Description
A 22-year-old woman with end-stage renal failure secondary to membranoproliferative glomerulonephritis presented with methicillin-sensitive Staphylococcus aureus sepsis from an infected haemodialysis catheter-related giant right atrial (RA) thrombus (figure 1A) with an additional mobile thrombus in the superior vena cava (SVC; figure 1B, C). The patient was undergoing haemodialysis via a tunnelled dual lumen 13.5 Fr, 36 cm Hickman chronic dialysis catheter inserted 9 months prior (figure 1D). Thrombophilia screening was negative.
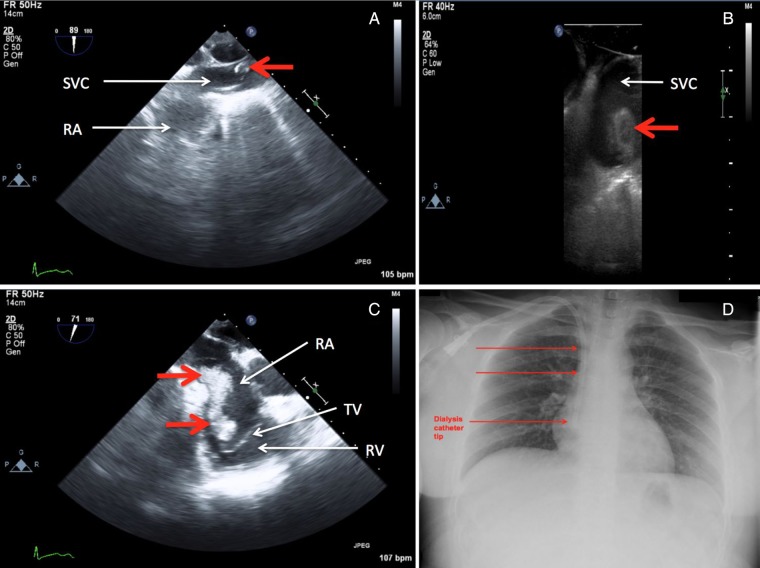
Figure 1.
Transoesophageal echocardiography demonstrating cardiac thrombi (thick red arrows) in the SVC–right atrial junction (A and B) and a giant thrombus attached to the lateral wall of the RA (C); the thombus extended onto the TV with preservation of the valve leaflets, but not in the RV. A chest radiograph (D) showing a tunnelled dual lumen chronic dialysis catheter (thin red arrows) with the tip positioned in the RA (RA, right atrium; RV, right ventricle; SVC, superior vena cava; TV, tricuspid valve).
In view of the size and separate intracardiac locations of the thrombi, management with systemic anticoagulation was considered prohibitive due to risks of fatal pulmonary embolus, right heart failure, infective endocarditis and progressive sepsis. Urgent surgical thrombectomies of the RA and SVC thrombi were performed uneventfully via a midline sternotomy requiring cardiopulmonary bypass. Histopathology is presented in figure 2A, B.
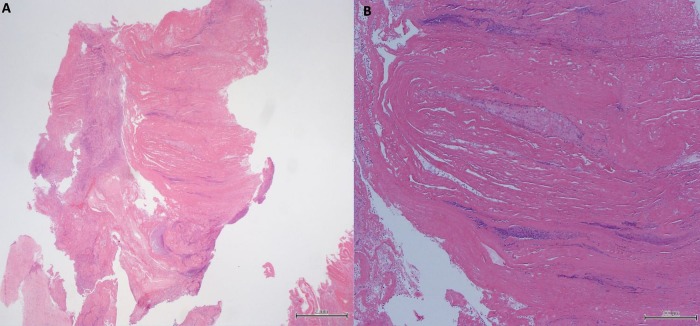
Figure 2.
Histological examination showing cardiac thrombus (stained with H&E) at ×40 (A) and ×100 (B) magnification. There are focally laminated collections of degenerated erythrocytes and fibrin admixed with neutrophils and cellular debris. In the periphery ingrowth of spindle cells representing myofibroblasts are present.
Symptomatic catheter-related thrombosis occurs in up to 28% adults with mortality rates in excess of 15%.1 2 Pathophysiological mechanisms of the catheter-related thrombi include activation of the coagulation cascade from direct mechanical trauma to the RA wall from the catheter tip, exacerbated by altered fluid dynamics in the RA around the catheter. While positioning the catheter tip in the right atrium is consistent with the National Kidney Foundation recommendations,3 achieving better blood flow rates during haemodialysis is often offset against the increased risks of catheter-related RA thrombi, as seen in this case.
The patient was given intravenous flucloxacillin for 6 weeks, and was discharged 15 days postoperatively after successful conversion to nocturnal automated peritoneal dialysis. The patient is currently being evaluated for renal transplantation.
Learning points.
There are no established guidelines for management of complex intracardiac catheter-related right atrial (RA) thrombi.
Early surgical evacuation should be considered in young patients with giant RA thrombi, especially if mobile elements are present, to prevent catastrophic complications such as a massive pulmonary embolus, right heart failure, infective endocarditis and sepsis.
Frequent echocardiographic screening for intracardiac thrombus formation should be mandatory for all long-standing chronic dialysis catheters whose tips are positioned in the RA.
Footnotes
Contributors: LW was responsible for the planning, conduct and writing of the report and obtained all transoesophageal images intraoperatively. FZ was responsible for the literature review, collation of clinical images and writing of the manuscript. ST was involved in preparation of all the images and writing of the report. NR was the principal cardiac surgeon who performed the thrombectomies and was involved in writing of the report. All authors have read and approved the final manuscript. LW was responsible for the overall content and is the guarantor.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Stavroulopoulos A, Aresti V, Zounis C. Right atrial thrombi complicating haemodialysis catheters. A meta-analysis of reported cases and a proposal of a management algorithm. Nephrol Dial Transplant 2012;27:2936–44 doi:10.1093/ndt/gfr739 [DOI] [PubMed] [Google Scholar]
- 2.Baskin JL, Pui CH, Reiss U et al. . Management of occlusion and thrombosis associated with long term indwelling central venous catheters. Lancet 2009;37:159–69 doi:10.1016/S0140-6736(09)60220-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.NKF/DOQI. Clinical Practice Guidelines for Vascular Access, 2006 Updates. CPG 2.4. http://www.kidney.org/professionals/KDOQI/guideline_upHD_PD_VA/va_guide2.htm (accessed Nov 2014).