Abstract
Objectives.
Research shows that socially disadvantaged groups—especially African Americans and people of low socioeconomic status (SES)—experience more unstable social environments. I argue that this causes higher rates of turnover within their personal social networks. This is a particularly important issue among disadvantaged older adults, who may benefit from stable networks. This article, therefore, examines whether social disadvantage is related to various aspects of personal network change.
Method.
Social network change was assessed using longitudinal egocentric network data from the National Social Life, Health, and Aging Project, a study of older adults conducted between 2005 and 2011. Data collection in Wave 2 included a technique for comparing respondents’ confidant network rosters between waves. Rates of network losses, deaths, and additions were modeled using multivariate Poisson regression.
Results.
African Americans and low-SES individuals lost more confidants—especially due to death—than did whites and college-educated respondents. African Americans also added more confidants than whites. However, neither African Americans nor low-SES individuals were able to match confidant losses with new additions to the extent that others did, resulting in higher levels of confidant network shrinkage. These trends are partly, but not entirely, explained by disadvantaged individuals’ poorer health and their greater risk of widowhood or marital dissolution.
Discussion.
Additional work is needed to shed light on the role played by race- and class-based segregation on group differences in social network turnover. Social gerontologists should examine the role these differences play in explaining the link between social disadvantage and important outcomes in later life, such as health decline.
Key Words: Aging, Bereavement, Network change, Race, Social inequality, Social networks.
One of the most enduring lessons to emerge from social science research over the past few decades is that the social networks in which people are embedded—through friendship, support, exchange, conflict, kinship, and other types of relationships (Wasserman & Faust, 1994)—are profoundly consequential for individuals. Social networks shape their access to resources, exposure to social influence and control, perceptions, attitudes, opportunities, and power, among other things (Wellman, 1983). Social networks are, therefore, implicated in a wide variety of outcomes, ranging from access to resources and social support to health-related behaviors, delinquency, and mortality (e.g., Cornwell & Waite, 2009; Holt-Lunstad, Smith, & Layton, 2010; Smith & Christakis, 2008; Stephens, Alpass, Towers, & Stevenson, 2011; Wellman & Wortley, 1990). But just as researchers have made tremendous gains in pinpointing the elements of social networks that drive these effects (e.g., network size and network members’ attributes), they have also come to realize that these elements are highly dynamic and prone to change. As such, the focus has begun to shift toward the problem of understanding the nature, consequences, and causes of social network change (see Snijders & Doreian, 2010; Wellman, Wong, Tindall, & Nazer, 1997). This article represents an attempt to understand some of the causes of change within individuals’ personal networks, specifically as it unfolds within the context of later life.
First, consider the nature and potential consequences of network change. Personal network change involves several unique processes, including the loss and addition of close contacts, network turnover, as well as subtler shifts in the configuration of social resources, influences, and relationships within an individual’s network. These processes are known to affect important individual outcomes such as health and mortality (Eng, Rimm, Fitzmaurice, & Kawachi, 2002; Giordano & Lindstrom, 2010; Holtzman et al., 2004; Kroenke, Kubzansky, Adler, & Kawachi, 2008; Seeman et al., 2011; Thomas, 2012). The implications of network change, however, depend on several factors. These include the nature of the social ties involved in the change in question (e.g., whether they are weak or strong, supportive or harmful) and whether change was purposeful and anticipated. For instance, losing or gaining close contacts may result in an unintended reshuffling of the social influences and norms that constitute one’s social environment. This can give rise to a sense of normlessness or detachment from society (Deflem, 1989), reduced capacity to locate specific forms of support within one’s network (Pescosolido, 1992), and disruption to preexisting routines and systems of coordination (Cornwell & Laumann, in press). Undesired network losses that are beyond one’s control can also reduce one’s sense of control and coping capacity (Gerstorf, Röcke, & Lachman, 2011)—especially when this involves an irreversible loss, such as the death of a friend. The analysis below will address these types of losses explicitly.
At the same time, individuals often purposefully cut ties with close network members and/or cultivate ties with new ones, perhaps in an effort to achieve a more emotionally close set of contacts (Charles & Carstensen, 2010) or a more strategically advantageous one (Burt, 2005). Making new friends, for example, can increase the number, range, and quality of social resources that are available to a person. In short, the consequences of change within an individual’s personal network are likely contingent on the nature of the ties involved and how those changes come about. This possibility makes it especially important to understand the determinants of network change, particularly those factors that reduce individuals’ control over such change.
The Relevance of Social Disadvantage
Several theoretical frameworks suggest that social disadvantage is one factor that greatly affects the extent to which, and why, individuals’ personal networks change. Sociological perspectives suggest that the social environments of disadvantaged groups—especially racial minorities and low–socioeconomic status (SES) individuals—are less stable than the environments of more advantaged groups. Persistent social disorder, greater prevalence of unemployment and contingent work, residential instability (e.g., due to evictions), poverty, and high incarceration rates combine to create unusually high levels of instability within the social environments (i.e., neighborhoods and households) within which disadvantaged groups are concentrated (Atkinson, Liem, & Liem, 1986; Cattell, 2001; Cornwell, 2014; Desmond, 2012a; Kasarda & Janowitz, 1974; Rose & Clear, 1998; Small, 2007; van Eijk, 2010; Wellman et al., 1997). This, in turn, can create distrust, uncertainty, asynchrony, and a lack of cooperation in disadvantaged individuals’ personal networks (Goffman, 2009; Miller-Cribbs & Farber, 2008; Smith, 2007). Indeed, research suggests that environmental instability can yield circumstances in which one’s network ties are rendered temporary, “disposable,” and substitutable (Desmond, 2012b). Though this is debatable, some research also implies that this results in smaller or more restricted personal networks within disadvantaged social strata—including in later life (see Ajrouch, Antonucci, & Janevic, 2001; Peek & O’Neill, 2001).
This circumstance suggests that some groups—especially African Americans and those with few material resources—experience turnover within their personal networks in a manner that mirrors the instability of the broader social environments in which they live. This research implies not only that disadvantaged groups experience higher rates of loss from the ranks of their personal social networks but also that they have greater difficulty recovering from and adapting to those losses. One reason this is such an important issue is that socially disadvantaged people—especially the urban poor—must rely disproportionately on network members (especially kin) for social support and for indirect access to resources to survive (e.g., Cantor, 1979; Small, 2009).
Network Change, Social Disadvantage, and Aging
Age is also an important determinant of personal network change. Social gerontologists have long been concerned about the implications of aging for social integration (e.g., Cumming & Henry, 1961), for later life is a time when the need for social support increases and when primary network ties are a key source of sense of belonging. Life-course transitions like retirement, widowhood, health decline, and residential changes can drastically alter a person’s network (Cornwell, 2009; Perry & Pescosolido, 2012; Schafer, 2013). Accordingly, social gerontologists have become increasingly interested in examining the nature and implications of change in individuals’ social networks (Shaw, Krause, Liang, & Bennett, 2007; van Tilburg, 1998; Wrzus, Hänel, Wagner, & Neyer, 2013). Much research has focused on how bereavement affects social engagement (e.g., Donnelly & Hinterlong, 2010), and there is increasing interest in how health problems affect older adults’ efforts to form and maintain social ties (e.g., Cornwell, 2009; Schafer, 2013). At the same time, network changes that occur in late life are often purposeful, perhaps motivated by a sense of a dwindling life span and the desire to cut ties with weaker contacts and to spend more time with loved ones (Charles & Carstensen, 2010), to be more autonomous (Marcum, 2013), or to achieve independence from abusive, exploitative, or otherwise stifling relationships (e.g., Cornwell, 2011; Pillemer, & Suitor, 1992). Moreover, continuity, activity, and adaptation theories argue that people grow accustomed to certain social roles and activities during their lives and often attempt to maintain their roles, or develop substitutes, through later-life transitions (e.g., Atchley, 1989; Donnelly & Hinterlong, 2010; Heckhausen, 2006). The loss of social ties associated with life-course transitions, therefore, often sparks efforts to adapt to and/or compensate by developing new ties (Bloem, van Tilburg, & Thomése, 2008; Cornwell & Laumann, in press; Lamme, Dykstra, & van Groenou, 1996; Zettel & Rook, 2004).
Network-oriented social-gerontological research usually treats these kinds of later-life transitions as challenges to general social network connectedness—developments that can threaten the stability of one’s personal network. One of the primary concerns that motivates this article is that such developments may be even more salient for aging minorities and members of lower socioeconomic strata. It is possible that the transitions of later life compound socially disadvantaged groups’ already problematic experiences with personal network change in part because their transitions, and those of their social contacts, are especially trying (e.g., see Shaw et al., 2007). In addition (and related) to the aspects of social disorganization discussed earlier, members of socially disadvantaged groups suffer from more health problems, worse health care, and higher mortality rates (Adler & Rehkopf, 2008; Kawachi, Kennedy, Lochner, & Prothrow-Stith, 1997; Link & Phelan, 1995; Williams & Collins, 1995). By implication, they also experience bereavement more frequently due to the health-related incapacitation, institutionalization, or death of network members (e.g., Hawkins & Abrams, 2007). Indeed, the congruence of environmental instability associated with social disadvantage and the challenges that accompany later life may contribute to a form of “double jeopardy” among older minorities (e.g., see Carreon & Noymer, 2011), producing a situation that exacerbates preexisting health-related and other forms of inequality within aging cohorts (see also Dannefer, 1987, 2003).
Accordingly, adaptation and compensation efforts may be a bigger part of socially disadvantaged older adults’ everyday lives. This could mean that they experience higher rates of both network loss and network growth, producing a cycle of chronic network turnover, or “churn,” that amplifies preexisting instability within their social environments. This picture of constant adaptation is complicated, however, by the fact that older disadvantaged adults are particularly short on the resources and opportunities needed to continually replenish their personal social networks. That is, to the extent that they experience a concurrence of greater health problems and more unstable environments, socially disadvantaged older adults may have greater difficulty than both other older adults and younger disadvantaged individuals in adapting to and compensating for unwanted changes in their personal social networks.
Method
I explore these ideas using data from two waves of the National Social Life, Health, and Aging Project (NSHAP), a nationally representative, population-based panel study funded by the National Institutes of Health. The NSHAP focuses on understanding connections between older adults’ social lives and health. Wave 1 (W1) was conducted in 2005–2006 and consisted of in-home interviews with 3,005 community-dwelling older adults between the ages of 57 and 85. The sample was selected using a multistage area probability design that oversampled by race/ethnicity, age, and gender. The final response rate for W1 was 75.5%. In 2010–2011, the NSHAP conducted a second wave (W2). Of the baseline respondents, 744 (24.8%) were lost to some form of attrition. NSHAP’s W2 response rate from among eligible surviving baseline respondents (N = 2,548) is 88.7%. In all, the NSHAP reinterviewed 75.2% of W1 respondents, yielding a panel of 2,261 older adults.
This analysis focuses on changes that occurred within respondents’ personal (“egocentric”) social networks during this study period. Starting at W1, all respondents were asked to list up to five people with whom they discuss “things that were important to you” during the past year (i.e., “confidants”). This procedure tends to elicit strong ties—ties through which social influence and resources are most likely to flow (see Bailey & Marsden, 1999; Cornwell, Laumann, & Schumm, 2008). To assess network change, the NSHAP collected respondents’ confidant rosters at both waves. Not only were the same network data collected at W2 as at W1 but the NSHAP also devised a computer-assisted personal interviewing (CAPI) exercise at W2 to reveal specific confidant changes between waves among the respondents who participated in both waves. At W2, interviewers first collected each respondent’s confidant roster and preliminary information about respondents’ relationships with confidants. The respondent’s W1 roster was preloaded into the CAPI instrument and was not visible to the respondent while completing this step. After the respondent completed the W2 roster, the CAPI was programmed to display a visual representation linking matches between the W1 and W2 rosters (Figure 1). The respondent was asked to verify if these computer-programmed matches were correct and was given the opportunity to correct any mismatches. The W1 roster line corresponding to the same W2 confidant was then recorded where applicable.
Figure 1.
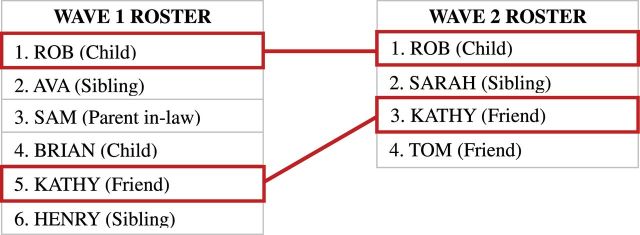
Sample screenshot of the CAPI interface used by a hypothetical National Social Life, Health, and Aging Project respondent to match her W1 network members to her W2 network members.
First, I calculate the number of confidants who were named at W1 but who were not named as confidants again at W2 (confidants “lost”). Second, I calculate the number of confidants who were named at W2 but who had not been named as such at W1 (confidants “added”). I measure overall net change in network size between waves by subtracting W1 network size from W2 network size (“overall change”). Finally, as an adjunct to the analysis of network loss, I calculate the number of W1 confidants who died between waves.
Multivariate Poisson regression analyses are used to predict the number of confidants lost from these respondents’ networks, the number who died, the number of who were lost due to reasons other than death, and the number of new network members added. Poisson is appropriate because these four variables are count models, and there is little evidence of overdispersion (the variances of these counts are about the same as their means). The number of network members at baseline was included as the exposure variable, which effectively controls for network size effects. Multivariate OLS regression is used to predict overall net change in the size of respondents’ networks during the study period. Baseline network size is controlled when predicting this outcome as well.
The models proceed first by regressing each of the dependent variables on a set of sociodemographic predictors, including age (which is divided by 10 to provide more meaningful coefficients), gender (male/female), race/ethnicity (white, African American, Latino, and other), and SES (high school education or less, some college, or college/professional degree). (SES can also be measured using ordinal information about respondents’ estimated assets. Unfortunately, this information is missing for nearly 15% of the baseline NSHAP sample. Supplemental analyses that measure SES using assets as a predictor reveal a similar pattern of results as those regarding education, with the exception of nonsignificant findings in the analysis of aggregate network change. Results are available upon request.) These initial models provide information about whether aspects of race and/or SES significantly predict measures of network change. Note that the first models for each dependent variable also control for respondents’ average frequency of contact with and closeness to their W1 confidants, the kin composition of their W1 networks, and their frequency of attendance at religious services. These baseline characteristics help to capture the structural features of social networks and community involvement that affect the stability of one’s network and opportunities to maintain and develop new ties. Table 1 provides detailed descriptions of variable construction, means/proportions, and standard deviations.
Table 1.
Descriptions, Weighted Means, and Standard Deviations of Key Variables (N = 2,119)a
| Variable | Description | Proportion or mean | SD |
|---|---|---|---|
| Age | R's age at baseline (in years, divided by 10). Range: 5.7–8.5 | 6.800 | 0.760 |
| Female | Whether R is female | 0.516 | 0.500 |
| Race/ethnicity | Whether R is non-Hispanic white | 0.804 | 0.397 |
| Whether R is non-Hispanic African American | 0.099 | 0.299 | |
| Whether R is Latino | 0.070 | 0.256 | |
| Whether R is some other race | 0.026 | 0.160 | |
| Education (W1) | R's had high school education or less | 0.455 | 0.498 |
| R has some college, but no degree | 0.299 | 0.458 | |
| R has a college or professional degree (ref.) | 0.247 | 0.431 | |
| Working (ref.) | Whether R was working at both waves | 0.174 | 0.379 |
| Retired | Whether R was retired at both waves | 0.471 | 0.499 |
| Other not working | Whether R was not working for other reasons at both waves | 0.144 | 0.351 |
| Became retired | Whether R became retired between W1 and W2 | 0.151 | 0.359 |
| Stopped working | Whether R stopped working between W1 and W2 for other reasons | 0.025 | 0.155 |
| Started working | Whether R started working between W1 and W2 | 0.035 | 0.185 |
| Married (ref.) | Whether R was married at both waves | 0.576 | 0.494 |
| Widowed | Whether R was a widow(er) at both waves | 0.162 | 0.368 |
| Unmarried | Whether R was not married at either wave for other reasons | 0.163 | 0.369 |
| Became widowed | Whether R was widowed between W1 and W2 | 0.070 | 0.255 |
| Became unmarried | Whether R became separated/divorced between W1 and W2 | 0.015 | 0.123 |
| Got married | Whether R got married between W1 and W2 | 0.013 | 0.115 |
| Functional impairment (W2) | R's self-rated ability to complete each of seven activities of daily living on their own at W1. Responses range from "unable to do" (=1) to "no difficulty" (=4) (α = .841). Items are averaged together. Range: −4.790 to 0.390 | 0.050 | 0.675 |
| Self-rated health (W2) | R's self-rated overall health, ranging from "poor" (=1) to excellent (=5) | 3.265 | 1.104 |
| Depressive symptoms (W2) | Average of R's standardized responses to 10 ordinal items from the CES-D scale assessing depressive symptoms. Responses range from "rarely or none of the time" (=0) to "most of the time" (=3). Items are averaged together. Range: −0.602 to 2.832 | −0.017 | 0.564 |
| W1 network size | Number of confidants at W1. Range: 1–5 | 3.587 | 1.392 |
| Δ in network size | Network size at W2 minus network size at W1. Range: −5 to 4 | 0.187 | 1.576 |
| Lost for any reason | Number of confidants lost between W1 and W2 | 1.486 | 1.252 |
| Lost (but not died) | Number of confidants lost between W1 and W2 (not including deaths) | 1.230 | 1.150 |
| Confidants died | Number of confidants who died between W1 and W2 | 0.256 | 0.529 |
| Confidants added | Number of new confidants added between W1 and W2 | 1.897 | 1.369 |
Notes. CES-D = Center for Epidemiologic Studies Depression scale; R = respondent.
aEstimates are weighted using National Social Life, Health, and Aging Project W1 person-weights (adjusted for attrition and selection at W2). Estimates are calculated for all respondents who have nonmissing data for key variables in the final models for all outcome variables.
For each dependent variable, a second set of models include a set of life-course-related measures that capture later-life transitions that may be related to network change. Life-course factors include baseline marital status and change in marital status between waves, as well as baseline employment status and change in employment status (Table 1). These models also include measures of functional health, self-reported health, and depression. To measure functional impairment, I use an index comprised of seven items (α = .84) that assesses how much difficulty respondents have with everyday tasks (e.g., walking). Self-rated health is reported by respondents as “poor,” “fair,” “good,” “very good,” or “excellent.” Depressive symptoms are measured using a modified Center for Epidemiologic Studies Depression scale (CES-D-ml), which is the average of standardized responses to 10 ordinal items assessing depressive symptomology (α = .77). The CES-D-ml scale does not include one measure typically included in the CES-D, which asks respondents how often they feel “lonely,” which helps to avoid endogeneity (Cornwell & Waite, 2009).
Residential mobility is important to consider in any study of network change. The NSHAP included a leave-behind questionnaire (LBQ) that respondents could complete and mail in later. On this, respondents reported how long they had lived at their current residence. I use this to create an indicator of whether respondents moved during the past 5 years. Unfortunately, 286 respondents did not complete the LBQ and 69 others did not respond to the residence question, creating additional selection issues. Therefore, I use the residential mobility indicator only in a set of supplemental analyses (Supplementary Table A1).
All models take into account the clustering and stratification of NSHAP’s sample and include weights to account for respondents’ differential probabilities of selection at W1. I also take into account the nonrandom loss of respondents due to attrition between waves. I begin by creating a variable for each of the 3,005 W1 respondents that indicates whether they were part of the final W2 sample and in the final model for a given dependent variable. I predict this indicator using a logit model, with baseline sociodemographic variables, health, and other factors entered as predictors. From this, I derive a predicted probability that each W1 respondent appears in the analysis. I take the inverse of this probability and multiply it by the NSHAP-supplied weight for that person at W1. Using these adjusted weights as the sampling weights in the models give more weight to individuals who were less likely to be in the W2 sample, effectively adjusting estimates toward where they would have been had all W1 respondents made it into the W2 sample (see Austin, 2011).
Results
The data reveal considerable change within these older adults’ confidant networks over the 5-year study period. Of the 2,126 respondents who provided valid data, only 7.2% reported a completely stable confidant network that involved neither losses nor additions. In general, respondents were more likely to add confidants than to lose them. Fully 81.6% of the sample added at least one new confidant between waves, whereas 73.5% lost at least one confidant. The average number of confidants lost between waves was 1.48 (95% confidence interval [95% CI]: 1.40, 1.57), and the average number added was 1.90 (95% CI: 1.83, 1.97). Just over one fifth of respondents (21.9%) experienced the death of at least one confidant. All told, most older adults’ networks grew between waves, with an average net change in network size of 0.19 (95% CI: 0.12, 0.26).
Race/Ethnicity
Race/ethnicity plays an important role in several aspects of change within these older adults’ personal networks. Descriptively speaking, African Americans experienced more change than other groups. White respondents were 91.4% more likely than African Americans, and Latinos were 110.9% more likely than African Americans, to maintain the same exact confidant network over the 5-year period (Supplementary Figure A1). Whereas 7.6% of white respondents and 8.3% of Latinos reported neither losing W1 confidants nor adding new confidants at W2, only 4.0% of African American respondents did. Likewise, African American respondents were 10.8% more likely to experience turnover that involved both multiple confidants lost and multiple confidants gained than whites and 66.7% more likely than Latinos, with 44.1% of African Americans experiencing this level of turnover compared with 39.8% of whites and 26.4% of Latinos.
These patterns are also evident in the multivariate analysis. As shown in the first column of regression coefficients in Table 2, African Americans experienced a 22.0% higher rate of loss from their confidant networks than whites over the study period (incidence rate ratio [IRR] = 1.220, standard error [SE] = 0.052). This coefficient is reduced slightly but remains significant at p < .05 when life-course factors such as retirement, widowhood, and health are taken into account. These patterns reflect both losses due to the deaths of confidants and losses due to other reasons, such as residential mobility and job changes. That African Americans expensed a significantly higher rate of nondeath-related confidant losses is shown in the third and fourth columns of regression coefficients. But perhaps even more importantly, African Americans reported a significantly higher confidant mortality rate (IRR = 1.321, SE = 0.156). This difference remains marginally significant (p < .07) even after life-course (e.g., widowhood) and health covariates are taken into account.
Table 2.
Coefficients From Multivariate Regression Models Predicting Different Aspects of Network Turnover Among Older Adults
| Predictor | Poisson models predicting number of network members | OLS models predictinga change in network size | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Lost for any reasonb | Lost (but not died)b | Diedb | Addedc | |||||||
| Age (divided by 10) | 1.037 (0.021) | 1.046 (0.024) | 0.980 (0.022) | 1.013 (0.028) | 1.350*** (0.089) | 1.212** (0.075) | 1.016 (0.018) | 1.027 (0.022) | −0.093* (0.038) | −0.120** (0.041) |
| Female | 0.960 (0.031) | 0.903** (0.028) | 0.942 (0.031) | 0.908** (0.029) | 1.045 (0.119) | 0.887 (0.106) | 0.978 (0.026) | 0.955 (0.025) | 0.227*** (0.056) | 0.276*** (0.062) |
| African American | 1.220*** (0.052) | 1.171*** (0.049) | 1.197*** (0.056) | 1.149** (0.050) | 1.321* (0.156) | 1.271 (0.159) | 1.079* (0.035) | 1.058 (0.034) | −0.297**(0.101) | −0.281** (0.096) |
| Latino | 1.036 (0.081) | 1.010 (0.063) | 1.142 (0.094) | 1.108 (0.079) | 0.549* (0.136) | 0.542* (0.127) | 1.028 (0.042) | 1.009 (0.037) | −0.106 (0.114) | −0.111 (0.140) |
| Other race | 1.156 (0.173) | 1.132 (0.157) | 1.271 (0.181) | 1.222 (0.162) | 0.576 (0.305) | 0.605 (0.331) | 1.164 (0.120) | 1.159 (0.124) | 0.125 (0.187) | 0.107 (0.172) |
| ≤High school education | 1.141* (0.057) | 1.081 (0.052) | 1.100 (0.058) | 1.070 (0.057) | 1.375* (0.184) | 1.151 (0.155) | 1.045 (0.042) | 1.037 (0.041) | −0.215* (0.093) | −0.177 (0.088) |
| Some college | 1.058 (0.044) | 1.042 (0.042) | 1.036 (0.056) | 1.038 (0.055) | 1.193 (0.175) | 1.067 (0.184) | 1.054 (0.028) | 1.054 (0.028) | −0.047 (0.092) | −0.036 (0.088) |
| Retired (W1 and W2) | 0.894** (0.037) | 0.890* (0.043) | 0.928 (0.132) | 0.930* (0.027) | 0.128 (0.119) | |||||
| Other not working (W1 and W2) | 1.099 (0.070) | 1.074 (0.088) | 1.255 (0.216) | 0.985 (0.041) | −0.192 (0.137) | |||||
| Became retired | 1.000 (0.055) | 0.999 (0.055) | 1.025 (0.179) | 0.997 (0.031) | 0.119 (0.123) | |||||
| Stopped working for other reasons | 1.119 (0.078) | 1.208* (0.109) | 0.610 (0.258) | 1.147** (0.053) | 0.518* (0.198) | |||||
| Started working | 0.929 (0.088) | 0.979 (0.099) | 0.702 (0.160) | 0.883 (0.057) | −0.141 (0.191) | |||||
| Widowed (W1 and W2) | 1.122** (0.047) | 1.096 (0.053) | 1.292 (0.184) | 1.022 (0.037) | 0.039 (0.082) | |||||
| Unmarried (W1 and W2) | 1.154** (0.051) | 1.129* (0.054) | 1.309 (0.216) | 1.060 (0.037) | −0.056 (0.101) | |||||
| Became widowed | 1.609*** (0.068) | 1.116 (0.080) | 4.517*** (0.580) | 1.286*** (0.060) | −0.237 (0.158) | |||||
| Became unmarried | 1.460*** (0.116) | 1.443** (0.172) | 1.586 (0.682) | 1.278** (0.094) | −0.168 (0.221) | |||||
| Got married | 1.094 (0.111) | 1.121 (0.137) | 0.926 (0.375) | 1.005 (0.060) | 0.297 (0.279) | |||||
| Functional impairment | 0.993 (0.037) | 1.004 (0.057) | 0.944 (0.085) | 0.973 (0.025) | −0.012 (0.083) | |||||
| Overall self-rated health | 0.990 (0.017) | 0.999 (0.021) | 0.946 (0.052) | 1.005 (0.012) | 0.013 (0.035) | |||||
| Depressive symptoms (CES-D) | 1.037 (0.034) | 1.047 (0.046) | 0.986 (0.121) | 1.012 (0.033) | 0.007 (0.074) | |||||
| Constant | 1.025 (0.183) | 1.029 (0.228) | 1.410 (0.303) | 1.147 (0.293) | 0.017*** (0.012) | 0.041*** (0.028) | 0.591** (0.102) | 0.549** (0.117) | −0.657 (0.349) | −0.663 (0.367) |
| (Pseudo) R 2 | 0.427 | 0.453 | 0.367 | 0.376 | 0.091 | 0.163 | 0.530 | 0.538 | 0.367 | 0.376 |
| F | 27.47*** (11, 40) | 31.13*** (24, 27) | 17.11*** (11, 40) | 12.82*** (24, 27) | 11.24*** (11, 40) | 29.69*** (24, 27) | 58.55*** (15, 36) | 50.53*** (28, 23) | 74.96*** (15, 36) | 58.42*** (28, 23) |
| N | 2,124 | 2,124 | 2,124 | 2,113 | 2,124 | |||||
Notes. All models control for frequency of interaction with, emotional closeness to, and kin composition of W1 confidants, religious attendance, and the intercept. CES-D = CES-D = Center for Epidemiologic Studies Depression scale.
aCoefficients are unstandardized coefficients from OLS regressions, and standard errors are presented in parentheses below these estimates. Number of W1 confidants is controlled using a set of dummy variables indicating baseline network size.
bCoefficients are incidence rate ratios, and standard errors are presented in parentheses below these estimates. Number of W1 confidants is used as the exposure.
cCoefficients are incidence rate ratios, and standard errors are presented in parentheses. W2 network size is used as the exposure, and W1 network size is controlled using a set of dummy variables indicating baseline network size.
*p < .05. **p < .01. ***p < .001.
Note that Latinos report only about half the rate of confidant mortality as whites (IRR = 0.549, SE = 0.136), a difference that remains when other factors are controlled. This is the only significant association between Latino race/ethnicity and network change. These associations are similar (but stronger) in the supplemental analysis that includes information about residential mobility (Supplementary Table A1).
An important analytic issue is that these models suffer from endogeneity due to the fact that death is present on both sides of the equation for respondents who named their spouses as confidants at W1 and who became widowed between waves. A supplemental analysis (available upon request) shows that even among those who did not become widowed between waves, African Americans suffered significantly higher rates of confidant death than whites (IRR = 1.561, SE = 0.227) and Latinos experienced lower rates of confidant death (IRR = 0.448, SE = 0.105).
African Americans also report adding more new confidants than whites (IRR = 1.079, SE = 0.035). This association is reduced to nonsignificance and becomes marginally smaller (adjusted Wald F = 3.13, p < .08) when life-course factors are included. OLS regression analyses show that, in the end, African Americans experienced larger net losses in the sizes of their confidant networks than whites (b = −0.297, SE = 0.101), a difference that remains significant even after controlling for other covariates. This association is reinforced by the supplemental analysis that controls for residential mobility (Supplementary Table A1). The overall change in network size measure is difficult to interpret, however, as it is difficult to determine whether networks are actually growing or shrinking. A supplemental multinomial logit model that predict three possible trajectories of overall network change (shrinkage, stability, or growth) show that African Americans have about 73% greater risk than whites of experiencing network shrinkage as opposed to network stability (relative risk ratio [RRR] = 1.730, SE = 0.312), but there is no significant difference in their relative risk of network growth (RRR = 0.860, SE = 0.224).
Socioeconomic Status
Socioeconomic status is also associated with confidant network turnover. The main significant difference with respect to education appears in the analysis of network loss. As shown in Table 2, those who had nothing beyond a high school education lost their confidants at a 14.1% greater rate than those who earned college degrees (IRR = 1.141, SE = 0.057). This association becomes nonsignificant when life-course and health measures are taken into account. Although not one set of these measures accounts for the reduction in the association, the health measures alone reduce the association to nonsignificance and also significantly reduces the magnitude of the association (adjusted Wald F = 7.56, p < .01). There are no statistically significant differences between those who had some college but did not earn a degree and those who went on to earn a college degree.
There is a strong association between education and confidant mortality. The least-educated group experienced a 38.1% greater confidant mortality rate than those who earned college degrees (IRR = 1.381, SE = 0.185). It is worth noting that this association is explained by the marital status/transition measures. This is mainly attributable to the fact that less-educated individuals were more likely to become widowed during the study period. (However, a supplemental analysis, which is available upon request, shows that even among those who did not become widowed between waves, low-SES individuals experienced marginally higher rates of confidant death [IRR = 1.308, p =. 08].) Controlling for the health measures without controlling for life-course transitions also reduces the association with marginal significance. Supplemental analyses that take into account residential mobility (Supplementary Table A1) echo these findings.
Levels of formal education are not significantly associated with the addition of new confidants over the study period. The OLS regression analyses predicting overall network change show that, in the end, those with only a high school (or less) education had significantly more overall negative change in the sizes of their confidant networks than those who had a college degree (b = −0.215, SE = 0.093). This net difference in network size change remains nearly significant (p = .05) despite controlling for other covariates (b = −0.177, SE = 0.088). Note that the analysis shown in Supplementary Table A1 provides some evidence that those who had some college experienced more network growth than those who had a college degree. Additional analyses (not shown) suggest that finding is an artifact of the fact that less-educated people lost a greater proportion of their Wave 1 confidants, which left them more room in the roster to add confidants.
Stratified Network Loss
Although the earlier analyses provide some clues as to group differences in confidant network change, they are not definitive accounts of different groups’ experiences with network instability. Nonetheless, there are systematic differences in different groups’ reports of why their confidant networks changed. Unfortunately, the NSHAP did not inquire about how new confidant relationships were developed. But the team did inquire about “lost” network members. For any W1 confidant who was not named again at W2, respondents reported whether that person was still alive and, if so, why the relationship ended. Based on coding of these brief responses, the NSHAP team devised several broad classes of network loss. Key categories are presented in Table 3.
Table 3.
Distribution of Aspects of Confidant Network Change by Race/Ethnicity and Socioeconomic Status (N = 1,551)a
| Lost any confidant(s) for following reasonb | Race/ethnicity | Highest level of education | |||||||
|---|---|---|---|---|---|---|---|---|---|
| White | African American | Latino | Other | χ2 | ≤HS | Some college | College | χ2 | |
| R or confidant moved/now too “distant” | 31.5 | 36.9 | 57.5 | 51.7 | 19.67* | 31.4 | 32.7 | 36.7 | 6.21 |
| The confidant died | 30.6 | 34.9 | 14.4 | 12.2 | 35.59*** | 31.4 | 31.0 | 25.0 | 10.59 |
| They “drifted apart”/circumstances changed | 23.5 | 20.7 | 19.5 | 20.3 | 2.83 | 20.5 | 24.3 | 25.6 | 8.15 |
| R or confidant suffers from health problems | 12.4 | 10.8 | 6.4 | 19.4 | 9.87 | 12.8 | 12.7 | 10.1 | 3.68 |
| There was a falling out/disagreement/conflict | 7.9 | 10.6 | 4.1 | 2.1 | 10.05 | 6.4 | 8.4 | 9.5 | 6.98 |
| R or confidant retired or changed jobs | 6.1 | 2.9 | 1.2 | 3.9 | 12.49 | 1.7 | 7.0 | 10.2 | 71.59*** |
Notes. HS = high school; R = respondent.
aEstimates are weighted using National Social Life, Health, and Aging Project W1 person-weights and adjusted using propensity score weighting. Significance of group differences as indicated by chi-square statistics is determined using a design-corrected F-test.
bCategorization based on assessments of two independent coders (80.1% agreement). Estimates ignore those who had any trouble with the roster matching exercise or who had missing data on any alter. "Lost" confidants do not include those appearing in Roster B or C at W2.
*p < .05. ***p < .001.
Based on an analysis of the 1,551 individuals who experienced the loss of at least one confidant and who provided valid information about these losses, Table 3 shows some significant differences in causes of network loss. Perhaps the most important finding echoes the multivariate results just discussed—that African Americans were more likely than members of other race/ethnic groups to experience the death of a confidant. Specifically, 34.9% of African Americans who lost a confidant lost one due to death, compared with 30.6% of whites, 14.4% of Latinos, and 12.2% of members of other races. Although African Americans were more likely than whites to experience the loss of confidants due to residential mobility or some other distance issue (36.9% vs. 31.5%, respectively), Latinos (57.5%) and members of other race groups (51.7%) were more likely to experience loss due to this. With respect to SES, the biggest difference between groups is that more highly educated respondents were most likely to lose a confidant due to a job-related change, as opposed to some other cause such as death.
Conclusion
Motivated by the dual observations that social network change is pervasive and consequential in later life (Cornwell & Laumann, in press; Eng et al., 2002; Holtzman et al., 2004) and that members of socially disadvantaged groups face more instability in general in their everyday social environments (Ajrouch et al., 2001; Hawkins & Abrams, 2007; Peek & O’Neill, 2001; Shaw et al., 2007), this study has sought to assess the link between social disadvantage and personal network change. Members of disadvantaged groups indeed experience disproportionate amounts of change in their personal social networks in later life. Namely, African Americans and less-educated individuals lost more of their confidants over a 5-year period—especially due to death—than did whites and those who had college degrees, respectively. Interestingly, African Americans added network members at a greater rate than whites. Yet, neither African Americans nor low-SES individuals were able to match their substantial network losses with equal numbers of new additions to the same extent as others did, ultimately resulting in more network shrinkage and less network growth than was observed in other groups.
Thus, it appears that disadvantaged older adults have both a greater need to replace losses to their social networks that are associated with later-life transitions and greater difficulty in doing so. Indeed, these associations are partly due to socially disadvantaged groups’ worse health and greater likelihood of transitioning out of marriage—either due to divorce or widowhood. This finding highlights one way in which disadvantage accumulates in later life and how personal social networks are implicated in that process (see Dannefer, 2003). Unfortunately, significant differences between these groups with respect to rates of confidant network turnover remain unexplained. Additional work is needed to understand how processes of adaptation and compensation in late life (e.g., Atchley, 1989; Bloem et al., 2008; Heckhausen, 2006; Lamme et al., 1996; Zettel & Rook, 2004) are experienced by especially disadvantaged groups, such as impoverished African Americans.
A particularly disturbing finding is the strong associations between social disadvantage and confidant mortality. The greater propensity for less-educated individuals to experience this is partly but not entirely a reflection of their higher rates of widowhood. For one, variation in physical and mental well-being helps to explain the association between both education and race and confidant mortality. Furthermore, even those who did not become widowed experienced higher rates of confidant mortality than their more socially advantaged counterparts. These findings likely reflect the influence of network homophily (McPherson, Smith-Lovin, & Cook, 2001). We know that people disproportionately form network ties with others of similar race/ethnicity and SES, so the confidants of disadvantaged individuals (who are themselves less healthy) are also at greater risk of mortality. It is also possible that health-related homophily (see Flatt, Agimi, & Albert, 2012; Schaefer, Kornienko, & Fox, 2011) shapes older adults’ closest network connections. Regardless of the mechanism, these patterns reflect the segregation of disadvantaged groups into social environments that are inherently less stable (e.g., see Desmond, 2012b) and that are largely disconnected from the networks of more advantaged social groups. Socially disadvantaged people are disproportionally connected to more vulnerable confidants, which in turn means that there is premature depletion of disadvantaged older adults’ stock of healthy (potential) close social contacts, combined with limited capacity to cultivate new (healthy) ties. This has serious implications for these individuals’ abilities to access social support and other resources in the face of already difficult later-life challenges like widowhood and health decline.
When combined with mounting evidence that socially disadvantaged groups have less access to valuable forms of social capital (see Lin, 2000; McDonald, Lin, & Ao, 2009)—including in later life (Ajrouch et al., 2001)—the fact that the personal networks these groups do have are less stable suggests a precarious situation for aging African Americans and low-SES individuals. In light of the fact that social disadvantage is associated with less social capital (at the neighborhood level as well), which in turn is associated with higher rates of health problems and mortality (e.g., see Cattell, 2001; Kawachi et al., 1997; Mendes de Leon & Glass, 2004), social gerontologists should examine the possibility that social network instability is a mechanism by which race- and SES-based health disparities develop and widen. The fact that Latinos reported the lowest levels of network loss of any group in this sample provides additional impetus for this research direction, given ongoing attempts to understand the “Latino paradox” in health and mortality (Borrell & Lancet, 2012).
Finally, these findings add a twist to the debate over whether (older) individuals’ social networks are, on the whole, shrinking. McPherson, Smith-Lovin, and Brashears (2006) have argued that people’s confidant networks are growing smaller. Likewise, some social gerontologists have argued that older adults’ networks usually shrink, as they come to favor closer ties (see Charles & Carstensen, 2010) and have less incidental social contact (Marcum, 2013). My findings challenge these ideas in principle, as they show that older adults’ personal networks are actually more likely to grow in size than to decline overall (see also Fischer, 2009; Paik & Sanchagrin, 2013). This may be because, even though later life is period of loss and transition, older adults are adaptive and compensate for such losses (e.g., Bloem et al., 2008; Donnelly & Hinterlong, 2010) and may be inclined to socialize even more beyond this. What the findings presented here suggest is that the narrative of general network decline and later-life network shrinkage may be more valid for socially disadvantaged groups, who are likely less able to adapt to and compensate for network losses.
Supplementary Material
Supplementary material can be found at: http://psychsocgerontology.oxfordjournals.org/
Funding
The National Social Life, Health, and Aging Project is supported by the National Institutes of Health (R01AG021487, R37AG030481, R01AG033903), which also provided partial funding for this research.
Supplementary Material
Acknowledgments
I am indebted to Erin York Cornwell and anonymous reviewers for many useful suggestions that improved this article.
References
- Adler N. E., Rehkopf D. H. (2008). U.S. disparities in health: Descriptions, causes, and mechanisms. Annual Review of Public Health, 29, 235–252. :10.1146/annurev.publhealth.29.020907.090852 [DOI] [PubMed] [Google Scholar]
- Ajrouch K. J., Antonucci T. C., Janevic M. R. (2001). Social networks among blacks and whites: The interaction between race and age. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 56, S112–S118. :10.1093/geronb/56.2.S112 [DOI] [PubMed] [Google Scholar]
- Atchley R. C. (1989). A continuity theory of normal aging. The Gerontologist, 29, 183–190. :10.1093/geront/29.2.183 [DOI] [PubMed] [Google Scholar]
- Atkinson T., Liem R., Liem J. H. (1986). The social costs of unemployment: Implications for social support. Journal of Health and Social Behavior, 27, 317–331. :10.2307/2136947 [PubMed] [Google Scholar]
- Austin P. C. (2011). An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate Behavioral Research, 46, 399–424. :10.1080/ 00273171.2011.568786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bailey S., Marsden P. V. (1999). Interpretation and interview context: Examining the General Social Survey name generator using cognitive methods. Social Networks, 21, 287–309. :10.1016/S0378-8733(99)00013-1 [Google Scholar]
- Bloem B. A., van Tilburg T. G., Thomése F. (2008). Changes in older Dutch adults’ role networks after moving. Personal Relationships, 15, 465–478. :10.1111/j.1475-6811.2008.00210.x [Google Scholar]
- Borrell L. N., Lancet E. A. (2012). Race/ethnicity and all-cause mortality in US adults: Revisiting the Hispanic paradox. American Journal of Public Health, 102, 836–843. :10.2105/AJPH.2011.300345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burt R. S. (2005). Brokerage and closure: An introduction to social capital. Oxford: Oxford University Press. [Google Scholar]
- Cantor M. H. (1979). Neighbors and friends: An overlooked resource in the informal support system. Research on Aging, 1, 434–463. :10.1177/016402757914002 [Google Scholar]
- Carreon D., Noymer A. (2011). Health-related quality of life in older adults: Testing the double jeopardy hypothesis. Journal of Aging Studies, 25, 371–379. :10.1016/j.jaging.2011.01.004 [Google Scholar]
- Cattell V. (2001). Poor people, poor places, and poor health: The mediating role of social networks and social capital. Social Science & Medicine, 52, 1501–1516. :10.1016/S0277-9536(00)00259-8 [DOI] [PubMed] [Google Scholar]
- Charles S. T., Carstensen L. L. (2010). Social and emotional aging. Annual Review of Psychology, 61, 383–409. :10.1146/annurev.psych.093008.100448 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cornwell B. (2009). Good health and the bridging of structural holes. Social Networks, 31, 92–103. :10.1016/j.socnet.2008.10.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cornwell B. (2011). Independence through social networks: Bridging potential among older women and men. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 66, 782–794. :10.1093/geronb/gbr111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cornwell B., Laumann E. O.(in press). The health benefits of network growth: New evidence from a national survey of older adults. Social Science & Medicine. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cornwell B., Laumann E. O., Schumm L. P. (2008). The social connectedness of older adults: A national profile. American Sociological Review, 73, 185–203. :10.1177/000312240807300201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cumming E., Henry W. E. (1961). Growing old. New York, NY: Basic Books. [Google Scholar]
- Dannefer D. (1987). Aging as intracohort differentiation: Accentuation, the Matthew effect, and the life course. Sociological Forum, 2, 211–236. :10.1007/BF01124164 [Google Scholar]
- Dannefer D. (2003). Cumulative advantage/disadvantage and the life course: Cross-fertilizing age and social science theory. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 58, S327–S337. :10.1093/geronb/58.6.S327 [DOI] [PubMed] [Google Scholar]
- Deflem M. (1989). From anomie to anomia and anomic depression: A sociological critique on the use of anomie in psychiatric research. Social Science & Medicine, 29, 627–634. :10.1016/0277-9536(89)90182-2 [DOI] [PubMed] [Google Scholar]
- Desmond M. (2012a). Eviction and the reproduction of urban poverty. American Journal of Sociology, 118, 88–133. :10.1086/666082 [Google Scholar]
- Desmond M. (2012b). Disposable ties and the urban poor. American Journal of Sociology, 117, 1295–1335. :10.1086/663574 [Google Scholar]
- Donnelly E. A., Hinterlong J. E. (2010). Changes in social participation and volunteer activity among recently widowed older adults. The Gerontologist, 50, 158–169. :10.1093/geront/gnp103 [DOI] [PubMed] [Google Scholar]
- Eng P. M., Rimm E. B., Fitzmaurice G., Kawachi I. (2002). Social ties and change in social ties in relation to subsequent total and cause-specific mortality and coronary heart disease incidence in men. American Journal of Epidemiology, 155, 700–709. :10.1093/aje/155.8.700 [DOI] [PubMed] [Google Scholar]
- Fischer C. S. (2009). The 2004 GSS finding of shrunken social networks: An artifact? American Sociological Review, 74, 657–669. 10.1177/000312240907400408 [Google Scholar]
- Flatt J. D., Agimi Y., Albert S. M. (2012). Homophily and health behavior in social networks of older adults. Family & Community Health, 35, 312–321. :10.1097/FCH.0b013e3182666650 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerstorf D., Röcke C., Lachman M. E.(2011). Antecedent–consequent relations of perceived control to health and social support: Longitudinal evidence for between-domain associations across adulthood. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 66, 61–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giordano G. N., Lindstrom M. (2010). The impact of changes in different aspects of social capital and material conditions on self-rated health over time: A longitudinal cohort study. Social Science & Medicine, 70, 700–710. :10.1016/j.socscimed.2009.10.044 [DOI] [PubMed] [Google Scholar]
- Goffman A. (2009). On the run: Wanted men in a Philadelphia ghetto. American Sociological Review, 74, 339–357. :10.1177/000312240907400301 [Google Scholar]
- Hawkins R. L., Abrams C. (2007). Disappearing acts: The social networks of formerly homeless individuals with co-occurring disorders. Social Science & Medicine, 65, 2031–2042. :10.1016/j.socscimed.2007.06.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heckhausen J. (2006). Developmental regulation in adulthood: Age-normative and sociostructural constraints as adaptive challenges. Cambridge, UK: Cambridge University Press. [Google Scholar]
- Holt-Lunstad J., Smith T. B., Layton J. B. (2010). Social relationships and mortality risk: A meta-analytic review. PLoS Medicine, 7, e1000316. :10.1371/journal.pmed.1000316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holtzman R. E., Rebok G. W., Saczynski J. S., Kouzis A. C., Wilcox Doyle K., Eaton W. W. (2004). Social network characteristics and cognition in middle-aged and older adults. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 59, P278–P284. :10.1093/geronb/59.6.P278 [DOI] [PubMed] [Google Scholar]
- Kasarda J. D., Janowitz M. (1974). Community attachment in mass society. American Sociological Review, 39, 328–339. :10.2307/2094293 [Google Scholar]
- Kawachi I., Kennedy B. P., Lochner K., Prothrow-Stith D. (1997). Social capital, income inequality, and mortality. American Journal of Public Health, 87, 1491–1498. :10.2105/AJPH.87.9.1491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke C. H., Kubzansky L. D., Adler N., Kawachi I. (2008). Prospective change in health-related quality of life and subsequent mortality among middle-aged and older women. American Journal of Public Health, 98, 2085–2091. :10.2105/AJPH.2007.114041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lamme S., Dykstra P. A., van Groenou M. I. B. (1996). Rebuilding the network: New relationships in widowhood. Personal Relationships, 3, 337–349. :10.1111/j.1475-6811.1996.tb00120.x [Google Scholar]
- Lin N. (2000). Inequality in social capital. Contemporary Sociology, 29, 785–795. :10.2307/2654086 [Google Scholar]
- Link B. G., Phelan J. (1995). Social conditions as fundamental causes of disease. Journal of Health and Social Behavior, 35, 80–94. :10.2307/2626958 [PubMed] [Google Scholar]
- Marcum C. S. (2013). Age differences in daily social activities. Research on Aging, 35, 612–640. :10.1177/0164027512453468 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDonald S., Lin N., Ao D. (2009). Networks of opportunity: Gender, race, and job leads. Social Problems, 56, 385–402. :10.1525/sp.2009.56.3.385 [Google Scholar]
- McPherson M., Smith-Lovin L., Brashears M. (2006). Social isolation in America. American Sociological Review, 71, 353–375. 10.1177/000312240607100301 [Google Scholar]
- McPherson M., Smith-Lovin L., Cook J. M. (2001). Birds of a feather: Homophily in social networks. Annual Review of Sociology, 27, 415–444. :10.1146/annurev.soc.27.1.415 [Google Scholar]
- Mendes de Leon C. F., Glass T. A. (2004). The role of social and personal resources in ethnic disparities in late-life health. In N. B. Anderson, R. A. Bulatao, & B. Cohen (Eds.), Critical perspectives on racial and ethnic differences in health in late life (pp. 353–405). Washington, DC: National Research Council. [Google Scholar]
- Miller-Cribbs J. E., Farber N. B. (2008). Kin networks and poverty among African Americans: Past and present. Social Work, 53, 43–51. :10.1093/sw/53.1.43 [DOI] [PubMed] [Google Scholar]
- Paik A., Sanchagrin K. (2013). Social isolation in America: An artifact. American Sociological Review, 78, 339–360. 10.1177/0003122413482919 [Google Scholar]
- Peek M. K., O’Neill G. S. (2001). Networks in later life: An examination of race differences in social support networks. International Journal of Aging & Human Development, 52, 207–229. :10.2190/F1Q1-JV7D-VN77-L6WX [DOI] [PubMed] [Google Scholar]
- Perry B. L., Pescosolido B. A. (2012). Social network dynamics and biographical disruption: The case of “first-timers” with mental illness. American Journal of Sociology, 118, 134–175. :10.1086/666377 [Google Scholar]
- Pescosolido B. A. (1992). Beyond rational choice: The social dynamics of how people seek help. American Journal of Sociology, 97, 1096–1138. :10.1086/229863 [Google Scholar]
- Pillemer K., Suitor J. J. (1992). Violence and violent feelings: What causes them among family caregivers? Journal of Gerontology, 47, S165–S172. :10.1093/geronj/47.4.S165 [DOI] [PubMed] [Google Scholar]
- Rose D. R., Clear T. R. (1998). Incarceration, social capital, and crime: Implications for social disorganization theory. Criminology, 36, 441–480. :10.1111/j.1745-9125.1998.tb01255.x [Google Scholar]
- Schaefer D. R., Kornienko O., Fox A. M. (2011). Misery does not love company: Network selection mechanisms and depression homophily. American Sociological Review, 76, 764–785. :10.1177/0003122411420813 [Google Scholar]
- Schafer M. H. (2013). Structural advantages of good health in old age investigating the health-begets-position hypothesis with a full social network. Research on Aging, 35, 348–370. :10.1177/0164027512441612 [Google Scholar]
- Seeman T. E., Miller-Martinez D. M., Stein Merkin S., Lachman M. E., Tun P. A., Karlamangla A. S. (2011). Histories of social engagement and adult cognition: Midlife in the U.S. study. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 66, i141–i152. :10.1093/geronb/gbq091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw B. A., Krause N., Liang J., Bennett J. (2007). Tracking changes in social relations throughout late life. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 62, S90–S99. :10.1093/geronb/62.2.S90 [DOI] [PubMed] [Google Scholar]
- Small M. L. (2007). Racial differences in networks: Do neighborhood conditions matter? Social Science Quarterly, 88, 320–343. :10.1111/j.1540-6237.2007.00460.x [Google Scholar]
- Small M. L. (2009). Unanticipated gains: Origins of network inequality in everyday life. New York, NY: Oxford University Press. :10.1093/acprof:oso/9780195384352.001.0001 [Google Scholar]
- Smith K. P., Christakis N. A. (2008). Social networks and health. Annual Review of Sociology, 34, 405–429. :10.1146/annurev.soc.34.040507.134601 [Google Scholar]
- Smith S. S. (2007). Lone pursuit: Distrust and defensive individualism among the black poor. New York, NY: Russell Sage Foundation. [Google Scholar]
- Snijders T. A. B., Doreian P. (2010). Introduction to the special issue on network dynamics. Social Networks, 32, 1–3. :10.1016/j.socnet.2009.12.002 [Google Scholar]
- Stephens C., Alpass F., Towers A., Stevenson B. (2011). The effects of types of social networks, perceived social support, and loneliness on the health of older people: Accounting for the social context. Journal of Aging and Health, 23, 887–911. :10.1177/0898264311400189 [DOI] [PubMed] [Google Scholar]
- Thomas P. A. (2012). Trajectories of social engagement and mortality in late life. Journal of Aging and Health, 24, 547–568. :10.1177/0898264311432310 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Eijk G. (2010). Unequal networks: Spatial segregation, relationships and inequality in the city. Amsterdam, The Netherlands: IOS Press BV. [Google Scholar]
- van Tilburg T. (1998). Losing and gaining in old age: Changes in personal network size and social support in a four-year longitudinal study. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 53, S313–S323. :10.1093/geronb/53B.6.S313 [DOI] [PubMed] [Google Scholar]
- Wasserman S., Faust K. (1994). Social network analysis: Methods and applications. Cambridge, UK: Cambridge University Press. :10.1017/CBO9780511815478 [Google Scholar]
- Wellman B. (1983). Network analysis: Some basic principles. Sociological Theory, 1, 155–200. :10.2307/202050 [Google Scholar]
- Wellman B., Wong R. Y., Tindall D., Nazer N. (1997). A decade of network change: Turnover, persistence and stability in personal communities. Social Networks, 19, 27–50. :10.1016/S0378-8733(96)00289-4 [Google Scholar]
- Wellman B., Wortley S. (1990). Different strokes from different folks: Community ties and social support. American Journal of Sociology, 96, 558–588. :10.1086/229572 [Google Scholar]
- Williams D. R., Collins C. (1995). US socioeconomic and racial differences in health: Patterns and explanations. Annual Review of Sociology, 21, 349–386. :10.1146/annurev.so.21.080195. 002025 [Google Scholar]
- Wrzus C., Hänel M., Wagner J., Neyer F. J. (2013). Social network changes and life events across the life span: A meta-analysis. Psychological Bulletin, 139, 53–80. :10.1037/a0028601 [DOI] [PubMed] [Google Scholar]
- York Cornwell E. (2014). Social resources and disordered living conditions: Evidence from a national sample of community-residing older adults. Research on Aging, 36, 399–430. :10.1177/0164027513497369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- York Cornwell E., Waite L. J.(2009). Social disconnectedness, perceived isolation, and health among older adults. Journal of Health and Social Behavior, 50, 31–48. :10.1177/00221 4650905000103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zettel L. A., Rook K. S. (2004). Substitution and compensation in the social networks of older widowed women. Psychology and Aging, 19, 433–443. :10.1037/0882-7974.19.3.433 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


