blinded to the study group or by spontaneous complaint by the patients during three periods within the first 48 h after anesthesia: 0–2 h in the post-anesthetic care unit, 2–24 h in the postpartum ward and 24–48 h in the general ward. Nausea was scored on an 11-point verbal rating scale from 0 (no nausea) to 10 (worst possible nausea): severity was scored as mild (1–3), moderate (4–6), or severe (7–10) [10]. The details of any adverse effects were recorded during study period by the attending anesthesiologist and gynecologist.
Postoperative analgesia was provided with inj. diclofenac (aquous) 75 mg (1 ml) administered intramuscularly every 12 h and inj. paracetamol 1 g (100 ml) infusion given intravenously every 8 h for first 48 h after operation, starting when the patients first complained of pain. Time taken from giving spinal anesthesia to the first complaint of pain by the woman was taken as the duration of analgesia. No opioids were given for postoperative analgesia at any point of time. Patient satisfaction regarding their satisfaction to be free of nausea and vomiting was performed on a four-point Likert scale (dissatisfied, neutral, satisfied, highly satisfied) at the completion of the study [8].
Sample size was predetermined using a power analysis to achieve an 80 % chance (β = 0.2) of detecting a 40 % reduction in PONV from a basal incidence of 70 % (from 70 % to 42 %) with an assumed significance level of α = 0.05 [14]. A calculated minimum sample size was 49 patients in each group. Our minimum sample size was similar to other relevant studies who calculated similar outcome differences [8, 11]. A larger number of patients were included to allow for possible incomplete data collection or patient dropout. Statistical analysis was performed using SPSS for Windows (version 14, SPSS Inc., Chicago, IL, USA). Student’s t test or Mann–Whitney rank sum tests were used to compare the continuous variables among the groups. If a significant difference was noted, a Bonferroni multiple comparison test was used to determine intergroup differences. Categorical variables were analyzed using the χ2 test or Fisher’s exact test, as appropriate. A p value of < 0.05 was considered statistically significant.
Results
All 109 patients recruited for this study completed the trial. Patient profile and information on the surgery and operative management are summarized in Tables 1 and 2. These were comparable between the groups receiving either palonosetron or ramosetron (p < 0.05).
Table 1.
Maternal demographics
| Palonosetron (n = 55) | Ramosetron (n = 54) | ||
|---|---|---|---|
| Age (years) | 25.8 ± 3.4 | 26.2 ± 4.0 | |
| Weight (Kg) | 58.8 ± 7.2 | 59.1 ± 7.7 | |
| Multipara (no.) | 18 | 16 | |
| Non-smoker status | 55 | 54 | |
| ASAGrade | |||
| 1 | 45 | 46 | |
| 2 | 10 | 8 | |
| Baseline systolic blood pressure (mm of Hg) | 124.6 ± 8.1 | 127.5 ± 7.7 | |
No significant difference
Table 2.
Operative management
| Palonosetron (n = 55) | Ramosetron (n = 54) | |
|---|---|---|
| Duration of surgery (min) | 49.2 ± 8.4 | 48.5 ± 7.6 |
| Duration of anesthesia (min) | 60.5 ± 4.1 | 58.8 ± 3.9 |
| Uterus exteriorised (no.) | 51 | 49 |
| Duration of uterus exteriorized (min) | 16.1 ± 8.4 | 16.5 ± 7.7 |
| No. of patients requiring intraop. phenylephrine | 10 | 10 |
| No. of patients receiving intraoperative fentanyl | 18 | 17 |
| Mean intraoperative fentanyl consumption (mcg) per patient | 75.4 ± 24.1 | 80.9 ± 22.1 |
| Duration of analgesia (min) | 130.4 ± 20.8 | 135.6 ± 21.9 |
No significant difference
The treatment groups were comparable with regard to patient demographics and operative management. The incidence of a complete response (no PONV, no rescue) 0–2 h after anesthesia was 85.5 % with palonosetron and 83.3 % with ramosetron (p > 0.05); the corresponding incidence 2–24 h after anesthesia was 70.9 % and 53.7 % (p < 0.05); while the corresponding incidence 24–48 h after anesthesia was 63.3 and 44.4 %, respectively (p < 0.05). Thus, a complete response after cesarean section was more frequent in patients receiving palonosetron (p < 0.05). The severity of nausea was also lesser with palonosetron during the corresponding study periods (2–24 and 24–48 h, respectively; p < 0.05). Retching episodes were also more with ramosetron (48.1 vs. 29.1, p < 0.05). Patients who received palonosetron were more satisfied than those who received ramosetron (p < 0.05) (Table 3).
Table 3.
Comparison of frequency of all PONV episodes between study groups
| Palonosetron (n = 55) | Ramosetron (n = 54) | p value | |
|---|---|---|---|
| 0–2 h after spinal anesthesia | |||
| Complete response (no PONV) | 47 (85.5) | 45 (83.3) | 0.7 |
| Nausea severity (mild/moderate/severe) | 1/2/1 | 1/3/1 | 0.7 |
| Vomiting | 6 (10.9) | 7 (12.9) | 0.6 |
| 2–24 h after spinal anesthesia | |||
| Complete response (no PONV) | 39 (70.9) | 29 (53.7) | 0.02* |
| Nausea severity (mild/moderate/severe) | 2/3/3 | 8/10/5 | 0.01* |
| Vomiting | 10 (18.2) | 16 (29.6) | 0.04* |
| 24–48 h after spinal anesthesia | |||
| Complete response (no PONV) | 35 (63.3) | 24 (44.4) | 0.04* |
| Nausea severity | 3/4/3 | 7/8/3 | 0.01* |
| Vomiting | 14 (25.4) | 21 (38.6) | 0.02* |
| Use of rescue antiemetic (no. of patients) | 24 (43.6) | 30 (55.5) | 0.1 |
| Overall retching episodes | 16 (29.1) | 26 (48.1) | 0.04* |
| Overall Satisfaction (dissatisfied/neutral/satisfied//highly satisfied) | 14/10/20/7 | 20/16/12/7 | 0.03* |
* p < 0.05
Observed adverse events were headache, dizziness, constipation, and myalgia which were not clinically serious. No difference in the incidence of adverse effects was observed between the groups as shown in Table 4.
Table 4.
Adverse effects
| Palonosetron (n = 55) | Ramosetron (n = 54) | |
|---|---|---|
| 0–2 h after spinal anesthesia | ||
| Headache | 8 (14.5 %) | 7 (12.9 %) |
| Dizziness | 5 (9.1 %) | 3 (5.5 %) |
| Constipation | 0 | 0 |
| Myalgia | 1 (1.8 %) | 1 (1.8 %) |
| 2–24 h after spinal anesthesia | ||
| Headache | 7 (12.7 %) | 8 (14.8 %) |
| Dizziness | 3 (5.4 %) | 3 (5.5 %) |
| Constipation | 2 (3.6 %) | 2 (3.7 %) |
| Myalgia | 0 | 0 |
| 24–48 h after spinal anesthesia | ||
| Headache | 6 (10.9 %) | 5 (9.2 %) |
| Dizziness | 3 (5.4 %) | 3 (5.7 %) |
| Constipation | 4 (7.2 %) | 4 (7.4 %) |
| Myalgia | 0 | 0 |
Discussion
This single-center double-blind randomized control study showed that palanosetron was superior to ramosetron regarding control of PONV from 2nd postoperative hour till 2nd postoperative day after surgery with higher overall patient satisfaction.
Pregnancy is associated with more chances of aspiration than non-pregnant state. Increased gastric volume, delayed gastric emptying, and a reduction of lower esophageal sphincter tone are the underlying causes [15]. Nausea and vomiting during regional anesthesia for cesarean section are relatively high without prophylactic antimetic [1]. Nausea and vomiting like pain is a subjective response of the individual woman which can vary according to her inherent tolerance and also her surroundings in the perioperative period. The etiology of emetic symptoms following regional anesthesia for cesarean delivery is complex and depends on a variety of factors including maternal demographics, operative procedure, the occurrence of postoperative pain, use of perioperative opioids, and anesthetic techniques, peritoneal traction and exteriorisation of uterus [1, 2, 12]. Maternal hypotension after induction of spinal anesthesia is related to an increased incidence of intraoperative, post-delivery emetic episodes. This hypotension may trigger the vomiting center to induce emesis due to hypoxia [1, 2, 14]. In this study pre-loading, left uterine displacement, and administration of incremental doses of phenylephrine were performed for the prevention and early treatment of hypotension. The requirement of introperative phenylephrine use was similar. Furthermore, patients consumed similar amounts of intraoperative fentanyl (a short acting potent opioid) after delivery to curtail stimuli of post-delivery uterine manipulations [14]. No intravenous patient controlled analgesia (IV-PCA) of opioids was administered as this is an independent risk factor of PONV [10]. Instead we only gave non-opioids (diclofenac injections and paracetamol infusions) in the postoperative period as opioids are a known cause of PONV [5, 10]. As patient characteristics and surgical management were comparable, we inferred that the differences in subsequent incidences of PONV and complete response (no PONV, no rescue) can only be attributed to effectiveness of the study drugs [12].
The exact mechanism of palonosetron and ramosetron in the prevention of PONV is unknown, but these drugs may act by potently blocking 5-HT3 receptors sites at area postrema and the nucleus tractus solitarius [10, 11]. The doses of palonosetron and ramosetron were based on similar studies in the Indian context [6, 8, 9, 12] based on dose-ranging studies regarding optimal adult dose of ramosetron and palonosetron.
We could not find any report to compare the efficacy of palonosetron and ramosetron for preventing PONV in cesarean section. Our results demonstrate that the antiemetic efficacy of ramosetron is similar to that of palonosetron for preventing PONV during the first 2 h (0–2 h) after anesthesia and that palonosetron is more effective than ramosetron regarding a complete response (no PONV, no rescue) for the next 46 h (2–48 h). This is similar to various studies done to compare these drugs in a variety of abdominal procedures [10, 11]. This suggests that palonosetron is a more potent antiemetic. The exact reason for the difference in effectiveness between palonosetron and ramosetron is not known, but may be related to more potent affinities of 5-HT3 receptor antagonists [8]. However, one study has found similar effectiveness regarding PONV of these drugs at 0 to 48 h [9], while another study found ramosetron to be more effective in the first 72 h after operation [13]. The side-effects of headache, dizziness, constipation, and myalgia are common with 5-HT3 receptor antagonists and did not differ among groups, a finding similar to other randomized controlled studies [10, 11].
The greater efficacy of palonosetron may be attributable to the fact that the binding affinity to the 5-HT3 receptor is 30 times higher than that of either ondansetron or ramosetron and to the extended half-life of palonosetron (approximately 40 h) [10]. The possible mechanisms of palonosetron and ramosetron for preventing PONV are similar, but palonosetron is further differentiated from other 5-HT3 receptor antagonists including ramosetron, by interacting with the receptors in an allosteric and positively cooperative manner, and may promote internalization of the 5-HT3 receptor and decrease the function of the receptor [10, 11]. This may be explained by unique structural characteristics; while older drugs are based on a 3-substituted indole structure resembling serotonin, palonosetron is based on a fused tricyclic ring system attached to a quinuclidine moiety.
Our study suffered from several limitations. First, we did not include a placebo control group to evaluate the baseline incidence of PONV as we considered it unethical to withhold prophylactic antiemetic drugs in patients at high risk for PONV. Second, combination therapy has been shown to be more effective to treat or prevent PONV, especially in high-risk patients. For example, dexamethasone is frequently combined with another class of drug, such as metoclopramide or 5-HT3 antagonists for a more complete response [4, 5]. Third, we excluded patients with past history of PONV or motion sickness which are significant predictors of PONV. Fourth, we compared ramosetron and palonosetron based on the known optimal doses without knowledge of their equipotent doses. The manufacturer’s recommended doses in available adult formulations of ramosetron and palonosetron are 0.3 and 0.075 mg intravenous, respectively, and were chosen for this study. Also measurements of outcome were done at prefixed time intervals (0–2, 2–24, 24–48 h) rather than clinical endpoints like patient transfer, stay at recovery room, transfer to general wards, the presence of family, ambulation, and diet. Another limitation of our study was not to exclude patients receiving drugs intraoperatively for prophylaxis of postpartum hemorrhage e.g., carboprost or methylergometrine, which are associated with significant incidences of nausea and vomiting. However, as the antiemetic medication was given immediately after clamping of umbilical cord it can be assumed that there was already an antiemetic action in place when these emetogenic uterotonic medications are used after failure of oxytocin. However, none of our patients required any other uterotonic drugs apart from oxytocin. To be on the safe side, future studies may include use of any of these drugs intraoperatively as an exclusion criterion.
Our study could also be criticized because we used opioid analgesia (inj. fentanyl bolus intravenously) intraoperatively, a recognized cause of PONV [4, 5]. But there is an association between pain and PONV, and treating pain with opioids may relieve PONV [5]. Our study suffered from the limitation that pain intensity of the patients were not studied postoperatively, and only the duration of analgesia and requirement of analgesic was recorded along with overall patient satisfaction. Another limitation was that in view of the comparatively longer half-life of palonosetron, a multi-dose regime of ramosetron may have been more appropriate. But till date no study focused on this issue, and there may be opportunity for future research in this direction.
Both palonosetron and ramosetron are much more expensive than other available antiemetics in our set up (approximately Rupees 150 and 35, respectively, compared to Rupees 25 or less for ondansetron 4 mg). However, we should also consider the outcome of the patients and overall cost of care if emesis was to occur, as single doses of both palonosetron and ramosetron are effective for 48 h or more.
In conclusion, prophylactic therapy with palonosetron and ramosetron was both effective for prevention of post cesarean emesis for first 48 h. Palonosetron as an antiemetic was significantly superior to ramosetron with an overall better patient satisfaction.
Acknowledgments
Compliance with ethical requirements and conflict of interest
This study has been carried out in Medical College and Hospital, Kolkata after obtaining institutional informed consent on 18.7.11, followed by informed consent obtained from all patients included in this study. Suman Chattopadhyay and Sebanti Goswami declare that they have no conflict of interest.
Suman Chattopadhyay
has completed MBBS from N.R.S. Medical College, Kolkata in 1997 and MD from Utkal University, Bhubaneswar in 2002. He was an elected member of National Academy of Medical Sciences, New Delhi in 2009. Presently, he is posted as an Associate Professor of Anaesthesiology at Medical College & Hospital, Kolkata. He is an Editorial Board Member of Indian Journal of Pain, the Scientific Secretary of Indian Society for Study of Pain (West Bengal Branch), and an Executive Committee Member of ISSP (WB branch). He has 28 publications in national and 4 in international journals. He is the Chapter author of Textbook in Forensic Medicine and Editor of four books in Anaesthesiology and Pain. He is an invited speaker at various national, zonal, and state conferences and CMEs. He is the Organising Secretary of WBISSPCON 2010 and Scientific Secretary of RSACPCON2008, WBISACON 2008, ITTACS National Conference 2009, and ISAJAC 2010. He is the Joint Scientific Secretary of WBISACON 2011, 2012, and 2013
References
- 1.Dasgupta M, Biswas BN, Chatterjee S, et al. Randomised, placebo-controlled trial of granisetron for control of nausea and vomiting during caesarean delivery under spinal anaesthesia. J Obstet Gynecol India. 2012;62(4):419–423. doi: 10.1007/s13224-012-0291-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ghosh B, Chattopadhyay S, Naskar TK, et al. Antiemetic in caesarean section under spinal anaesthesia: new option. IOSR J Pharm Biol Sci. 2012;3(2):1–5. [Google Scholar]
- 3.Chandrakantan A, Glass PSA. Multimodal therapies for postoperative nausea and vomiting, and pain. Br J Anaesth. 2011;107(S1):i27–i40. doi: 10.1093/bja/aer358. [DOI] [PubMed] [Google Scholar]
- 4.Gan TJ, Diemunsch P, Habib AS, et al. Consensus guidelines for the management of postoperative nausea and vomiting. Anesth Analg. 2014;118:85–113. doi: 10.1213/ANE.0000000000000002. [DOI] [PubMed] [Google Scholar]
- 5.Chatterjee S, Rudra A, Sengupta S. Current concepts in the management of postoperative nausea and vomiting. Anesthesiol Res Pract. 2011;2011:748031. doi: 10.1155/2011/748031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ansari MM, Siddiqui OA, Haleem S, et al. Comparison of ramosetron and ondansetron for control of post-operative nausea and vomiting following laparoscopic cholecystectomy. Indian J Med Sci. 2010;64:272–280. doi: 10.4103/0019-5359.99606. [DOI] [PubMed] [Google Scholar]
- 7.Chun HR, Jeon IS, Park SY, et al. Efficacy of palonosetron for the prevention of postoperative nausea and vomiting: a randomized, double-blinded, placebo-controlled trial. Br J Anaesth. 2014;112(3):485–490. doi: 10.1093/bja/aet340. [DOI] [PubMed] [Google Scholar]
- 8.Laha B, Hazra A, Mallick S. Evaluation of antiemetic effect of intravenous palonosetron versus intravenous ondansetron in laparoscopic cholecystectomy: a randomized controlled trial. Indian J Pharmacol. 2013;45(1):24–29. doi: 10.4103/0253-7613.106430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Piplai G, Chakrabarty I, Mukhopadhyay M, et al. A comparative study between palonosetron and ramosetron to prevent postoperative nausea and vomiting after laparoscopic cholecystectomy. Int Res J Pharmacy Pharmacol. 2012;2(8):193–197. [Google Scholar]
- 10.Kim SH, Hong JY, Kim WO, et al. Palanosetron has superior prophylactic antiemetic efficacy compared with ondansetron or ramosetron in high-risk patients. Korean J Anesthesiol. 2013;64(6):517–523. doi: 10.4097/kjae.2013.64.6.517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Park SK, Cho EJ, Kang SH, et al. A randomized, double-blind study to evaluate the efficacy of ramosetron and palonosetron for prevention of postoperative nausea and vomiting after gynecological laparoscopic surgery. Korean J Anesthesiol. 2013;64(2):133–137. doi: 10.4097/kjae.2013.64.2.133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Swaika S, Pal A, Chatterjee S, et al. Ondansetron, ramosetron, or palonosetron: which is a better choice of antiemetic to prevent postoperative nausea and vomiting in patients undergoing laparoscopic cholecystectomy? Anesthesia. 2011;5(2):182–186. doi: 10.4103/0259-1162.94761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Roh GU, Yang SY, Shim JK, et al. Efficacy of palonosetron versus ramosetron on preventing opioid-based analgesia-related nausea and vomiting after lumbar spinal surgery: a prospective, randomized, and double-blind trial. Spine. 2014;39(9):E543–E549. doi: 10.1097/BRS.0000000000000236. [DOI] [PubMed] [Google Scholar]
- 14.Manullang TR, Viscomi CM, Pace NL. Intrathecal fentanyl is superior to intravenous ondansetron for the prevention of perioperative nausea during caesarean delivery with spinal anaesthesia. Anaesth Analg. 2000;90:1162–1166. doi: 10.1097/00000539-200005000-00030. [DOI] [PubMed] [Google Scholar]
- 15.Gaiser R. Physiologic changes in pregnancy. In: Chestnut DH, Polley LS, Tsen LC, Wong CA, editors. Chestnut’s Obstetric Anesthesia: Principles and Practice. 4. Philadelphia: Mosby Elsevier; 2009. pp. 15–36. [Google Scholar]