Abstract
Objectives
To review the limitations, major complications, and conversion rates associated with non-descent vaginal hysterectomy (NDVH); and develop a scoring system to predict the possibility of successful NDVH.
Methods
The risk analysis of conversion rates from vaginal to abdominal route while attempting NDVH was applied to formulate a scoring system for the assessment of successful NDVH. Parameters were selected based on Kovacs guidelines to determine the route of hysterectomy.
Results
From April 2005 to December 2008, NDVH was attempted in 364/1,378 women undergoing hysterectomy for benign conditions (Gp-I). Eight out of 364 cases (2.1 %) either had to be converted to the abdominal route or had major complication. Endometriosis and repeated sections had the highest risk. Scoring system was developed based on the risk analysis. Validity of this scoring system was tested in 1,177 women from January 2009 to September 2012 (Gp-II). 460 women with a score of 16 or less underwent NDVH successfully with a conversion rate of 0.2 %.
Conclusion
Careful assessment by a simple scoring system can help in deciding the feasibility of performing NDVH.
Keywords: Vaginal hysterectomy, Non-prolapsed uterus, Scoring system
Introduction
Hysterectomy is one of the common major gynecological operative procedures; however, the method of hysterectomy—vaginal, abdominal, or laparoscopic—was once a matter of controversy. Several studies have compared the abdominal and the vaginal routes of hysterectomy. The largest among them—the CREST study—included 1,856 women, who underwent non-emergency, non-radical hysterectomy between 1978 and 1981, with fewer complications in the vaginal hysterectomy (VH) group [1].
It is well established that the vaginal route is associated with fewer morbidities, lesser hospital stay, and better patient satisfaction; therefore, this method of hysterectomy should not be restricted to the conventional indication of uterovaginal prolapse [2, 3]. However, in the absence of a prolapse there are a few limitations to this method of hysterectomy which includes—a large uterine size, nulliparity, previous pelvic surgeries, LSCS or endometriosis, and ovarian masses. With the introduction of Laparoscopic assisted vaginal hysterectomy (LAVH) in the 1990s, the interest shifted to minimally invasive surgeries. Several studies since then have included LAVH in the comparison of hysterectomy routes. Johns et al. [4] reviewed 2,563 hysterectomies performed for non-malignant indications and they concluded that LAVH was safe with similar complication rates as abdominal or vaginal hysterectomy, and was superior to abdominal hysterectomy (AH).
It is well known that laparoscopic hysterectomy has its limitations—higher cost, expensive instruments, longer learning curve, and morbidities depending on the surgeon’s expertise; while the postoperative recovery is similar to VH. With increasing need to provide cost-effective quality, there is a need to review the limitations for non-descent vaginal hysterectomy (NDVH) and the feasibility of performing it without laparoscopic aid.
Aims and Objectives
The aim of this study was to review the limitations, major complications, and conversion rates associated with NDVH; and based on them to develop a scoring system for pre-surgical assessment of women undergoing hysterectomy for benign gynecological conditions. This scoring system would enable to grade women as having low, intermediate, or high risk for complications and/or conversion rates if subjected to VH, and thereby predict the feasibility to perform a successful NDVH.
Materials and Methods
This is a prospective study conducted in a tertiary referral center, from April 2005 to September 2012. In the initial phase of the study (from April 2005 to December 2008), a conscious effort was made to perform as many NDVH with or without salpingo-oophorectomy, in benign gynecological conditions. Normally considered contraindications to VH like large uterine size, nulliparity, mild-to-moderate endometriosis, previous pelvic surgery or Caesarean section, and simple adnexal mass <6 cm were also included in the study group (Group I). Uterine size of >18 weeks’ gestation, complex adnexal masses, severe endometriosis, immobile uterus, suspected or diagnosed malignancy, and women opting for the abdominal route were excluded from the study. Over this period of time, the rates of NDVH gradually increased from 9.6 % in 2005 to 46.7 % in 2008—but there were some major complications and conversions to the abdominal route. A detailed risk analysis for each of these cases was done. Based on this and Kovacs guidelines on determining the routes of hysterectomy [5], parameters were selected for a scoring system to predict the chances of a successful vaginal route of hysterectomy. The scoring system was applied for preoperative assessment from January 2009 to predict the feasibility of successful NDVH (Group II).
The following parameters were considered for formulating the scoring system [5]:
- Accessibility of the uterus transvaginally
- mobility
- vaginal breadth at apex
- uterine size >12 weeks’ gestation after morcellation
- Pathology not confined to uterus
- adnexal mass
- endometriosis
- Pelvic adhesions
- puckering of the post-vaginal wall at the cervicovaginal junction
- immobility of the uterus
- bladder adhesion due to repeated LSCS.
A score of 1–6 was given based on the minimum to maximum risk for conversion (Table 1).
Table 1.
Scoring system to determine the feasibility of NDVH
| Parameter | Score of 1 to 6 for minimum to maximum risk for conversion | |||
|---|---|---|---|---|
| Mobility of uterus | Mobile—1 | Restricted—6 | ||
| Narrow vagina | >2 finger—1 | <2 finger—6 | ||
| Uterine size | <12 weeks—1 | 12–16 w—2 | 16–18w—3 | Broad Uterus—6 |
| Endometriosis | Absent—1 | Mild—2 | Moderate—6 | |
| Removal of adnexa/mass | No—1 | Yes—2 | <6 cm-3 | >6 cm-6 |
| Post LSCS | None—1 | 1 PCSa—2 | 2 PCSa—6 | |
| Puckering of PODb | Absent—1 | Present—6 | ||
| Min score—7 | Safe score 7–11 | Mod risk of conversion—12 to 16 | High risk > 16 | |
aPost caesarean section
bPouch of douglaus
The accessibility of uterus transvaginally was reflected by the mobility of the uterus, laxity of the vagina (which can be affected by parity), and uterine size. Uterus with restricted mobility, narrow vagina < 2 finger width at the apex, and a very broad uterus (width > 12 cm in USG), extending laterally to the pelvic wall, in which volume-reducing techniques would be difficult was given a score of 6.
Pathology not confined to the uterus was assessed by the presence of endometriosis and need for removal of adnexa or adnexal masses, which can be associated with problems in placing the clamps over the infundibulopelvic ligaments. Endometriosis can be associated with distorted pelvic anatomy and adhesions. A score of 6 was allocated for moderate degree of endometriosis and need for removal of adnexal mass >6 cm in size.
Previous lower-segment Caesarean sections (LSCS) can lead to pelvic as well as bladder adhesions, the latter can predispose to bladder tear and this risk increases with the number of repeat sections. Previous two LSCS were given a score of 6.
Pelvic adhesions due to any cause, obliterating the cul-de-sac, maybe occasionally recognized by puckering or dimpling of the posterior vaginal vault at the cervicovaginal junction. In these patients, opening the posterior peritoneum may be difficult and likely to have complications if subjected to NDVH. This was given a score of 6.
The final and complete scoring is under anesthesia when the mobility of the uterus and the posterior pouch can be best assessed.
An uterine size of >18 weeks’ gestation, cervical fibroids, three or more previous LSCS, and severe endometriosis are beyond the scope of this scoring system.
All women undergoing hysterectomy for benign conditions from January 2009 to September 2012 were subjected to the scoring system—they formed the study group (Group II); and the outcome with respect to the major complications and/or conversions to the abdominal route was compared to the control group of women who had undergone NDVH prior to the application of the scoring system (Group I). However, a retrospective scoring based on medical records was done for all the cases in Group I.
Result and Analysis
During the initial phase of the study from April 2005 to December 2008, 1,379 women underwent hysterectomy for benign conditions. A total of 364 women during this period had been taken up for NDVH. Women with certain limiting factors such as previous pelvic surgeries or LSCS, uterine size greater than 16 weeks’ gestation, endometriosis, nulliparity, and simple ovarian masses ≤ 6 cm were also included in the study (Group I). During this period, the rates of NDVH gradually increased from 9.6 % (33/342) in 2005 to 47.1 % (173/368) in 2008.
However, there were some major complications or conversion rates in 8/364 women subjected to NDVH. Three had bladder tear, in four the posterior pouch could not be opened due to dense adhesions, and in one the uterus was >16 weeks’ gestation—very broad and could not be delivered vaginally. One woman required relaparotomy on the first postoperative day due to hemoperitoneum following NDVH with bilateral removal of adnexas (Table 2). (Although the latter was considered for risk analysis for vaginal adenexectomy, it was not taken as a failure for the surgical procedure for NDVH).
Table 2.
Complications and conversions in Group I (n = 364)
| Reason for failure | Number | Risk factor | No risk factor |
|---|---|---|---|
| Bladder tear | 3 | PCS-2 | 1 |
| Inability to open the POD | 4 | Endometriosis-3 Postsurgical-1 |
0 |
| Uterus could not be delivered | 1 | Size > 16 weeks’ gestation broad, could not be reduced | 0 |
| Laparotomy due to hemoperitoneum | Relaparotomy | Removal of bilateral adnexa | 0 |
One out of these eight complications was in the low-risk group, i.e., in women without any confounding factors for NDVH (n = 198), giving a complication or conversion rate of 0.5 %. On the other hand, seven of the women with various limiting factors (n = 166) had to be converted to the abdominal route or had a complication, giving a conversion/complication rate of 4.2 %. The overall failure rate for NDVH was 8/364 (2.1 %).
A risk analysis for the conversion of each of these confounding factors is mentioned below (Table 3). Endometriosis, previous repeat sections, and a broad large irreducible uterus were associated with high conversion rates. Clinically, they were reflected by restricted mobility of the uterus, dimpling of the posterior cervicovaginal junction, and the lateral bulk of the uterus. A non-prolapsed uterus that is broad and extends laterally to the pelvis may not allow a vaginal approach to the uterine arteries. On the other hand, a large but mobile uterus that does not extend to the pelvic sidewalls will allow the surgeon to easily clamp and ligate the uterine arteries, after which morcellation techniques can be easily accomplished. Many authors have suggested that the position and mobility of the uterus are more critical than only the size in deciding the route of approach [6].
Table 3.
Risk analysis for confounding factors
| Risk factor | n | Conversion | Relative risk | 95 % CI | Odds ratio |
|---|---|---|---|---|---|
| Previous LSCS | 22 | 2 | 4.4 | 1.2–15.6 | 3.6 |
| Endometriosis | 9 | 3 | 23.1 | 6.6–72.1 | 34.3 |
| Nulliparity | 4 | 0 | – | – | – |
| Previous pelvic surgery | 26 | 1 | 1.7 | 0.2–11.3 | 1.85 |
| Uterine size < 16 weeks’ | 20 | 1 | 2.3 | 0.3–15.1 | 2.4 |
| Need for adnextomy | 62 | 1 (relap) | 0.7 | 0.1–4.1 | 0.7 |
Based on the risk analysis and clinical parameters selected from Kovacs guidelines for deciding the route of hysterectomy, a scoring system was devised for easy clinical application to determine the best and safest route of hysterectomy.
A retrospective scoring based on previous clinical records of the 364 women in Group I showed 340 women to have a score of ≤11 with conversion in one case, 19 with a score between 12 and 16 with two conversions, and five with score >16 with conversion in all. The single conversion in the low-risk group had a score of 7 (no confounding factor for NDVH). The lowest score with conversion in women with confounding factors for NDVH was 12, so this was taken as the lower limit for moderate risk. On the other hand, successful NDVH was possible only till a score of 16, which was taken as the outer limit of intermediate risk for conversion. Thus, a score of 11 or less was taken as low risk, between 12 and 16 was taken as intermediate risk, and >16 was taken as high risk for conversion. The huge differences in the two probabilities of conversion 0.2 % in the low-risk group and 100 % in the high-risk group indicate the ability of the scoring system to identify the high-risk cases for conversion in an effective manner. A score of ≥12 as a predictor of risk had a sensitivity of 87.5 %, specificity of 95.2 %, PPV of 29.2 %, and NPV of 99.7 %.
The scoring system was applied for pre-surgical assessment of 1,177 women undergoing hysterectomy for benign conditions from January 2009 (Group II) for deciding the route of hysterectomy. 456 women with a score of ≤11 (low risk) and five patients with a score of 12–16 (intermediate risk) were subjected to NDVH with only one conversion in the intermediate risk due to pelvic adhesions in a case of unsuspected endometriosis.
The rate of NDVH prior to application of the scoring system (Group I) was 356/1,378 (25.8 %) and the rate subsequent to the application was 460/1,177 (39.8 %) (Group II). The conversion rate decreased from 8/364 (2.1 %) to 1/461 (0.2 %) (p = 0.013 Fisher’s exact test, 95 % CI 0.004–0.035) and visceral injury while attempting NDVH from four (3 bladder tear and 1 gut injury) to none.
Discussion
Evidence supports that VH is superior; it also supports the use of AH only when documented pathologic conditions preclude the vaginal route [5–9]. Conventional limiting factors for NDVH need to be addressed, because in most of the cases it can be overcome and hysterectomy can be completed by the vaginal route. It is, therefore, important to individualize the approach for each patient rather than rely on a single technique.
The proponents of laparoscopic surgery claim to overcome the limitations of VH with laparoscopic assistance and convert a potential abdominal to vaginal route of hysterectomy. However, advantage of LAVH or total laparoscopic hysterectomy (TLH) has not been established over NDVH. Whereas laparoscopic hysterectomy is associated with increased cost and morbidities related to surgeon’s expertise and learning curve, the surgical outcome is similar to NDVH. A Cochrane Review [10] concluded that VH is far superior compared to the other techniques and has the best outcomes; however, when VH is not possible, laparoscopic hysterectomy has advantages over AH.
We believe that there is a little need for laparoscopy during NDVH, and we use it infrequently during this procedure. However, we do not wish to understate the role of laparoscopy—its use in specific instances can certainly avoid laparotomy or help determine when an abdominal route of hysterectomy is more appropriate.
The complications and conversion rates in our study were similar 9/825 (1.1 %) to other studies, as were the need for conversions [11–13]. In the study by Paparella et al, laparoscopy was used prior to conversion to the abdominal route. They reported a reduction in the conversion rate by only 1 % with laparoscopic assistance [13].
Pre-surgical assessment of our cases with a simple scoring system helped us to classify women needing hysterectomy for benign conditions into low-, intermediate-, and high-risk group. Women having a low risk (≤11) can be safely subjected to NDVH; whereas women with a high risk (≥17) should be offered abdominal hysterectomy. Women with a score of 12–16 need further assessment. If the uterine size is >12 weeks’ gestation and the pathology confined to the uterus—possibility of morcellation techniques needs to be assessed for successful NDVH. When the pathology is not confined to the uterus alone, laparoscopic evaluation should be done to assess if the pathology is appropriate for laparoscopic resection. If laparoscopic surgery is indicated, it is beneficial to convert to a VH as early as possible in the procedure. Several studies have suggested that nothing is gained by continuing the laparoscopic dissection once a vaginal hysterectomy can be performed safely, since it only prolongs surgery, increases costs, and increases the risk of morbidity [14].
Thus, the application of a scoring system, which was simple, easy, reproducible, and did not involve any extra cost to the patient, helped in objectively classifying women into low-, intermediate-, and high-risk groups for complications if subjected to NDVH. This was of great help while counseling women on the method of hysterectomy being selected for them as well as the probability of risk for complications and conversion to AH, for a better informed consent when opting for VH.
The algorithm and parameters for selecting the optimal route of hysterectomy are essentially based on Kovacs guidelines for determining the route of hysterectomy [5, 7]. This study further objectively quantified it with a scoring system for easy application and decision making (Fig. 1).
Fig. 1.
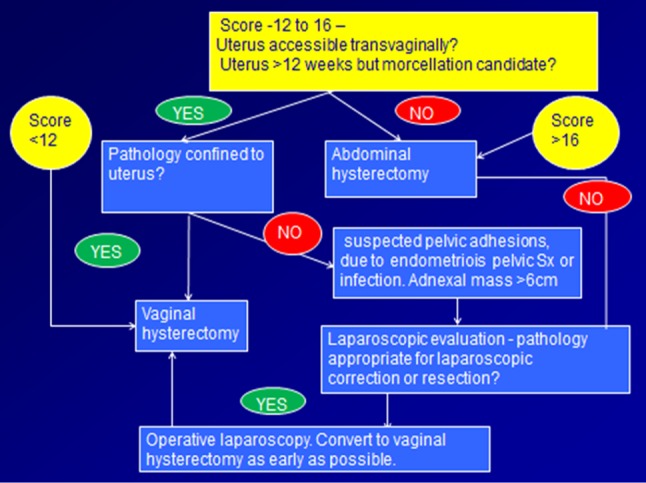
Algorithm for deciding the optimal route and method of hysterectomy [5, 7]
Conclusion
Female pelvic organs have two portals of entry: one vaginal which is the natural orifice and the other surgically created—abdominal. The vaginal approach is the hallmark of the gynecological surgeon [15].
The route of hysterectomy gynecologists choose should not only benefit the patient but also represent a wise use of health care resources. There is no debate that abdominal hysterectomy or laparoscopy should be performed for severe disease. However, opting for other methods of hysterectomy without assessing patients for NDVH is like opting for LSCS in all pregnant women without giving them a fair chance for vaginal delivery [15].
In this study, assessment of women requiring hysterectomy for benign conditions by a scoring system helped in deciding the feasibility to perform NDVH and/or the need for laparoscopy, where indicated. Application of this scoring system significantly decreased the complication rates from 2.1 to 0.2 % in women being subjected to this method of hysterectomy.
Acknowledgments
Compliance with ethical requirements and Conflict of interest
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008. Informed consent was obtained from all patients for being included in this study. Dr. Alokananda Ray, Dr. Luna Pant and Dr. Navneet Magon declare that they have no conflict of interest.
Dr. Alokananda Ray
is a specialist in the Department of OBGYN in Tata Main Hospital, Jamshedpur. She has completed her MBBS from NRS Medical College; MD in OBGYN from IPGMER, Kolkata; and Fellowship in Maternal Fetal Medicine from National University Hospital, Singapore. She served the local OBGYN society in Jamshedpur as secretary from 2001 to 2006 and as CME secretary during 2007–08, and is currently holding the post of President since 2012. She involved in Post graduate training programmes for the Diplomat of National Board. She has special interest in Fetal Medicine, Emergency Obstetrics, Medical disorders in pregnancy, and VH; and has several presentations, publications, and awards to her merit. She is also the peer reviewer for the International Journal of Gynaecology, Obstetrics and Neonatal care as well as the AOGD newsletter and Journal, New Delhi
Contributor Information
Alokananda Ray, Email: alokanandaray@yahoo.com.
Luna Pant, Email: lunapant@yahoo.co.in.
Navneet Magon, Email: navneetmagon@gmail.com.
References
- 1.Dicker RC, Greenspan JR, Strauss LT, et al. Complications of abdominal and vaginal hysterectomy among women of reproductive age in the United States. Am J Obstet Gynecol. 1982;144:841–848. doi: 10.1016/0002-9378(82)90362-3. [DOI] [PubMed] [Google Scholar]
- 2.Ray A, Pant L, Balsara R, et al. Nondescent vaginal hysterectomy—a constantly improving surgical art. J Obstet and Gynecol India. 2011;61(2):182–188. doi: 10.1007/s13224-011-0021-z. [DOI] [Google Scholar]
- 3.Sheth SS. The scope of vaginal hysterectomy. Eur J Obstet Gynecol Repod Biol. 2004;115(2):224–230. doi: 10.1016/j.ejogrb.2004.02.016. [DOI] [PubMed] [Google Scholar]
- 4.Johns DA, Carrera B, Jones J, et al. The medical and economic impact of laparoscopic-assisted vaginal hysterectomy in a large, metropolitan, not-for-profit hospital. Am J Obstet Gynecol. 1995;172:1709–19. [DOI] [PubMed]
- 5.Kovac SR. Guidelines to determine route of hysterectomy. Obstet Gynecol. 1995;85:18–23. doi: 10.1016/0029-7844(94)00318-8. [DOI] [PubMed] [Google Scholar]
- 6.McCracken Geoff, Lefebvre Guylaine G. Vaginal hysterctomy: dispelling the myths. J Obstet Gynaecol Can. 2007;29(5):424–428. doi: 10.1016/S1701-2163(16)35494-9. [DOI] [PubMed] [Google Scholar]
- 7.Cardosi RJ, Hoffman MS. Determinimg the best route for hysterectomy. OBG Manag. 2002;14(7):31–38. [Google Scholar]
- 8.Saha R, Shrestha NS, Thapa M, et al. Non Descent Vaginal hysterectomy—safety and feasibility. NJOG. 2012;7(2):14–16. [Google Scholar]
- 9.Kovac SR. Abdominal versus vagianl hysterectomy: a statistical model for determining physician decision making and patient outcome. Med Decis Mak. 1991;11:19–28. doi: 10.1177/0272989X9101100103. [DOI] [PubMed] [Google Scholar]
- 10.Nieboer TE, Johnson N, Lethaby A et al. Surgical approach to hysterectomy for benign gynecological disease. Cochrane Database Syst Rev. 2009; 3. CD003677. [DOI] [PubMed]
- 11.Dewan R, Agarwal S, Manisha et al. Non-descent vaginal hysterectomy—an experience. J Obstet Gynaecol India. 2004; 54:376–8.
- 12.Ottosen C, Lingman G, Ottosen L. Three methods of hysterectomy: a randomized, prospective study of short term outcome. BJOG. 2000;107:1380–1385. doi: 10.1111/j.1471-0528.2000.tb11652.x. [DOI] [PubMed] [Google Scholar]
- 13.Paparella P, Sizzi O, Rossetti A, et al. Vaginal hysterectomy in generally considered contraindications to vaginal surgery. Arch Gynecol Obstet. 2004;270:104–109. doi: 10.1007/s00404-003-0505-x. [DOI] [PubMed] [Google Scholar]
- 14.American College of Obstetricians and Gynecologists ACOG committee opinion No. 444: choosing the route of hysterectomy for benign disease. Obstet Gynecol. 2009;114:1156–1158. doi: 10.1097/AOG.0b013e3181c33c72. [DOI] [PubMed] [Google Scholar]
- 15.Sheth Shirish S, Paghdiwalla Kurush P, Hajari Anju R. Vaginal route: a gynaecological route for much more than hysterectomy. Best Prac Res Clin Obstet Gynaecol. 2011;25:115–132. doi: 10.1016/j.bpobgyn.2010.12.005. [DOI] [PubMed] [Google Scholar]


