Abstract
Rationale: Surrogates of critically ill patients often have inaccurate expectations about prognosis. Yet there is little research on how intensive care unit (ICU) clinicians should discuss prognosis, and existing expert opinion–based recommendations give only general guidance that has not been validated with surrogate decision makers.
Objective: To determine the perspectives of key stakeholders regarding how prognostic information should be conveyed in critical illness.
Methods: This was a multicenter study at three academic medical centers in California, Pennsylvania, and Washington. One hundred eighteen key stakeholders completed in-depth semistructured interviews. Participants included 47 surrogates of adult patients with acute respiratory distress syndrome; 45 clinicians working in study ICUs, including physicians, nurses, social workers, and spiritual care providers; and 26 experts in health communication, decision science, ethics, family-centered care, geriatrics, healthcare disparities, palliative care, psychology, psychiatry, and critical care.
Measurements and Main Results: There was broad support among surrogates for existing expert recommendations, including truthful prognostic disclosure, emotional support, tailoring the disclosure strategy to each family’s needs, and checking for understanding. In addition, stakeholders offered suggestions that add specificity to existing recommendations, including: (1) In addition to conveying prognostic estimates, clinicians should help families “see the prognosis for themselves” by showing families radiographic images and explaining the clinical significance of physical manifestations of severe disease at the bedside. (2) Many physicians did not support using numeric estimates to convey prognosis to families, whereas many surrogates, clinicians from other disciplines, and experts believed numbers could be helpful. (3) Clinicians should conceptualize prognostic communication as an iterative process that begins with a preliminary mention of the possibility of death early in the ICU stay and becomes more detailed as the clinical situation develops. (4) Although prognostic information should be initially disclosed by physicians, other members of the multidisciplinary team—nurses, social workers, and spiritual care providers—should be given explicit role responsibilities to reinforce physicians’ prognostications and help families process a poor prognosis emotionally.
Conclusions: Family members, clinicians, and experts identified specific communication behaviors that clinicians should use to discuss prognosis in the critical care setting. These findings extend existing opinion-based recommendations and should guide interventions to improve communication about prognosis in ICUs.
Keywords: critical care, communication, prognosis
One-fifth of Americans die after receiving care in an intensive care unit (ICU) (1). Many patients who survive prolonged ICU stays have poor functional outcomes and quality of life (2–4). Yet many ICU surrogates do not recall prognostic discussions with clinicians, and surrogates frequently have overly optimistic expectations for the patients’ survival, functional status, and quality of life (4–7). Misunderstandings and poor communication about prognosis may lead to patients receiving care that is unlikely to achieve their goals. Furthermore, ineffective discussions about prognosis may leave families unprepared for a patient’s death, which is a known risk factor for complicated grief and adverse bereavement outcomes (8–14).
There are several gaps in the evidence base that impede the development of effective interventions to improve prognostic communication in ICUs. First, clinical practice guidelines regarding family support, palliative care, and end-of-life care in ICUs are often based on low-level evidence and expert opinion and do not include surrogate decision makers’ perspectives (15–17). Second, although these guidelines emphasize that it is important to discuss prognosis, there is little specificity about how clinicians should do so. Third, much existing literature on how to discuss prognosis was developed for non-ICU settings (18), and there are contextual differences in the critical care setting that may limit the applicability of these guidelines, such as rapidly evolving clinical situations, discussions occurring primarily with surrogates as opposed to patients, and a lack of prior relationship between the clinicians and family.
Input from key stakeholders is a key factor in designing and implementing effective interventions (19, 20). Research has begun to describe the importance of prognostic information to ICU surrogates (5–7, 21, 22), yet their perspectives on how prognosis should be communicated have not been described. Thus, the goal of our study was to describe the perspectives of surrogates, as well as ICU clinicians and experts from multiple disciplines, on how prognosis should be communicated in the critical care setting.
Methods
Design
We conducted a qualitative study at three U.S. academic medical centers located in California, Pennsylvania, and Washington between November 2010 and June 2013. Each center had at least five ICUs and 50 ICU beds and infrastructure supporting research on family communication and acute respiratory distress syndrome (ARDS). They served as a quaternary referral centers and primary hospitals for patients residing near them. All had medical-surgical, cardiac, and neurologic ICUs; two had trauma ICUs.
Participants
Surrogates for ICU Patients
We enrolled surrogate decision makers for adult ICU patients who lacked decision-making capacity and had ARDS (23). We focused on patients with ARDS because of their high mortality and morbidity (24–27). We conducted the study within the U.S. ARDS research network and used its standardized approach to screening for ARDS (28–30). Trained coordinators calculated Acute Physiology and Chronic Health Evaluation (APACHE) II scores to assess severity of illness. We included patients with an APACHE II score of at least 25 (31). For patients with neurologic diagnoses, we included patients for whom the attending physician estimated a 50% or greater risk of hospital mortality or long-term severe functional impairment. We excluded patients who were awaiting organ transplantation or imminently dying. Surrogates were approached consecutively by study coordinators during the first 2 weeks of the patient’s ICU stay, after the patient’s physician reported having at least one prognostic discussion with the surrogate.
Clinicians
We identified physicians who had a prognostic discussion with an eligible surrogate and nonphysician clinicians who had observed or been involved in prognostic discussions in the study ICUs. To obtain a breadth of perspectives, we used a purposeful sampling strategy to maximize breadth of demographics, clinical specialties, areas of practice, and disciplines (32). Coordinators contacted clinicians by e-mail to request interviews.
Experts
We also interviewed a multidisciplinary sample of experts who were affiliated with U.S. and Canadian institutions. Areas of expertise included health communication, decision science, ethics, family-centered care, geriatrics, healthcare disparities, palliative care, psychology, psychiatry, and critical care. The goals of these interviews were to describe the experts’ opinion on the specific question of how prognosis should be communicated in the ICU and to identify barriers to best practices. We identified an initial set of experts as first or last authors on research publications identified with a PubMed keyword search for “communication,” “critical care,” and “prognosis.” We used a snowball sampling approach to identify additional experts, using related articles and reference lists, and asking participants to recommend others. We used purposeful sampling aiming for diversity in demographics, geographic location, specialty, and discipline (32). Several clinicians at the study institutions are national experts on communication and end-of-life care in ICUs and were enrolled in the expert stakeholders group. Experts were contacted by email to request interviews.
The Institutional Review Boards at the University of Pittsburgh, the University of California, San Francisco, and the University of Washington approved the study protocol. Surrogates and clinicians at the study hospitals provided written informed consent; experts provided verbal consent.
Data Collection
We designed semistructured interview topic guides (see online supplement) to elicit participants’ perspectives on how clinicians should communicate about prognosis when they believed the patient could die or have significant mental or physical impairment. Guides were based on past work (5, 21, 22, 33) and modified during early interviews to ensure they elucidated key themes. Study coordinators at each site were trained in qualitative interviewing (34) and performed all interviews, which lasted 30 to 90 minutes. Surrogates’ interviews occurred in conference rooms near the ICU; family members of the same patient were interviewed separately to minimize contamination. Surrogates who agreed to be contacted were called for an additional telephone interview 3 to 4 months after the patient’s death or hospital discharge. The goals of the follow-up interview were to see whether surrogates’ perspectives had changed since leaving the hospital and to obtain their feedback on a summary of our findings. Coordinators interviewed clinicians in their offices or a conference room and experts via telephone. Interviews were audio-recorded and professionally transcribed for analysis. We obtained demographic information about the study sample using brief surveys of participants and review of patients’ medical records.
Analysis
A multidisciplinary team, including investigators with training and experience in qualitative methods, performed a qualitative descriptive analysis of the interview transcripts (32). The team collaboratively developed an initial coding scheme based on open coding of early interviews, then clarified and modified this scheme in successive application to additional transcripts. We began to note recurrence and did not note new additional main themes after conducting approximately 30 interviews, indicating a degree of thematic saturation. We continued interviewing to refine the main themes and confirm our findings. To evaluate intercoder reliability of the final coding scheme, the three study coders independently coded 200 passages from the transcripts. The average kappa scores for key codes was 0.85, range 0.7 to 1.0, indicating substantial to excellent reliability (35). As a final step in coding, we collaboratively grouped themes into categories: goals of prognostic communication, recommended processes, and barriers. We further divided the processes category into three subcategories: timing of communication, information exchange, and emotional support. We used Atlas.ti version 6.2 (Berlin, Germany) for data management.
Because of the open-ended format of the interview questions, participants might not articulate a theme during their interview because it did not come to their mind. To assess whether differences in the percentages of participants who spontaneously identified a theme might indicate disagreement among different stakeholder groups, we presented a summary of our findings to 29 participants, including 14 surrogates, 5 clinicians, and 10 experts at the end of their interview. Except for differences in opinion about whether numeric estimates should be used to convey prognostic information, none of these participants disagreed with the themes presented here.
Role of the Funding Source
This research was supported by grants from the National Institutes of Health. The authors had full responsibility in designing the study; collecting, analyzing, and interpreting the data; writing the manuscript; and deciding to submit the manuscript for publication.
Results
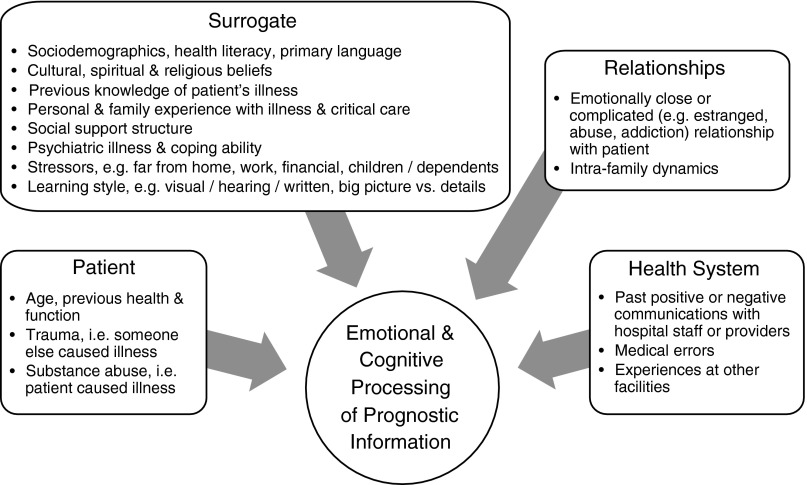
We conducted 142 in-depth interviews with 118 participants, including 47 surrogates of 44 patients, 17 physicians, 14 nurses, 7 social workers, 7 chaplains, and 26 experts. Of 63 eligible surrogates who we approached about the study, 47 (75%) consented and were interviewed; 24 completed an additional telephone interview after the patient’s discharge or death. Participation rates were 100% for physicians, 96% for nonphysician clinicians, and 81% for experts. Table 1 describes the participants’ characteristics. Participants described a number of factors that impact how surrogates receive and process prognostic information, including those related to the patient, surrogate, surrogates’ relationships, and health system (Figure 1). Participants identified discrete communication processes that help families process this information as well as barriers.
Table 1.
Characteristics of study participants
| Characteristic | Patients | Surrogates | Physicians | Nonphysician Clinicians | Experts |
|---|---|---|---|---|---|
| Participants, n | 44 | 47 | 17 | 28 | 26 |
| Mean age (SD), yr | 57 (14) | 53 (14) | 41 (9) | 45 (12) | 55 (9) |
| Male sex, n (%) | 26 (59) | 13 (28) | 11 (65) | 3 (11) | 8 (31) |
| Hispanic ethnicity, n (%) | 3 (7) | 3 (6) | 1 (6) | 2 (7) | 0 |
| Race, n (%) | |||||
| White | 40 (91) | 42 (89) | 14 (82) | 22 (79) | 21 (81) |
| African American | 2 (5) | 1 (2) | 2 (12) | 1 (4) | 1 (4) |
| Asian | 1 (2) | 2 (4) | 1 (6) | 2 (7) | 4 (15) |
| Native American, American Indian/Alaskan Native | 1 (2) | 1 (2) | — | 2 (7) | — |
| Mixed | — | 1 (2) | — | 1 (4) | — |
| ICU admission diagnoses, n (%) | |||||
| Respiratory failure | 16 (25) | ||||
| Shock | 15 (23) | ||||
| Renal failure | 11 (17) | ||||
| Neurologic failure | 8 (12) | ||||
| Trauma | 6 (9) | ||||
| Other | 9 (20) | ||||
| Patient limitation of life-sustaining therapy during hospitalization, n (%) | 15 (34) | ||||
| Patient discharge disposition, n (%) | |||||
| Died in hospital | 14 (32) | ||||
| Hospice | — | ||||
| Home | 9 (20) | ||||
| Skilled nursing facility | 9 (20) | ||||
| Long-term acute care facility | 4 (9) | ||||
| Acute rehabilitation facility | 3 (7) | ||||
| Other | 5 (11) | ||||
| Surrogate relationship to patient, n (%) | |||||
| Spouse or partner | 26 (55) | ||||
| Parent | 6 (13) | ||||
| Child | 10 (21) | ||||
| Sibling | 2 (4) | ||||
| Other | 3 (6) | ||||
| Patient living at surrogate follow-up interview, n (%) | 13 (57) | ||||
| Physician specialty, n (%) | |||||
| Critical Care | 11 (65) | ||||
| Internal Medicine | 13 (76) | ||||
| Anesthesia | 2 (12) | ||||
| Surgery | 2 (12) | ||||
| Neurology | 1 (6) | ||||
| Nonphysician clinician discipline, n (%) | |||||
| Nursing | 14 (50) | ||||
| Social work | 7 (25) | ||||
| Chaplain | 7 (25) | ||||
| Nonphysician practice location/role, n (%) | |||||
| Critical care | 21 (75) | ||||
| Nursing administration/coordination | 8 (29) | ||||
| Bedside nursing | 7 (25) | ||||
| Hospital spiritual care service | 6 (21) | ||||
| Palliative care service | 3 (11) | ||||
| Clinician mean time in practice, (SD), yr | 11 (9) | 18 (11) | |||
| Expert discipline, n (%) | |||||
| Physicians | 15 (58) | ||||
| Nursing | 7 (27) | ||||
| Social work | 2 (8) | ||||
| Social science | 2 (8) | ||||
| Expert areas of expertise, n (%) | |||||
| Critical care | 14 (54) | ||||
| Health communication | 9 (35) | ||||
| Ethics and decision science | 13 (50) | ||||
| Family centered care | 2 (8) | ||||
| Geriatrics | 4 (15) | ||||
| Healthcare disparities | 3 (12) | ||||
| Palliative care | 18 (69) | ||||
| Psychiatry and psychology | 5 (19) |
Definition of abbreviation: ICU = intensive care unit.
Figure 1.
Factors identified by participants as influencing surrogates’ emotional and cognitive processing of prognostic information. Participants identified patient-, surrogate-, relationship-, and health system–related factors.
Support for and Extension of ICU Family Support, Palliative Care, and End-of-Life Guidelines
The themes identified by family, clinician, and expert participants regarding how a poor prognosis should be communicated in the ICU support a number of recommendations in clinical practice guidelines (15–17) (Table 2). For example, study participants emphasized truthful prognostic disclosure, emotional support, tailoring the disclosure strategy to each family’s needs, and checking for understanding. Exemplar quotations for the themes that support current recommendations can be found in the online supplement (Table E1). In addition, stakeholders offered suggestions that extend and add specificity to existing recommendations; these themes are listed in Table 3 and described in detail below. Exemplar quotations for these novel themes are shown in Table 4.
Table 2.
Support for published practice guidelines (15–17): themes identified by stakeholders regarding how a poor prognosis should be communicated in the intensive care unit
| Themes | Participants Who Identified Concept during Their
Interview* |
||||
|---|---|---|---|---|---|
| All (n = 118) | Surrogates (n = 47) | Physicians (n = 17) | Nonphysician Clinicians (n = 28) | Experts (n = 26) | |
| Disclose prognostic information in a truthful and clear manner | 102 (86) | 40 (85) | 15 (88) | 26 (97) | 21 (81) |
| Adapt communication to each family member’s needs | 100 (85) | 35 (74) | 16 (94) | 25 (89) | 24 (92) |
| Before giving information, elicit family perspective and understanding | 42 (36) | 4 (9) | 11 (65) | 15 (54) | 12 (46) |
| After giving information, check family understanding and provide opportunities for questions | 108 (92) | 40 (85) | 16 (94) | 27 (96) | 25 (96) |
| Frame prognostic discussions within patient and family goals and values | 80 (68) | 19 (40) | 15 (88) | 25 (89) | 21 (81) |
| Attend to family emotion and demonstrate empathy | 111 (94) | 46 (98) | 14 (82) | 27 (96) | 24 (92) |
| Barriers | |||||
| ICU culture: valuing families and communication | 102 (86) | 42 (89) | 13 (76) | 26 (93) | 21 (81) |
| Inadequate staffing and time for discussions | 59 (50) | 17 (36) | 7 (41) | 14 (50) | 21 (81) |
| Lack of availability of space for discussions | 62 (53) | 21 (45) | 12 (71) | 18 (64) | 11 (42) |
| Lack of clinician training in communication | 61 (52) | 11 (23) | 16 (94) | 16 (57) | 18 (69) |
Definition of abbreviation: ICU = intensive care unit.
Data presented as n (%).
Not identifying a concept does not mean participants did not endorse its importance, only that they did not spontaneously identify it in their semistructured interview. In the final stage of the interviewing, we presented these themes to 29 participants, including 14 surrogates, 5 clinicians, and 10 experts at the end of their interview; with the exception of differences in preference for use of numeric estimates to convey prognosis, none these interviewees disagreed with the findings presented.
Table 3.
Novel themes identified by stakeholders regarding how a poor prognosis should be communicated in the intensive care unit
| Themes | Participants Who Identified Concept during Their
Interview* |
||||
|---|---|---|---|---|---|
| All (n = 118) | Surrogates (n = 47) | Physicians (n = 17) | Nonphysician Clinicians (n = 28) | Experts (n = 26) | |
| Help families to see prognosis through education, pictures, radiographs, and bedside explanations | 84 (71) | 37 (79) | 13 (76) | 19 (68) | 15 (58) |
| Convey the possibility of poor outcomes early | 99 (84) | 45 (96) | 13 (76) | 21 (75) | 20 (77) |
| Discuss prognosis regularly over the course of the ICU stay, as the patient’s course evolves | 74 (63) | 20 (43) | 15 (88) | 20 (71) | 19 (73) |
| Numeric estimates may be helpful to families | 63 (53) | 31 (66) | 2 (12) | 17 (61) | 13 (50) |
| Engaging multiple clinical disciplines in coordinated prognostic communication | 113 (96) | 45 (96) | 16 (94) | 28 (100) | 24 (92) |
Definition of abbreviation: ICU = intensive care unit.
Data presented as n (%).
Not identifying a concept does not mean participants did not endorse its importance, only that they did not spontaneously identify it in their semistructured interview. In the final stage of the interviewing, we presented these themes to 29 participants, including 14 surrogates, 5 clinicians, and 10 experts at the end of their interview; with the exception of differences in preference for use of numeric estimates to convey prognosis, none these interviewees disagreed with the findings presented.
Table 4.
Exemplar quotations for novel themes identified by stakeholders regarding how a poor prognosis should be communicated in the intensive care unit
| Theme | Exemplar Quotation |
|---|---|
| Help families to see prognosis through education, pictures, radiographs, and bedside explanations | Surrogate: Rather than using the terms [that clinicians] are more familiar with, [they should] think of it like they were telling their mom or their daughter....[Use] videos or booklets or charts or little models or something to show what’s going on. Most regular folks don’t know specifically how the body works or fails. –Wife of a man with sepsis and renal failure |
| Physician: If a patient isn’t weaning off the ventilator, I show the family. I’ll put them on a weaning trial, right in front of them. “This is a bad prognosis, the fact that they can’t breathe on their own.”…That conveys a lot of prognostic information—more than me saying, “We tried this and it isn’t working.” –Pulmonary and critical care physician | |
| Nonphysician clinician: It goes much better when you paint a picture for families, as to what will this person look like, in 3 months, in 6 months, in a year. What are the possibilities? We say a lot of medical gobbledygook…[Instead we should] say, “What does this mean, concretely, for your activities of daily living?” –Trauma nurse coordinator | |
| Expert: If a physician sees a patient who’s had a massive stroke, the family needs to see a picture of the scan of the head that shows what a stroke looks like…so they can get a sense of, “This is an impairment and this is going to be permanent.”…What works best is auditory and visual. –Clinical social worker and expert in ethics | |
| Convey the possibility of poor outcomes early | Surrogate: [I’d want to hear prognostic information] early, right off the bat…right up front. I would want somebody to be honest right up front, rather than let me imagine that things are going to be okay. –Husband of a woman hospitalized after a drug overdose |
| Physician: It’s good to keep the family informed as much as possible, right from the very beginning.…I don’t think one has to go right out on a limb and say, “This is a dismal prognosis,” before you’re really comfortable that it is a dismal prognosis. But the family should know there’s a serious problem going on. –Neurologist | |
| Nonphysician clinician: If there’s any question that [a patient’s situation] could become a poor prognosis, that needs to be discussed as soon as the team is aware. It’s really important that the family, looking back, once the outcome is reached, to understand that they’ve been updated and no information has ever been withheld from them. –Trauma nurse coordinator | |
| Expert: Initially, there’s so much uncertainty....[So] we don’t even [begin to discuss prognosis] until we’re fairly certain that the outcome is going to be terrible....[We need to] share with families up front, what the signs are that we’re going be looking for....If you prepare them for that, then when that starts happening, you’ve got that frame of reference. –Nurse and expert in ethics, critical care, and palliative care | |
| Discuss prognosis regularly over the course of the ICU stay | Surrogate: I think you have to say, “At this particular point, I can’t give you a definite prognosis, but I’m going to keep you informed of what is happening and this will be a day by day process.” –Daughter of a woman with aspiration pneumonia |
| Physician: If I have met with the family on admission and say, “We need to wait 24 to 48 hours to see which way things are going.” And then we meet 48 hours later, I will say, “We talked initially and he has not done well in the last 48 hours. He’s done worse.” –Internal medicine physician | |
| Nonphysician clinician: [The ICU clinicians] should touch base with the family on admit.…Then, over the next 2 days or 3 days, have a sit down conference with the medical team, the family, and the nurse, and make sure everyone’s [updated]—do they have any questions? –Nurse manager in a medical ICU | |
| Expert: We create a lot of stress by springing [the prognosis] on people without giving them some warning that it’s coming. People need time. You have to have these conversations repeatedly. You have to be willing to allow time in between these discussions. –Nurse and expert in critical care, ethics, and palliative care | |
| Numeric estimates may be helpful to families | Surrogate: I’m an analytical person. So, for me statistics, numbers, those are things I can compute in my head. That’s comforting. –Wife of a man with abdominal trauma |
| Physician: I think you need to be sensitive to the fact that some people value numbers and statistics. –Surgeon and critical care physician | |
| Nonphysician clinician: A lot of times, families ask. “Do you have any statistics about this diagnosis—that show how many have been [able] to improve with rehab[ilitation]?”…It’s helpful to the families when the doctors have those facts at their fingertips. –Social worker in a neurological ICU | |
| Expert: I know that physicians sometimes don’t like to give percentages and I understand that. But families are looking for that kind of thing, like what percentage risk [the patient] has of dying. –Medical social worker and expert in critical care and palliative care | |
| Numeric estimates are not helpful to families | Surrogate: My church has a saying for statistics—statistics are just that. Everybody’s different and you never know. Statistics are about something that’s already happened and you’re not a statistic. You’re a person. –Wife of a trauma patient |
| Physician: One of the most important things is to be as honest and forthright—not necessarily using numbers, but using words like “death,” “dying,” “near death,” “no chance,” or “little chance” of survival. –Pulmonary and critical care physician | |
| Nonphysician clinician: [Numbers] are not very useful because I’ve seen it go both ways—where you give them a great percentage, but [the patient] has a horrible outcome, or you give them a bad percentage, but they have a very good outcome. –Social worker in a burn ICU | |
| Expert: The problem with being really quantitative is that [families] get stuck in the numbers because they view the numbers are real or true in a fixed way, rather than, “They’re my best guesstimate at the time.” So, I usually don’t use numbers. –Physician and expert in communication, ethics, and palliative care | |
| Engaging multiple clinical disciplines in coordinated prognostic communication | Surrogate: You’re around the nurses more and you’re more comfortable talking to the nurses. They learn you and get to know you and talk to you in a different way than the doctors are able to. –Wife of a man with sepsis |
| Physician: A nurse, who has taken care of the patient and seen the family for hours can say, “The family is really concerned about this.”…They can give you the information that you need to know about whether the family’s prepared [to hear prognostic information] or not. –Neurologist | |
| Nonphysician clinician: Physicians are often the ones who communicate the medical information…I see nurses as the primary folks to help with…clarifying some of the questions…[and being] the point person to draw in other support resources. As spiritual care providers, we try to honor and respect the spiritual and cultural values of the patient and family; sometimes we have more time to support people with grief and loss. –Chaplain | |
| Expert: [When planning a prognostic discussion] you first need to say, “Is there somebody else that should be at the doctor’s side that’s going to communicate and translate any questions later?” And that would naturally be the nurse. Sometimes, the patient’s family has a very strong relationship with a chaplain or a social worker or case manager or respiratory therapist. If that’s the case, then those disciplines should be there at the side of the physician when making the discussion. Because [after the meeting] the family is left with the other caregivers and questions will come to the surface later. [Including those clinicians] provides an element of trust in the room because they know them quite well, from spending hours with them. –Nurse and expert in critical care |
Definition of abbreviation: ICU = intensive care unit.
Helping Families to See the Prognosis for Themselves
Many participants (n = 84, 71%) recommended that clinicians should not simply provide a prognostic estimate but should also educate families and help them to understand how they arrived at their estimate. To come to an understanding and acceptance of a poor prognosis, families needed to understand the disease processes causing a poor prognosis. Lay language explanations of medical information were essential but often not sufficient. Participants recommended using different modalities to help families understand information. Many found visual illustrations to be helpful. For example, families appreciated drawings on scratch paper or blackboards as well as clinicians reviewing radiographs with them. The surrogate of a patient who developed ARDS after a subarachnoid hemorrhage explained how reviewing a radiograph helped him to understand the severity of his brother’s pneumonia, “They explained to me the darkness and that was good and the light was not good and so the next time they flash one up, I can tell whether it’s getting better or getting worse. Seeing those graphic pictures was helpful. Then I can look at it and form my own opinion.”
Although families often felt uncomfortable discussing specific prognostic information at the bedside where the patient might overhear, bedside rounds were key opportunities to provide education and support for prognostic estimates, for example by showing the treatments the patient was requiring. Discussing prognosis in terms of a patient’s goals of care and the big picture, for example which daily activities the patient might be able to do or not do, was another way to make information more concrete and understandable. Finally, families also requested informational materials that they could review after talking with clinicians, as they often found it hard to understand and retain information from a discussion.
To ensure that families had understood information presented, participants emphasized that clinicians actively assess family understanding as opposed to simply giving time for questions. Many family members did not feel comfortable stating that they did not understand or asking for education, or might not know what questions to ask. The wife of a man who developed ARDS after being admitted with pneumonia conveyed, “There’s a lot of times [the doctors] say, ‘Well, do you have any questions?’ And I don’t know what to ask.…I may say, ‘No,’ because I don’t know what to ask.”
Disagreement between Physicians and Other Stakeholders about Whether Numeric Prognostic Estimates Are Helpful to Families
Although we found general agreement among stakeholder groups about how a poor prognosis could be communicated, we did identify a difference of opinion between physicians and other stakeholders about the use of numeric estimates to convey prognostic information. Almost all participants (n = 114, 97%) commented on whether or not numeric prognostic estimates were helpful to families. Many surrogates (n = 31, 66%), nonphysician clinicians (n = 17, 61%), and experts (n = 13, 50%) said that numbers could be helpful and should be offered to families. In contrast, few physicians (n = 2, 12%) believed that numbers were a helpful format in which to provide families with prognostic information. Participants who reported that numbers could be helpful believed they provided a concrete gauge for families. Respondents who did not find numerical estimates helpful said that families often misinterpreted numbers, prognosis could not be pinpointed, and statistics could not predict what would happen to an individual. Even those advocating for numeric estimates emphasized that numbers might not help everyone and should be accompanied by qualitative explanations.
Conceptualizing Prognostic Communication as an Iterative Process that Occurs in Multiple Venues over the Course of the ICU Stay
Participants provided specific guidance about how prognosis should be discussed within the regular family meetings that practice guidelines recommend (15–17). They believed that communication about prognosis should begin with a preliminary mention of the possibility of death early in the ICU stay and become more detailed as the clinical situation developed. Families particularly wanted clinicians to alert them to the possibility that the patient could die, so that they could prepare emotionally and tell other family members. The wife of a patient admitted to the ICU after a motor vehicle accident said, “Say [my husband’s doctors] were thinking he might die. If they didn’t tell me right away, I don’t have the option of calling his children or anybody else who might want to come and say their farewells.” Communicating about prognosis over a series of discussions allowed families time to understand complicated medical information and emotionally accept a poor prognosis. The friend of a patient with sepsis and renal failure said, “You don’t want to see your family member go. You need to hear it a number of times, before it will sink in.”
Regarding the venue and format of prognostic communications, participants noted that family meetings and discussions with physicians could be stressful for families, who often did not understand information presented and might not feel comfortable asking questions. As the wife a man who developed ARDS after neurologic surgery described, “Some [family members] are embarrassed to say they don’t understand because then it shows they’re not very smart.” More informal discussions with team members from multiple disciplines before and after meetings gave families chances to ask questions and ensure they understood information.
Explicit Role Responsibilities for Clinicians from Multiple Disciplines in Prognostic Communication
Participants perceived important and complementary roles for clinicians from multiple disciplines in supporting family members’ cognitive and emotional processing of prognostic information. Surrogates often preferred to receive prognostic assessments from those who were most knowledgeable in an area, physicians in charge or specialists. Generalists such as critical or palliative care clinicians helped families to integrate information into a big picture of how a patient was doing.
Nonphysician clinicians—such as nurses, social workers, and chaplains—had training and time to reinforce information and answer questions, educate families, and provide emotional support. These clinicians could prepare families and physicians for discussions by assessing family concerns and readiness for prognostic information. The presence in prognostic discussions of clinicians such as nurses who spent a lot of time at the bedside helped families to trust information presented. These clinicians could talk with families after discussions, to translate and reinforce information. Such interactions were often less stressful than family meetings or discussions with physicians, as the brother of a patient with a subarachnoid hemorrhage detailed, “A social worker or that kind of a person might be called in and talk more person-to-person than doctor-to-patient. Somebody who understands what the doctors are saying and would sit down with the family—because the doctors are a little intimidating to the average person.”
Barriers
Participants identified barriers to implementing the processes they recommended. A key barrier was ICU culture. An ICU culture of valuing families and communication was necessary to implement the behaviors the participants recommended. Families felt valued when clinicians spent time with them, listened, and seemed available and approachable. ICU staffing was another barrier; clinicians could not spend adequate time with families unless their ICU was staffed to prioritize family communication as a core aspect of clinical care. Participants also mentioned the importance of identifying and using private discussion spaces for prognostic communication: families were often uncomfortable asking questions about prognosis information in the patient’s room, even if the patient was not responsive. Finally, inadequate training of clinicians, both regarding attitudes of valuing families and communication, and skill to communicate about prognosis, was a barrier.
Discussion
To our knowledge, this is the first multicenter engagement of surrogates of ICU patients, as well as ICU clinicians and experts from a broad range of disciplines and areas of expertise, on how a poor prognosis should be communicated in the setting of critical illness. Although previous research has documented that surrogates and clinicians often have discordant perspectives about a patient’s prognosis (5–7), we found that these stakeholders had similar views on how to improve the process of prognostic communication. This consensus is an important step in developing interventions, which are more likely to be assimilated into practice if they include the elements stakeholder perceive to be important (19, 20).
Our stakeholders’ views prompt further investigation and refinement of published ICU guidelines on family support (15), palliative care (17), and end-of-life care (16). For example, current guidelines rely on the family meeting as the key venue of prognostic communication. Our surrogate participants endorsed the importance of early and regular prognostic communication, yet some experienced family meetings as stressful and intimidating. Surrogates might not understand information presented, but did not feel comfortable asking a question or did not know what questions to ask. Our findings indicate that family meetings should be supplemented with regular, less formal prognostic discussions at the bedside with clinicians who can interpret and reinforce information and provide emotional support.
Our participants provide specific recommendations about how clinicians should discuss prognosis with surrogates. Stakeholders emphasized that clinicians should explain and show families information supporting their prognostic estimates, so families could see the prognosis for themselves. Few families could comprehend complicated prognostic information without understanding the underlying medical processes. Using visual data, such as drawing pictures and showing surrogates medical images such as radiographs, may be a powerful way to help them come to an understanding of prognosis.
Interestingly, many surrogates, nonphysician clinicians, and experts favored using numeric estimates to convey prognostic information, whereas most physicians did not. Further research should identify surrogate factors associated with preference for numeric information about prognosis and investigate whether providing numeric information improves surrogate understanding of prognosis. Our data do support the recommendation from prognostic communication guidelines in the non-ICU setting that surrogates be offered numeric estimates if they are available (18).
Finally, stakeholders highlighted the importance of engaging all disciplines in prognostic communication and outlined specific and complementary roles that each should take. Previous work has highlighted the importance of nurses being involved in communication and quality improvement (36–39). Our data detail the crucial roles that nurses, social workers, and spiritual care have in supporting prognostic understanding. This suggests that interventions to improve prognostic communication in ICUs should ensure that these clinicians are trained to serve these roles, systematize their involvement, and emphasize multidisciplinary team work (36, 40).
Our study has several limitations. First, because we described themes based on participants’ spontaneous statements during semistructured interviews, and interviewed some surrogates of the same patient, we cannot quantify the percentage of stakeholders in each group who agree or disagree with each theme or test associations between themes and participants’ characteristics. Second, clinician stakeholders may lack insight into the problems to which they contributed. Third, though the 29 interviewees who reviewed a summary of our findings did not disagree with the themes presented here, there is a potential for framing bias in their review. Finally, although we included participants from different geographic locations and used a purposeful sampling strategy for clinicians and experts to maximize diversity in race and other factors, most of the stakeholders we interviewed were of white race and from academic medical centers in the urban United States. Also, the centers at which we conducted the study have previously led research on ICU communication. Stakeholders in other settings may have different perspectives.
In conclusion, in this multicenter study, surrogates of ICU patients with ARDS, ICU clinicians from multiple disciplines, and experts identified specific recommendations for how prognosis should be communicated in the ICU. Their perspectives should inform practice guidelines and interventions to improve prognostic communication in ICUs.
Acknowledgments
Acknowledgment
The authors thank the families, clinicians, and experts who generously donated their time to participate in this study. They also thank Anne-Marie Shields, M.S.N., R.N., Program Manager for Ethics and Decision Making in Critical Illness at the Department of Critical Care Medicine and Clinical Research, Investigation, and Systems Modeling of Acute Illness Laboratory, University of Pittsburgh School of Medicine, for her guidance and support in the implementation of this project.
Footnotes
Supported by the National Heart, Lung, and Blood Institute, National Institutes of Health grant R01HL094553 and the National Center for Advancing Translational Sciences, National Institutes of Health, through University of California San Francisco Clinical and Translational Science Institute grant KL2 TR000143.
The article’s contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH.
Author Contributions: W.G.A., S.S.C., J.R.C., C.L.H., B.L., M.A.M., M.W.P., J.S.S., and D.B.W. contributed to the conception and design of the study. J.W.C., A.U., K.J.S., and L.A.P. acquired the data. W.G.A., J.W.C., A.U., N.C.E., K.J.S., L.A.P., and P.B. performed the analysis. All authors contributed to interpretation of the data. W.G.A. prepared the initial draft, and all authors provided critical revisions to the drafts. W.G.A., S.S.C., J.R.C., C.L.H., B.L., M.A.M., M.W.P., J.S.S., and D.B.W. obtained funding.
This article has an online supplement, which is accessible from this issue’s table of contents at www.atsjournals.org
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1.Angus DC, Barnato AE, Linde-Zwirble WT, Weissfeld LA, Watson RS, Rickert T, Rubenfeld GD. Use of intensive care at the end of life in the United States: an epidemiologic study. Crit Care Med. 2004;32:638–643. doi: 10.1097/01.ccm.0000114816.62331.08. [DOI] [PubMed] [Google Scholar]
- 2.Unroe M, Kahn JM, Carson SS, Govert JA, Martinu T, Sathy SJ, Clay AS, Chia J, Gray A, Tulsky JA, et al. One-year trajectories of care and resource utilization for recipients of prolonged mechanical ventilation: a cohort study. Ann Intern Med. 2010;153:167–175. doi: 10.1059/0003-4819-153-3-201008030-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Carson SS, Kahn JM, Hough CL, Seeley EJ, White DB, Douglas IS, Cox CE, Caldwell E, Bangdiwala SI, Garrett JM, et al. ProVent Investigators. A multicenter mortality prediction model for patients receiving prolonged mechanical ventilation. Crit Care Med. 2012;40:1171–1176. doi: 10.1097/CCM.0b013e3182387d43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cox CE, Martinu T, Sathy SJ, Clay AS, Chia J, Gray AL, Olsen MK, Govert JA, Carson SS, Tulsky JA. Expectations and outcomes of prolonged mechanical ventilation. Crit Care Med. 2009;37:2888–2894. doi: 10.1097/CCM.0b013e3181ab86ed. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Boyd EA, Lo B, Evans LR, Malvar G, Apatira L, Luce JM, White DB. “It’s not just what the doctor tells me:” factors that influence surrogate decision-makers’ perceptions of prognosis. Crit Care Med. 2010;38:1270–1275. doi: 10.1097/CCM.0b013e3181d8a217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zier LS, Burack JH, Micco G, Chipman AK, Frank JA, Luce JM, White DB. Doubt and belief in physicians’ ability to prognosticate during critical illness: the perspective of surrogate decision makers. Crit Care Med. 2008;36:2341–2347. doi: 10.1097/CCM.0b013e318180ddf9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zier LS, Sottile PD, Hong SY, Weissfield LA, White DB. Surrogate decision makers’ interpretation of prognostic information: a mixed-methods study. Ann Intern Med. 2012;156:360–366. doi: 10.1059/0003-4819-156-5-201203060-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Anderson WG, Arnold RM, Angus DC, Bryce CL. Posttraumatic stress and complicated grief in family members of patients in the intensive care unit. J Gen Intern Med. 2008;23:1871–1876. doi: 10.1007/s11606-008-0770-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Azoulay E, Pochard F, Kentish-Barnes N, Chevret S, Aboab J, Adrie C, Annane D, Bleichner G, Bollaert PE, Darmon M, et al. Risk of post-traumatic stress symptoms in family members of intensive care unit patients. Am J Respir Crit Care Med. 2005;171:987–994. doi: 10.1164/rccm.200409-1295OC. [DOI] [PubMed] [Google Scholar]
- 10.Jones C, Skirrow P, Griffiths RD, Humphris G, Ingleby S, Eddleston J, Waldmann C, Gager M. Post-traumatic stress disorder-related symptoms in relatives of patients following intensive care. Intensive Care Med. 2004;30:456–460. doi: 10.1007/s00134-003-2149-5. [DOI] [PubMed] [Google Scholar]
- 11.Kross EK, Engelberg RA, Gries CJ, Nielsen EL, Zatzick D, Curtis JR. ICU care associated with symptoms of depression and posttraumatic stress disorder among family members of patients who die in the ICU. Chest. 2011;139:795–801. doi: 10.1378/chest.10-0652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Prigerson HG, Cherlin E, Chen JH, Kasl SV, Hurzeler R, Bradley EH. The Stressful Caregiving Adult Reactions to Experiences of Dying (SCARED) Scale: a measure for assessing caregiver exposure to distress in terminal care. Am J Geriatr Psychiatry. 2003;11:309–319. [PubMed] [Google Scholar]
- 13.Siegel MD, Hayes E, Vanderwerker LC, Loseth DB, Prigerson HG. Psychiatric illness in the next of kin of patients who die in the intensive care unit. Crit Care Med. 2008;36:1722–1728. doi: 10.1097/CCM.0b013e318174da72. [DOI] [PubMed] [Google Scholar]
- 14.Wright AA, Zhang B, Ray A, Mack JW, Trice E, Balboni T, Mitchell SL, Jackson VA, Block SD, Maciejewski PK, et al. Associations between end-of-life discussions, patient mental health, medical care near death, and caregiver bereavement adjustment. JAMA. 2008;300:1665–1673. doi: 10.1001/jama.300.14.1665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Davidson JE, Powers K, Hedayat KM, Tieszen M, Kon AA, Shepard E, Spuhler V, Todres ID, Levy M, Barr J, et al. American College of Critical Care Medicine Task Force, Society of Critical Care Medicine. Clinical practice guidelines for support of the family in the patient-centered intensive care unit: American College of Critical Care Medicine Task Force 2004–2005. Crit Care Med. 2007;35:605–622. doi: 10.1097/01.CCM.0000254067.14607.EB. [DOI] [PubMed] [Google Scholar]
- 16.Truog RD, Campbell ML, Curtis JR, Haas CE, Luce JM, Rubenfeld GD, Rushton CH, Kaufman DC. American Academy of Critical Care M. Recommendations for end-of-life care in the intensive care unit: a consensus statement by the American College [corrected] of Critical Care Medicine. Crit Care Med. 2008;36:953–963. doi: 10.1097/CCM.0B013E3181659096. [DOI] [PubMed] [Google Scholar]
- 17.Lanken PN, Terry PB, Delisser HM, Fahy BF, Hansen-Flaschen J, Heffner JE, Levy M, Mularski RA, Osborne ML, Prendergast TJ, et al. ATS End-of-Life Care Task Force. An official American Thoracic Society clinical policy statement: palliative care for patients with respiratory diseases and critical illnesses. Am J Respir Crit Care Med. 2008;177:912–927. doi: 10.1164/rccm.200605-587ST. [DOI] [PubMed] [Google Scholar]
- 18.Clayton JM, Hancock KM, Butow PN, Tattersall MH, Currow DC.Australian and New Zealand Expert Advisory Group, Adler J, Aranda S, Auret K, Boyle F, et al. Clinical practice guidelines for communicating prognosis and end-of-life issues with adults in the advanced stages of a life-limiting illness, and their caregivers. Med J Aust2007186S77, S79, S83–108 [DOI] [PubMed] [Google Scholar]
- 19.Hoffman A, Montgomery R, Aubry W, Tunis SR. How best to engage patients, doctors, and other stakeholders in designing comparative effectiveness studies. Health Aff (Millwood) 2010;29:1834–1841. doi: 10.1377/hlthaff.2010.0675. [DOI] [PubMed] [Google Scholar]
- 20.Frank L, Basch E, Selby JV. Patient-Centered Outcomes Research Institute. The PCORI perspective on patient-centered outcomes research. JAMA. 2014;312:1513–1514. doi: 10.1001/jama.2014.11100. [DOI] [PubMed] [Google Scholar]
- 21.Apatira L, Boyd EA, Malvar G, Evans LR, Luce JM, Lo B, White DB. Hope, truth, and preparing for death: perspectives of surrogate decision makers. Ann Intern Med. 2008;149:861–868. doi: 10.7326/0003-4819-149-12-200812160-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schenker Y, White DB, Crowley-Matoka M, Dohan D, Tiver GA, Arnold RM. “It hurts to know… and it helps”: exploring how surrogates in the ICU cope with prognostic information. J Palliat Med. 2013;16:243–249. doi: 10.1089/jpm.2012.0331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.ARDS Definition Task Force. Ranieri VM, Rubenfeld GD, Thompson BT, Ferguson ND, Caldwell E, Fan E, Camporota L, Slutsky AS. Acute respiratory distress syndrome: the Berlin Definition. JAMA. 2012;307:2526–2533. doi: 10.1001/jama.2012.5669. [DOI] [PubMed] [Google Scholar]
- 24.Wang CY, Calfee CS, Paul DW, Janz DR, May AK, Zhuo H, Bernard GR, Matthay MA, Ware LB, Kangelaris KN. One-year mortality and predictors of death among hospital survivors of acute respiratory distress syndrome. Intensive Care Med. 2014;40:388–396. doi: 10.1007/s00134-013-3186-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Villar J, Blanco J, Anon JM, Santos-Bouza A, Blanch L, Ambros A, Gandia F, Carriedo D, Mosteiro F, Basaldua S, et al. The ALIEN study: incidence and outcome of acute respiratory distress syndrome in the era of lung protective ventilation. Intensive Care Med. 2011;37:1932–1941. doi: 10.1007/s00134-011-2380-4. [DOI] [PubMed] [Google Scholar]
- 26.Herridge MS, Tansey CM, Matte A, Tomlinson G, Diaz-Granados N, Cooper A, Guest CB, Mazer CD, Mehta S, Stewart TE, et al. Canadian Critical Care Trials Group. Functional disability 5 years after acute respiratory distress syndrome. N Engl J Med. 2011;364:1293–1304. doi: 10.1056/NEJMoa1011802. [DOI] [PubMed] [Google Scholar]
- 27.Hopkins RO, Weaver LK, Collingridge D, Parkinson RB, Chan KJ, Orme JF., Jr Two-year cognitive, emotional, and quality-of-life outcomes in acute respiratory distress syndrome. Am J Respir Crit Care Med. 2005;171:340–347. doi: 10.1164/rccm.200406-763OC. [DOI] [PubMed] [Google Scholar]
- 28.Matthay MA, Brower RG, Carson S, Douglas IS, Eisner M, Hite D, Holets S, Kallet RH, Liu KD, MacIntyre N, et al. Randomized, placebo-controlled clinical trial of an aerosolized beta(2)-agonist for treatment of acute lung injury. Am J Respir Crit Care Med. 2011;184:561–568. doi: 10.1164/rccm.201012-2090OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rice TW, Wheeler AP, Thompson BT, Steingrub J, Hite RD, Moss M, Morris A, Dong N, Rock P. Initial trophic vs full enteral feeding in patients with acute lung injury: the EDEN randomized trial. JAMA. 2012;307:795–803. doi: 10.1001/jama.2012.137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rice TW, Wheeler AP, Thompson BT, deBoisblanc BP, Steingrub J, Rock P. Enteral omega-3 fatty acid, gamma-linolenic acid, and antioxidant supplementation in acute lung injury. JAMA. 2011;306:1574–1581. doi: 10.1001/jama.2011.1435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med. 1985;13:818–829. [PubMed] [Google Scholar]
- 32.Sandelowski M. Whatever happened to qualitative description? Res Nurs Health. 2000;23:334–340. doi: 10.1002/1098-240x(200008)23:4<334::aid-nur9>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- 33.Evans LR, Boyd EA, Malvar G, Apatira L, Luce JM, Lo B, White DB. Surrogate decision-makers' perspectives on discussing prognosis in the face of uncertainty. Am J Respir Crit Care Med. 2009;179:48–53. doi: 10.1164/rccm.200806-969OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Charmaz K.Constructing grounded theory: a practical guide through qualitative analysis. London: Sage; 2006 [Google Scholar]
- 35.Landis R, Koch G. An application of hierarchical kappa-type statistics in the assessment of majority agreement among multiple observers. Biometrics. 1977;33:363–374. [PubMed] [Google Scholar]
- 36.Krimshtein NS, Luhrs CA, Puntillo KA, Cortez TB, Livote EE, Penrod JD, Nelson JE. Training nurses for interdisciplinary communication with families in the intensive care unit: an intervention. J Palliat Med. 2011;14:1325–1332. doi: 10.1089/jpm.2011.0225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Nelson JE, Cortez TB, Curtis JR, Lustbader DR, Mosenthal AC, Mulkerin C, Ray DE, Bassett R, Boss RD, Brasel KJ, et al. The IPAL-ICU Project. Integrating palliative care in the ICU: the nurse in a leading role. J Hosp Palliat Nurs. 2011;13:95–96. doi: 10.1097/NJH.0b013e318203d9ff. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Nelson JE, Puntillo KA, Pronovost PJ, Walker AS, McAdam JL, Ilaoa D, Penrod J. In their own words: patients and families define high-quality palliative care in the intensive care unit. Crit Care Med. 2010;38:808–818. doi: 10.1097/ccm.0b013e3181c5887c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pronovost P, Vohr E.Safe patients, smart hospitals: how one doctor’s checklist can help us change health care from the inside out. New York: Hudson Street Press; 2010 [Google Scholar]
- 40.Shaw DJ, Davidson JE, Smilde RI, Sondoozi T, Agan D. Multidisciplinary team training to enhance family communication in the ICU. Crit Care Med. 2014;42:265–271. doi: 10.1097/CCM.0b013e3182a26ea5. [DOI] [PubMed] [Google Scholar]