Abstract
This study aimed to introduce a novel mini-open pedicle screw fixation technique via Wiltse approach, and compared it with the traditional posterior open method. A total of 72 cases of single-segment thoracolumbar fractures without neurologic injury underwent pedicle screw fixation via two different approaches. Among them, 37 patients were treated using posterior open surgery, and 35 patients received mini-open operation via Wiltse approach. Crew placement accuracy rate, operative time, blood loss, postoperative drainage, postoperative hospitalization time, radiation exposure time, postoperative improvement in R value, Cobb's angle and visual analog scale (VAS) scores of the two methods were compared. There were no significant differences in the accuracy rate of pedicle screw placement, radiation exposure and postoperative R value and Cobb's angle improvement between the two groups. However, the mini-open method had obvious advantages over the conventional open method in operative time, blood loss, postoperative drainage, postoperative hospitalization time, and postoperative improvement in VAS. The mini-open pedicle screw technique could be applied in treatment of single-segment thoracolumbar fracture without neurologic injury and had advantages of less tissue trauma, short operative and rehabilitative time on the premise of guaranteed accuracy rate and no increased radiation exposure.
Keywords: thoracolumbar fracture, pedicle screw, Mini-open, Wiltse approach, minimally invasive
Introduction
The thoracolumbar spine is one of the most common areas for spinal fractures[1],[2]. For treatment of cases with neurological injuries, internal fixation after decompression has been widely accepted. The choice of treatment in the absence of a neurological deficit depends on the Thoracolumbar Injury Classification and Severity Score (TLICS) scores[3],[4]. However, for patients with thoracolumbar biomechanical changes as a result of a certain degree of spinal deformity, low back pain and even neurological symptoms may occur over time, which may seriously jeopardize their work and daily life. Therefore, some scholars advocate early surgical treatment, even for stable thoracolumbar fractures (TLICS: score ≤ 3)[5],[6].
In the conventional open posterior pedicle screw fixation with posterior midline incision, detachment of the paraspinal muscles may be required to reduce soft tissue ischemia, alleviate dysfunction of the paraspinal muscles and relieve chronic pain[7]-[10]. In addition, this open approach may be disadvantaged by prolonged operative time, increased intraoperative bleeding and delayed functional rehabilitation[11]. All these problems appear to defeat our original intention of surgical treatment. With the advantage of no paraspinal muscle stripping, the percutaneous pedicle screw placement technique is attracting increasing attention as it brings a multitude of benefits including less bleeding, lower infection risk, lower incidence of postoperative pain, shorter rehabilitative time and reduced hospitalization time[12]-[20]. It is also worth mentioning that the incidences of both postoperative intractable low back pain and muscle atrophy are also significantly reduced12,16,[21]-[24].
Although percutaneous pedicle screw fixation is a mature technique, it still requires specialized equipments and long learning curve[25] before implementation. High incidence of screw malposition[26],[27] and large doses of radiation exposure[28],[29] have caused a sluggish evolution.
In this study, we described a novel mini-open pedicle screw fixation technique via Wiltse approach for single-segment thoracolumbar fractures and compared the reliability and safety of this approach with the conventional posterior open method.
Patients and methods
Patients
The clinical data of 72 cases of single-segment thoracolumbar fractures without neurologic injury were reviewed. Among them, 35 cases (21 males and 14 females) from the mini-open group underwent pedicle screw internal fixation via Wiltse approach. Thirty-seven cases (23 males and 14 females) received conventional open surgeries via the posterior midline approach. The inclusion criteria were as follows: patients with single-segment thoracolumbar vertebral fractures classified as A1, A2, A3 or B1 type according to the AO classification, aged from 16 to 65 years, patients had fresh fractures and were treated surgically within 10 days after the injury, TLICS score ≥ 4 and load-sharing score < 7. The exclusion criteria were as follows: patients with neurological injury, spinal anatomical variations or vertebral deformity, a history of neurological dysfunction or mental illness, significant surgical contraindications, osteoporosis [dual-energy X-ray absorptiometry (DEXA) examination, T value ≤ -2.5], and patients who refused to sign informed consent.
Surgical methods
For the conventional posterior open approach, we firstly performed a posterior midline incision at the target segment and striped the paraspinal muscle along the spinous process and the vertebral lamina. Then, the facet joints and roots of the transverse process were exposed by an automatic retractor. The entry point was determined based on anatomical landmarks according to the AO method.
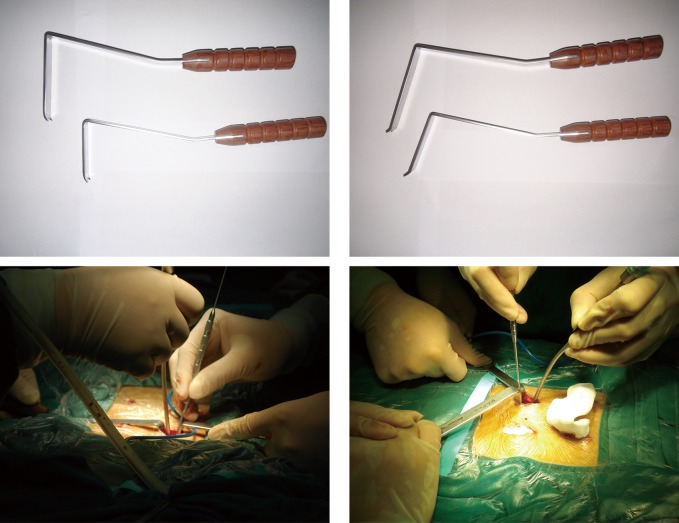
For pedicle screw internal fixation via Wiltse approach, body positioning and anesthesia were performed the same as for patients receiving the conventional posterior open approach. Manipulative reduction was performed to correct the kyphosis of the fractured vertebral body before routine sterilization. Positions of four small incisions were accurately determined by the locator and C-arm (Fig. 1A). Then, dissection was performed till the outer edge of the facet joints was reached through the intermuscular plane between the multifidus and the longissimus muscles after four 1.5-2.0-centimeter-long incisions were made (Fig. 1B). With the help of mini-retractor designed by ourselves, the pedicle entry point was exposed clearly (Fig. 2). The determination of the entry point was also based on the anatomical landmarks using the same method as the conventional open group. The guide wire was inserted perpendicular to the corresponding supraspinal ligament[30], and then C-arm was performed to check whether the guide wire was in the pedicle before pedicle screw placement. If the guide wire was in a satisfactory position, the pedicle screw could be inserted; otherwise, position of the guide wire should be adjusted. Likewise, after the procedure of rod installation and distraction for restoration, positions of pedicle screws and height of the fractured vertebraewere confirmed using C-arm again.
Fig. 1. Location of four small incisions.
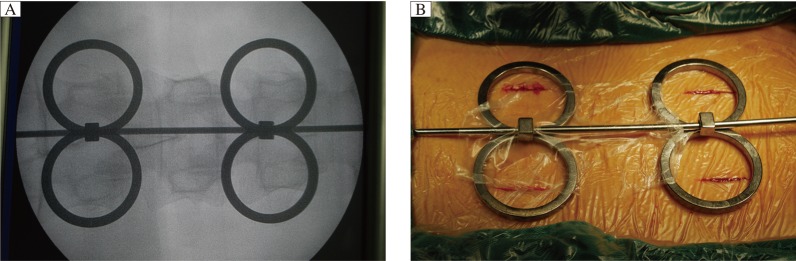
A: Four small incisions can be accurately determined by the locator and C-arm. B: Four 1.5-2.0-centimeter-long incisions are made with reference to the locator.
Fig. 2. Self-designed mini-retractor.
With the help of the mini-retractor, the pedicle entry point is exposed clearly and the determination of the entry point is based on the anatomical landmarks using the same method as in the conventional open group.
Study parameters
The study parameters included operative time from the first skin incision to skin suture, estimated blood loss, postoperative drainage, postoperative hospital stays, X-ray exposure time, which was automatically accumulated by C-arm machine, R value, Cobb's angle, visual analog scale (VAS) scores, postoperative complications, and accuracy rate of screws. Blood loss was carefully measured by weighing the sponges and determining the volume of shed blood in the suction bottle. The volume of postoperative drainage was estimated by weighing wound dressings in the mini-open group as drainage tube placement was not required and was estimated by blood volume in the drainage bag and wound dressings in the open group. Hospital stay was calculated from the first postoperative day to the discharge day. R value was determined by the following formula:
The mean height of the fractured vertebral body/the mean height of upper and lower adjacent vertebral bodies × 100%
Cobb's angle was delineated on lateral radiographs as the angle of the vertical line to the upper endplate of the upper adjacent vertebral body and lower endplate of the lower adjacent vertebral body. VAS was evaluated preoperatively, three days and one week postoperatively. Positions of pedicle screws were assessed by a single-blinded, independent and board-certified spine surgeon according to postoperative CT scans within one week after surgery. Screw which was extrapedicular or breached the front edge of the vertebral body, inferior or superior endplate was regarded as a failure.
Statistical analysis
All continuous data were presented as mean ± standard deviation (SD) and all categorical data as percentages or numbers. Statistical analyses for comparisons between groups were performed using the unpaired Student's t-test, χ2 test, or non-parametric Kruskal-Wallis test. P < 0.05 was considered statistically significant. Statistical analysis was done using SPSS 20.0 (SPSS, Chicago, IL, USA).
Results
Accuracy rate of pedicle screw placement
Among all the pedicle screws, both groups required no intraoperative adjustment. No complications such as spinal cord, nerve root or blood vessel injuries occurred. In the open group, according to postoperative CT image, two screws broke through the medial cortex of the pedicle; two broke through the lateral cortex; one broke through the front cortex of the vertebral body. No screw broke through vertebral endplates. The accuracy rate of pedicle screw placement was 96.6%. In the mini-open group: five pedicle screws broke through the lateral cortex of pedicle; one broke through the front cortex of the vertebral body; no screw broke through the vertebral endplate. The accuracy rate was 95.7%. There was no significant difference in the accuracy rate of pedicle screw placement between the two groups (Table 1).
Table 1. Patient data and clinical outcomes in two groups (mean±SD).
| The open group (n = 37) | The mini-open group (n = 35) | P | |
| Age (years) | 38.4±20.2 | 41.2±16.6 | 0.524 |
| Sex (male/female) | 23/14 | 21/14 | 0.851 |
| T11/ T12/ L1/ L2 | 6/11/13/7 | 6/10/11/8 | 0.973 |
| Total screws placed(successes/failure) | 148(143/5) | 140(134/6) | 0.688 |
| Fluoroscopy time (seconds) | 9.2±2.1 | 9.6±2.2 | 0.430 |
| Operative time (minutes) | 95.0±23.2 | 82.5±20.4 | 0.018 |
| Blood loss (mL) | 144.8±56.6 | 34.5±13.4 | <0.001 |
| Postoperative drainage (mL) | 77.9±37.3 | 11.9±5.4 | <0.001 |
| Postoperative hospital stay (days) | 9.1±1.8 | 3.4±1.2 | <0.001 |
Surgical outcomes
There were significant differences in operative time (P = 0.018), blood loss (P < 0.001), postoperative drainage (P < 0.001) and postoperative hospitalization time (P < 0.001) between the two groups (Table 1). The results showed that the mini-open method had obvious advantages in these aspects compared with the conventional open method. There were no significant differences in R value and Cobb's angle between the two groups before and after surgery (P > 0.05, Table 2). But in either group, operation brought significant improvement compared with preoperative data (P < 0.001, Table 3). No significant differences were found in improvement of R value and Cobb's angle between the two groups (P > 0.05, Table 2).
Table 2. Comparison of R value and Cobb's angle between the two groups (mean±SD).
| Parameter | The open group | The mini-open group | P | |
| Preoperative | R value | 58.5 ± 8.4 | 56.9 ± 10.2 | 0.48 |
| Cobb's angle | 29.5° ± 5.8° | 30.9° ± 6.4° | 0.33 | |
| Postoperative | R value | 93.54 ± 4.4 | 92.8 ± 4.8 | 0.52 |
| Cobb's angle | 5.6° ± 3.0° | 5.9° ± 3.6° | 0.31 | |
| Improvement | R value | 35.07 ± 7.69 | 35.93 ± 10.87 | 0.72 |
| Cobb's angle | 23.91 ± 6.41 | 25.07 ± 7.69 | 0.49 |
Table 3. Comparison between preoperative and postoperative R value and Cobb's angle in the two groups (mean±SD).
| Group | Preoperative | Postoperative | P | |
| The open group | R value | 58.5 ± 8.4 | 93.54 ± 4.4 | < 0.001 |
| Cobb's angle | 29.5° ± 5.8° | 5.6° ± 3.0° | < 0.001 | |
| The mini-open group | R value | 56.9 ± 10.2 | 92.8 ± 4.8 | < 0.001 |
| Cobb's angle | 30.9° ± 6.4° | 5.9° ± 3.6° | < 0.001 |
Preoperative VAS for the two groups showed no significant difference (P > 0.05). In general, VAS for both groups showed significant improvement compared with preoperative value (P < 0.01). However, the degree of this improvement between the two groups was not the same. The results showed that the mini-open method had greater improvement in VAS scores at postoperative day 3 and 7 (P < 0.01) than the open approach (Table 4).
Table 4. VAS scores of the two groups (mean±SD).
| Group | Preoperative date | Postoperative day 3 | Postoperative day 7 |
| The open group | 8.1 ± 1.0 | 4.8 ± 1.2a | 2.3 ± 1.5b |
| The mini-open group | 8.2 ± 1.1 | 1.8 ± 1.1a | 1.0 ± 0.8b |
| P | 0.66 | < 0.001 | < 0.001 |
Compared with Preoperative VAS, there were significant differences (P < 0.01);
Compared with VAS of three days after surgery, there were significant differences (P < 0.01).
Discussion
In 1968, Wiltse[31] first described the paraspinal sacrospinalis-splitting approach between the multifidus and the longissimus which was associated with less bleeding and tissue dissection compared with the single midline incision approach[32]-[34]. Drawbacks including extensive stripping of the paraspinal muscle, electrical-burn damage from electric knife and prolonged mechanical compression by automatic retractor could be effectively avoided in the procedure of entry point exposure through the mini-open method via Wiltse approach. The mini-open approach had rapid recovery with slight pain and markedly shorter hospitalization time compared with the traditional open approach. All patients from the mini-open group were mobile with the protection of the waist brace 24 hours after surgery and discharged after an average of 3.4 days postoperatively. However, for those patients who underwent the open surgery, the drainage tubes were removed on postoperative day 2, the mean postoperative hospital stay was 9.1 days, and activity was permitted at least two weeks after surgery.
The conventional open method had advantage over the mini-open technique in exposure of pedicle screw entry point based on clear anatomical landmarks. However, the operation time in the open group was prolonged, which may be due to more soft tissue dissection and skin suture. Smooth surgical procedure of the mini-open group was another important reason. Four small incisions were rapidly located by the locator with few X-ray exposure (Fig. 1A); Two separated blunt hook teeth of the retractor which were confirmed suitable for varied local bone structures played an important role in preventing muscles slipping away (Fig. 2). Aimed by the self-designed retractor, the entry point could also be easily exposed and determined based on the anatomical landmarks identical to the open approach. With intact coverage of the sarcolemma, muscle creep could be effectively avoided in muscle dissection if only the approach was strictly along the muscle gap. Especially for segments of L4 and L5, muscle gaps were absolutely clear and the sarcolemmas were relatively hypertrophic[35].
Radiation exposure in pedicle screw placement has always been the focus of attention, and the risk of long-term low-doses X-ray remains unclear[29]. In our research, determination of pedicle screw entry point in the two groups both required C-arm assistance. For the reason given above, there was no obvious difference in X-ray exposure (9.2 ± 2.1 seconds for the open group vs. 9.6 ± 2.2 seconds for the mini-open group) between the two groups. Namely, the mini-open approach did not increase radiation exposure in the operation.
The mini-open technique is similar to the open method in restoration of vertebral body height, improvement of Cobb's angle and accuracy rate of screw placement. There were no cases of spinal cord, nerve or vessel injury in both groups. Study limitations included lack of long-term follow-up in such as postoperative loss of the vertebral height. However, the only distinction between the two groups was the surgical approach. In aspects of fixation method and pedicle screw type, the two techniques were the same. Therefore, we can infer that the mini-open approach was similar to the open method in postoperative loss of vertebral height in long-term follow-up.
The biggest current limitation of the mini-open approach is that it is not suitable for posterior laminectomy and posterolateral fusion. Therefore, the inclusion criteria was strictly limited to cases of single segment thoracolumbar vertebral fractures classified as A1, A2, A3 or B1 type according to AO classification. Additionally, the patient's load-sharing score (spinal load scoring system) must be less than seven points to ensure the security of only posterior fixation for thoracolumbar fractures. Narrow indication is the drawback of this technique.
In conclusion, compared with the traditional open posterior surgery, the mini-open surgery via Wiltse approach has the following advantages on the premise of no increased radiation exposure, less bleeding, shorter operative time, less postoperative pain and tissue trauma, and shorter rehabilitative and hospitalization time. Therefore, it is reliable in treating cases of thoracolumbar fractures without neurological damage.
Acknowledgments
This work was supported by the National Natural Science Foundation of China (Grant No. 30973058, 81171694, and 81371968); the Program for Development of Innovative Research Team in the First Affiliated Hospital of NJMU (No. IRT-015), and A Project Funded by the Priority Academic Program Development of Jiangsu Higher Education Institutions. This study was approved by Ethical Committee of the First Affiliated Hospital of Nanjing Medical University. The clinicltrails.gov number is “ChiCTR-OCC-10001133”, and written informed consent were obtained from all patients.
Reference
- 1.Gertzbein SD.Spine update. Classification of thoracic and lumbar fractures. Spine (Phila Pa 1976) 199419(5), 626–628. [DOI] [PubMed] [Google Scholar]
- 2.Magerl F, Aebi M, Gertzbein SD, et al. A comprehensive classification of thoracic and lumbar injuries. Eur Spine J 19943(4), 184–201. [DOI] [PubMed] [Google Scholar]
- 3.Vaccaro AR, Zeiller SC, Hulbert RJ, et al. The thoracolumbar injury severity score: a proposed treatment algorithm. J Spinal Disord Tech 200518(3), 209–215. [PubMed] [Google Scholar]
- 4.Vaccaro AR, Lehman RA, Jr, Hurlbert RJ, et al. A new classification of thoracolumbar injuries: the importance of injury morphology, the integrity of the posterior ligamentous complex, and neurologic status. Spine (Phila Pa 1976) 200530(20), 2325–2333. [DOI] [PubMed] [Google Scholar]
- 5.Domenicucci M, Preite R, Ramieri A, et al. Thoracolumbar fractures without neurosurgical involvement: surgical or conservative treatment? J Neurosurg Sci 199640(1), 1–10. [PubMed] [Google Scholar]
- 6.Siebenga J, Leferink VJ, Segers MJ, et al. Treatment of traumatic thoracolumbar spine fractures: a multicenter prospective randomized study of operative versus nonsurgical treatment. Spine (Phila Pa 1976) 200631(25), 2881–2890. [DOI] [PubMed] [Google Scholar]
- 7.Kawaguchi Y, Yabuki S, Styf J, et al. Back muscle injury after posterior lumbar spine surgery. Topographic evaluation of intramuscular pressure and blood flow in the porcine back muscle during surgery. Spine (Phila Pa 1976) 199621(22), 2683–2688. [DOI] [PubMed] [Google Scholar]
- 8.Kawaguchi Y, Matsui H, Tsuji H.Back muscle injury after posterior lumbar spine surgery. A histologic and enzymatic analysis. Spine (Phila Pa 1976) 199621(8), 941–944. [DOI] [PubMed] [Google Scholar]
- 9.Sihvonen T, Herno A, Paljarvi L, et al. Local denervation atrophy of paraspinal muscles in postoperative failed back syndrome. Spine (Phila Pa 1976) 199318(5), 575–581. [DOI] [PubMed] [Google Scholar]
- 10.Styf JR, Willen J.The effects of external compression by three different retractors on pressure in the erector spine muscles during and after posterior lumbar spine surgery in humans. Spine (Phila Pa 1976) 199823(3), 354–358. [DOI] [PubMed] [Google Scholar]
- 11.Kim DH, Vaccaro AR.Osteoporotic compression fractures of the spine; current options and considerations for treatment. Spine J 20066(5), 479–487. [DOI] [PubMed] [Google Scholar]
- 12.Kim DY, Lee SH, Chung SK, et al. Comparison of multifidus muscle atrophy and trunk extension muscle strength: percutaneous versus open pedicle screw fixation. Spine (Phila Pa 1976) 200530(1), 123–129. [PubMed] [Google Scholar]
- 13.Court C, Vincent C.Percutaneous fixation of thoracolumbar fractures: current concepts. Orthop Traumatol Surg Res 201298(8), 900–909. [DOI] [PubMed] [Google Scholar]
- 14.Cox JB, Yang M, Jacob RP, et al. Temporary percutaneous pedicle screw fixation for treatment of thoracolumbar injuries in young adults. J Neurol Surg A Cent Eur Neurosurg 201374(1), 7–11. [DOI] [PubMed] [Google Scholar]
- 15.Ma YQ, Li XL, Dong J, et al. [Comparison of percutaneous versus open monosegment instrumentation in the treatment of incomplete thoracolumbar burst fracture]. Zhonghua Yi Xue Za Zhi 201292(13), 904–908. [PubMed] [Google Scholar]
- 16.Song HP, Lu JW, Liu H, et al. Case-control studies between two methods of minimally invasive surgery and traditional open operation for thoracolumbar fractures. Zhongguo Gu Shang 201225(4), 313–316..(in Chinese) [PubMed] [Google Scholar]
- 17.De Iure F, Cappuccio M, Paderni S, et al. Minimal invasive percutaneous fixation of thoracic and lumbar spine fractures. Minim Invasive Surg. 2012;2012:141032. doi: 10.1155/2012/141032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Palmisani M, Gasbarrini A, Brodano GB, et al. Minimally invasive percutaneous fixation in the treatment of thoracic and lumbar spine fractures. Eur Spine J 200918( Suppl 1), 71–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yang WE, Ng ZX, Koh KM, et al. Percutaneous pedicle screw fixation for thoracolumbar burst fracture: a Singapore experience. Singapore Med J 201253(9), 577–581. [PubMed] [Google Scholar]
- 20.Fang LM, Zhang YJ, Zhang J, et al. Minimally invasive percutaneous pedicle screw fixation for the treatment of thoracolumbar fractures and posterior ligamentous complex injuries. Beijing Da Xue Xue Bao 201244(6), 851–854..(in Chinese) [PubMed] [Google Scholar]
- 21.Zhang ZC, Sun TS, Liu Z, et al. [Minimally invasive percutanuous cannulated pedicle screw system fixation for the treatment of thoracolumbar flexion-distraction fracture without neurologic impairment]. Zhongguo Gu Shang 201124(10), 802–805..(in Chinese) [PubMed] [Google Scholar]
- 22.Rampersaud YR, Annand N, Dekutoski MB.Use of minimally invasive surgical techniques in the management of thoracolumbar trauma: current concepts. Spine (Phila Pa 1976) 200631(11 Suppl), S96–102; discussion S104. [DOI] [PubMed] [Google Scholar]
- 23.Chen Z, Zhao JQ, Fu JW, et al. Modified minimally invasive percutaneous pedicle screws osteosynthesis for the treatment of thoracolumbar fracture without neural impairment. Zhonghua Yi Xue Za Zhi 201090(21), 1491–1493..(in Chinese) [PubMed] [Google Scholar]
- 24.Luo P, Xu LF, Ni WF, et al. Therapeutic effects and complications of percutaneous pedicle screw fixation for thoracolumbar fractures. Zhonghua Wai Ke Za Zhi 201149(2), 130–134..(in Chinese) [DOI] [PubMed] [Google Scholar]
- 25.Garfin SR, Fardon DF.Emerging technologies in spine surgery. Spine J 20022(20), 1–4. [DOI] [PubMed] [Google Scholar]
- 26.Ringel F, Stoffel M, Stuer C, et al. Minimally invasive transmuscular pedicle screw fixation of the thoracic and lumbar spine. Neurosurgery 200659(4 Suppl 2), ONS361–366; discussion ONS366–367. [DOI] [PubMed] [Google Scholar]
- 27.Schizas C, Michel J, Kosmopoulos V, et al. Computer tomography assessment of pedicle screw insertion in percutaneous posterior transpedicular stabilization. Eur Spine J 200716(5), 613–617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Perisinakis K, Theocharopoulos N, Damilakis J, et al. Estimation of patient dose and associated radiogenic risks from fluoroscopically guided pedicle screw insertion. Spine (Phila Pa 1976) 200429(14), 1555–1560. [DOI] [PubMed] [Google Scholar]
- 29.Rampersaud YR, Foley KT, Shen AC, et al. Radiation exposure to the spine surgeon during fluoroscopically assisted pedicle screw insertion. Spine (Phila Pa 1976) 200025(20), 2637–2645. [DOI] [PubMed] [Google Scholar]
- 30.Li J, Zhao H, Xie H, et al. A new free-hand pedicle screw placement technique with reference to the supraspinal ligament. J Biomed Res 201428(1), 64–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wiltse LL, Bateman JG, Hutchinson RH, et al. The paraspinal sacrospinalis-splitting approach to the lumbar spine. J Bone Joint Surg Am 196850(5), 919–926. [PubMed] [Google Scholar]
- 32.Wiltse LL, Spencer CW.New uses and refinements of the paraspinal approach to the lumbar spine. Spine (Phila Pa 1976) 198813(6), 696–706. [PubMed] [Google Scholar]
- 33.Olivier E, Beldame J, Ould Slimane M, et al. Comparison between one midline cutaneous incision and two lateral incisions in the lumbar paraspinal approach by Wiltse: a cadaver study. Surg Radiol Anat 200628(5), 494–497. [DOI] [PubMed] [Google Scholar]
- 34.Wiltse LL.The paraspinal sacrospinalis-splitting approach to the lumbar spine. Clin Orthop Relat Res 1973(91), 48–57. [DOI] [PubMed] [Google Scholar]
- 35.Vialle R, Wicart P, Drain O, et al. The Wiltse paraspinal approach to the lumbar spine revisited: an anatomic study. Clin Orthop Relat Res. 2006;445:175–180. doi: 10.1097/01.blo.0000203466.20314.2a. [DOI] [PubMed] [Google Scholar]