Abstract
Objective
Conduct a pilot trial of a new dissonance-based group eating disorder treatment designed to be a cost-effective front-line transdiagnostic treatment that could be more widely disseminated than extant individual or family treatments that are more expensive and difficult to deliver.
Method
Young women with a DSM-5 eating disorder (N = 72) were randomized to an 8-week dissonance-based Body Acceptance Therapy group treatment or a usual care control condition, completing diagnostic interviews and questionnaires at pre, post, and 2-month follow-up.
Results
Intent-to-treat analyses revealed that intervention participants showed greater reductions in outcomes than usual care controls in a multivariate multilevel model (χ2[6] = 34.1, p < .001), producing large effects for thin-ideal internalization (d = 0.79), body dissatisfaction (d = 1.14), and blinded interview-assessed eating disorder symptoms (d = .95), and medium effects for dissonance regarding perpetuating the thin ideal (d = .65) and negative affect (d = .55). Midway through this pilot we refined engagement procedures, which was associated with increased effect sizes (e.g., the d for eating disorder symptoms increased from .51 to 2.30).
Conclusions
This new group treatment produced large reductions in eating disorder symptoms, which is encouraging because it requires about 1/20th the therapist time necessary for extant individual and family treatments, and has the potential to provide a cost-effective and efficacious approach to reaching the majority of individuals with eating disorders who do not presently received treatment.
Keywords: eating disorder, treatment, group, efficacy trial, dissonance
Eating disorders affect 13-15% of females (Allen, Byrne, Oddy, & Crosby, 2013; Stice, Marti, & Rohde, 2013c). The fact that over 50% of individuals seeking treatment meet criteria for an eating disorder not otherwise specified (EDNOS), such as subthreshold bulimia nervosa or purging disorder (Eddy et al., 2008; Fairburn & Bohn, 2005), rather than for a full threshold Diagnostic and Statistical Manual (DSM)-IV eating disorder, prompted an expansion of eating disorder diagnoses for DSM-V. Eating disorders are marked by chronicity, relapse, distress, functional impairment, and risk for future obesity, depression, suicide attempts, anxiety disorders, substance abuse, and morbidity (Crow et al., 2009; le Grange et al., 2006; Swanson et al., 2011). The standardized mortality ratio (observed deaths in a population/expected deaths) is 5.9 for anorexia nervosa and 1.9 for bulimia nervosa and EDNOS (Arcelus et al., 2011).
Several treatments have received empirical support relative to usual care control conditions (we focus on trials that used a similar control condition to aid cross-trial comparison). Cognitive-behavioral therapy (CBT) is effective for bulimia nervosa, producing larger pre-post reductions in symptoms (M d = .94) and remission rates than control conditions (29-52% vs. 6-24%) (e.g., Kirkley, Schneider, Agras, & Bachman, 1985; Spielmans et al., 2013). CBT is also effective for binge eating disorder, producing larger pre-post symptom reductions (M d = 1.07) and remission rates than control conditions (39-73% vs. 0-30%) (e.g., Grilo, Masheb, & Wilson, 2005; Peterson et al., 2009). Family therapy for anorexia nervosa has produced small symptom reductions (d = .37) and remission rates (14% vs. 0%) relative to usual care after 1 year (Dare et al., 2001).
Although eating disorders are pernicious, 80-97% of afflicted individuals do not receive treatment (Swanson et al., 2011), in part because it is difficult to locate clinicians who deliver evidence-based treatments and because training is intensive and only offered at select sites (Zandberg & Wilson, 2013). For instance, training to deliver enhanced CBT takes 6 months (Fairburn et al., 2009). Thus, even those who do receive eating disorder treatment typically do not receive evidence-based interventions (Lilienfeld et al., 2013). Further, current treatments for eating disorders are very intensive, typically requiring 20 individual sessions delivered over 6 months (Wilson & Zandberg, 2012) and expensive, approximating the cost of treatment for schizophrenia (Striegel-Moore et al., 2000). The fact that treatments differ for the various eating disorders also complicates intervention delivery. These factors have hindered broad dissemination of extant eating disorder treatments, suggesting that it would be useful to develop a brief front-line treatment for the spectrum of DSM-5 eating disorders that could be easily, inexpensively, and widely disseminated.
Guided bibliotherapy for eating disorders is one solution to the paucity of clinicians who can deliver evidence-based treatments (Wilson & Zandberg, 2012). Yet, findings have been mixed, with some trials suggesting that bibliotherapy is as efficacious as alternative interventions (Grilo & Masheb, 2005; Schmidt et al., 2007; Wilson, 2010), others producing small effects (Mitchell et al., 2011; Thiels et al., 1998), and still others finding virtually no effects (Steele & Wade, 2008; Walsh et al., 2004). Plus, bibliotherapy has only received support for bulimia nervosa and binge eating disorder, not other eating disorders (Wilson & Zandberg, 2012).
Another limitation of extant treatments is that individuals often report continued pursuit of the thin ideal and body dissatisfaction after termination, which often leads to relapse (Bardone-Cone et al., 2010). This implies that a treatment that is effective in reducing these factors would be optimal.
It may be possible to translate the intervention theory from an effective and widely disseminated eating disorder prevention program into a new front-line treatment that could be easily and inexpensively disseminated. Although a few prevention programs have reduced eating disorder symptoms in single trials (e.g., Jones et al., 2008; McVey, Tweed, & Blackmore, 2007), more empirical support has emerged for a dissonance-based prevention program (the Body Project; Stice, Shaw, Burton, & Wade, 2006). In this selective prevention program young women with body image concerns voluntarily critique the thin ideal in verbal, written, and behavioral exercises (e.g., they argue the group facilitator out of pursuing this ideal in role-plays and write a letter to a younger girl about how to avoid body dissatisfaction). Criticizing the thin ideal publically theoretically reduces pursuit of the thin ideal because people seek to maintain consistency between their behaviors and attitudes. The reduced subscription to the thin ideal putatively decreases body dissatisfaction, negative affect, unhealthy weight control behaviors, eating disorder symptoms, and future eating disorder onset. Thus, this intervention targets a linchpin risk factor that is at the headwaters of a cascade of risk processes that appear to lead to eating disorders. We target young women with body dissatisfaction because it is the most robust risk factor for predicting future onset of eating disorders (e.g., Beato-Fernandez et al., 2004; McKnight, 2003; Stice, Marti, & Durant, 2011).
Efficacy and effectiveness trials have found that the Body Project produces greater reductions in risk factors (e.g., thin-ideal internalization, body dissatisfaction), eating disorder symptoms, and eating disorder onset over a 3-year follow-up than alternative interventions and assessment-only controls (Becker, Smith, & Ciao, 2005; Halliwell & Diedrichs, 2013; Matusek, Wendt, & Wiseman, 2004; Mitchell, Mazzeo, Rausch, & Cooke, 2007; Stice, Butryn, Rohde, Shaw, & Marti, 2013b; Stice, Marti, Spoor, Presnell, & Shaw, 2008b; Stice, Rohde, Shaw, & Gau, 2011; Stice et al., 2006). It is the only prevention program that has reduced eating disorder onset, produced effects through 3-year follow-up, outperformed alternative interventions, and produced independently replicated effects.
In support of the intervention theory, reductions in thin-ideal internalization mediate effects of the Body Project on symptom reductions (Seidel, Presnell, & Rosenfield, 2009; Stice, Presnell, Gau, & Shaw, 2007) and participants assigned to high- versus low-dissonance versions of this program showed greater symptom reductions (Green, Scott, Diyankova, Gasser, & Pederson, 2005; McMillan, Stice, & Rohde, 2011). The Body Project produced larger effects for those with initial elevations in thin-ideal internalization (Stice, Marti, Shaw, & O'Neil, 2008a), consistent with the thesis that they should experience more dissonance. The Body Project reduced the risk conveyed by the most potent baseline risk factor in one trial - denial of the costs of pursuing the thin ideal (Stice, Rohde, Gau, & Shaw, 2012): among participants with this risk factor, those who completed the Body Project showed an eating disorder incidence of 0% over 3-year follow-up versus 18% for those who completed alternative interventions and 50% for assessment-only controls. The Body Project also eliminated the effect of exposure to thin models on body dissatisfaction in young girls (Halliwell & Diedrichs, 2013). Further, participants who completed the Body Project showed a greater pre-post reduction in functional magnetic resonance imaging (fMRI) assessed caudate (a reward region) response to images of thin models and anterior cingulate (an attention region) response to thin-ideal statements relative to controls (Stice, Becker, & Yokum, 2013a), implying participants may not perceive the thin ideal as a desirable goal and may allocate less attention to thin-ideal statements after completing this prevention program.
A moderator paper found that the Body Project produced significantly larger eating disorder symptom reductions for participants with elevated pretest symptoms (Stice et al., 2008a), prompting us to pool data from 3 trials to test whether this program produced stronger effects for those with versus without a DSM-5 eating disorder at baseline (anorexia nervosa = 7, bulimia nervosa = 20, binge eating disorder = 23, atypical anorexia nervosa = 8, subthreshold bulimia nervosa = 12, subthreshold binge eating disorder = 10, purging disorder = 9). It produced significantly stronger pre-post symptom reductions for those with versus without an eating disorder at pretest (d = .71 and .18 respectively; Müller & Stice, 2013). Given that the Body Project has produced large clinically meaningful symptom reductions for individuals with DSM-5 eating disorders and has been widely disseminated, we developed a new dissonance-based eating disorder treatment, referred to as Body Acceptance Therapy. The present report describes a preliminary evaluation of this new dissonance-based group treatment relative to a usual-care control condition.
Several considerations guided the design of this new treatment. First, we retained the Body Project exercises wherein participants critique the thin ideal, which putatively creates dissonance about pursuing this unrealistic ideal, because these exercises reduce thin-ideal internalization and eating disorder symptoms. It is vital to decrease thin-ideal internalization because pursuit of this ideal predicts maintenance of eating disorder symptoms (Bohon, Stice, & Spoor, 2009; Stice & Agras, 1998) and is often a residual problem after treatment. Second, we developed new verbal, written, and behavioral exercises designed to produce dissonance about body image concerns, which also predicts eating disorder symptom maintenance (Bohon et al., 2009, Fairburn et al., 2003), and engaging in the specific eating disordered behaviors endorsed by each participant, as this would allow this treatment to be offered to individuals with a variety of eating disorders. For instance, participants discuss the interpersonal costs of body dissatisfaction and the health costs of eating disorder symptoms, which should promote body acceptance and motivate participants to discontinue disordered eating. By asking each participant to discuss the costs of their particular symptoms, the treatment naturally adapts to a range of eating disorders. Thus, in contrast to the Body Project, which focuses solely on producing dissonance about thin-ideal internalization, Body Acceptance Therapy focuses on producing dissonance about thin-ideal internalization, body dissatisfaction, and eating disorder symptoms. Third, we wanted to keep this intervention brief to minimize implementation cost and complexity, and to enhance retention. The Body Project has been successfully disseminated broadly in part because it is much briefer than other eating disorder prevention programs and can thus be easily implemented. Fourth, sessions first focus on reducing pursuit of the thin ideal and body image concerns before turning to the more sensitive topic of creating dissonance about engaging in core eating disorder symptoms because we thought reducing subscription to the thin ideal and improving body satisfaction would increase willingness to reduce symptoms.
Methods
Participants and Procedure
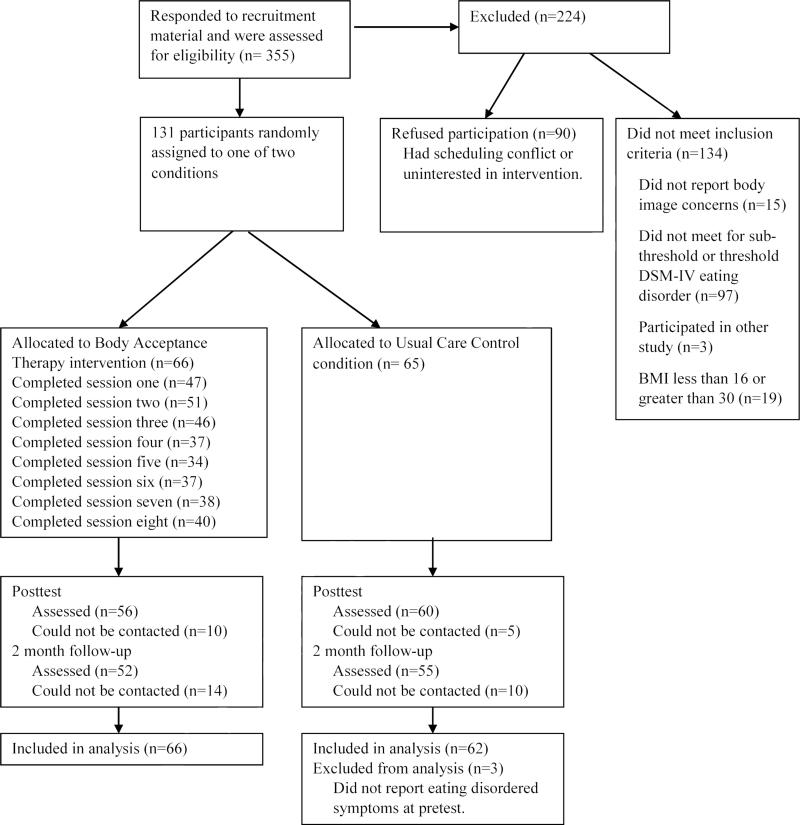
A total of 136 young women recruited from universities in Oregon, Texas, and Pennsylvania initially enrolled based on data provided on a web-screener for eating pathology. However, 64 did not meet criteria for a DSM-5 eating disorder at the pretest diagnostic interview, which was the central inclusion criteria, and were therefore excluded from analyses. The 72 remaining participants had a mean age = 23.7 (SD = 7.3) and a mean BMI (kg/m2) = 24.3 (SD = 5.3). The sample was 54% European American, 15% Asian/Pacific Islander, 23% Hispanic, 6% African American, and 1% American Indian/Alaska Native. Parental education (highest of mother or father) was 14% high school graduate or less, 14% some college, 38% college graduate, and 34% advanced graduate or professional degree. Participants were randomized to the Body Acceptance Therapy (n = 43) or a usual care control condition (n = 29) using a random number table (see Figure 1 for participant flowchart). The intervention consisted of 8 weekly 1-hour group sessions with 4-10 participants. Participants completed assessments at pretest, posttest [2-months later], and 2-months after posttest.
Figure 1.
Participant flow throughout the study.
Facilitators had either a doctoral or master's degree in clinical psychology. Facilitator training involved reading the intervention manual and attending a 4-hour workshop to learn the rationale for the Body Acceptance Therapy group intervention, role-played intervention components, and discussed process issues (e.g., homework compliance and retention). During delivery of a Body Acceptance Therapy group, facilitators tracked each participant's attendance (4-point scale; absent, partial attendance, full attendance, make-up session), participation (3-point scale; none or negative, minimal, good/active), and homework completion level (4-point scale; none, some, all, didn't bring materials). Treatment sessions were videorecorded and reviewed by supervisors (second and third authors), who provided emailed supervision before the next treatment session.
The no-show rate and attrition from the first few groups was relatively high, as is common in eating disorder treatment trials (Dare et al., 2001; Grilo et al., 2005; Peterson et al., 2009). This prompted us to refine our engagement procedures midway through this preliminary trial. To maximize initial attendance we asked facilitators to call participants assigned to the intervention a few days before the first session to introduce themselves, describe the topics discussed in the sessions and how beneficial past participants have found the intervention, encourage them to read testimonial letters from participants who had previously completed the intervention (posted on the Internet), and address any concerns voiced by the participant. To promote retention, facilitators began to note that past participants who attended all of the sessions showed the greatest benefit from the group. To promote home exercise completion, facilitators began to note that past participants who did all of the home exercises showed the greatest benefit from the group, increased in-session accountability to complete the home exercises, and better explained their clinical value. We also began asking all participants to eat 3 healthy meals a day for their first eating disorder symptom behavioral challenge in rather than allowing them to identify their personal linchpin symptom because meal skipping appeared to increase binge eating later in the day and this standard change is a less threatening request than other possibilities.
Body Acceptance Therapy
Session 1
group members are asked to voluntarily participate verbally in the session (all sessions start this way), complete an in-session motivational writing exercise about the importance of improving body satisfaction, collectively define the thin-ideal, discuss costs of pursuing this ideal, and are assigned home exercises (write a letter to a younger adolescent girl about the costs of pursuing the thin ideal; complete a mirror-based self-affirmation exercise).
Session 2
participants read their letter to a younger girl about the cost of pursuing the thin ideal to the group, which are recorded so participants could post the letter or video of them reading the letter on the Internet, discuss the self-affirmation home exercise and share what they most like about themselves, dissuade facilitators from pursuing the thin ideal in role-plays, and are assigned home exercises (write a letter to someone who pressured them to be thinner, saying how the message affected them and how they would respond now to that comment; generate a top-10 list of “body activism” behaviors young women can do to challenge the thin-ideal).
Session 3
participants read their “rewind response” letter, complete a motivational in-session writing exercise about the interpersonal consequences of their body image concerns, discuss behaviors they avoid because of body image concerns (e.g., wearing shorts), are asked to engage in a behavior that they avoid because of body image concerns twice as a home exercise, discuss the Top 10 list of body activism behaviors, and are asked to do 2 acts of body activism for a home exercise (e.g., hang a “love your body” poster in a women's bathroom on campus).
Session 4
participants discuss their body image behavioral challenge and body activism home exercises, briefly challenge thin-ideal statements made by facilitators in role-plays, and are assigned home exercises (begin consuming 3 healthy meals daily; write a letter to a younger adolescent girl about avoiding body image concerns).
Session 5
participants discuss their progress on eating 3 healthy meals a day, review negative effects of binge eating, read the letter they wrote to a younger girl about avoiding body image concerns, complete a motivational in-session writing exercise discussing the importance of resolving disordered eating behaviors, and are assigned home exercises (reduce their linchpin eating disorder behavior [e.g., binge eating, which prompts use of compensatory behaviors], which is referred to as an eating disorder behavior challenge; create a brief presentation on the adverse effects of an eating disorder).
Session 6
participants give their 1-minute presentation on adverse effects of eating disorders, discuss their eating disorder behavior challenge home exercise, discuss health costs of eating disorders, and are assigned home exercises (reduce their linchpin eating disorder behavior further or another eating disorder symptom; write a letter to their eating disorder expressing the problems it causes, how much they resent it, and their wish to end the behavior).
Session 7
participants read their grievance letter to their eating disorder, discuss their second eating disorder behavior challenge home exercise, discuss the interpersonal costs of their eating disorder, dissuade facilitators out of engaging in disordered eating behaviors in role-plays, discuss why it is helpful to speak out against disordered eating behaviors, and are assigned home exercises (reduce their linchpin eating disorder behavior further or another symptom; describe things they would rather do than obsess about their body and eating).
Session 8
participants discuss more valuable uses of their time than obsessing about their body/eating and are encouraged to engage in pleasant activities, discuss their third eating disorder behavior challenge home exercise, discuss the benefits of completing this intervention, and are assigned exit home exercises (make a pact to engage in a self-affirmation activity; generate strategies to maintain the gains they have made [e.g., write themselves a letter about the importance of continuing the healthy changes they made and the costs of reverting back to disordered eating]).
Measures
Thin-ideal internalization
The 6-item Ideal-Body Stereotype Scale-Revised assessed thin-ideal internalization (Stice et al., 2008b) using response options ranging from 1 = strongly disagree to 5 = strongly agree. Items were averaged for this and the other scales. The scale has shown internal consistency (α = .91), 2-week test-retest reliability (r = .80), predictive validity for eating disorder symptom onset, and sensitivity to detecting effects of eating disorder prevention programs (Stice et al., 2008b). Based on prior observations that Cronbach's α was low for the scale (Stice et al., 2013b), the item, Shapely women are more attractive, which is no longer consistent with the other items was dropped, increasing the pretest α from .51 to .64.
Dissonance regarding affirming the thin ideal
We created 10 items for this pilot that assess feelings of cognitive dissonance regarding engaging in behaviors that affirm the thin ideal (e.g., I feel uneasy if I find myself obsessing about aspects of my appearance that don't conform to the thin ideal), including several reverse worded items (e.g., “I feel better about myself if I challenge my friends not to pursue the thin ideal for women glorified in the media), using response options ranging from 1 = “strongly agree” to 5 =“strongly disagree”. In the present trial this scale showed internal consistency (α = .75), 8-week test-retest reliability in controls (r = .61), and sensitivity to detecting intervention effects (see results).
Body dissatisfaction
The Satisfaction and Dissatisfaction with Body Parts Scale (Berscheid, Walster, & Bohrnstedt, 1973) assessed body dissatisfaction using response options ranging from 1 = extremely satisfied to 5 = extremely dissatisfied. It has exhibited internal consistency (α = .94), 3-week test-retest reliability (r = .90), predictive validity for bulimic symptom onset, and sensitivity to intervention effects (Stice et al., 2008b); α = .77 at pretest.
Negative affect
The 21-item Beck Depression Inventory (Beck, Steer, & Carbin, 1988) assessed negative affect on a scale with response options ranging from 0 = no symptoms present to 3 = severe symptoms. It has shown internal consistency (α = .73 to .95), test-retest reliability (r = .60 to .90), and convergent validity with both clinician ratings of depressive symptoms (M r = .75; Beck et al., 1988) and other self-report measures of negative affect (r = .56 to .58; Watson, Clark, & Tellegen, 1988); α = .92 at pretest.
Eating disorder symptoms
The semi-structured Eating Disorder Diagnostic Interview (EDDI; Stice et al., 2006), which was originally adapted from the Eating Disorder Examination (EDE; Fairburn & Cooper, 1993) by inquiring about symptoms over a longer period than just the past month and by retaining only the diagnostic items, assessed eating disorder symptoms and eating disorders. This interview assesses whether participants endorsed each eating disorder symptom on a month-by-month basis and the frequency of symptoms for the past 3 months at pretest and since the last interview for subsequent assessments. Data from this interview were used to confirm inclusion criteria and served as the primary outcome. For inclusion, participants had to meet criteria for a DSM-V eating disorder on the baseline interview, which included Eating and Feeding Disorders Not Elsewhere Classified (see Stice et al., 2013c for definitions). We also calculated a continuous eating disorder symptom composite, which reflected symptoms in the past month (frequency of binge eating, vomiting, laxative/diuretic use, fasting, and excessive exercise, as well as distress about binge eating, endorsement of key features of binge eating [e.g., rapid eating, feeling disgusted, depressed or guilty about binge eating], overvaluation of weight/shape, fear of weight gain/becoming fat, and less than 85% of expected weight). This composite has shown internal consistency (α = .92), inter-rater agreement (ICC r = .93), 1-week test-retest reliability (ICC r = .95), sensitivity to detecting prevention and treatment intervention effects, and predictive validity for future onset of depression (Burton & Stice, 2006; Stice et al., 2008b; Stice, Rohde, Gau, & Shaw, 2009); α = .61 at pretest.
Functional impairment
Functional impairment with family members, peers, and at school and work was assessed with items from the Social Adjustment Scale (Weissman & Bothwell, 1976) using response options ranging from 1= never to 5 = very often. The original scale demonstrated validity with clinician and collateral ratings (M r = .72), discriminant validity, and treatment sensitivity (Weissman & Bothwell, 1976). The adapted items, which were the items most relevant to young women, have shown internal consistency (α = .77), 1-week test-retest reliability (r = .83), and sensitivity to detecting effects of prevention programs (Stice et al., 2006; Stice et al., 2008b); α = .74 at pretest.
Ancillary Treatment
Participants were coded as having received ancillary treatment if they had spoken to a primary care doctor or other physician, a psychiatrist, a nurse, a therapist, psychologist, or other counselor, or a support group about a mental health problem, a weight problem, an eating disorder or body image concern, a physical health problem, injury or illness, or another personal problem. Ancillary treatment was assessed over the past year at pretest, and since the last assessment at posttest and 2-month follow-up.
Statistical Methods
Preliminary analyses
We examined the distribution of outcomes and, in the event of skewed or kurtotic distributions, applied normalizing transformations to reduce the potential for disproportionate influence of outliers and to decrease residual heterogeneity. We evaluated potential sources of non-independence from intervention groups and study sites by fitting separate 3-level models in which intercept coefficients were random to account for non-independence across groups and sites. The group effect was evaluated using a partially clustered design (Baldwin, Bauer, Stice, & Rohde, 2011) that accounts for group variability where participants in one condition are in clusters (i.e., therapy groups) and participants in the other condition are not (i.e., the controls) by fitting the intervention effect as random on therapy groups, reflecting the fact that only intervention participants exhibited clustered effects. The 3-level model examining site variability nested participants within sites in a standard multilevel structure. Level-3 variance was assessed using a deviance test that compared models with and without level-3 variance; if the deviance test indicated that there was not a difference between models with and without level-3 variance, the variance component was not included in subsequent models. Comparisons between intervention and control cases were made for pretest values of the outcomes and demographics (race, ethnicity, age, year in school, parental education) to assess whether randomization created equivalent groups; any significant pretest differences were included as covariates in subsequent analyses.
Model building
Linear mixed effects models assessed treatment effects. These models accommodate multilevel data structures and unequal numbers of observations across participants (Raudenbush & Bryk, 2002). Models were constructed following longitudinal model-building suggestions from Singer and Willett (2003) in which multiple unconditional growth models are evaluated. We examined an unconditional means model (i.e., no longitudinal change), a linear model, and an elevation change model assessed elevation change (i.e., mean difference) between pretest and follow-up time points (posttest [2 months later] and 2-month follow-up), hereafter referred to as the pre versus follow-up model. Longitudinal change in this model is dummy coded (pretest = 0, 2- and 4-month time points = 1), serving to contrast pretest values with the average across follow-up time points. Models were compared using the Akaike Information Criterion (AIC) to assess the best longitudinal model. Next, level-2 predictors and cross-level interactions were added to the model.
We first fit a multivariate multilevel model using SAS PROC MIXED that included thin-ideal internalization, dissonance regarding the thin ideal, body dissatisfaction, negative affect, eating disorder symptoms, and functional impairment as outcomes. The multivariate model was fit as a no intercept model with outcome variables represented by dummy coded vectors using standardized values of the outcomes following recommendations from Baldwin, Imel, Braithwaite, and Atkins (2014). The outcome dummy-coded vectors essentially serve as outcome specific intercepts for the individual dependent variables in the model and effects for independent variables are constructed as interactions with the dummy-coded vectors. Interactions were constructed between each outcome dummy-coded vector and pretest ancillary treatment, time, condition (Body Acceptance Therapy condition = 1), and the time x condition interaction in the full model. In addition, an interaction between the pretest measure of each outcome and the respective outcome dummy-coded vector was included. The multivariate time x condition interaction was assessed by fitting models with and without the time x condition interactions and comparing models using a likelihood ratio test.
After establishing that there was a multivariate time x condition interaction reflecting treatment effects, we fit additional models to test whether the refinements in the engagement procedures implemented during this pilot study resulted in larger intervention effects: the first included all control participants and participants who completed the intervention before the engagement refinements and the second model included all control participants and participants who completed the intervention after the engagement refinements. We also fit models for intervention participants to test whether effects were stronger for those who had higher session attendance and homework completion. These models were identical to the multivariate multilevel model described initially, with the exception that a putative engagement variable was used in place of the condition variable. Effect sizes for models that contained control and intervention participants were derived by dividing the difference between the estimated means of control and intervention groups at the end of study using univariate models constructed using the same model-building sequence as described above. Dividing group differences divided by the baseline standard deviation produces an effect size for growth models that is equivalent to Cohen's d (Feingold, 2009). For the multivariate engagement model effects (e.g., attendance), effect sizes were estimated for high and low levels of engagement by conducting a median split on a putative engagement variable and fitting a univariate model for half of the split data, then converting t values for the time parameter (i.e., within subject change in the intervention condition) to an r equivalent (Lipsey & Wilson, 2001).
Model assessment
Modeling incomplete data using maximum likelihood-based methods requires that data are missing at random (MAR), which has the following requirements: missing data are confined to the outcome, the MAR assumption is viable, variables in the MAR mechanism are included in the model, and the model is correctly specified (van Buuren, 2011). All participants had complete baseline data and all person-level data were included in the model (e.g., intervention condition), confining missing data to outcomes. We assessed possible not missing at random (NMAR) mechanisms by fitting pattern-mixture models in which a dummy variable indicating dropout was included in a model as a main effect and as an interaction with each model parameter (Hedeker & Gibbons, 2006); significant dropout effects indicate a NMAR pattern and, in that event, the dropout parameters are thus retained. Models were deemed correctly specified as they were constructed adhering to model-building recommendations after an assessment of the possible threats to the MAR assumption. Model residuals were assessed using graphical techniques recommend by Baayen (2008), which included residual density plots, QQ plots, and predicted by residual scatterplots. After model building, the influence of outliers was assessed by using Cook's distance for each participant with the requirement that values were less than the 50th percentile of the F distribution (Kutner, Nachtsheim, Neter, & Li, 2005).
Results
Participants in Body Acceptance Therapy groups attended a mean of 4.5 (SD = 3.1) sessions. Seven (16%) attended all 8 sessions, 21 (49%) attended 5 to 7 sessions, 6 (14%) attended 1 to 4 sessions, and 9 (21%) did not attend any sessions. It should be noted that no participant attended only sessions 1-4, which were similar in content to the Body Project. Participants attended a mean of 0.6 (SD = .95) make-up sessions. Sixteen attended at least 1 make-up session. Participants completed an average of 57% of the home exercises. There were 60 (83%) participants who were assessed at post and 56 (78%) who provided data at 2-month follow-up.
Distributions of the dependent variables approximated normality, with the exceptions of negative affect and eating disorder symptoms, which were normalized with natural log transformations. Participants in the intervention and control conditions did not differ significantly on demographics, pretest values of the outcomes, or ancillary treatment at any assessment (intervention and control participants respectively reported ancillary treatment during the intervention period [40% vs. 38%] and over the 2-month follow-up [52% vs. 64%]). During the 4-month study period, the most common presenting problem reported by participants was mental health problems (45%), personal problems (25%) body image concerns (25%), and weight problems (24%). Means and SDs for outcomes for each condition at each time point are presented in Table 1. There was not significant variability in the intercept coefficient attributable to either group or site. Thus, all models were fit as two-level models. The assessment of time in the multivariate models indicated that the pre versus follow-up time model had the best fit.
Table 1.
Means and standard deviations for outcomes by condition at pretest, 2-month posttest, and 4-month posttest
| Variable | Pretest | Posttest | 2-month posttest |
|---|---|---|---|
| Thin-ideal internalization | |||
| Control | 4.25(0.56) | 4.06(0.71) | 4.27(0.49) |
| Body Project | 4.27(0.50) | 3.70(0.50) | 3.81(0.48) |
| Dissonance about affirming thin ideal | |||
| Control | 2.45(0.66) | 2.46(0.78) | 2.57(0.55) |
| Body Acceptance Therapy | 2.40(0.61) | 1.96(0.59) | 1.99(0.64) |
| Body dissatisfaction | |||
| Control | 3.96(0.58) | 3.73(0.75) | 3.66(0.80) |
| Body Acceptance Therapy | 4.09(0.42) | 3.22(0.72) | 3.25(0.70) |
| Negative affect | |||
| Control | 24.48(12.50) | 17.27(13.69) | 16.17(12.28) |
| Body Acceptance Therapy | 24.51(10.69) | 14.39(12.49) | 14.09(11.69) |
| Eating disorder symptoms | |||
| Control | 48.07(18.10) | 30.67(19.66) | 24.43(24.96) |
| Body Acceptance Therapy | 48.67(20.94) | 22.52(12.56) | 17.29(11.40) |
| Functional Impairment | |||
| Control | 2.72(0.53) | 2.37(0.69) | 2.24(0.67) |
| Body Acceptance Therapy | 2.62(0.47) | 2.29(0.54) | 2.18(0.41) |
The comparison between intent-to-treat multivariate models with and without time x condition interactions indicated that Body Acceptance Therapy participants showed greater reductions in outcomes over follow-up than usual care controls (χ2[6] = 34.1, p < .001). As shown on the left side of Table 2, there were large effects for thin-ideal internalization (d = 0.79), body dissatisfaction (d = 1.14), and eating disorder symptoms (d = .95), medium effects for dissonance regarding perpetuating the thin ideal (d = .65) and negative affect (d = .55), and a very small effect for functional impairment (d = .04). We confirmed that symptoms decreased for each eating disorder category represented in the sample, but we were not powered to conduct separate analyses for each category. The assessment of missing-not-at-random indicated that dropouts did not consistently differ from non-dropouts. There were five dropout parameters in each model (dropout main effect, time x dropout, condition x dropout, baseline measure of the outcome x dropout, and time x condition x dropout) for each of the seven outcomes that we evaluated. Across these parameters, there were no significant effects. Thus, finding no evidence to reject the MAR assumption, we did not implement pattern-mixture models. There were no outliers that exceeded the cutoff criterion. Assessment of model residual density plots, QQ plots, and predicted by residual scatterplots did not indicate any violations of the normality of residuals.
Table 2.
Control v intervention effect sizes for full sample, original script, and revised script
| Outcome | All Participants | Original Script | Revised Script |
|---|---|---|---|
| Thin-ideal internalization | 0.79 | 0.70 | 1.00 |
| Dissonance about affirming thin ideal | 0.65 | 0.61 | 0.77 |
| Body dissatisfaction | 1.14 | 0.99 | 1.31 |
| Negative affect | 0.55 | 0.40 | 0.88 |
| Eating disorder symptoms | 0.95 | 0.51 | 2.30 |
| Functional Impairment | 0.04 | -0.03 | 0.23 |
We then estimated models to test whether the effect sizes increased after the engagement procedures were refined. Results indicated that Body Acceptance Therapy versus usual care participants showed greater reductions in outcomes in the multivariate multilevel model both before (χ2[6] = 27.7, p < .001) and after the engagement refinement (χ2[6] = 34.5, p < .001). Effect sizes presented on the right side of Table 2 indicate that the effect sizes consistently increased after engagement refinement.
Next, we estimated models with only participants in the Body Acceptance Therapy condition to test whether effect sizes were larger for participants who attended more sessions and completed more home exercises. Both the time x attendance interaction (χ2[6] = 22.4, p < .001) and time x homework interaction (χ2[6] = 16.6, p = .011) were significant, indicating that effect sizes were larger for participants who attended more sessions and completed more home exercises. Within-condition effect sizes were larger for participants above (M r = .71, range .54 - .79) versus below (M r = .45, range .15 - .63) the median of session attendance. Likewise, within-condition effect sizes were larger for participants above (M r = .66, range .46 - .77) versus below (M r = .56, range .38 - .75) the median home exercise completion rate.
Given that many individuals with eating disorders are reluctant to engage in treatment, it is important to consider the acceptability of this new dissonance-based eating disorder treatment. At a behavioral level, among those that attended the first session, 25 out of 30 (83%) attended more than 50% of the sessions, suggesting good acceptability. Qualitative data from participants revealed several themes. First, among high attenders (those attending more than half of the sessions), the most positive aspect of the group (mentioned by 70%) was sharing with other women who had similar concerns, followed by having accountability for change (mentioned by 20%). Second, among high, low, and non-attenders, the most common reason for non-attendance (mentioned by 50% from each group) was embarrassment, followed by the intervention being too time-consuming (mentioned by 20%). Third, women with low attendance often attributed their non-attendance to parking problems and the broad age range of the group. Fourth, women who failed to attend a single session stated that they did not want to meet others who had the same problem, they were already in individual therapy, they wanted a group that focused on just one type of eating disorder, or they wanted an educational rather than psychotherapeutic intervention. Fifth, the most frequent suggestion for improving recruitment and initial attendance was to provide more information (especially video testimonials from actual clients) about what the intervention entailed. Lastly, suggestions for improving retention included adding an initial “icebreaker” activity, directly acknowledging the issue of stigma, and more clearly differentiating the person from her disorder (“you are not your diagnosis”).
Discussion
Participants in the new dissonance-based group eating disorder treatment showed greater reductions in thin-ideal internalization, dissonance regarding affirming the thin ideal, body dissatisfaction, negative affect, and eating disorder symptoms over the 4-month study period relative to those receiving usual care. Rates and type of ancillary treatment over follow-up were similar across conditions, suggesting that differential care should not have biased estimates of intervention effects. The eating disorder symptom reduction effect (d = .95), which was large in magnitude, was similar to effects produced by the individual treatments of choice for various eating disorders relative to usual care controls (M d = .79; Dare et al., 2001; Grilo et al., 2005; Kirkley et al., 1985; Peterson et al., 2009; Spielmans et al., 2013) and for enhanced CBT for women with binge spectrum EDs (d = .98; Fairburn et al. 2009, though threshold/subthreshold anorexia nervosa cases were excluded from the latter trial). The similarity in effects is noteworthy because Body Acceptance Therapy is more cost-effective than the typical 20-session individual treatment; one clinician can treat 8 individuals in 8 hours of group therapy, versus 160 hours required for individual therapy with 8 patients (8 patients x 20 hours). Thus, individuals can be treated for 1/20th the number of therapist hours (8/160 = .05). Similar calculations show that patients can be treated with Body Acceptance Therapy for 1/5th the therapist time necessary for guided bibliotherapy.
The retention rate (78% after adjusting for initial no-shows) is comparable to average attendance rates for the individual treatments for eating disorders (77%; Dare et al., 2001; Grilo et al., 2005; Kirkley et al., 1985; Peterson et al., 2009). Our 78% retention rate was higher than the 67% retention rate from the Fairburn and associates (2009) trial and the 50% retention rate from an uncontrolled study of enhanced CBT (Byrne et al., 2011). Although these data imply that the acceptability of this new group treatment might be superior to enhanced CBT, which appears to be the only other treatment designed for a range of eating disorders, attendance was suboptimal. We therefore made improvements to engagement (e.g., asking facilitators to call each participant before the group to discuss what to expect and any concerns, encourage participants to read testimonials about the treatment from prior participants, told participants that those who attend the most sessions and do the most home exercises show the greatest benefit, more clearly described the rational or the home exercises) midway through this preliminary trial. Although these refinements had only trivial effects on attendance of the initial session and retention, they were associated with an increase in effect sizes (M d for outcomes increased from .53 to 1.08). Perhaps most noteworthy, the effect size for eating disorder symptom reduction increased from .51 to 2.30.
The evidence that participants who attended more sessions and completed more home exercises showed significantly larger reductions in outcomes, imply that one way to increase the efficacy of this treatment would be to improve retention and home exercise completion. Towards this end, we made several additional refinements to the engagement procedures and intervention script. First, we added dissonance-based motivational enhancement questions to the phone script for the initial engagement call that facilitators make before the first session. Specifically, we ask the participant to describe health, interpersonal, and financial costs of their eating disordered behavior to increase their desire for reducing their eating disordered behaviors. Second, as suggested by the qualitative feedback, we are creating video testimonials regarding the benefits of completing this new group-based eating disorder treatment from women who have gone through the intervention. Third, also as suggested by the qualitative feedback, we added a fun icebreaker exercise to the first session, as well as an engaging playful activity and a complement activity, with the hope of improving retention. Fourth, we now acknowledge the strong stigma associated with eating disorders and underscore that their eating disorder does not define the person, as recommended in the qualitative feedback.
It is important to consider the limitations of this study when interpreting the findings. First, because usual care was not standardized across sites, it is difficult to understand the precise nature of the treatment the control participants typically received, though data suggested that treatment often focused on more general mental health/personal problems rather than body image concerns or weight problems. Also, usual care consisted almost entirely of individual therapy and never consisted of a manualized group approach. Arguably this approach to capturing usual care has ecological validity, but future efficacy trials should consider using a standardized control treatment, such as educational support groups that each university offered to students with eating disorders (though they differ across universities) to match conditions on the amount, duration, and format of care. Second, we were not able to conduct longer-term follow-up in this preliminary trial, which precluded estimating the effects of this new treatment on eating disorder remission. Third, the moderate sized sample attenuated power to detect small effects. Fourth, all of the data were based on self-report, which might have artificially increased the apparent intervention effects due to demand characteristics.
In conclusion, Body Acceptance Therapy, a new dissonance-based eating disorder treatment, produced reductions in eating disorder symptoms that are on par with those produced by more intensive individual and family treatments for individual eating disorders. These preliminary findings are encouraging given that this group intervention requires approximately 1/20th the therapist time necessary for extant treatments of choice for various eating disorders. We hope that with continued refinement to engagement and retention procedures and to the intervention content we may be able to produce an even more efficacious front-line group treatment for the range of eating disorders that could be broadly disseminated, addressing a key barrier in the eating disorder treatment field.
Highlights.
Pilot tested a new dissonance-based group eating disorder treatment
Randomized 128 women with eating disorder to Body Acceptance Therapy or usual care
Intervention reduced all outcomes (M d = .53) through 2-month follow-up
Higher attendance and homework completion predicted stronger effects
Results are very encouraging given cost-effectiveness of this group treatment
Table 3.
Time X Body Acceptance Therapy interactions and effect sizes
| Outcome | B | SE | df | t | p | d |
|---|---|---|---|---|---|---|
| Thin-ideal internalization | −0.36 | 0.08 | 209 | −4.42 | <001 | 0.69 |
| Dissonance regarding the thin ideal | −0.42 | 0.09 | 208 | −4.45 | <.001 | 0.68 |
| Body dissatisfaction | −0.39 | 0.09 | 209 | −4.28 | <.001 | 0.71 |
| Dieting | −0.30 | 0.12 | 207 | −2.48 | .014 | 0.40 |
| Negative affect | −0.31 | 0.11 | 209 | −2.72 | .007 | 0.45 |
| Eating disorder symptoms | −0.15 | 0.07 | 211 | −2.15 | .032 | 0.49 |
| Functional impairment | −0.17 | 0.08 | 209 | −2.17 | .031 | 0.27 |
Table 4.
Time X attendance and time X homework interaction effects and effect sizes
| Outcome | B | SE | Df | t | p | d |
|---|---|---|---|---|---|---|
| Time X attendance | ||||||
| Thin-ideal internalization | −0.04 | 0.02 | 104 | −1.71 | .091 | 0.34 |
| Dissonance regarding the thin ideal | −0.02 | 0.02 | 103 | −0.92 | .360 | 0.18 |
| Body dissatisfaction | −0.10 | 0.03 | 104 | −4.04 | <.001 | 0.79 |
| Dieting | −0.01 | 0.03 | 103 | −0.15 | .883 | 0.03 |
| Negative affect | −0.08 | 0.03 | 104 | −2.39 | .019 | 0.47 |
| Eating disorder symptoms | −0.04 | 0.02 | 103 | −1.78 | .079 | 0.35 |
| Functional impairment | −0.06 | 0.02 | 104 | −2.78 | .006 | 0.55 |
| Time X homework | ||||||
| Thin-ideal internalization | −0.20 | 0.15 | 104 | −1.31 | .192 | 0.26 |
| Dissonance regarding the thin ideal | −0.31 | 0.17 | 103 | −1.86 | .066 | 0.37 |
| Body dissatisfaction | −0.63 | 0.18 | 104 | −3.51 | <.001 | 0.69 |
| Dieting | −0.02 | 0.24 | 103 | −0.08 | .935 | 0.02 |
| Negative affect | −0.69 | 0.21 | 104 | −3.28 | .001 | 0.64 |
| Eating disorder symptoms | −0.25 | 0.15 | 103 | −1.70 | .092 | 0.34 |
| Functional impairment | −0.28 | 0.14 | 104 | −1.95 | .054 | 0.38 |
Acknowledgments
This study was supported by grant (DK072932) from the National Institutes of Health. We thank project research assistants Maartje Mulders and Madeline Kirch.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Eric Stice, Oregon Research Institute.
Paul Rohde, Oregon Research Institute.
Meghan Butryn, Drexel University.
Katharine S. Menke, University of Texas at Austin
C. Nathan Marti, University of Texas at Austin.
References
- Allen K, Byrne S, Oddy W, Crosby R. DSM-IV-TR and DSM-5 eating disorders in adolescents; Prevalence, stability, and psychosocial correlates in a population-based sample of male and female adolescents. Journal of Abnormal Psychology. 2013;122:720–732. doi: 10.1037/a0034004. [DOI] [PubMed] [Google Scholar]
- Arcelus J, Mitchell A, Wales J, Nielsen S. Mortality rates in patients with anorexia nervosa and other eating disorders: A meta-analysis of 36 studies. Archives of General Psychiatry. 2011;68:724–31. doi: 10.1001/archgenpsychiatry.2011.74. [DOI] [PubMed] [Google Scholar]
- Baayen RH. Analyzing Linguistic Data. Cambridge University Press; New York, NY: 2008. [Google Scholar]
- Baldwin S, Bauer D, Stice E, Rohde P. Evaluating models for partially clustered designs. Psychological Methods. 2011;16:149–165. doi: 10.1037/a0023464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baldwin S, Imel Z, Braithwaite S, Atkins D. Analyzing multiple outcomes in clinical research using multivariate multilevel models. Journal of Consulting and Clinical Psychology. 2014;82:920–930. doi: 10.1037/a0035628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bardone-Cone A, Harney M, Maldonado C, Lawson M, Robinson D, Smith R, Tosh A. Defining recovery from an eating disorder: Conceptualization, validation, and examination of psychosocial functioning and psychiatric comorbidity. Behaviour Research & Therapy. 2010;48:194–202. doi: 10.1016/j.brat.2009.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beato-Fernandez L, Rodriguez-Cano T, Belmonte-Llario A, Martinez-Delgado C. Risk factors for eating disorders in adolescents: A Spanish community-based longitudinal study. European Child and Adolescent Psychiatry. 2004;13:287–294. doi: 10.1007/s00787-004-0407-x. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Carbin MG. Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clinical Psychology Review. 1988;8:77–100. [Google Scholar]
- Becker CB, Smith LM, Ciao AC. Reducing eating disorder risk factors in sorority members: A randomized trial. Behavior Therapy. 2005;36:245–253. [Google Scholar]
- Berscheid E, Walster E, Bohrnstedt G. The happy American body: A survey report. Psychology Today. 1973;7:119–131. [Google Scholar]
- Bohon C, Stice E, Spoor S. Female emotional eaters show abnormalities in consummatory and anticipatory food reward: A functional magnetic resonance imaging study. International Journal Of Eating Disorders. 2009;42(3):210–221. doi: 10.1002/eat.20615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burton E, Stice E. Evaluation of a healthy-weight treatment program for bulimia nervosa: A preliminary randomized trial. Behaviour Research and Therapy. 2006;44:1727–1738. doi: 10.1016/j.brat.2005.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crow S, Peterson C, Swanson S, Raymond N, Specker S, Eckert E, Mitchell J. Increased mortality in bulimia nervosa and other eating disorders. American Journal of Psychiatry. 2009;166:1342–1346. doi: 10.1176/appi.ajp.2009.09020247. [DOI] [PubMed] [Google Scholar]
- Dare C, Eisler I, Russell G, Treasure J, Dodge L. Psychological therapies for adults with anorexia nervosa: Randomised controlled trial of outpatient treatments. British Journal of Psychiatry. 2001;178:216–221. doi: 10.1192/bjp.178.3.216. [DOI] [PubMed] [Google Scholar]
- Eddy K, Celio Doyle A, Hoste R, Herzog D, le Grange D. Eating disorder not otherwise specified in adolescents. Journal of the American Academy of Child and Adolescent Psychiatry. 2008;47:156–64. doi: 10.1097/chi.0b013e31815cd9cf. [DOI] [PubMed] [Google Scholar]
- Fairburn C, Bohn K. Eating disorder NOS (EDNOS): an example of the troublesome “not otherwise specified” (NOS) category in DSM-IV. Behaviour Research and Therapy. 2005;43:691–701. doi: 10.1016/j.brat.2004.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairburn C, Cooper Z. The eating disorder examination (12th ed.). In: Fairburn C, Wilson G, editors. Binge eating: Nature, assessment, and treatment. Guilford; NY: pp. 317–360. [Google Scholar]
- Fairburn C, Cooper Z, Doll H, O'Connor M, Bohn K, Hawker D, Palmer RL. Transdiagnostic Cognitive-Behavioral Therapy for Patients With Eating Disorders: A Two-Site Trial With 60-Week Follow-Up. American Journal of Psychiatry. 2009;166:311–319. doi: 10.1176/appi.ajp.2008.08040608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairburn C, Stice E, Cooper Z, Doll H, Norman P, O'Connor M. Understanding persistence of bulimia nervosa: A five-year naturalistic study. Journal of Consulting and Clinical Psychology. 2003;71:103–109. [PubMed] [Google Scholar]
- Feingold A. Effect sizes for growth-modeling analysis for controlled clinical trials in the same metric as for classical analysis. Psychological Methods. 2009;14:43–53. doi: 10.1037/a0014699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green M, Scott N, Diyankova I, Gasser C, Pederson E. Eating disorder prevention: An experimental comparison of high level dissonance, low level dissonance, and no-treatment control. Eating Disorders. 2005;13:157–169. doi: 10.1080/10640260590918955. [DOI] [PubMed] [Google Scholar]
- Grilo C, Masheb R. Correlates of body image dissatisfaction in treatment-seeking men and women with binge eating disorder. International Journal Of Eating Disorders. 2005;38:162–166. doi: 10.1002/eat.20162. [DOI] [PubMed] [Google Scholar]
- Grilo C, Masheb R, Wilson G. Efficacy of cognitive behavioral therapy and fluoxetine for the treatment of binge eating disorder: A randomized double-blind placebo-controlled comparison. Biological Psychiatry. 2005;57:301–309. doi: 10.1016/j.biopsych.2004.11.002. [DOI] [PubMed] [Google Scholar]
- Halliwell E, Diedrichs P. Testing a Dissonance Body Image Intervention Among Young Girls. Health Psychology. 2013;33:201–204. doi: 10.1037/a0032585. [DOI] [PubMed] [Google Scholar]
- Hedeker D, Gibbons R. Longitudinal data analysis. Wiley; New York, NY: 2006. [Google Scholar]
- Jones M, Luce K, Osborne M, Taylor K, Cunning D, Doyle A, et al. Randomized, controlled trial of an Internet-facilitated intervention for reducing binge eating and overweight in adolescents. Pediatrics. 2008;121:453–462. doi: 10.1542/peds.2007-1173. [DOI] [PubMed] [Google Scholar]
- Kirkley B, Schneider J, Agras W, Bachman J. Comparison of two group treatments for bulimia. Journal Of Consulting And Clinical Psychology. 1985;53:43–48. doi: 10.1037//0022-006x.53.1.43. [DOI] [PubMed] [Google Scholar]
- Kutner M, Nachtsheim C, Neter J, Li W. Applied linear statistical models. McGraw-Hill; New York, NY: 2005. [Google Scholar]
- le Grange D, Binford RB, Peterson CB, Crow SJ, Crosby RD, Klein M,H, et al. DSM-IV threshold versus subthreshold bulimia nervosa. International Journal of Eating Disorder. 2006;39:462–467. doi: 10.1002/eat.20304. [DOI] [PubMed] [Google Scholar]
- Lilienfeld S, Ritschel L, Lynn S, Brown A, Cautin R, Latzman R. The research-practice Gap: Bridging the schism between eating disorder researchers and practitioners. International Journal Of Eating Disorders. 2013;46:386–394. doi: 10.1002/eat.22090. [DOI] [PubMed] [Google Scholar]
- Lipsey M, Wilson D. Practical meta-analysis. Sage; Thousand Oaks, CA: 2001. [Google Scholar]
- Matusek J, Wendt S, Wiseman C. Dissonance thin-ideal and didactic healthy behavior eating disorder prevention programs: Results from a controlled trial. International Journal of Eating Disorders. 2004;36:376–388. doi: 10.1002/eat.20059. [DOI] [PubMed] [Google Scholar]
- McKnight I. Risk factors for the onset of eating disorders in adolescent girls: Results of the McKnight longitudinal risk factor study. The American Journal of Psychiatry. 2003;160:248–254. doi: 10.1176/ajp.160.2.248. [DOI] [PubMed] [Google Scholar]
- McMillan W, Stice E, Rohde P. High- and low-level dissonance-based eating disorder prevention programs with young women with body image concerns: An experimental trial. Journal of Consulting and Clinical Psychology. 2011;79:129–134. doi: 10.1037/a0022143. [DOI] [PubMed] [Google Scholar]
- McVey G, Tweed S, Blackmore E. Healthy schools-healthy kids: A controlled evaluation of a comprehensive eating disorder prevention program. Body Image. 2007;4:115–136. doi: 10.1016/j.bodyim.2007.01.004. [DOI] [PubMed] [Google Scholar]
- Mitchell J, Agras S, Crow S, Halmi K, Fairburn C, Bryson S, et al. Stepped care and cognitive-behavioural therapy for bulimia nervosa: Randomised trial. British Journal of Psychiatry. 2011;198:391–7. doi: 10.1192/bjp.bp.110.082172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell K, Mazzeo S, Rausch S, Cooke K. Innovative interventions for disordered eating: Evaluating dissonance-based and yoga interventions. International Journal of Eating Disorders. 2007;40:120–128. doi: 10.1002/eat.20282. [DOI] [PubMed] [Google Scholar]
- Müller S, Stice E. Moderators of the intervention effects for a dissonance-based eating disorder prevention program; results from an amalgam of three randomized trials. Behaviour Research And Therapy. 2013;51:128–133. doi: 10.1016/j.brat.2012.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peterson C, Mitchell J, Crow S, Crosby R, Wonderlich S. The efficacy of self-help group treatment and therapist-led group treatment for binge eating disorder. The American Journal of Psychiatry. 2009;166:1347–1354. doi: 10.1176/appi.ajp.2009.09030345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raudenbush SW, Bryk AS. Advanced quantitative techniques in the social sciences. 2nd ed. SAGE; Thousand Oaks, CA: 2002. Hierarchical linear models: Applications and data analysis methods: Vol. 1. [Google Scholar]
- Schmidt U, Lee S, Beecham J, et al. A randomized control trial of family therapy and cognitive behavior therapy guided self-care for adolescents with bulimia nervosa and related disorders. American Journal of Psychiatry. 2007;164:591–598. doi: 10.1176/ajp.2007.164.4.591. [DOI] [PubMed] [Google Scholar]
- Seidel A, Presnell K, Rosenfield D. Mediators in the dissonance eating disorder prevention program. Behaviour Research and Therapy. 2009;47:645–653. doi: 10.1016/j.brat.2009.04.007. [DOI] [PubMed] [Google Scholar]
- Singer J, Willett J. Applied longitudinal data analysis: Modeling change and event occurrence. Oxford University Press; New York, NY: 2003. [Google Scholar]
- Spielmans G, Benish S, Marin C, Bowman W, Menster M, Wheeler A. Specificity of psychological treatments for bulimia nervosa and binge eating disorder? A meta-analysis of direct comparisons. Clinical Psychology Review. 2013;33:460–469. doi: 10.1016/j.cpr.2013.01.008. [DOI] [PubMed] [Google Scholar]
- Steele A, Wade T. A randomized trial investigating guided self-help to reduce perfectionism and its impact on bulimia nervosa: A pilot study. Behaviour Research and Therapy. 2008;26:1316–1323. doi: 10.1016/j.brat.2008.09.006. [DOI] [PubMed] [Google Scholar]
- Stice E, Agras WS. Predicting onset and cessation of bulimic behaviors during adolescence: A longitudinal grouping analysis. Behavior Therapy. 1998;29:257–276. [Google Scholar]
- Stice E, Becker C, Yokum S. Eating disorder prevention: Current evidence-base and future directions. International Journal of Eating Disorders. 2013a;46:478–485. doi: 10.1002/eat.22105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Butryn M, Rohde P, Shaw H, Marti N. An effectiveness trial of a new enhanced dissonance eating disorder prevention program among female college students. Behaviour Research and Therapy. 2013b;51:862–871. doi: 10.1016/j.brat.2013.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Marti N, Durant S. Risk factors for onset of eating disorders: Evidence of multiple risk pathways from an 8-year prospective study. Behaviour Research and Therapy. 2011;49:622–627. doi: 10.1016/j.brat.2011.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Marti N, Rohde P. Prevalence, incidence, impairment, and course of the proposed DSM-5 eating disorder diagnoses in an 8-year prospective community study of young women. Journal Of Abnormal Psychology. 2013c;122:445–457. doi: 10.1037/a0030679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Marti N, Shaw H, O'Neil K. General and program-specific moderators of two eating disorder prevention programs. International Journal Of Eating Disorders. 2008a;41:611–617. doi: 10.1002/eat.20524. [DOI] [PubMed] [Google Scholar]
- Stice E, Marti N, Spoor S, Presnell K, Shaw H. Dissonance and healthy weight eating disorder prevention programs: Long-term effects from a randomized efficacy trial. Journal of Consulting and Clinical Psychology. 2008b;76:329–340. doi: 10.1037/0022-006X.76.2.329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Presnell K, Gau J, Shaw H. Testing mediators of intervention effects in randomized controlled trials: An evaluation of two eating disorder prevention programs. Journal of Consulting and Clinical Psychology. 2007;75:20–32. doi: 10.1037/0022-006X.75.1.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Rohde P, Gau J, Shaw H. An effectiveness trial of a dissonance-based eating disorder prevention program for high-risk adolescents girls. Journal of Consulting and Clinical Psychology. 2009;77:825–834. doi: 10.1037/a0016132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Rohde P, Gau J, Shaw H. Effect of a Dissonance-Based Prevention Program on Risk for Eating Disorder Onset in the Context of Eating Disorder Risk Factors. Prevention Science. 2012;13:129–139. doi: 10.1007/s11121-011-0251-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Rohde P, Shaw H, Gau J. An effectiveness trial of a selected dissonance-based eating disorder prevention program for female high school students: Long-term effects. Journal of Consulting and Clinical Psychology. 2011;79:500–508. doi: 10.1037/a0024351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Shaw H, Burton E, Wade E. Dissonance and healthy weight eating disorder prevention programs: A randomized efficacy trial. Journal of Consulting and Clinical Psychology. 2006;74:263–275. doi: 10.1037/0022-006X.74.2.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Striegel-Moore RH, Leslie D, Petrill SA, Garvin V, Rosenheck RA. One-year use and cost of inpatient and outpatient services among female and male patients with an eating disorder: Evidence from a national database of health insurance claims. International Journal of Eating Disorders. 2000;27:381–389. doi: 10.1002/(sici)1098-108x(200005)27:4<381::aid-eat2>3.0.co;2-u. [DOI] [PubMed] [Google Scholar]
- Swanson S, Crow S, Le Grange D, Swendsen J, Merikangas K. Prevalence and correlates of eating disorders in adolescents: Results from the National Comorbidity Survey Replication Adolescent Supplement. Archives of General Psychiatry. 2011;68:714–723. doi: 10.1001/archgenpsychiatry.2011.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thiels C, Schmidt U, Treasure J, Garthe R, et al. Guided self-change for bulimia nervosa incorporating use of a self-care manual. American Journal of Psychiatry. 1998;155:947–53. doi: 10.1176/ajp.155.7.947. [DOI] [PubMed] [Google Scholar]
- van Buuren S. Multiple imputation of multilevel data. In: Hox J, Roberts J, editors. Handbook of advanced multilevel analysis. Routledge; New York, NY: 2011. [Google Scholar]
- Walsh B, Fairburn C, Mickley D, Sysko R, Parides M. Treatment of bulimia nervosa in a primary care setting. American Journal of Psychiatry. 2004;161:556–61. doi: 10.1176/appi.ajp.161.3.556. [DOI] [PubMed] [Google Scholar]
- Watson D, Clark L, Tellegen A. Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal Of Personality And Social Psychology. 1988;54:1063–1070. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- Weissman M, Bothwell S. Assessment of social adjustment by patient self-report. Archives of General Psychiatry. 1976;33:1111–1115. doi: 10.1001/archpsyc.1976.01770090101010. [DOI] [PubMed] [Google Scholar]
- Wilson G, Zandberg L. Cognitive–behavioral guided self-help for eating disorders: Effectiveness and scalability. Clinical Psychology Review. 2012;32:343–357. doi: 10.1016/j.cpr.2012.03.001. [DOI] [PubMed] [Google Scholar]
- Wilson G. Cognitive behavioral therapy for eating disorders. In: Agras WS, editor. The Oxford Handbook of Eating Disorders. Oxford University Press; Oxford: 2010. pp. 331–347. [Google Scholar]
- Zandberg L, Wilson G. Train-the-trainer: Implementation of cognitive behavioural guided self-help for recurrent binge eating in a naturalistic setting. European Eating Disorders Review. 2013;21:230–237. doi: 10.1002/erv.2210. [DOI] [PubMed] [Google Scholar]