Abstract
Rationale: Use of physical and/or occupational therapy in the intensive care unit (ICU) is safe, feasible, and demonstrates improvements in functional status with early administration. Access to physical and/or occupational therapy in the ICU is variable, with little known regarding its use in community ICUs.
Objectives: Determine what proportion of hospitals across Washington State report use of physical activity in mechanically ventilated patients and investigate process of care factors associated with reported activity delivery.
Methods: Cross-sectional telephone interview survey study of nurse managers in hospitals caring for patients on mechanical ventilation across Washington State in 2013. Survey responses were linked with hospital-level data available in the Washington State Department of Health Comprehensive Hospital Abstract Reporting System database. Chi-square testing was used to explore unadjusted associations between potential process of care factors and report on activity delivery. Two multivariable logistic regression models were developed to explore the association between presence of a mobility protocol and report on delivery of activity.
Measurements and Main Results: We identified 54 hospitals caring for patients on mechanical ventilation; 47 participated in the survey (response rate, 85.5%). Nurse managers from 36 (76.6%) hospitals reported use of physical activity in patients on mechanical ventilation, with 22 (46.8%) reporting use of high-level physical activity (transferring to chair, standing or ambulating) and 24 (51.1%) reporting use in high-severity patients (patients requiring mechanical ventilation and/or vasopressors). Presence of a written ICU activity protocol (odds ratio [OR], 5.54; 95% confidence interval [CI], 1.60–19.18; P = 0.006), hospital volume (OR, 5.33; 95% CI, 1.54–18.48; P = 0.008), and academic affiliation (OR, 4.40; 95% CI, 1.23–15.63; P = 0.02) were associated with report of higher level activity. Presence of a written ICU activity protocol (OR, 6.00; 95% CI, 1.69–21.14; P = 0.005) and academic affiliation (OR, 4.50; 95% CI, 1.21–16.46; P = 0.02) were associated with report of delivery of physical activity to high-severity patients.
Conclusions: Nurse managers at three-fourths (76.6%) of eligible hospitals across Washington State reported use of physical activity in patients on mechanical ventilation. Hospital-level factors including hospital volume, academic affiliation, and presence of a mobility protocol were associated with report of higher level activity and delivery of activity to high-severity patients.
Keywords: early mobilization, critical illness myopathy, physical therapy, intensive care unit–acquired weakness
Physical functional impairments are increasingly common sequelae after critical illness. Studies of critically ill patients hospitalized in the intensive care unit (ICU) for at least 7 days suggest that greater than one-fourth develop neuromuscular weakness attributable to the ICU stay (1–9). This disablement is associated with reductions in health-related quality of life, increased psychological distress, and delayed return to work (3–8) with impairments persisting for years after the index hospitalization.
Use of early physical activity, delivered within 48 hours of mechanical ventilation by a mobility team consisting of nurses and physical and/or occupational therapists is shown to reduce functional dependency at hospital discharge in patients recovering from acute respiratory failure (10–15). Early ICU activity is also associated with reductions in durations of delirium and mechanical ventilation and a trend toward decreased development of ICU-acquired weakness (15). Multiple studies demonstrate that early physical activity as an intervention is safe and feasible in critically patients, with few adverse effects (16–19). However, despite these potential benefits, adoption of early mobility into clinical practice remains poor and delivery of activity to patients on mechanical ventilation remains low. A single-day prevalence study across German ICUs reported that only 24% of a total of 185 patients receiving mechanical ventilation mobilized out of bed in a 24-hour study period (20). A similar single-day prevalence study across Australian and New Zealand ICUs reported that no patient among 224 requiring mechanical ventilation mobilized out of bed on the study date (21).
Data regarding the use of physical activity in ICUs across the United States remain limited to a small number of single academic center studies, most with targeted interest in mobility as an intervention. Little is known regarding the broader use in academic hospitals without an early ICU activity focus or in community hospitals. Understanding current use of ICU activity may inform broader implementation efforts aimed at enhancing delivery. Therefore, we sought to determine what proportion of hospitals caring for mechanically ventilated patients across Washington State use physical activity in the ICU and to identify process of care factors associated with reported activity delivery.
Methods
Study Design
We conducted a cross-sectional study of all nonfederal, nonchildren’s hospitals in Washington State caring for patients on mechanical ventilation between September 2012 and September 2013. Acute-care hospitals were identified via the Washington State Department of Health (DOH) hospital database and the Washington State Hospital Association hospital list. Hospitals that did not provide mechanical ventilation or provided short-term mechanical ventilation (defined as <24 h) before transfer to a higher level care facility were excluded from the analysis.
Questionnaire Development and Administration
A 28-item questionnaire (see the online supplement) was developed regarding physical activity practices in the ICU. Focus groups were conducted with critical care physicians, nurses, and physical therapists at Harborview Medical Center to aid in questionnaire development and pilot-tested with nurse managers from several nonmedical intensive care units at Harborview Medical Center before use.
A single nurse manager from the medical ICU at each eligible hospital was identified via the Washington State DOH and contacted via written letter for participation. We opted to focus on nurse managers for the interview because they are often responsible for unit-level quality assurance and maintain an up-to-date understanding of practices in their ICU. Telephone confirmation of participation was performed if no written response was received. The questionnaire was administered via script by a single investigator to each of the nurse managers with administration an average of 10 minutes. Hospital and ICU characteristics, including number of ICU beds, teaching affiliation, and care network participation were obtained from nurse manager questionnaires and confirmed for accuracy with publically available statistics from 2011 reported on the Washington State DOH website and the American Hospital Association website.
Physical Activity Definitions
Physical activity variables were obtained from nurse manager questionnaires. Physical activity was defined as any level of activity performed in the ICU beyond range of motion exercises. Our primary outcomes of interest were report of higher level activity for patients on mechanical ventilation and use of activity in patients with high illness severity. Nurse managers were asked to report whether certain activities occurred in their ICU for an average patient on mechanical ventilation (dangling, transferring from bed to chair, standing, and ambulating). An activity was reported to occur routinely if the nurse manager responded that it occurred on greater than one-third of the ICU days for an average patient. Hospitals were defined as delivering high-level activity if nurse managers reported mechanically ventilated patient participation in transferring from bed to chair, standing, or ambulating in the ICU. Hospitals were defined as delivering activity to high-severity patients if the nurse manager indicated that both patients on mechanical ventilation and those receiving vasopressor agents were eligible for participation in physical activity.
Hospital-Level Variables
Hospital characteristics were obtained from the Washington State DOH website and a publically available hospital database, the Comprehensive Hospital Reporting Abstract System (CHARS). This database is compiled by the Washington State DOH annually, on the basis of hospital-reported data. Number of hospital beds, number of acute-care patient-days, and number of ICU patient-days were obtained from the 2011 hospital DOH end-of-year report. One participating hospital did not report 2011 data. Data from the 2010 hospital DOH end-of-year report was used in this case. One hospital did not report data to the DOH in either 2010 or 2011 and was treated as missing data for this analysis. Hospital volume was dichotomized as less than 20,000 and 20,000+ acute-care patient-days/year, based on the median value for the hospital cohort. Likewise, ICU volume was dichotomized as less than 5,000 and 5,000+ ICU patient-days/year.
We identified the following hospital-level factors, a priori, as potential covariates of interest for report of high-level activity and/or delivery of activity to high-severity patients: presence of written activity protocol, academic ICU, intensivist-led ICU, membership in a hospital network, hospital and ICU volume, presence of advanced care providers, use of computer order entry in the ICU, and report of staffing or sedation as a barrier to activity. An intensivist was defined as a physician who was board eligible or board certified in critical care medicine (22). An academic ICU was defined as any ICU reporting a teaching affiliation (report of presence of resident physicians rotating in the ICU) subsequently confirmed on the American Hospital Association website. Membership in a hospital network was defined as an entity operating two or more hospitals in Washington State or an adjacent metro area.
The University of Washington Institutional Review Board reviewed the study and determined the study was human subjects exempt.
Statistical Analysis
Hospital and ICU characteristics were summarized using proportions for categorical variables. In unadjusted analysis, we used chi-square testing to investigate associations between our hospital-level covariates and receipt of higher level activity or use of activity in high-severity patients.
Multivariable logistic regression was used to model the relationship between presence of a protocol and report of higher level activity or reported delivery of activity to high-risk patients (in separate models). Hospital-level factors chosen a priori were explored including hospital and ICU volume, teaching hospital status, open ICU, and participation in a care network. Hospital and ICU volume demonstrated colinearity. Given concerns for multiple comparisons with increasing model parameters, hospital volume was chosen as the summary measure for care volume in final models. A two-sided P value less than 0.05 was used to denote statistical significance. Hospital-level factors identified as significant in unadjusted analysis were included in the multivariable models to determine whether any factors were independently associated with report of activity. All statistical tests were performed with STATA version 13.0 (StataCorp, College Station, TX).
Results
Hospital Sample
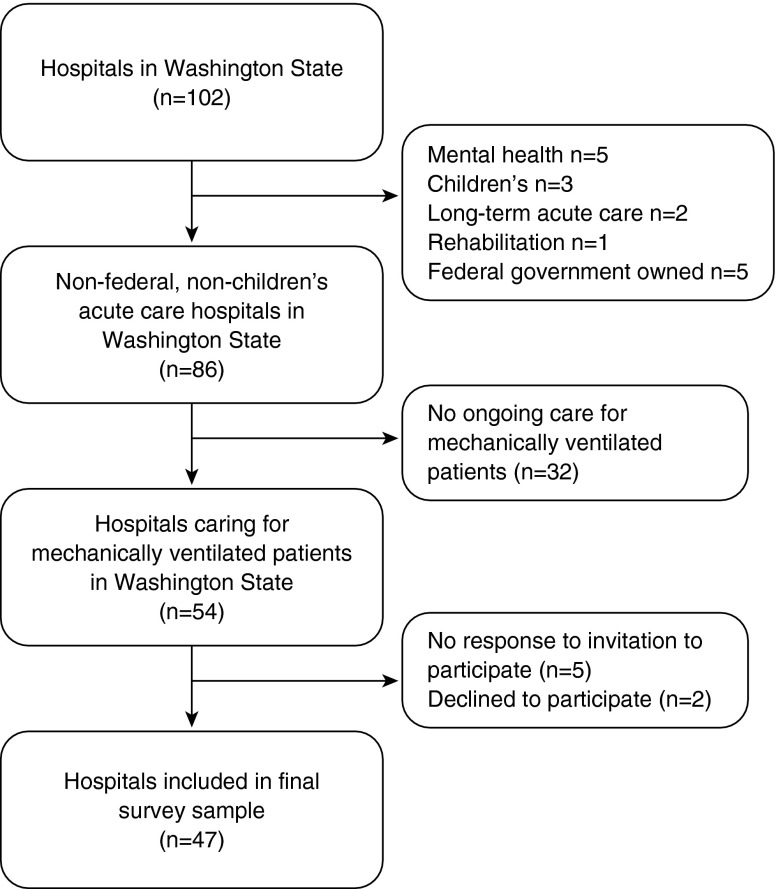
A total of 102 hospitals in Washington were identified. Of these, 86 were nonfederal, nonchildren’s hospitals. Thirty-two hospitals (37.2%) did not provide ongoing care for patients on mechanical ventilation; all but 1 of these 32 were critical access hospitals (defined as caring for fewer than 25 patients). The remaining 54 hospitals were contacted for possible participation (Figure 1). Five hospitals (9.1%) failed to reply to the written invitation and were unreachable for confirmation of participation. Two hospitals (4%) declined to participate. A total of 47 hospitals were included in the final analysis representing 87% of the hospitals caring for mechanically ventilated patients across Washington State.
Figure 1.
Hospital cohort derivation.
Characteristics of the 47 participating ICUs are summarized in Table 1. ICUs varied in size from 4 to 46 beds with a median of 14 beds. ICUs with higher patient volume (>5,000 ICU patient-days/yr) were more likely to be a teaching status ICU (OR, 11.38; 95% CI, 2.67–47.40; P = 0.006). Larger volume hospitals (>20,000 acute-care patient-days/yr) were more likely to be part of a larger hospital network (OR, 4.40; 95% CI, 1.30–15.16; P = 0.02) and to have an academic affiliation (OR, 13.3; 95% CI, 2.72–23.89; P = 0.006).
Table 1.
Participating hospital intensive care unit characteristics
| n (%) | |
|---|---|
| Number of ICU beds | |
| 0–10 | 19 (40.5) |
| 11–20 | 16 (34.0) |
| >20 | 12 (25.5) |
| Number of ICUs in hospital | |
| 1 | 38 (80.9) |
| 2–4 | 9 (20.1) |
| Primary medical ICU | 46 (97.9) |
| Other patient populations cared for in ICU | |
| Postsurgical | 43 (91.5) |
| Trauma | 21 (44.7) |
| Neurology | 24 (51.1) |
| Neurosurgery | 18 (40.0) |
| Cardiac | 38 (80.9) |
| Post-transplant | 4 (8.9) |
| Academic ICU | 17 (30.4) |
| Critical care physicians only in the ICU | 8 (17.0) |
| Advanced care providers practicing in the ICU | 28 (59.6) |
Definition of abbreviation: ICU = intensive care unit.
Missing hospitals included two critical access hospitals both with fewer than 10 ICU beds, four hospitals with 10–20 ICU beds, and two hospitals with more than 20 ICU beds. Three of the missing hospitals were part of a larger hospital network (defined as an entity operating two or more hospitals in Washington State). Hospital networks that included the missing hospitals were represented by other hospitals that participated in the study.
Use of Physical Activity in the ICU
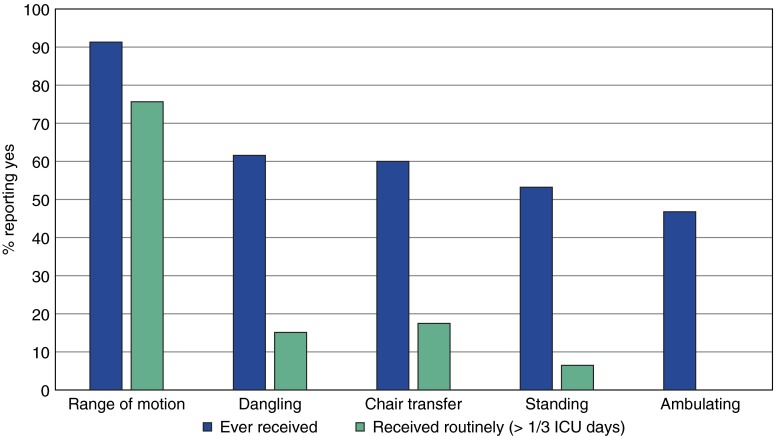
Nurse managers from 45 hospitals (95.7%) reported use of any physical activity (defined as activity beyond passive range motion) to any patients (nonmechanically ventilated and/or mechanically ventilated) within their ICU. Thirty-six nurse managers (76.6%) reported use of physical activity in patients on mechanical ventilation. Frequency and levels of reported activity for patients on mechanical ventilation are presented in Figure 2.
Figure 2.
Reported frequency of physical activity for patients on mechanical ventilation (MV). Twenty-two nurse managers (46.8%) reported use of higher level physical activity (out of bed to chair, standing, or ambulating) ever in patients on mechanical ventilation. Only three hospitals (6.4%) reported that patients on MV stood out of bed routinely (more than one-third of ICU days) and none (0.0%) reported routine ambulation for patients on MV. ICU = intensive care unit.
In hospitals reporting use of physical activity in the ICU, 93.6% (n = 44) indicated that physical and/or occupational therapists (PT/OTs) participated in physical activity sessions within the ICU. Nearly half of all activity reported for patients on mechanical ventilation occurred with both PT/OT and bedside nursing present (dangle [14 of 29, 48%], standing [11 of 25, 44%], walking [11 of 22, 50%]); chair transfers occurred with equal frequency by nursing alone or a combination of nursing and PT/OT (13 of 28; 46%, respectively). Most levels of activity for patients on mechanical ventilation were led by a PT/OT (dangling [17 of 29, 59%], chair transfer [15 of 28, 54%], standing [17 of 25, 68%], walking [14 of 22, 64%]). Twenty-nine hospitals (63.8%) reported a mechanism for screening ICU patients for participation in physical activity in the ICU, with most screening performed by the bedside nurse (38.3%) or a physical or occupational therapist (36.2%). Less than half of all participating hospitals (44.4%, n = 20) reported the use of a written protocol for physical activity in the ICU. Physicians remained responsible for initiation of activity, with a physician order in 82.2% of hospitals sampled.
Factors Associated with High-Level Activity
Twenty-two hospital nurse managers (46.8%) reported delivery of high-level activity (defined as out of bed to a chair, standing/marching in place, or ambulation) for patients on mechanical ventilation in their ICUs. Larger volume hospitals (OR, 5.33; 95% CI, 1.54–18.48; P = 0.008) and ICUs (OR, 5.20; 95% CI, 1.51–17.93; P = 0.008) and academic ICUs (OR, 4.40; 95% CI, 1.23–15.63; P = 0.02) were more likely to report delivery of higher level physical activity. Unadjusted associations between hospital-level process of care factors and report of delivery of higher ICU physical activity are reported in Table 2. Presence of a written protocol, hospital volume, ICU volume, teaching status ICU, and the presence of advanced care providers in the ICU were associated with report of higher level physical activity in the ICU. Adjusting for academic ICU affiliation and hospital volume, presence of a written protocol remained associated with report of higher level activity (OR, 5.26; 95% CI, 1.23–22.55; P = 0.025) although the stability of this estimate is uncertain given the small sample size.
Table 2.
Associations between hospital process-structure factors and reported delivery of high-level activity to patients on mechanical ventilation
| High-Level Activity Hospitals (n = 22) | OR | 95% CI | P Value | |
|---|---|---|---|---|
| Hospital volume >20,000 patient-days/yr, n (%) | 16 (72.7) | 5.33 | 1.54–18.48 | 0.008 |
| ICU volume >5,000 patient-days/yr, n (%) | 15 (68.2) | 5.20 | 1.51–17.93 | 0.008 |
| Part of a larger hospital network, n (%) | 13 (59.1) | 2.57 | 0.80–8.21 | 0.11 |
| Academic ICU, n (%) | 11 (52.4) | 4.40 | 1.23–15.63 | 0.02 |
| Intensivist-led ICU, n (%) | 4 (18.2) | 1.17 | 0.28–4.94 | 0.84 |
| Advanced care providers in ICU, n (%) | 17 (77.3) | 4.33 | 1.24–14.93 | 0.02 |
| Computerized order entry, n (%) | 17 (77.3) | 1.32 | 0.37–4.75 | 0.68 |
| Written protocol for ICU activity, n (%) | 14 (63.6) | 5.54 | 1.60–19.18 | 0.006 |
Definition of abbreviations: CI = confidence interval; ICU = intensive care unit; OR = odds ratio.
Factors Associated with Activity in High-Severity Patients
At a total of 24 hospitals (51.1%), nurse managers reported use of delivery of physical activity to patients on mechanical ventilation and vasopressor agents (high severity). Reported delivery of physical activity to higher severity patients did not differ by hospital (OR, 1.42; 95% CI, 0.45–4.46; P = 0.56) or ICU volume (OR, 2.02; 95% CI, 0.63–6.44; P = 0.24). Academic ICUs were more likely to report use of physical activity for high-severity patients in the ICU (OR, 4.5; 95% CI, 1.21–16.46; P = 0.02). Unadjusted associations between hospital-level process of care factors and report of ICU physical activity delivery to high-severity patients are reported in Table 3. Presence of a written activity protocol and being an academic ICU were associated with report of activity to high-severity patients. Adjusting for hospital volume and teaching status, presence of a protocol remained independently associated with report of activity to high-severity patients (OR, 6.64; 95% CI, 1.52–29.08; P = 0.012).
Table 3.
Associations between hospital process-structure factors of hospitals reporting delivery of activity to high-severity patients in the intensive care unit
| Delivery to High-Severity Patients (n = 24) | OR | 95% CI | P Value | |
|---|---|---|---|---|
| Hospital volume >20,000 patient-days/yr, n (%) | 16 (72.7) | 1.41 | 0.45–4.46 | 0.56 |
| ICU volume >5,000 patient-days/yr, n (%) | 15 (68.2) | 2.02 | 0.63–6.44 | 0.24 |
| Part of a larger hospital network, n (%) | 13 (54.2) | 1.84 | 0.59–5.77 | 0.30 |
| Academic ICU, n (%) | 9 (37.5) | 4.50 | 1.21–16.47 | 0.02 |
| Intensivist-led ICU, n (%) | 23 (95.8) | 4.72 | 0.74–30.06 | 0.02 |
| Advanced care providers in ICU, n (%) | 18 (75.0) | 3.90 | 1.15–13.13 | 0.03 |
| Computerized order entry, n (%) | 18 (75.0) | 1.06 | 0.30–3.78 | 0.93 |
| Written protocol for ICU activity, n (%) | 15 (62.5) | 6.00 | 1.69–21.14 | 0.005 |
Definition of abbreviations: CI = confidence interval; ICU = intensive care unit; OR = odds ratio.
Reported Barriers to Delivery of ICU Activity
At 31 hospitals (67.4%), nurse managers reported sedation as a barrier to delivery of physical activity in the ICU. Nurse mangers from 24 hospitals (51.1%) reported staffing as a limitation to delivery of physical activity to all patients in the ICU. Nurse managers who reported sedation was a barrier to ICU activity were not more likely to report lower level activity in the ICU (OR, 1.34; 95% CI, 0.41–4.65; P = 0.60). There was a trend toward an association between lack of activity among high-risk patients in hospitals indicating staffing limitations (OR, 3.13; 95% CI, 0.97–10.11; P = 0.06), but no association was found between indication of staffing limitations and delivery of higher level activity (OR, 1.08; 95% CI, 0.35–3.36; P = 0.9).
Discussion
In a large state-wide cohort of hospitals caring for mechanically ventilated patients across Washington State, we found that nearly all hospitals (95.7%) reported use of physical activity in nonmechanically ventilated patients in the ICU, with 76.6% reporting use in mechanically ventilated patients. Most hospitals required a physician order for initiation of physical activity. Several hospital-level factors including presence of a mobility protocol, hospital volume, and ICU academic affiliation were associated with report of higher level activity and delivery of activity to patients on mechanical ventilation and vasoactive agents.
Current data regarding use of physical activity in the ICU in the United States remain limited to single, primarily academic centers, many with particular research interest in early ICU mobilization (15, 17, 18, 23). Our study expands on our current knowledge by attempting to understand implementation of ICU activity out of academic centers. In our study, 66% of community-based nurse managers reported that physical activities beyond range of motion are provided to patients on mechanical ventilation. These events were reportedly performed by a variety of care teams, with nearly half of all events led by a multidisciplinary team with both nursing and PT/OT involvement. Although most studies of ICU activity, to date, have focused on PT/OT-delivered therapy, we found that mobility care teams vary in community practice. Nursing-driven ICU mobility represents a more feasible and generalizable care model. A study of implementation of the Awakening, Breathing Coordination, Delirium Management, and Early Mobilization “ABCDE” bundle, which includes early mobilization, demonstrated improved outcomes with primarily nursing-driven care (24). Studies are needed to assess the effectiveness of nursing-led ICU activity compared with PT/OT-led activity.
It remains unclear to what degree this report translates into actual ICU activity in clinical practice. Point prevalence studies suggest that actual performance of physical activity is low. A German point prevalence study of academic and community hospitals reported that only 8% of patients on mechanical ventilation received higher level physical activity, and a similar study across Australia/New Zealand found that no patients on mechanical activity were mobilized out of bed (20, 21). Further studies are needed to understand to what degree nurse manager or medical ICU leadership report correlates to clinical practice of ICU mobility and to measure provision of ICU mobility using activity point prevalence estimates across U.S. academic and community hospitals.
The presence of a mobility protocol was associated with report of delivery of activity to higher severity patients and higher level activity for mechanically ventilated patients. An increasing number of studies have suggested that use of protocols for delivery of critical care improves intervention use and patient outcomes. Brook and colleagues reported in a randomized controlled trial that nurse-driven sedation via a dedicated sedation protocol resulted in shorter durations of mechanical ventilation and reductions in hospital and ICU length of stay (25). Additional studies have confirmed these findings, suggesting that use of a dedicated protocol may serve as a means of changing clinical practice. In our study, however, less than half of the hospitals (n = 20, 44%) reported use of a dedicated ICU protocol for physical activity. This mobility protocol use is slightly higher than estimates of mobility protocol use across U.S. hospitals. A study completed by the U.S. Critical Care Trials Group across 69 primarily academic hospitals reported that 36% of the participating hospitals used a mobility protocol (26). Protocols for ventilator management, infection control, and venous thromboembolism were universally adopted in 97–99% of hospitals. The presence of a mobility protocol may serve as a modifiable means of increasing access to physical activity in critically ill patients. Future studies should aim to understand barriers to broader implementation of ICU activity protocols in clinical practice and to better understand the relationship between having a protocol and delivery of documented physical activity.
Hospital and ICU volume were associated with report of higher level physical activity in our study. Numerous studies demonstrate associations between larger hospital volume and better patient outcomes (27–29). In addition, more recent studies suggest that hospital volume may serve as a surrogate for overall hospital participation in quality improvement initiatives. In a study of sedation and analgesia order set implementation and quality across Washington State, hospital volume was independently associated with a higher sedation/analgesia order set quality score (22). The finding that hospital volume is also associated with report of higher level ICU activity in Washington hospitals likely results in part from larger hospitals implementing higher quality sedation order sets, as mobility use is often linked to levels of sedation (16, 19, 30). Care bundles that have linked sedation and mobility, such as the “ABCDE” bundle proposed by Ely and colleagues, may result in greater adoption of mobility as an intervention (31–33).
Finally, academic ICU status was also associated with report of higher level activity and report of delivery of activity to higher severity patients in our cohort. This association is potentially expected given that most literature regarding use of ICU activity is derived from academic medical centers. However, to our knowledge, no data exist regarding factors associated with the implementation of critical care interventions outside of academic settings into community clinical practice. Further studies are needed to understand mechanisms for community-based participatory research of critical care therapies.
Our study has some important limitations. First, our study examined nurse manager report of activity rather than actual physical activity in the ICU. It is possible that nurse managers who work at hospitals with an ICU activity protocol are more likely to report higher level activity. Studies are needed linking survey response from ICU leadership (nurse managers and medical directors) to clinical practice to better understand the correlations between survey report and true practice in critical care. Second, it is not possible to determine whether the association we identified results from development of protocols in hospitals already using physical activity in the ICU or whether the development of the protocol leads to greater delivery of physical activity, given the cross-sectional nature of our study design. However, the presence of a protocol may serve as a means to organize practice and decrease variation in care delivery. Our study is underpowered to investigate effects with multiple adjustments. It is possible that hospital volume, teaching ICU status, and presence of a protocol serve as mediators of physical activity, but we are unable to fully explore these relationships in our current study. Further study is needed to understand the manner by which organizational factors exert their effects in complex critical care interventions. Finally, our study reports the results of a single state’s experience with ICU activity in hospitals caring for mechanically ventilated patients. Therefore, our results may not be generalizable to other states or regions of the country. However, Washington is the thirteenth most populated state in the United States, thereby providing a reasonably heterogeneous sample of rural and urban hospitals caring for mechanically ventilated patients.
Conclusions
In this statewide cohort of hospitals caring for mechanically ventilated patients, we found that most hospitals report use of physical activity for patients in the ICU. Nurse managers from less than half of the participating hospitals reported use of a dedicated ICU activity protocol. Use of a protocol was statistically significantly associated with report of higher level activity and delivery of activity to higher severity patients. Hospital volume and academic affiliation were associated with report of higher level activity, and academic affiliation was associated with report of activity to higher severity patients. Further studies are needed to explore the relationship between mobility protocols and delivery of ICU mobility and to determine whether protocols serve as a modifiable mechanism for increasing access to ICU activity.
Footnotes
Supported by NIH T32 training grant HL007287-31.
Author Contributions: S.E.J., C.R.D., and C.L.H. participated in the design of the study and study materials. All authors participated in drafting of the manuscript and approved its submission for publication.
This article has an online supplement, which is accessible from this issue’s table of contents online at www.atsjournals.org
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1.De Jonghe B, Sharshar T, Lefaucheur JP, Authier FJ, Durand-Zaleski I, Boussarsar M, Cerf C, Renaud E, Mesrati F, Carlet J, et al. Groupe de Réflexion et d’Etude des Neuromyopathies en Réanimation. Paresis acquired in the intensive care unit: a prospective multicenter study. JAMA. 2002;288:2859–2867. doi: 10.1001/jama.288.22.2859. [DOI] [PubMed] [Google Scholar]
- 2.Hough CL. Neuromuscular sequelae in survivors of acute lung injury [abstract] Clin Chest Med. 2006;27:691–703. doi: 10.1016/j.ccm.2006.07.002. [DOI] [PubMed] [Google Scholar]
- 3.Barnato AE, Albert SM, Angus DC, Lave JR, Degenholtz HB. Disability among elderly survivors of mechanical ventilation. Am J Respir Crit Care Med. 2011;183:1037–1042. doi: 10.1164/rccm.201002-0301OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bienvenu OJ, Colantuoni E, Mendez-Tellez PA, Dinglas VD, Shanholtz C, Husain N, Dennison CR, Herridge MS, Pronovost PJ, Needham DM. Depressive symptoms and impaired physical function after acute lung injury: a 2-year longitudinal study. Am J Respir Crit Care Med. 2012;185:517–524. doi: 10.1164/rccm.201103-0503OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Davydow DS, Hough CL, Russo JE, Von Korff M, Ludman E, Lin EH, Ciechanowski P, Young B, Oliver M, Katon WJ. The association between intensive care unit admission and subsequent depression in patients with diabetes. Int J Geriatr Psychiatry. 2012;27:22–30. doi: 10.1002/gps.2684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dowdy DW, Eid MP, Dennison CR, Mendez-Tellez PA, Herridge MS, Guallar E, Pronovost PJ, Needham DM. Quality of life after acute respiratory distress syndrome: a meta-analysis. Intensive Care Med. 2006;32:1115–1124. doi: 10.1007/s00134-006-0217-3. [DOI] [PubMed] [Google Scholar]
- 7.Hopkins RO, Weaver LK, Collingridge D, Parkinson RB, Chan KJ, Orme JF., Jr Two-year cognitive, emotional, and quality-of-life outcomes in acute respiratory distress syndrome. Am J Respir Crit Care Med. 2005;171:340–347. doi: 10.1164/rccm.200406-763OC. [DOI] [PubMed] [Google Scholar]
- 8.Unroe M, Kahn JM, Carson SS, Govert JA, Martinu T, Sathy SJ, Clay AS, Chia J, Gray A, Tulsky JA, et al. One-year trajectories of care and resource utilization for recipients of prolonged mechanical ventilation: a cohort study. Ann Intern Med. 2010;153:167–175. doi: 10.1059/0003-4819-153-3-201008030-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Batt J, dos Santos CC, Cameron JI, Herridge MS. Intensive care unit-acquired weakness: clinical phenotypes and molecular mechanisms. Am J Respir Crit Care Med. 2013;187:238–246. doi: 10.1164/rccm.201205-0954SO. [DOI] [PubMed] [Google Scholar]
- 10.Chen S, Su CL, Wu YT, Wang LY, Wu CP, Wu HD, Chiang LL. Physical training is beneficial to functional status and survival in patients with prolonged mechanical ventilation. J Formos Med Assoc. 2011;110:572–579. doi: 10.1016/j.jfma.2011.07.008. [DOI] [PubMed] [Google Scholar]
- 11.Chiang LL, Wang LY, Wu CP, Wu HD, Wu YT. Effects of physical training on functional status in patients with prolonged mechanical ventilation. Phys Ther. 2006;86:1271–1281. doi: 10.2522/ptj.20050036. [DOI] [PubMed] [Google Scholar]
- 12.Clini E, Ambrosino N. Early physiotherapy in the respiratory intensive care unit. Respir Med. 2005;99:1096–1104. doi: 10.1016/j.rmed.2005.02.024. [DOI] [PubMed] [Google Scholar]
- 13.Kress JP. Clinical trials of early mobilization of critically ill patients. Crit Care Med. 2009;37(10) Suppl:S442–S447. doi: 10.1097/CCM.0b013e3181b6f9c0. [DOI] [PubMed] [Google Scholar]
- 14.Morris PE, Griffin L, Berry M, Thompson C, Hite RD, Winkelman C, Hopkins RO, Ross A, Dixon L, Leach S, et al. Receiving early mobility during an intensive care unit admission is a predictor of improved outcomes in acute respiratory failure. Am J Med Sci. 2011;341:373–377. doi: 10.1097/MAJ.0b013e31820ab4f6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schweickert WD, Pohlman MC, Pohlman AS, Nigos C, Pawlik AJ, Esbrook CL, Spears L, Miller M, Franczyk M, Deprizio D, et al. Early physical and occupational therapy in mechanically ventilated, critically ill patients: a randomised controlled trial. Lancet. 2009;373:1874–1882. doi: 10.1016/S0140-6736(09)60658-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bailey PP, Miller RR, III, Clemmer TP. Culture of early mobility in mechanically ventilated patients. Crit Care Med. 2009;37:S429–S435. doi: 10.1097/CCM.0b013e3181b6e227. [DOI] [PubMed] [Google Scholar]
- 17.Morris PE, Goad A, Thompson C, Taylor K, Harry B, Passmore L, Ross A, Anderson L, Baker S, Sanchez M, et al. Early intensive care unit mobility therapy in the treatment of acute respiratory failure. Crit Care Med. 2008;36:2238–2243. doi: 10.1097/CCM.0b013e318180b90e. [DOI] [PubMed] [Google Scholar]
- 18.Needham DM, Korupolu R, Zanni JM, Pradhan P, Colantuoni E, Palmer JB, Brower RG, Fan E. Early physical medicine and rehabilitation for patients with acute respiratory failure: a quality improvement project. Arch Phys Med Rehabil. 2010;91:536–542. doi: 10.1016/j.apmr.2010.01.002. [DOI] [PubMed] [Google Scholar]
- 19.Zanni JM, Korupolu R, Fan E, Pradhan P, Janjua K, Palmer JB, Brower RG, Needham DM. Rehabilitation therapy and outcomes in acute respiratory failure: an observational pilot project. J Crit Care. 2010;25:254–262. doi: 10.1016/j.jcrc.2009.10.010. [DOI] [PubMed] [Google Scholar]
- 20.Nydahl P, Parker Ruhl A, Bartoszek G, Dubb R, Filipovic S, Flohr H, Kaltwasser A, Mende H, Rothaug O, Schuchhardt D, et al. Early mobilization of mechanically ventilated patients: a 1-day point-prevalence study in Germany. Crit Care Med. 2013;42:1178–1186. doi: 10.1097/CCM.0000000000000149. [DOI] [PubMed] [Google Scholar]
- 21.Berney SC, Harrold M, Webb SA, Seppelt I, Patman S, Thomas PJ, Denehy L. Intensive care unit mobility practices in Australia and New Zealand: a point prevalence study. Crit Care Resusc. 2013;15:260–265. [PubMed] [Google Scholar]
- 22.Dale CR, Hayden SJ, Treggiari MM, Curtis JR, Seymour CW, Yanez ND, III, Fan VS. Association between hospital volume and network membership and an analgesia, sedation and delirium order set quality score: a cohort study. Crit Care. 2012;16:R106. doi: 10.1186/cc11390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bailey P, Thomsen GE, Spuhler VJ, Blair R, Jewkes J, Bezdjian L, Veale K, Rodriquez L, Hopkins RO. Early activity is feasible and safe in respiratory failure patients. Crit Care Med. 2007;35:139–145. doi: 10.1097/01.CCM.0000251130.69568.87. [DOI] [PubMed] [Google Scholar]
- 24.Balas MC, Burke WJ, Gannon D, Cohen MZ, Colburn L, Bevil C, Franz D, Olsen KM, Ely EW, Vasilevskis EE. Implementing the awakening and breathing coordination, delirium monitoring/management, and early exercise/mobility bundle into everyday care: opportunities, challenges, and lessons learned for implementing the ICU Pain, Agitation, and Delirium Guidelines. Crit Care Med. 2013;41(9) Suppl 1:S116–S127. doi: 10.1097/CCM.0b013e3182a17064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Brook AD, Ahrens TS, Schaiff R, Prentice D, Sherman G, Shannon W, Kollef MH. Effect of a nursing-implemented sedation protocol on the duration of mechanical ventilation. Crit Care Med. 1999;27:2609–2615. doi: 10.1097/00003246-199912000-00001. [DOI] [PubMed] [Google Scholar]
- 26.Checkley W, Martin GS, Brown SM, Chang SY, Dabbagh O, Fremont RD, Girard TD, Rice TW, Howell MD, Johnson SB, et al. United States Critical Illness and Injury Trials Group Critical Illness Outcomes Study Investigators. Structure, process, and annual ICU mortality across 69 centers: United States critical illness and injury trials group critical illness outcomes study. Crit Care Med. 2014;42:344–356. doi: 10.1097/CCM.0b013e3182a275d7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Durairaj L, Torner JC, Chrischilles EA, Vaughan Sarrazin MS, Yankey J, Rosenthal GE. Hospital volume-outcome relationships among medical admissions to ICUs. Chest. 2005;128:1682–1689. doi: 10.1378/chest.128.3.1682. [DOI] [PubMed] [Google Scholar]
- 28.Kahn JM, Goss CH, Heagerty PJ, Kramer AA, O’Brien CR, Rubenfeld GD. Hospital volume and the outcomes of mechanical ventilation. N Engl J Med. 2006;355:41–50. doi: 10.1056/NEJMsa053993. [DOI] [PubMed] [Google Scholar]
- 29.Ross JS, Normand SL, Wang Y, Ko DT, Chen J, Drye EE, Keenan PS, Lichtman JH, Bueno H, Schreiner GC, et al. Hospital volume and 30-day mortality for three common medical conditions. N Engl J Med. 2010;362:1110–1118. doi: 10.1056/NEJMsa0907130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Engel HJ, Needham DM, Morris PE, Gropper MA. ICU early mobilization: from recommendation to implementation at three medical centers. Crit Care Med. 2013;41(9) Suppl 1:S69–S80. doi: 10.1097/CCM.0b013e3182a240d5. [DOI] [PubMed] [Google Scholar]
- 31.Morandi A, Brummel NE, Ely EW. Sedation, delirium and mechanical ventilation: the ‘ABCDE’ approach. Curr Opin Crit Care. 2011;17:43–49. doi: 10.1097/MCC.0b013e3283427243. [DOI] [PubMed] [Google Scholar]
- 32.Pandharipande P, Banerjee A, McGrane S, Ely EW. Liberation and animation for ventilated ICU patients: the ABCDE bundle for the back-end of critical care. Crit Care. 2010;14:157. doi: 10.1186/cc8999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Carrothers KM, Barr J, Spurlock B, Ridgely MS, Damberg CL, Ely EW. Contextual issues influencing implementation and outcomes associated with an integrated approach to managing pain, agitation, and delirium in adult ICUs. Crit Care Med. 2013;41(9) Suppl 1:S128–S135. doi: 10.1097/CCM.0b013e3182a2c2b1. [DOI] [PubMed] [Google Scholar]