Abstract
Background: There are conflicting findings regarding long- and short-term effects of income on health. Whereas higher average income is associated with better health, there is evidence that health behaviours worsen in the short-term following income receipt. Prior studies revealing such negative short-term effects of income receipt focus on specific subpopulations and examine a limited set of health outcomes.
Methods: The United States Earned Income Tax Credit (EITC) is an income supplement tied to work, and is the largest poverty reduction programme in the USA. We utilize the fact that EITC recipients typically receive large cash transfers in the months of February, March and April, in order to examine associated changes in health outcomes that can fluctuate on a monthly basis. We examine associations with 30 outcomes in the categories of diet, food security, health behaviours, cardiovascular biomarkers, metabolic biomarkers and infection and immunity among 6925 individuals from the U.S. National Health and Nutrition Survey. Our research design approximates a natural experiment, since whether individuals were sampled during treatment or non-treatment months is independent of social, demographic and health characteristics that do not vary with time.
Results: There are both beneficial and detrimental short-term impacts of income receipt. Although there are detrimental impacts on metabolic factors among women, most other impacts are beneficial, including those for food security, smoking and trying to lose weight.
Conclusions: The short-term impacts of EITC income receipt are not universally health promoting, but on balance there are more health benefits than detriments.
Keywords: Income, public policy, biomarkers, health behaviours, socioeconomic, tobacco
Key Messages.
Although higher average income is generally associated with better health, the majority of evidence suggests that health related behaviours worsen in the short term following income receipt.
We utilize the fact that in-work tax credit recipients in the USA receive large cash transfers in the months of February, March and April, as a natural experiment.
In the months when cash transfers occurred, about one-third of the health-related outcomes examined differ as compared with those of eligible individuals in control months.
Eligible individuals in the disbursement months had less food insecurity, less smoking or exposure to smoke and were more likely to be trying to lose weight.
Compared with prior work that examined specific subpopulations of individuals or only substance use outcomes, our findings show on balance beneficial impacts of income receipt on health-related outcomes in individuals in households with dependent children.
Background
Existing research on income and health reveals an apparent puzzle. Having a higher level of income has long been shown to be associated with better health outcomes and behaviours.1,2 In contrast, income receipt, conceptually distinct from income itself, has been shown to increase some unhealthy behaviours and mortality. Focusing on income receipt and using multiple identification strategies, studies have documented higher rates of substance use, drug-related hospitalizations, and mortality in the days and weeks following disbursement of government transfers and wage payments from the military.3–7 These findings raise concerns about potential unintended negative short-term health consequences of income transfers. However, existing studies have focused on a small range of health outcomes, emphasizing negative health behaviours (e.g. substance use) while leaving other relevant health outcomes untested. Behavioural and psychological responses to income are complex and it is reasonable that income receipt effects may vary for different health outcomes. In addition, most prior studies have been limited to specific subpopulations, such as individuals in the military or older individuals,6 and these results may not generalize to broader populations.
To present a more comprehensive examination of short-term health consequences of income receipt, we analyse data from the U.S. National Health and Nutrition Examination Survey (NHANES) and examine 30 health-related outcomes that fluctuate over short periods of time (i.e. less than 1 month) in the categories of diet, food security, health behaviours, cardiovascular biomarkers, metabolic biomarkers, and infection and immunity. Our analytical strategy takes a natural experiment approach. It utilizes the fact that in the USA, recipients of the Earned Income Tax Credit (EITC) typically receive lump sum payments in February, March and April, following the processing of federal and state income taxes. Over 80% of individuals who qualify for the EITC actually receive the credit.8 Because the NHANES study surveys individuals throughout the year, we can measure a ‘treatment’ group of EITC-eligible individuals who were surveyed in February, March or April and a ‘comparison’ group of EITC-eligible individuals who were surveyed in May through January. The benefit for inference is that the month in which an individual is surveyed is random with respect to individual characteristics. To account for temporal trends in health outcomes unrelated to income receipt, we can further compare EITC-ineligible individuals who were surveyed in February, March or April vs May through January. This analytical strategy, a Difference-in-Difference approach, overcomes many of the common confounding problems that arise in analyses of income receipt and health, since many of the unmeasured individual-level characteristics that may jointly determine income receipt and health are unlikely to have seasonal variations that differ between EITC-eligible individuals and non-EITC-eligible individuals.
The EITC is an in-work tax credit. Since the EITC is the largest anti-poverty programme in the USA,8 this analysis also helps illuminate the health consequences of a major piece of US social welfare policy, with potential relevance to other in-work tax refund policies in other industrialized countries.9 There is a developing body of work that has examined the effects of the EITC in the USA, and of similar types of in-work tax credits in other countries, on health and development outcomes.10–13 Our work builds on this prior work by focusing specifically on the effects of income receipt, rather than on income more generally. This study, focusing on short-term fluctuations in health, captures health consequences of a time-delimited cash transfer that occurs in particular months.14
Methods
Data and analytical sample
Data for our analysis were from the U.S. Third National Health and Nutrition Examination Survey (NHANES III), which was designed to be representative of the non-institutionalized population of the USA.15 These data were collected as a cross-sectional study from 1988–94. Since the EITC is much more generous for individuals with dependents, we restricted our sample to respondents between the ages of 21 and 50 years (n = 10 022) because this age group is most likely to have children in the household who are aged 18 years or under. There were less than 3% of participants missing any specific outcome: we excluded 672 individuals who were missing data on any of the outcomes examined. We also excluded from our analysis respondents living in the Mid-Western and North-Eastern United States because these regions did not have year-round data collection, due to snowfall in winter. The remaining population of individuals from the Western and Southern United States numbered 6925. Of these 6925 individuals, 1689 (24%) were measured in the ‘treatment’ months of February through April, 2225 (32%) qualified for some EITC and 870 (13%) qualified for at least $1000 (in year-2000 dollars) of EITC. There were 167 women who qualified for at least $1000 of EITC in the treatment months, and 392 women who qualified for any EITC in the treatment months. There were 111 men who qualified for at least $1000 of EITC in the treatment months, and 276 men who qualified for any EITC in the treatment months.
The Earned Income Tax Credit exposure
Estimated eligibility and predicted amounts of federal EITC credit were calculated for each household, based on the following characteristics: (i) earned income; (ii) number of dependent children; and (iii) year. Earned income was self-reported for the household. Number of dependent children was not directly reported, but was calculated based on the total number of related persons living in a household, subtracting two if the respondent was cohabitating/married, and subtracting one if the household was single-headed. We then predicted EITC amounts using the National Bureau of Economic Research’s TAXSIM programme,16 which calculates exact qualifying values of the EITC using federal and state income tax code. This form of exposure results in an intent-to-treat interpretation of model coefficients. Because moderate-to-large income transfers are more likely to be consequential for health, we defined an EITC-eligible household as one eligible for $1000 (in year-2000 dollars) or more in EITC benefits. The $1000 cut-point was chosen as a relatively large credit, but not so high a level that there would only be a small population receiving the credit. As a secondary analysis, we examined the population eligible for any EITC credit. Our hypothesis was that there will be greater magnitudes of association with outcomes for those who are eligible for greater amounts of EITC dollars.
Health outcomes
The choice of outcomes was done a priori, based on the following criteria: (i) factor available in NHANES III; (ii) factor shown in the literature to be associated with health; and (iii) factor that can vary within a 1-month period based on environmental changes. We examined an overall diet measure using the Healthy Eating Index (ranging from 1 to 100) created by the U.S. Centers for Disease Control, as well as specific measures of intake of vegetables, fruit, meat, dairy, sodium, saturated fat and variety of foods (each ranging from 1 to 10).17–19 Food insecurity was assessed with two validated questions.20 The first question captured how many days in the past month a family had no food or was unable to buy food, and the second assessed whether this was because of insufficient money, food stamps or vouchers. We dichotomized this count as 0 days or at least 1 day. For the behaviours we examined: self-report of current smoking (yes or no); self-report of trying to lose weight (yes or no); cotinine (a continuous biomarker assessing exposure to second-hand smoke and individual smoking); self-reported marijuana smoking (any days in the past month); percent of kCal from alcohol (derived from self-report of alcohol consumption in the past 3 days) and a self-report of the number of days in the past month on which the participant walked a mile (dichotomized as less than 4, or 4 or more).15 For cardiovascular biomarkers we examined: systolic blood pressure; diastolic blood pressure; and forced expiratory volume.21 For metabolic biomarkers we examined: high-density lipoprotein (HDL) cholesterol; low-density lipoprotein (LDL) cholesterol; trigylcerides; haemoglobin (Hb) A1c and plasma glucose.21 For infection and immunity we examined: C-reactive protein; fibrinogen; lymphocytes; self-report of respiratory illness in the past 4 weeks; and self-report of cold or flu episodes in the past 4 weeks.21 To facilitate interpretation and comparison with previous studies focusing on negative health behaviours, all the outcomes are coded so that higher values indicate a negative (i.e. worsening) health indicator/behaviour.
Statistical model
The difference-in-difference approach was specified as:
Treatment months indicates that the respondents’ measurements were taken in February–April. EITC qualified indicates qualification for >= $1000 of EITC. β3 reflects differences in health between the treatment and the comparison group. All analyses are done stratified by gender, due to literature suggesting different health-related associations with income by gender22,23 and differences in household structure of male and female EITC recipients.24 To correct for the sample design of the NHANES,25 all the results are weighted and adjusted for clustering using the survey package in R.26 When presenting results, continuous outcomes are expressed in terms of Z-scores to facilitate comparisons across coefficients. Using the survey package in R to implement a generalized linear approach, we modelled dichotomous outcomes with a binomial model with the logit link function, and continuous outcomes with a Gaussian error distribution with the identity link function.
Prior work suggests that standard asymptotic assumptions of error distribution for difference-in-difference models with small numbers of treatment groups may underestimate the true variance.27 To address this, we perform additional robustness checks by creating nine placebo treatment groups based on all possible adjacent 3-month combinations between May and January (i.e. non-treatment months), and fit models with each of these 3-month groups as a placebo treatment. We will have increased confidence in our primary analysis if the coefficients from each of the nine placebo treatment groups are closer to the null than the coefficient from our actual treatment group.
Results
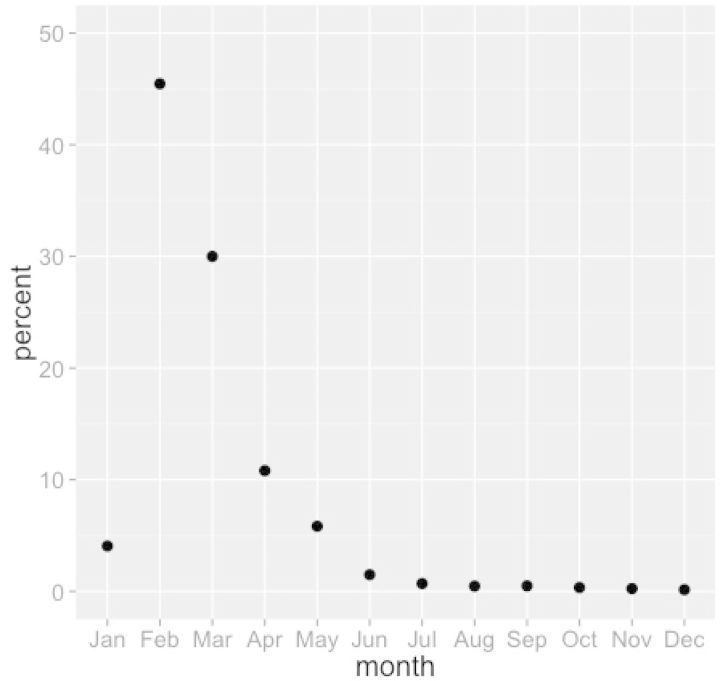
Figure 1 presents data on how EITC is distributed by month in the US population, showing February, March and April as the months when most households receive their credit.
Figure 1.
Distribution of Earned Income Tax Credit Disbursement by month. Authors’ calculation from Monthly U.S. Treasury Receipt Data.
Table 1 presents the racial/ethnic and educational distribution of the population who did not qualify for a minimum of $1000 in EITC as compared with those who did in the treatment months (February–April) and the control months (May–January), by gender. Among both men and women, non-Whites and respondents with lower education were overrepresented among those qualifying for at least $1000 in EITC. This differential distribution motivates the need for quasi-experimental approaches to examine impacts of EITC disbursement. The identical distribution of characteristics between those surveyed in the treatment as compared with the control months suggests random distributions of these characteristics throughout the year.
Table 1.
Percentages (and standard deviation) of not eligible for $1000 or more EITC vs qualifiers by treatment and control month, stratified by gender, NHANES III
| Women |
Men |
|||||
|---|---|---|---|---|---|---|
| Not eligible | EITC eligible |
Not eligible | EITC eligible |
|||
| Feb–Apr | May–Jan | Feb–Apr | May–Jan | |||
| (n = 3012) | (n = 167) | (n = 392) | (n = 2967) | (n = 111) | (n = 276) | |
| Race | ||||||
| White | 72 (0.44) | 42 (0.46) | 42 (0.49) | 71 (0.45) | 42 (0.42) | 42 (0.49) |
| Black | 12 (0.32) | 28 (0.45) | 28 (0.45) | 12 (0.32) | 26 (0.38) | 26 (0.44) |
| Mexican American | 7.0 (0.26) | 13 (0.48) | 13 (0.34) | 8.5 (0.28) | 21 (0.50) | 21 (0.40) |
| Other | 9.2 (0.29) | 17 (0.23) | 17 (0.37) | 8.6 (0.28) | 12 (0.48) | 12 (0.33) |
| Education | ||||||
| <High school | 16 (0.36) | 41 (0.50) | 41 (0.49) | 19 (0.40) | 52 (0.48) | 52 (0.50) |
| High school diploma | 36 (0.48) | 41 (0.46) | 41 (0.49) | 32 (0.47) | 31 (0.40) | 31 (0.46) |
| Some college | 48 (0.50) | 17 (0.37) | 17 (0.38) | 49 (0.50) | 17 (0.36) | 17 (0.38) |
Supplementary Figure 1 (available as Supplementary data at IJE online) shows the distribution of annual income for individuals qualifying for at least $1000 of EITC in the middle, those qualifying for less than $1000 but more than zero on the left and those who do not qualify for any EITC on the right. Because the EITC is targeted at low-wage workers, the income distribution for qualifiers is much more restricted than for non-qualifiers. Table 2 presents means (continuous measures), percentages (dichotomized measures) and standard deviations for the 30 health outcomes examined among those who did not qualify for a minimum of $1000 in EITC as compared with those who did, in the treatment months (February–April) and the control months (May–January), by gender.
Table 2.
Means (or proportions) and standard deviation of risk factors, by gender, NHANES III (n = 6925)
| Women |
Men |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Not eligible | EITC eligible |
Not eligible | EITC eligible |
|||||||||
| Feb–Apr | May–Jan | Feb–Apr | May–Jan | |||||||||
| (n = 3012) | (n = 167) | (n = 392) | (n = 2967) | (n = 111) | (n = 276) | |||||||
| Diet | ||||||||||||
| Overall diet | 62.7 | 12.2 | 59.5 | 10.5 | 60.7 | 11.9 | 60.9 | 12.0 | 59.7 | 11.9 | 58.6 | 11.1 |
| Vegetables | 5.98 | 3.45 | 5.21 | 3.55 | 5.20 | 3.44 | 5.97 | 3.38 | 5.71 | 3.37 | 5.39 | 3.57 |
| Fruit | 3.35 | 3.78 | 2.35 | 3.45 | 2.70 | 3.52 | 2.64 | 3.37 | 3.17 | 3.74 | 2.00 | 3.27 |
| Meat | 6.76 | 3.09 | 7.24 | 2.79 | 6.78 | 3.04 | 7.97 | 2.73 | 8.26 | 2.73 | 8.23 | 2.69 |
| Dairy | 6.13 | 3.67 | 5.66 | 3.74 | 5.52 | 3.84 | 6.76 | 3.61 | 6.47 | 3.83 | 5.62 | 4.02 |
| Sodium | 6.62 | 3.68 | 6.58 | 3.79 | 7.05 | 3.64 | 4.01 | 4.03 | 4.39 | 4.19 | 4.00 | 4.11 |
| Saturated fat | 6.19 | 3.96 | 5.92 | 4.12 | 6.44 | 3.92 | 6.31 | 3.87 | 6.49 | 3.82 | 6.82 | 3.72 |
| Diet variety | 7.54 | 3.29 | 6.50 | 3.60 | 6.67 | 3.59 | 7.98 | 2.93 | 7.53 | 3.23 | 7.26 | 3.35 |
| Food security | ||||||||||||
| Not enough fooda | 0.01 | 0.11 | 0.15 | 0.36 | 0.09 | 0.29 | 0.02 | 0.13 | 0.07 | 0.26 | 0.10 | 0.29 |
| No money for fooda | 0.01 | 0.11 | 0.16 | 0.37 | 0.10 | 0.30 | 0.02 | 0.13 | 0.08 | 0.27 | 0.10 | 0.31 |
| Health behaviours | ||||||||||||
| Smokinga | 0.25 | 0.43 | 0.38 | 0.49 | 0.33 | 0.47 | 0.37 | 0.48 | 0.40 | 0.40 | 0.55 | 0.50 |
| Not try lose weighta | 0.57 | 0.50 | 0.66 | 0.47 | 0.63 | 0.48 | 0.76 | 0.43 | 0.70 | 0.46 | 0.80 | 0.40 |
| Cotinine | 54.9 | 113 | 69.3 | 121 | 90.9 | 153 | 105 | 165 | 90.7 | 117 | 153 | 166 |
| Marijuanaa | 0.06 | 0.23 | 0.06 | 0.24 | 0.09 | 0.28 | 0.14 | 0.35 | 0.10 | 0.30 | 0.21 | 0.41 |
| Alcohol | 2.24 | 6.04 | 1.11 | 4.05 | 1.58 | 5.99 | 3.73 | 7.29 | 3.09 | 7.70 | 4.26 | 10.2 |
| Not walk mile/weeka | 0.69 | 0.46 | 0.78 | 0.42 | 0.73 | 0.45 | 0.68 | 0.47 | 0.68 | 0.47 | 0.62 | 0.49 |
| Cardiovascular | ||||||||||||
| Systolic pressure | 71.9 | 9.52 | 69.6 | 10.6 | 71.4 | 9.69 | 77.1 | 9.49 | 75.9 | 10.9 | 75.8 | 10.1 |
| Diastolic pressure | 113 | 12.7 | 110 | 14.4 | 111 | 13.1 | 120 | 11.2 | 120 | 12.4 | 120 | 11.8 |
| Forced Expiratory volume | 3653 | 623 | 3554 | 577 | 3458 | 613 | 5096 | 822 | 4752 | 860 | 4852 | 789 |
| Pulse rate | 76.3 | 11.8 | 78.0 | 11.8 | 76.9 | 11.2 | 72.8 | 11.3 | 76.7 | 13.0 | 73.2 | 12.2 |
| Metabolic | ||||||||||||
| HDL cholesterol | 1.43 | 0.39 | 1.39 | 0.34 | 1.31 | 0.38 | 1.18 | 0.35 | 1.20 | 0.36 | 1.18 | 0.36 |
| LDL cholesterol | 3.00 | 0.83 | 3.09 | 0.87 | 3.02 | 1.02 | 3.36 | 0.90 | 3.14 | 0.95 | 3.15 | 0.98 |
| Trigylcerides | 5.00 | 0.93 | 5.12 | 1.20 | 4.96 | 1.14 | 5.13 | 1.04 | 5.21 | 1.14 | 4.97 | 1.07 |
| Haemoglobin A1c | 5.11 | 0.67 | 5.34 | 0.99 | 5.26 | 1.02 | 5.29 | 0.70 | 5.50 | 0.84 | 5.32 | 0.67 |
| Glucose | 91.2 | 19.2 | 95.5 | 31.7 | 92.9 | 31.5 | 97.0 | 23.1 | 98.8 | 31.3 | 94.5 | 16.6 |
| Infection & immunity | ||||||||||||
| C-reactive protein | 0.42 | 0.53 | 0.48 | 0.56 | 0.50 | 0.63 | 0.31 | 0.40 | 0.38 | 0.47 | 0.37 | 0.38 |
| Lymphocytes | 31.9 | 8.14 | 32.2 | 7.77 | 32.8 | 8.14 | 32.5 | 7.74 | 32.8 | 9.55 | 34.1 | 8.79 |
| Illnessa | 0.22 | 0.42 | 0.23 | 0.42 | 0.23 | 0.42 | 0.16 | 0.37 | 0.26 | 0.44 | 0.26 | 0.44 |
| Respiratory infectiona | 0.08 | 0.28 | 0.10 | 0.30 | 0.07 | 0.26 | 0.03 | 0.18 | 0.11 | 0.31 | 0.06 | 0.24 |
| Colda | 0.35 | 0.48 | 0.35 | 0.48 | 0.36 | 0.48 | 0.29 | 0.45 | 0.34 | 0.47 | 0.33 | 0.47 |
aVariables that are dichotomous. Means (or percentages for dichotomous variables) and standard deviations are calculated using study sampling weights.
As a specification test, Table 3 presents odds ratios, coefficients and 95% confidence intervals for the treatment months and EITC qualification interaction term (i.e. β3 from our model) for demographic and anthropometric factors that could not vary over time. The purpose of these models was to test whether there were any significant differences in the sample by month that could confound our estimates. All 95% confidence intervals in this table included the null, which is consistent with our prior belief that there would be no meaningful demographic differences across EITC-eligible individuals who were surveyed in February through April compared with other months.
Table 3.
Impact of EITC disbursement month and qualifying for at least $1000 in EITC on negative control dependent outcomes from difference-in-difference models, by gender, NHANES III (n = 6925)
| Dependent variable | Women (n = 3571) |
Men (n = 3354) |
||||
|---|---|---|---|---|---|---|
| Coef/OR | Lower 95% CI | Upper 95% CI | Coef/OR | Lower 95% CI | Upper 95% CI | |
| White | 0.927 | 0.504 | 1.702 | 1.434 | 0.607 | 3.385 |
| Black | 0.972 | 0.615 | 1.536 | 0.919 | 0.453 | 1.864 |
| Mexican American | 1.081 | 0.762 | 1.535 | 1.290 | 0.797 | 2.088 |
| <High school | 1.678 | 0.877 | 3.209 | 0.962 | 0.485 | 1.907 |
| High school diploma | 0.649 | 0.369 | 1.140 | 1.326 | 0.620 | 2.836 |
| Some college | 1.013 | 0.621 | 1.653 | 0.742 | 0.361 | 1.521 |
| Annual income | 1692 | −1786 | 5170 | 828 | −1727 | 3383 |
| Height | 0.019 | −0.006 | 0.043 | 0.034 | −0.007 | 0.075 |
| Currently working | 1.001 | 0.999 | 1.002 | 1.002 | 1.000 | 1.003 |
Models include age, treatment month, EITC qualification, and treatment month*EITC qualification interaction term. Only the coefficient for interaction term is shown in the table, as an odds ratio for categorical variables and as a coefficient for continuous variables (annual income and height). Annual income is in year 2000 American dollars. Height is in centimetres.
Coef, coefficient; OR, odds ratio.
Table 4 presents primary findings for our 30 health outcomes, stratified by gender. As in Table 3, these results reflect the treatment months and EITC qualification interaction term (i.e. β3 from our model). Continuous outcomes are Z-scored, thus coefficients can be interpreted in terms of the difference in standard deviations of the outcome associated with EITC treatment. Associations with dichotomous outcomes are expressed as odds ratios. Because all the outcomes are coded with higher values indicating worse health, values greater than the null (0 for continuous measures, 1 for dichotomous measures) indicate that EITC treatment is associated with worse health-related outcomes. Among the 60 relationships examined, 21 had 95% confidence intervals that did not include the null, substantially more than the three that would be expected by chance. Of the 13 factors where 95% confidence intervals did not include the null for women, nine were in a direction associated with better health (meat, not enough food, not enough money for food, smoking, not trying to lose weight, marijuana use, HDL cholesterol, lymphocytes and colds), and 4 were in the direction associated with worse health (sodium, pulse rate, LDL cholesterol and trigylcerides). Of the eight factors where 95% confidence intervals did not include the null for men, seven were in a direction associated with better health (fruit, dairy, not enough food, not enough money for food, not trying to lose weight, cotinine and marijuana) and one was not (saturated fat). In general, effect sizes were small, with impacts on smoking, trying to lose weight and food insecurity around 2–3%, and differences in metabolic factors and diet around one-third of a standard deviation.
Table 4.
Impact of EITC disbursement month and qualifying for at least $1000 in EITC in difference-in-difference models, by gender, NHANES III (n = 6925)
| Women (n = 3571) |
Men (n = 3354) |
|||||
|---|---|---|---|---|---|---|
| Coef/OR | Lower 95% CI | Upper 95% CI | Coef/OR | Lower 95% CI | Upper 95% CI | |
| Diet | ||||||
| Overall diet | 0.150 | −0.056 | 0.355 | 0.004 | −0.154 | 0.162 |
| Vegetables | 0.071 | −0.141 | 0.284 | −0.098 | −0.465 | 0.269 |
| Fruit | 0.066 | −0.103 | 0.235 | −0.396 | −0.631 | −0.162 |
| Meat | −0.382 | −0.615 | −0.150 | −0.043 | −0.263 | 0.177 |
| Dairy | 0.114 | −0.140 | 0.369 | −0.326 | −0.633 | −0.019 |
| Sodium | 0.330 | 0.120 | 0.540 | −0.262 | −0.632 | 0.108 |
| Saturated fat | −0.020 | −0.342 | 0.303 | 0.393 | 0.116 | 0.670 |
| Diet variety | 0.149 | −0.207 | 0.506 | −0.107 | −0.379 | 0.166 |
| Food security | ||||||
| Not enough fooda | 0.968 | 0.952 | 0.985 | 0.973 | 0.954 | 0.991 |
| No money for fooda | 0.970 | 0.954 | 0.987 | 0.972 | 0.954 | 0.991 |
| Health behaviours | ||||||
| Smokinga | 0.982 | 0.974 | 0.989 | 1.003 | 0.995 | 1.011 |
| Not try lose weighta | 0.977 | 0.964 | 0.990 | 0.974 | 0.964 | 0.984 |
| Cotinine | −0.045 | −0.318 | 0.228 | −0.314 | −0.531 | −0.097 |
| Marijuanaa | 0.997 | 0.995 | 0.998 | 0.994 | 0.992 | 0.996 |
| Alcohol | −0.004 | −0.213 | 0.206 | 0.009 | −0.417 | 0.435 |
| Not walk mile/weeka | 0.998 | 0.996 | 1.001 | 1.002 | 0.999 | 1.006 |
| Cardiovascular | ||||||
| Systolic blood pressure | −0.078 | −0.232 | 0.076 | 0.207 | −0.033 | 0.447 |
| Diastolic blood pressure | −0.125 | −0.273 | 0.023 | 0.171 | −0.004 | 0.347 |
| Forced expiratory volume | −0.082 | −0.247 | 0.083 | 0.045 | −0.254 | 0.343 |
| Pulse rate | 0.343 | 0.074 | 0.611 | 0.174 | −0.070 | 0.418 |
| Metabolic | ||||||
| HDL cholesterol | −0.386 | −0.681 | −0.092 | 0.120 | −0.153 | 0.394 |
| LDL cholesterol | 0.238 | 0.038 | 0.437 | 0.152 | −0.275 | 0.578 |
| Trigylcerides | 0.218 | 0.020 | 0.417 | −0.053 | −0.300 | 0.194 |
| Haemoglobin A1c | 0.186 | −0.005 | 0.377 | 0.069 | −0.106 | 0.244 |
| Glucose | 0.089 | −0.046 | 0.225 | 0.095 | −0.044 | 0.234 |
| Infection & immunity | ||||||
| C-reactive protein | 0.026 | −0.087 | 0.138 | 0.003 | −0.174 | 0.180 |
| Lymphocytes | −0.342 | −0.506 | −0.178 | −0.135 | −0.551 | 0.281 |
| Illnessa | 0.999 | 0.997 | 1.002 | 1.000 | 0.998 | 1.001 |
| Respiratory infectiona | 1.001 | 1.000 | 1.002 | 1.000 | 0.999 | 1.001 |
| Colda | 0.990 | 0.983 | 0.997 | 0.995 | 0.990 | 1.001 |
Coefficients are from interaction term of disbursement month X EITC qualified for at least $1000. All continuous outcomes are Z-scored. Positive coefficients indicate association with worse health. Odds ratios above 1 indicate association with worse health. Coefficients and 95% confidence intervals are emboldened when the 95% confidence interval does not include the level of the coefficient indicating no association.
aCoefficients for dichotomous outcomes are presented as odds ratios.
Coef, coefficient; OR, odds ratio.
As a sensitivity analysis, Supplementary Table 1 (available as Supplementary data at IJE online) presents a similar analysis but for individuals qualifying for an EITC of any size. Among the 60 relationships examined, 13 had confidence intervals that did not cross the null. Among women, all six confidence intervals were associated with better health (meat consumption, smoking, not trying to lose weight, marijuana use, diastolic blood pressure and colds). Among men, six were associated with better health (overall diet, fruit, sodium, not trying to lose weight, cotinine and marijuana) and one was not (Haemoglobin A1c).
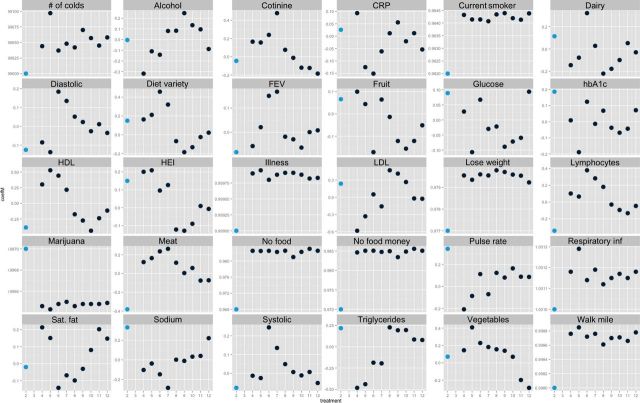
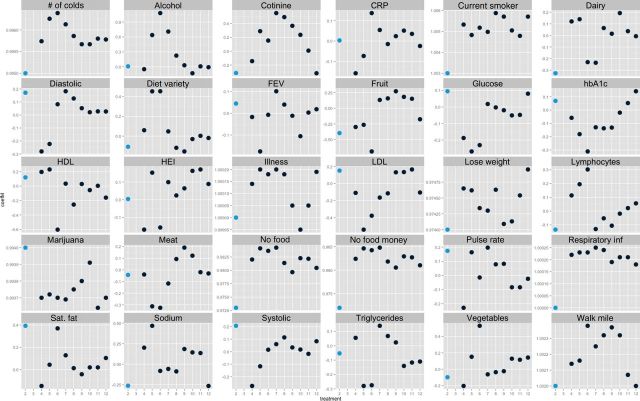
Figures 2 and 3 show results of the permutation tests of placebo treatments for women and men, respectively. The light-coloured dot at 2 on the x-axis shows the coefficient for the true treatment months shown in Table 4, and the black dots indicate the placebo treatment permutation analysis for the nine other groups, with starting month as indicated on the x-axis (i.e. 4 indicates April, May, June; 5 indicates May, June, July). When the coefficient for the true treatment group is further from the null than all nine of the placebo treatments, this indicates support for a true difference during the treatment months. This was for most factors consistent with the findings presented in Table 4 with the exception of marijuana use for men and women, LDL cholesterol for women and fruit consumption for men.
Figure 2.
Permutation tests of placebo treatments for difference-in-difference models of EITC receipt and health-related outcomes, women. Light dots indicate point estimate of actual exposure. Black dots indicate point estimates of placebo permutation exposures. Y-axis for each plot differs depending on scale of outcome. X-axis indicates first month of 3-month group of exposure (i.e. 2 indicates true treatment months of Feb, Mar, Apr; 4 indicates placebo treatment months of Apr, May, Jun). FEV, Forced Expiratory Volume; HEI, Healthy Eating Index Overall Diet.
Figure 3.
Permutation tests of placebo treatments for difference-in-difference models of EITC receipt and health-related outcomes, men. Light dots indicate point estimate of actual exposure. Black dots indicate point estimates of placebo permutation exposures. Y = axis for each plot differs depending on scale of outcome. X-axis indicates first month of 3-month group of exposure (i.e. 2 indicates true treatment months of Feb, Mar, Apr; 4 indicates placebo treatment months of Apr, May, Jun). FEV, Forced Expiratory Volume; HEI, Healthy Eating Index Overall Diet.
Discussion
The majority of outcomes we examined were not affected by income receipt among EITC recipients. Among factors that were affected, the short-term effects of EITC receipt were on balance more health-promoting than detrimental. Indeed, many outcomes that are key determinants of health (e.g. food security, smoking/exposure to smoke) were affected in a health-promoting direction. Focusing on results for respondents who were eligible for at least $1000 of EITC, nine of the 13 factors where the 95% confidence interval did not include the null for women, and seven of the eight factors where the 95% confidence interval did not include the null for men, are in a direction associated with better health. Results related to diet were mixed. On the positive side, EITC income receipt appeared associated with a healthier level of meat consumption for women and a healthier level of dairy consumption for men. On the negative side, EITC income receipt appeared to increase sodium for women and saturated fat for men. Given prior studies documenting increased substance use in response to income receipt, it is also noteworthy that we find that EITC income lowers smoking-related outcomes (i.e. self-reported smoking for women and cotinine levels for men) and we further find no evidence that EITC income increases alcohol consumption. When repeating our analysis with a different treatment group, those eligible for an EITC of any size, results for many of the outcomes (most notably, efforts at weight loss, indicators of smoking, and some gender-specific results related to meat consumption) remained consistent, although they were typically more modest in magnitude, which is unsurprising given that the mean qualified credit amount was lower.
There is some evidence that social spending and cash assistance programmes may have important public health consequences.28 However, individuals’ psychological and behavioural responses to income receipt are likely to be complex and potentially variable. Consequently, there are ongoing debates as to whether income transfers tend, on average, to be more health promoting or health hindering. Examining the EITC, which is the largest anti-poverty programme in the USA, and considering the wide variety of health-related outcomes that were selected a priori to avoid selective publication bias of only significant findings,29 the above results shed important light on this issue. Contextualizing these results in terms of the existing literature, we note that our results roughly align with existing studies of EITC income. Prior studies have examined how changes in EITC policies predict specific health outcomes, such as infant health,30–32 biomarkers,33 obesity34 and self-assessed health.33 Most of these studies suggest that EITCs are health promoting,30,32,33 but there are exceptions which reveal deleterious health effects of the EITC.31,34 Our analysis, which reveals mixed effects but on balance, more health-promoting effects, conforms to this general pattern in the literature. It is important to highlight, though, that our study stands apart from these prior studies because, whereas most of these studies focus on annual trends and capture effects of both income transfers and employment incentives of the EITC, our study of seasonal fluctuations isolates effects of income transfers from the EITC.
The results challenge prior literature that suggests that substance use and abuse increase in the short term following income receipt.4–6 One possible explanation is that our study has less power to detect effects because we do not know the exact date and amount of income received, thus likely biasing our effect estimates to the null. Consistent with this explanation, our estimates of association are smaller in magnitude than other income disbursement studies.7 Other potential explanations for differences in findings are that unlike prior studies of income receipt among military and older individuals,6 our sample included very few single men. Since EITC qualification requires dependent children, and single-parent male-headed households are rare in the USA, most men in our sample are married and cohabiting with children.
A few issues and caveats to our results should be considered. First, this was an intent-to-treat analysis (ITT). Using the NHANES, we could not know when or whether a particular respondent received the EITC. Rather, we compared health outcomes across seasonal periods and subgroups that align with the structure of the EITC. Compared with estimates based on direct measurement of the EITC, this ITT strategy may yield downwardly biased results because of measurement error, but it also avoids a likely source of upward bias if healthier individuals are more likely to actually receive the EITC. No nationally representative US health datasets collect information on individuals’ EITC receipt, in part because many people who use tax preparation services are not actually aware of what portion of their tax refund reflected the EITC. Given these issues, and the fact that most EITC-eligible individuals (80–86%8) receive the credit, an ITT analysis is likely a preferable strategy for modelling EITC effects. There also is likely some small misclassification of findings because the dependency status of children living with their parents is unknown. Because of lack of year-round data collection in the Mid-Western and North-Eastern United States, generalizability of our results to these regions is precluded. We also note that our sample size of treated individuals was small (167 women and 111 men), thus our findings should be replicated to determine the stability of our results.
Given our identification strategy, the most likely sources of confounding bias are related to seasonal variations. There are noted seasonal fluctuations in health behaviours and biomarkers,35,36 but for these variations to upwardly bias our estimates, EITC-qualifiers would need to have more positive seasonal variation in outcomes than non-qualifiers. For example, individuals in the EITC-qualifying range may be more likely to be working in the new year or more likely to maintain health-promoting behaviours for several months following new-year resolutions.37
Our analysis could not speak to the mechanisms that link EITC income to positive or negative health-related outcomes. It is reasonable to suspect that such mechanisms are related to a combination of material factors, consumption patterns and psychological mechanisms. For example for low-wage workers, receiving at least $1000 of EITC income may reduce psychological stress related to finances, making it easier to improve health behaviours like reducing smoking. Future researchers involved in more focused primary data collection may be able to shed light on these important issues. Additionally, given the structure of the NHANES, we cannot know how long the short-term effects documented in this study might be sustained over time.
Supplementary Data
Supplementary data are available at IJE online.
Funding
This work was supported by the Robert Wood Johnson Foundation Health & Society Scholars Program through its support of D.H.R. and K.W.S as Health & Society Scholars. D.H.R. is supported by grant number K01AG047280 from the National Institute of Aging.
Conflict of interest: None declared.
Supplementary Material
References
- 1.Kawachi I, Adler NE, Dow WH. Money, schooling, and health: Mechanisms and causal evidence. Ann N Y Acad Sci 2010;1186:56–68. [DOI] [PubMed] [Google Scholar]
- 2.Kitagawa E, Hauser P. Differential Mortality in the United States . Cambridge, MA: Harvard University Press, 1973. [Google Scholar]
- 3.Dobkin C, Puller SL. The effects of government transfers on monthly cycles in drug abuse, hospitalization and mortality. J Public Econ 2007;91:2137–57. [Google Scholar]
- 4.Halpern SD, Mechem CC. Declining rate of substance abuse throughout the month. Am J Med 2001;110:347–51. [DOI] [PubMed] [Google Scholar]
- 5.Phillips DP, Christenfeld N, Ryan NM. An increase in the number of deaths in the United States in the first week of the month - an association with substance abuse and other causes of death. N Engl J Med 1999;341:93–98. [DOI] [PubMed] [Google Scholar]
- 6.Evans WN, Moore TJ. The short-term mortality consequences of income receipt. J Public Econ 2011;95:1410–24. [Google Scholar]
- 7.Apouey B, Clark AE. Winning Big but Feeling No Better? The Effect of Lottery Prizes on Physical and Mental Health Health Economics. Health Econ 2014; doi: 10.1002/hec.3035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Scholz JK. The earned income tax credit: participation, compliance, and antipoverty effectiveness. Natl Tax J 1994;47:63–87. [Google Scholar]
- 9.Pega F, Carter K, Blakely T, Lucas P. In work tax credits for families and their impact on health status in adults. Cochrane Database Syst Rev 2012;7:CD009963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Averett S, Wang Y. The effects of Earned Income Tax Credit payment expansion on maternal smoking. Health Econ 2013;22:1344–59. [DOI] [PubMed] [Google Scholar]
- 11.Cowan B, Tefft N. Education, maternal smoking, and the Earned Income Tax Credit. The BE Journal of Economic Analysis & Policy. 2012;12:1–39. [Google Scholar]
- 12.Dahl GB, Lochner L. The Impact of Family Income on Child Achievement: Evidence from Changes in the Earned Income Tax Credit. American Economic Review 2012;102:1927–56. [Google Scholar]
- 13.Pega F, Carter K, Kawachi I, et al. The impact of in-work tax credit for families on self-rated health in adults: a cohort study of 6900 New Zealanders. J Epidemiol Community Health 2013;67:682–88. [DOI] [PubMed] [Google Scholar]
- 14.Edwards RD. Macroeconomic implications of the earned income tax credit. Natl Tax J 2004;57:45–66. [Google Scholar]
- 15.National Center for Health Statistics. NHANES III Examination Data File Documentation, December 1996 . Hyattsville, MD: National Center for Health Statistics, 1996. [Google Scholar]
- 16.Feenberg D, Coutts E. An introduction to the TAXSIM model. J Policy Anal Manag 1993;12:189–94. [Google Scholar]
- 17.Kennedy ET, Ohls J, Carlson S, Fleming K. The Healthy Eating Index: design and applications. J Am Diet Assoc 1995;95:1103–08. [DOI] [PubMed] [Google Scholar]
- 18.Hann CS, Rock CL, King I, Drewnowski A. Validation of the Healthy Eating Index with use of plasma biomarkers in a clinical sample of women. Am J Clin Nutr 2011;74:479–86. [DOI] [PubMed] [Google Scholar]
- 19.Weinstein SJ, Vogt TM, Gerrior SA. Healthy Eating Index scores are associated with blood nutrient concentrations in the third National Health And Nutrition Examination Survey. J Am Diet Assoc 2004;104:576–84. [DOI] [PubMed] [Google Scholar]
- 20.Briefel RR, Flegal KM, Winn DM, Loria CM, Johnson CL, Sempos CT. Assessing the nation's diet: limitations of the food frequency questionnaire. J Am Diet Assoc 1992;92:959–62. [PubMed] [Google Scholar]
- 21.Gunter EW, Lewis BG, Koncikowski SM. Laboratory Procedures Used for the Third National Health and Nutrition Examination Survey (NHANES III), 1988–1994 . Hyattsville, MD: National Center for Health Statistics, 1996. [Google Scholar]
- 22.Furnée CA, Groot W, Pfann GA. Health and income: a meta-analysis to explore cross-country, gender and age differences. Eur J Public Health 2011;21:775–80. [DOI] [PubMed] [Google Scholar]
- 23.Kavanagh A, Bentley RJ, Turrell G, Shaw J, Dunstan D, Subramanian S. Socioeconomic position, gender, health behaviours and biomarkers of cardiovascular disease and diabetes. Soc Sci Med 2010;71:1150–60. [DOI] [PubMed] [Google Scholar]
- 24.Eissa N, Hoynes H. Behavioural responses to taxes: lessons from the EITC and labor supply. Tax Policy Econ 2005;20:73–110. [Google Scholar]
- 25.National Center for Health Statistics. Analytic and Reporting Guidelines: The Third National Health and Nutrition Examination Survey (NHANES III), 1988–1994. Hyattsville, MD: National Center for Health Statistics, 1996. [Google Scholar]
- 26.Lumley T. Survey: analysis of complex survey samples. R Package 2009;version 3.16. [Google Scholar]
- 27.Conley TG, Taber CR. Inference with ‘difference in differences’ with a small number of policy changes. Rev Econ Stat 2011;93:113–25. [Google Scholar]
- 28.Schoeni RF, House JS, Kaplan GA, Pollack H. Making Americans healthier: social and economic policy as health policy. Thousand Oaks, CA: Russell Sage Foundation, 2008. [Google Scholar]
- 29.Ioannidis JPA. Why Most Published Research Findings Are False. PLoS Med 2005;2:e124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Strully KW, Rehkopf DH, Xuan Z. Effects of prenatal poverty on infant health: State Earned Income Tax Credits and birth weight. Am Sociol Rev 2010;75:534–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bruckner TA, Rehkopf DH, Catalano RA. Income gains and very low-weight birth among low-income black mothers in California. Biodemogr Soc Biol 2013;59:141–56. [DOI] [PubMed] [Google Scholar]
- 32.Hoynes HW, Miller DL, Simon D. Income, the Earned Income Tax Credit, and Infant Health . Cambridge, MA: National Bureau of Economic Research, 2012. [PubMed] [Google Scholar]
- 33.Evans WN, Garthwaite CL. Giving Mom a Break: The Impact of Higher EITC Payments on Maternal Health. American Econ J: Econ Policy 2014;6:258–90. [Google Scholar]
- 34.Schmeiser MD. Expanding wallets and waistlines: the impact of family income on the BMI of women and men eligible for the Earned Income Tax Credit. Health Econ 2009;18:1277–94. [DOI] [PubMed] [Google Scholar]
- 35.Lewington S, Li L, Sherliker P, et al. Seasonal variation in blood pressure and its relationship with outdoor temperature in 10 diverse regions of China: the China Kadoorie Biobank. J Hypertens 2012;30:1383–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tseng CL, Brimacombe M, Xie M, et al. Seasonal patterns in monthly hemoglobin A1c values. Am J Epidemiol 2005;161:565–74. [DOI] [PubMed] [Google Scholar]
- 37.Norcross JC, Vangarelli DJ. The resolution solution: longitudinal examination of New Year's change attempts. J Subst Abuse 1988;1:127–34. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.