Abstract
Irritable bowel syndrome (IBS) is a common, chronic, functional gastrointestinal disorder with a high incidence rate in the general population, and it is common among the Chinese population. The pathophysiology, etiology and pathogenesis of IBS are poorly understood, with no evidence of inflammatory, anatomic, metabolic, or neoplastic factors to explain the symptoms. Treatment approaches are mainly focused on symptom management to maintain everyday functioning and to improve quality of life for patients with IBS. However, prescribed medications often result in significant side effects, and many IBS sufferers (particularly Chinese) do not improve. Instead of taking a variety of conventional medications, many have turned to taking traditional Chinese medicine or integrated Chinese and Western medicine for remedy. A number of clinical trials have shown that Chinese herbal, acupuncture or integrative therapies presented improved treatment outcomes and reduced side effects in IBS patients. The purpose of this review article is to examine the treatment approaches of IBS that have been published in recent years, especially in China, to assess the possible differences in treating IBS between China and other countries. This would provide some useful information of unique treatment approach in clinical practice for physicians in the management of IBS in China, thus offering more treatment options for IBS patients with potentially better treatment outcomes while reducing the medical cost burden.
Keywords: Irritable bowel syndrome, Integrated treatment, Traditional Chinese medicine, China
Core tip: Irritable bowel syndrome (IBS) is a common, chronic, functional gastrointestinal disorder highly prevalent in the general population, and it is common among Chinese population. The current review examines the differences between IBS treatment approaches in China and Western countries. The review reveals more treatment options in China in using traditional Chinese medicine (TCM) alone or in conjunction with conventional treatments, with the integration of TCM with Western medicine showing rather promising results. Besides providing extra treatment options, this information would foster future research for more effective treatment to provide IBS patients with better outcomes while reducing the financial burden.
INTRODUCTION
Irritable bowel syndrome (IBS) is a common, functional gastrointestinal disorder that is highly prevalent in the general population. Depending on the diagnostic criteria used to define the condition, it is reported to affect approximately 5%-20% of the general population worldwide[1,2]. Two large population surveys performed in China reported that the prevalence of IBS was estimated to be 7.26% (Manning criteria) or 0.82% (Rome criteria) in Beijing[3] and 11.5% (Manning criteria) or 5.67% (Rome criteria) in Guangdong[4].
IBS is characterized by recurrent abdominal pain and discomfort associated with alterations in the frequency or consistency of stool, that present as diarrhea or constipation. Based on the Rome III diagnostic criteria, which classify IBS according to different bowel behaviors, there are four subtypes: IBS-D (diarrhea-predominant), IBS-C (constipation-predominant), IBS-M (mixed), and unspecified IBS (IBS-U)[1,5]. Clinically, the complexity and diversity of IBS presentation make treatment difficult. In practice, clinicians generally make treatment decisions for symptom reduction in IBS according to the type and severity of the symptoms. However, many pharmacological treatment approaches are associated with side effects that result in a decreased benefit to the patient in terms of treatment outcomes[1]. Hence, IBS sufferers often have absenteeism, reduced health-related quality of life and multiple healthcare-seeking behaviors, leading to great social and economic burdens[6,7].
In terms of health care delivery, China has a unique cultural background in developing traditional Chinese medicine (TCM) as well as an extensive experience in its implementation. In fact, as opposed to other countries, TCM is practiced alongside conventional Western medicine in China. This is reflected by the substantial number of Chinese proprietary herbal medicines included in the National Essential Medicines List in China. Chinese physicians are often trained in both Western and Chinese medicine techniques and often use combined TCM and conventional Western medicine to manage different diseases and disorders. In recent years, due to dissatisfaction with conventional treatments, many IBS suffers have turned to alternative medicine, particularly TCM or integrated Chinese and Western medicine for remedy. A number of clinical trials have shown that TCM therapies alone or combined with Western medicine produced improved treatment outcomes in IBS patients[8-19]. However, as most of these studies were published in China, the results and potential benefits for IBS treatment using TCM or integrative therapies are little known in other countries.
This review will examine the differences between IBS treatment approaches in China and Western countries, with special attention to clinical research carried out in China, in order to provide alternative treatment options in clinical practice for physicians who manage IBS. Furthermore, we believe that this assessment would also foster and facilitate potential areas of future research for more effective treatment models, thus providing IBS patients with better treatment outcomes while reducing the medical cost burden.
CURRENT TREATMENT APPROACHES FOR IBS
Although IBS is a highly prevalent disease, there is still no universally accepted satisfactory treatment. As in Western countries[1], treatment approaches in China are also mainly focused on symptom management through lifestyle modification, psychotherapy and pharmacotherapy. The treatment objective is to maintain everyday functioning and improve quality of life. For clinical research, most of the performed clinical trials focused on the comparison between complementary and alternative medicines and on standard care with pharmacological therapies in treating IBS symptoms[11,20]. In the following sections, we will provide a brief description of treatment approaches commonly used in China to treat IBS.
Lifestyle modification
The first treatment option normally adopted is lifestyle modification. Common lifestyle modifications include encouraging regular exercise, sharp reductions in drinking, dietary changes, abstinence from alcohol and coffee, and developing regular sleeping habits. Physical activity is frequently used as a primary treatment modality in IBS. This is based on the results of many published studies showing the benefits of physical activity for IBS. A recently published randomized controlled trial (RCT) involving 102 patients with IBS showed that those who were randomized to physical activity group had fewer IBS symptoms compared with the control group[21]. Other studies also indicated that physical activity can improve patients’ moods and symptoms of fatigue, bloating and abdominal discomfort; regular physical activity can improve defecation patterns and colonic transit times in patients complaining of chronic constipation[11,22,23].
Regarding dietary changes, one Chinese research group reported that certain foods could contribute to IBS symptom onset. After eliminating certain specific food from the diet, the symptoms were alleviated to some extent in IBS patients[24]. Other Chinese clinical researchers have also linked the causation of IBS to food through a number of mechanisms, such as an allergy or intolerance to a particular food[25,26], which is similar to results from a Western study by Brandt et al[1]. Patients with IBS are advised to avoid fatty foods, beans and gas-producing foods that may contribute to symptoms of diarrhea, bloating and distension. For some patients with IBS-C, increasing the intake of foods high in soluble fiber can improve symptoms. Individual diet health management plans can be advocated[27].
If such non-pharmacological measures are unsuccessful, pharmacologic interventions are then recommended.
Psychotherapy
Psychological factors, such as certain depressive and anxiety disorders, play a role in the pathophysiology of IBS. Patients with IBS are more likely to have depression and “abnormal” behavior patterns, including anxiety and somatization symptoms[28]. In IBS patients, feelings of frustration, inadequacy and powerlessness in dealing with medically unexplained symptoms can also adversely affect both medical decision making and the physician-patient relationship.
Psychotherapies have been evaluated for their potential application in IBS. Patients, once diagnosed, should be educated and reassured about the non-life-threatening nature of the disease[14]. Mind-body therapies, such as hypnotherapy and cognitive-behavioral therapy, are effective in managing IBS symptoms[22]. Many Chinese clinical researchers are also focusing on psychological disturbances observed in IBS patients[14]. A study by Tang et al[29] found that most IBS patients complained of nonspecific somatic symptoms, such as dizziness, insomnia and fatigue. A further study by the same group reported that in young and middle-aged patients (18-57 years), quality of life was negatively correlated with anxiety and depression, but it was not associated with the severity of abdominal pain/discomfort[30]. The use of non-drug treatments for IBS is popular with patients who are disappointed by their lack of response to standard drug treatment or concerned about its potential side effects. Therefore, only improving gastrointestinal symptoms may not improve quality of life[30]. Clinical evidence has demonstrated that the use of psychological interventions in conjunction with conventional treatment can improve IBS symptoms and overall quality of life[26].
Pharmacotherapy
The available pharmacological approaches are mainly targeted at symptom reduction, as there is a wide range of the symptoms that may be experienced. These conventional pharmacological treatments include antispasmodics[31,32], antidiarrheals[1,33], laxatives or bulking agents[1,5], 5-hydroxytryptamine-3 (5-HT3) receptor antagonists, 5-HT4 receptor agonists[34], probiotics[35], tricyclic antidepressants[36], selective serotonin reuptake inhibitors[37], and antibiotics[38]. Antispasmodics plus stool consistency modifiers are usually the first-line drug treatment options to treat the major symptoms and defecation. Antidepressants are also commonly used for all subtypes of IBS. As gastrointestinal microbiota are thought to be involved in the pathogenesis of IBS, probiotics, when administered in adequate amounts, can sometimes be beneficial for the patient[39]. Table 1 summarizes the conventional pharmacological treatments for IBS in Western medicine[32].
Table 1.
Conventional pharmacological treatments for irritable bowel syndrome
| Drug category | Drug functions | Examples |
| Antispasmodics | Antagonists of muscarinic receptors and calcium channels of smooth muscle | Pinaverium bromide, mebeverine, trimebutine maleate |
| Antidiarrheals | μ-opioid receptors agonists | Loperamide |
| Laxatives | Osmotic, stimulant | Bisacodyl, polyethylene glycol, lactulose |
| Bulking agents | Water binding to increase stool bulk | Methylcellulose, psyllium |
| Receptor targeted | 5-HT3 receptor antagonists | Alosetron, cilansetron |
| 5-HT4 receptor agonists | Metoclopramide, domperidone | |
| Probiotics | To balance intestinal flora | Lactobacilli, bifidobacteriae |
| Psychiatrics | Tricyclic antidepressants | Amitriptyline, doxepin |
| Selective serotonin reuptake inhibitors | Citalopram, fluoxetine | |
| Antibiotics | To inhibit gut microorganisms | Neomycin, rifaximin |
These pharmacotherapeutic treatments are widely used in China, as in Western countries. However, the use of these medications has been limited by side effects, expensive drug costs, and high recurrence rates. In order to reduce symptoms of IBS and improve the quality of life of patients, other more effective therapies with fewer side effects, such as TCM, should be considered.
USE OF TCM FOR IBS IN CHINA
As a therapeutic discipline, TCM was derived and developed after many centuries of clinical practice and experience of traditional Chinese physicians. In China, many physicians consider TCM superior to the use of conventional Western medicine for IBS treatment[10,19]. Long-term clinical practice has accumulated rich experience and has perfected methods of employing TCM to treat the main symptoms of IBS[19]. Clinical evidence also shows that a combination of pharmacotherapy with TCM treatments provides the best symptom relief and highest quality of life for IBS patients[11,20]. According to the consensus of Chinese Society of Gastroenterology and the China Association of Integrative Medicine[40,41], the recommended procedure to treat IBS in China is shown in Figure 1.
Figure 1.
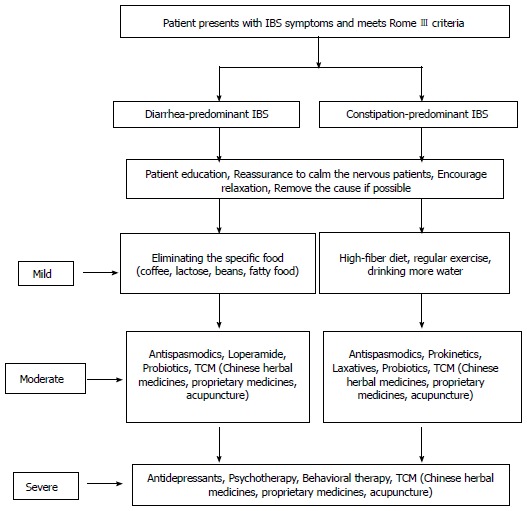
Flow diagram of the treatment of irritable bowel syndrome in China. IBS: Irritable bowel syndrome; TCM: Traditional Chinese medicine.
Chinese herbal medicines and proprietary medicines
Unique Chinese herbal mixtures and proprietary medicines have been used in China for a long time. Based on low levels of satisfaction with pharmacotherapy in the management of IBS, an increasing number of patients and practitioners have turned to herbal therapies for symptomatic relief. In recent years, the study of Chinese herbal medicines in managing IBS has gained much progress in China[13]. Chinese proprietary medicines, usually formulated as tablets or capsules for convenient administration, are frequently used for patients with special syndromes. TCM represents one aspect of the Chinese medical philosophy, which is characterized by its emphasis on maintaining and restoring balance in the human body. When used appropriately, herbal medicine may provide benefits in relieving symptoms and reducing their recurrence[14]. According to the symptoms assessment in TCM, patients might be diagnosed to have the nature of “cold” or “heat”, and whether this nature is “in deficiency” or “in excess”. The syndrome differentiation can then effectively guide the clinical treatment of the individuals with TCM[19]. Chinese herbal medicines can then be prescribed for different individuals based on the differentiation of symptoms according to traditional Chinese medicine diagnostic patterns. Hence, using Chinese herbal medicine is a strategy that provides the patient with individualized and comprehensive treatments[19].
Clinical studies by Chinese researchers have been performed on a number of herbal products either as single herbs or as combined products in managing IBS. The trials showed a significant reduction in abdominal pain and severity compared to placebo, and the herbs appeared to be safe[42,43]. Studies also confirmed that Chinese Shugan Jianpi Granules, when compared with Western medicine, showed better efficacy in treating patients with IBS-D[12,44]. Another study demonstrated the beneficial effects of herbal Tongxie Yaofang (TXYF) Granules in alleviating abdominal pain and distention, restoring normal stool consistency, reducing the frequency of defecation, and improving mental tension and depression in IBS-D patients[8]. Furthermore, another Chinese group had performed a systematic review about the effectiveness of TXYF alone and with different Chinese herbal additions (e.g., TXYF-A) in the management of IBS. They found that in the nine included studies, the TXYF-A group had better results than did the control group[9]. The evidence suggested that TXYF-A was useful and effective for IBS treatment. Another group retrieved literature from CNKI and screened effective medical records to establish a database using a structural electronic medical case collecting system. The methods of Chinese physicians to diagnose and treat IBS were then analyzed. They found that liver depression and spleen deficiency were the main diagnoses of pathogenesis for IBS. Hence, diagnosis and treatment of IBS should be performed clinically according to this pathogenesis, with TXYF used as the basic prescription with modification according to syndrome differentiation[10]. According to the results of these studies, Chinese herbal formulas may offer improvements of IBS symptoms globally.
Although treating IBS with TCM appears to be effective, safety is certainly another concern with the use of herbal medicines, as TCM is not without adverse effects. Shi et al[45] reviewed RCTs in the literature on IBS treatment with and without herbal medicine and found that herbal medicines had a therapeutic benefit in IBS with few adverse events. However, it is possible that because of the lack of rigorous monitoring, adverse effects including serious events may be under-reported. Hence, the side effects of Chinese herbal medicine such as liver toxicity and renal damage must be monitored. In addition, the long-term therapeutic effect as well as toxicity should be further observed through well-designed studies with larger samples[46]. Like using any therapy, clinicians should weigh the potential benefits and uncertainties when advising patients about using herbal medicines.
Acupuncture
Acupuncture, a well-known old therapeutic modality anchored in TCM, has been used to treat several gastrointestinal symptoms in functional and organic diseases in China for centuries. Acupuncture can regulate visceral reflex activity, gastric emptying, and acid secretion through affecting various endogenous neurotransmitter systems. Studies have shown that the application of acupuncture targeting serotonergic, cholinergic, and glutamatergic pathways in IBS patients can increase the concentration of endogenous opioids, which in turn reduces visceral and global pain perception[47-49].
A number of clinical trials investigating the effect of acupuncture on symptom relief in IBS patients have recently been conducted in China[50-52]. One clinical study on acupuncture to treat IBS-D patients with liver-stagnation and spleen-deficiency syndrome found that the clinical symptoms were improved after one week of treatment in the acupuncture group, which had a faster onset of effects than did the medicine treatment group. At the same time, the total effective rate was 90.48% in the acupuncture group compared with 78.95% in the medicine treatment group[50]. Another clinical study compared the therapeutic effects of electro-acupuncture with probiotics combined with Deanxit in treating IBS-D. The results indicated that both electro-acupuncture and Western medication could effectively treat IBS-D accompanied with anxiety and/or depression. However, while both groups showed improvement in IBS symptoms, electro-acupuncture had better long-term therapeutic effects[52]. Likewise, a study by Li et al[51] compared the therapeutic effects of acupuncture with Western medication on IBS-D symptom severity scores and quality of life scores and found a significant improvement in both scores over the course of four weeks as well as a remarkable reduction of the recurrence rate at 12 wk.
There were also meta-analyses evaluating the efficacy of acupuncture in managing IBS. A meta-analysis of 11 clinical RCTs with 969 patients through retrieval from CNKI and VIP showed the effective rate of acupuncture and moxibustion superior to conventional Western medication treatment[53]. Another meta-analysis of six RCTs also confirmed that acupuncture improved the symptoms of IBS, including abdominal pain and distension, sensations of incomplete defecation, times of defecation per day, and consistency of stool[54]. All these Chinese clinical trials and systemic reviews showed that acupuncture is beneficial and can achieve an improvement in quality of life for IBS patients. Furthermore, no serious adverse events associated with acupuncture were reported.
Acupuncture has gained increasing acceptance in Western medicine over the past few decades and is therefore an attractive treatment option for IBS. However, the efficiency of acupuncture in IBS is still inconclusive. Although Chinese trials reported greater benefits from acupuncture than from pharmacological therapies, other investigators from Western countries showed no significant differences after treatment with true or sham acupuncture. A recently published systematic review and meta-analysis of randomized controlled trials to estimate the effects of acupuncture for treating IBS found no benefits of acupuncture relative to a credible sham acupuncture control on IBS symptom severity or IBS-related quality of life[55]. Due to the conflicting conclusions between the meta-analyses conducted in China and in Western countries, further research is required to more accurately assess the efficacy and mechanism of action of acupuncture for IBS treatment. Future trials may help to clarify whether these reportedly greater benefits of acupuncture relative to pharmacological therapies are due entirely to patients’ preferences for acupuncture or to patients’ greater expectations of improvement with acupuncture relative to drugs[55].
Integrated traditional Chinese and Western medicine
In recent years, clinical investigators have paid more attention to integrated traditional Chinese and Western medicine. According to Chinese experts’ opinion, the integration of conventional pharmacological therapy and TCM treatment may provide long-term symptom alleviation and highest quality of life to IBS patients.
In fact, the combination of TCM with Western medicine has been used for a long time by Chinese practitioners to treat IBS[10]. A number of clinical trials as well as systematic reviews conducted and published in China have shown that the integrated approach is superior to either treatment alone[11,16-18,20,56]. These trials compared use of the combination of Chinese herbal medicines with Western medicine with use of Western medicine alone, and they used global improvement of symptoms as the main outcomes. A clinical study by Sun et al[18] reported that TXYF combined with Trimebutine and Bifid Lriple Viable capsules were effective in treating IBS-D. Wu et al[16] showed a statistically significant beneficial effect of using a Chinese medication called Anshen Ningchang Tang in combination with Trimebutine over Trimebutine treatment alone. A RCT study showed that Shugan Jianpi Granules, a Chinese herbal medication, reduced the number of gut mucosal serotonin-positive cells in patients with IBS-D, and its effect was enhanced when used in combination with conventional recognition-behavior therapy and symptomatic treatment by Western medicine[44]. Another Chinese study also reported a better efficacy of the combination use of psychotherapy and TXYF over TXYF alone[57]. All these studies provided evidence to support the efficacy of the combination of TCM with Western medicine in managing IBS. Conceptually, the use of combination therapy with TCM and Western medicine for IBS is in line with recommendation of using combination therapy by America College of Gastroenterology and the British Society for Gastroenterology[1].
Recently, our research group evaluated the clinical efficacy of the combination of TCM and Western medicine in the treatment of IBS via a series of meta-analyses. Compared to the Western medicine treatment alone, our results showed that TCM combined with Western pharmacological interventions significantly improved global symptoms of IBS (RR = 1.21; 95%CI: 1.18-1.24). Moreover, the relapse rate was lower, and no serious adverse events were reported. These results would provide further evidence indicating that treating IBS with integrated traditional Chinese medicine with Western medicine showed better efficacy than treating with conventional Western medicine alone.
CONCLUSION
Despite the wide range of available medications and the continuous development of new drugs, the management of IBS remains a challenge, and to date, no completely effective remedy is available. Compared to treatment options available to physicians in other countries, physicians from China have the additional options in the use of TCM, including Chinese herbal medicines and acupuncture, in addition to conventional medicines available to other countries to treat IBS based on the individual symptoms presented in each IBS patient. These strategies have produced beneficial effects, with lower adverse effects and lower reoccurrence rates. These additional treatment approaches from China may provide good options for the best symptom relief and highest quality of life to IBS patients. Among these, the integration of Chinese herbal medicine with conventional Western medicine appears rather promising.
Footnotes
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Peer-review started: July 25, 2014
First decision: September 27, 2014
Article in press: December 16, 2014
P- Reviewer: Leung PC S- Editor: Yu J L- Editor: Wang TQ E- Editor: Zhang DN
References
- 1.Brandt LJ, Chey WD, Foxx-Orenstein AE, Schiller LR, Schoenfeld PS, Spiegel BM, Talley NJ, Quigley EM. An evidence-based position statement on the management of irritable bowel syndrome. Am J Gastroenterol. 2009;104 Suppl 1:S1–35. doi: 10.1038/ajg.2008.122. [DOI] [PubMed] [Google Scholar]
- 2.Liu J, Hou X. A review of the irritable bowel syndrome investigation on epidemiology, pathogenesis and pathophysiology in China. J Gastroenterol Hepatol. 2011;26 Suppl 3:88–93. doi: 10.1111/j.1440-1746.2011.06641.x. [DOI] [PubMed] [Google Scholar]
- 3.Pan G, Lu S, Ke M, Han S, Guo H, Fang X. [An epidemiologic study of irritable bowel syndrome in Beijing - a stratified randomized study by clustering sampling] Zhonghua Liu Xing Bing Xue Zazhi. 2000;21:26–29. [PubMed] [Google Scholar]
- 4.Xiong LS, Chen MH, Chen HX, Xu AG, Wang WA, Hu PJ. [A population-based epidemiologic study of irritable bowel syndrome in Guangdong province] Zhonghua Yi Xue Zazhi. 2004;84:278–281. [PubMed] [Google Scholar]
- 5.Longstreth GF, Thompson WG, Chey WD, Houghton LA, Mearin F, Spiller RC. Functional bowel disorders. Gastroenterology. 2006;130:1480–1491. doi: 10.1053/j.gastro.2005.11.061. [DOI] [PubMed] [Google Scholar]
- 6.Ringel Y, Williams RE, Kalilani L, Cook SF. Prevalence, characteristics, and impact of bloating symptoms in patients with irritable bowel syndrome. Clin Gastroenterol Hepatol. 2009;7:68–72; quiz 3. doi: 10.1016/j.cgh.2008.07.008. [DOI] [PubMed] [Google Scholar]
- 7.Nellesen D, Yee K, Chawla A, Lewis BE, Carson RT. A systematic review of the economic and humanistic burden of illness in irritable bowel syndrome and chronic constipation. J Manag Care Pharm. 2013;19:755–764. doi: 10.18553/jmcp.2013.19.9.755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pan F, Zhang T, Zhang YH, Xu JJ, Chen FM. Effect of Tongxie Yaofang Granule in treating diarrhea-predominate irritable bowel syndrome. Chin J Integr Med. 2009;15:216–219. doi: 10.1007/s11655-009-0216-7. [DOI] [PubMed] [Google Scholar]
- 9.Bian Z, Wu T, Liu L, Miao J, Wong H, Song L, Sung JJ. Effectiveness of the Chinese herbal formula TongXieYaoFang for irritable bowel syndrome: a systematic review. J Altern Complement Med. 2006;12:401–407. doi: 10.1089/acm.2006.12.401. [DOI] [PubMed] [Google Scholar]
- 10.Zhang BH, Gao R, Li ZH, Li BS, Wang FY, Tang XD. [Treatment of irritable bowel syndrome by Chinese medicine and pharmacy: an analysis of data mining on experiences of experts] Zhongguo Zhong Xi Yi Jie He Zazhi. 2013;33:757–760. [PubMed] [Google Scholar]
- 11.Grundmann O, Yoon SL. Complementary and alternative medicines in irritable bowel syndrome: an integrative view. World J Gastroenterol. 2014;20:346–362. doi: 10.3748/wjg.v20.i2.346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tao Y, Chen DM, Dong MX, Wu ZH. The clinical study on Shugan decoction in treating diarrhea-predominant irritable bowel syndrome. Zhonghua Zhongyiyao Xuekan. 2007;27:48–50. [Google Scholar]
- 13.Liu YD, Tao HW. The progress of Chinese medicine treatment to IBS. Zhonghua Zhongyiyao Xuekan. 2009;27:767–769. [Google Scholar]
- 14.Wang JW. Irritable Bowel Syndrome and Relationship Between Emotional Factors Probe. Zhongguo Shiyong Neike Zazhi. 2011;25:56–58. [Google Scholar]
- 15.Zhang SS, Wang HB, Li ZH. [A multi-center randomized controlled trial on treatment of diarrhea-predominant irritable bowel syndrome by Chinese medicine syndrome-differentiation therapy] Zhongguo Zhong Xi Yi Jie He Zazhi. 2010;30:9–12. [PubMed] [Google Scholar]
- 16.Wu XH, Wang ZL, Wang JY. Treatment of 67 irritable bowel syndrome cases with integrated traditional Chinese and western medicine. Zhognwai Yixue Yanjiu. 2010;8:29–30. [Google Scholar]
- 17.Wang DB. Treatment of IBS with integrated trational Chinese and western medicine. Zhongguo Minkang Yixue. 2009;21:73–74. [Google Scholar]
- 18.Sun YL, Zhao XD. Treatment of irritable bowel syndrome with modified Tongxieyaofang: A 83 cases study. Guoji Zhongyi Zhongyao Zazhi. 2009;31:429–430. [Google Scholar]
- 19.Tang ZP. Traditional Chinese medicine clinical experience of the treatment for irritable bowel syndrome. Chin J Integr Med. 2009;15:93–94. doi: 10.1007/s11655-009-0093-0. [DOI] [PubMed] [Google Scholar]
- 20.Grundmann O, Yoon SL. Irritable bowel syndrome: epidemiology, diagnosis and treatment: an update for health-care practitioners. J Gastroenterol Hepatol. 2010;25:691–699. doi: 10.1111/j.1440-1746.2009.06120.x. [DOI] [PubMed] [Google Scholar]
- 21.Johannesson E, Simrén M, Strid H, Bajor A, Sadik R. Physical activity improves symptoms in irritable bowel syndrome: a randomized controlled trial. Am J Gastroenterol. 2011;106:915–922. doi: 10.1038/ajg.2010.480. [DOI] [PubMed] [Google Scholar]
- 22.Yoon SL, Grundmann O, Koepp L, Farrell L. Management of irritable bowel syndrome (IBS) in adults: conventional and complementary/alternative approaches. Altern Med Rev. 2011;16:134–151. [PubMed] [Google Scholar]
- 23.De Schryver AM, Keulemans YC, Peters HP, Akkermans LM, Smout AJ, De Vries WR, van Berge-Henegouwen GP. Effects of regular physical activity on defecation pattern in middle-aged patients complaining of chronic constipation. Scand J Gastroenterol. 2005;40:422–429. doi: 10.1080/00365520510011641. [DOI] [PubMed] [Google Scholar]
- 24.Yang CM, Li YQ. [The therapeutic effects of eliminating allergic foods according to food-specific IgG antibodies in irritable bowel syndrome] Zhonghua Nei Ke Zazhi. 2007;46:641–643. [PubMed] [Google Scholar]
- 25.Wang EM, Yan XJ, Chen SL. Advances in study on food factor in irritable bowel syndrome. Wei Chang Bing Xue. 2012;17:633–635. [Google Scholar]
- 26.Liu L, Yao SK. The possible related pathogenic factors and mechanisms in irritable bowel syndrome. Weichangbingxue He Ganbingxue Zazhi. 2013;22:1055–1058. [Google Scholar]
- 27.Yang X, Wang YZ, Yie N, Wang Y, Zhao J, Zhang S, Fang J, Zhou HF. Effects of individual diet health management on patients with constipation-predominant irritable bowel syndrome. Zhonghua Linchuang Yishi Zazhi. 2013;7:8233–8236. [Google Scholar]
- 28.Blanchard EB, Lackner JM, Jaccard J, Rowell D, Carosella AM, Powell C, Sanders K, Krasner S, Kuhn E. The role of stress in symptom exacerbation among IBS patients. J Psychosom Res. 2008;64:119–128. doi: 10.1016/j.jpsychores.2007.10.010. [DOI] [PubMed] [Google Scholar]
- 29.Tang YR, Yang WW, Wang YL, Lin L. Sex differences in the symptoms and psychological factors that influence quality of life in patients with irritable bowel syndrome. Eur J Gastroenterol Hepatol. 2012;24:702–707. doi: 10.1097/MEG.0b013e328351b2c2. [DOI] [PubMed] [Google Scholar]
- 30.Tang YR, Yang WW, Liang ML, Xu XY, Wang MF, Lin L. Age-related symptom and life quality changes in women with irritable bowel syndrome. World J Gastroenterol. 2012;18:7175–7183. doi: 10.3748/wjg.v18.i48.7175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Darvish-Damavandi M, Nikfar S, Abdollahi M. A systematic review of efficacy and tolerability of mebeverine in irritable bowel syndrome. World J Gastroenterol. 2010;16:547–553. doi: 10.3748/wjg.v16.i5.547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chang FY. Irritable bowel syndrome: the evolution of multi-dimensional looking and multidisciplinary treatments. World J Gastroenterol. 2014;20:2499–2514. doi: 10.3748/wjg.v20.i10.2499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Regnard C, Twycross R, Mihalyo M, Wilcock A. Loperamide. J Pain Symptom Manage. 2011;42:319–323. doi: 10.1016/j.jpainsymman.2011.06.001. [DOI] [PubMed] [Google Scholar]
- 34.Ford AC, Brandt LJ, Young C, Chey WD, Foxx-Orenstein AE, Moayyedi P. Efficacy of 5-HT3 antagonists and 5-HT4 agonists in irritable bowel syndrome: systematic review and meta-analysis. Am J Gastroenterol. 2009;104:1831–143; quiz 1844. doi: 10.1038/ajg.2009.223. [DOI] [PubMed] [Google Scholar]
- 35.Ortiz-Lucas M, Tobías A, Saz P, Sebastián JJ. Effect of probiotic species on irritable bowel syndrome symptoms: A bring up to date meta-analysis. Rev Esp Enferm Dig. 2013;105:19–36. doi: 10.4321/s1130-01082013000100005. [DOI] [PubMed] [Google Scholar]
- 36.Rahimi R, Nikfar S, Rezaie A, Abdollahi M. Efficacy of tricyclic antidepressants in irritable bowel syndrome: a meta-analysis. World J Gastroenterol. 2009;15:1548–1553. doi: 10.3748/wjg.15.1548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bundeff AW, Woodis CB. Selective serotonin reuptake inhibitors for the treatment of irritable bowel syndrome. Ann Pharmacother. 2014;48:777–784. doi: 10.1177/1060028014528151. [DOI] [PubMed] [Google Scholar]
- 38.Rezaie A, Nikfar S, Abdollahi M. The place of antibiotics in management of irritable bowel syndrome: a systematic review and meta-analysis. Arch Med Sci. 2010;6:49–55. doi: 10.5114/aoms.2010.13507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Stevenson C, Blaauw R. Probiotics, with special emphasis on their role in the management of irritable bowel syndrome. S Afr Clin Nutr. 2011;24:63–73. [Google Scholar]
- 40.Study group of gastrointestinal motility, Chinese Society of Digestive Diseases, Chinese Medical Association. Consensus on the diagnosis and treatment of irritable bowel syndrome (2007,Changsha) Zhongguo Xiaohua Zazhi. 2008;28:38–40. [Google Scholar]
- 41.China Association of Integrative Medicine Professional Committee of digestive disease. Consensus on the diagnosis and treatment of irritable bowel syndrome with integrative Chinese and Westernmedicine (2010, Suzhou) Chin J Integr Med. 2011;31:587–590. [Google Scholar]
- 42.Tan HC. Treating 95 cases of diarrhea-predominant irritable bowel syndrome by invigorating spleen and soothing liver. Zhongyi Linchuang Yanjiu. 2011;3:32–33. [Google Scholar]
- 43.Niu SL. Clinical effect of the Sijunzi decoction plus Tongxie prescription on treating 36 cases of IBS of diarrhea type. Zhongyi Linchuang Yanjiu. 2013;5:79–81. [Google Scholar]
- 44.Wang ZJ, Li HX, Wang JH, Zhang F. Effect of Shugan Jianpi Granule () on gut mucosal serotonin-positive cells in patients with irritable bowel syndrome of stagnated Gan-qi attacking Pi syndrome type. Chin J Integr Med. 2008;14:185–189. doi: 10.1007/s11655-008-9001-2. [DOI] [PubMed] [Google Scholar]
- 45.Shi J, Tong Y, Shen JG, Li HX. Effectiveness and safety of herbal medicines in the treatment of irritable bowel syndrome: a systematic review. World J Gastroenterol. 2008;14:454–462. doi: 10.3748/wjg.14.454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Liu JP, Yang M, Liu YX, Wei M, Grimsgaard S. Herbal medicines for treatment of irritable bowel syndrome. Cochrane Database Syst Rev. 2006;(1):CD004116. doi: 10.1002/14651858.CD004116.pub2. [DOI] [PubMed] [Google Scholar]
- 47.Ma XP, Tan LY, Yang Y, Wu HG, Jiang B, Liu HR, Yang L. Effect of electro-acupuncture on substance P, its receptor and corticotropin-releasing hormone in rats with irritable bowel syndrome. World J Gastroenterol. 2009;15:5211–5217. doi: 10.3748/wjg.15.5211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Zhou EH, Liu HR, Wu HG, Shi Y, Wang XM, Tan LY, Yao LQ, Zhong YS, Jiang Y, Zhang LL. Suspended moxibustion relieves chronic visceral hyperalgesia via serotonin pathway in the colon. Neurosci Lett. 2009;451:144–147. doi: 10.1016/j.neulet.2008.12.026. [DOI] [PubMed] [Google Scholar]
- 49.Tian SL, Wang XY, Ding GH. Repeated electro-acupuncture attenuates chronic visceral hypersensitivity and spinal cord NMDA receptor phosphorylation in a rat irritable bowel syndrome model. Life Sci. 2008;83:356–363. doi: 10.1016/j.lfs.2008.06.027. [DOI] [PubMed] [Google Scholar]
- 50.Wu XL, Wang YL, Sun JH, Shu YY, Pei LX, Zhou JL, Chen D, Zhang JW, Zhan DW. [Clinical observation on acupuncture for diarrhea-predominant irritable bowel syndrome patients in syndrome of liver-stagnation and spleen-deficiency and its impact on Th1/Th2] Zhongguo Zhen Jiu. 2013;33:1057–1060. [PubMed] [Google Scholar]
- 51.Li H, Pei LX, Zhou JL. [Comparative observation on therapeutic effects between acupuncture and western medication for diarrhea-predominant irritable bowel syndrome] Zhongguo Zhen Jiu. 2012;32:679–682. [PubMed] [Google Scholar]
- 52.Chen YH, Chen XK, Yin XJ. [Comparison of the therapeutic effects of electroacupuncture and probiotics combined with deanxit in treating diarrhea-predominant irritable bowel syndrome] Zhongguo Zhong Xi Yi Jie He Zazhi. 2012;32:594–598. [PubMed] [Google Scholar]
- 53.Pei LX, Zhang XC, Sun JH, Geng H, Wu XL. [Meta analysis of acupuncture-moxibustion in treatment of irritable bowel syndrome] Zhongguo Zhen Jiu. 2012;32:957–960. [PubMed] [Google Scholar]
- 54.Chao GQ, Zhang S. Effectiveness of acupuncture to treat irritable bowel syndrome: a meta-analysis. World J Gastroenterol. 2014;20:1871–1877. doi: 10.3748/wjg.v20.i7.1871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Manheimer E, Wieland LS, Cheng K, Li SM, Shen X, Berman BM, Lao L. Acupuncture for irritable bowel syndrome: systematic review and meta-analysis. Am J Gastroenterol. 2012;107:835–47; quiz 848. doi: 10.1038/ajg.2012.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wang X, Zhu JM. Clinical experience on integrared traditional Chinese and western medicine in treatment of 58 patients with constipation type irritable bowel syndrome. Xiandai Yiyao Yu Jiankang. 2009;25:2260–2261. [Google Scholar]
- 57.Li N, Zhang QW, Liu D. Clinical efficacy observation of the treatment on diarrhea-predominant irritable bowel syndrome by the combination of psychotherapy and Tongxieyaofang. Liaoning Zhongyiyao Daxue Xuebao. 2012;14:172–174. [Google Scholar]


