Abstract
Background
Recent studies have shown that Gaviscon Double Action Liquid (a combination alginate-antacid) administered postprandially co-localizes with the acid pocket, the ‘reservoir’ for postprandial acid reflux.
Aim
This study compared the effectiveness of Gaviscon Double Action Liquid to an equivalent strength antacid without alginate in controlling postprandial acid reflux in GERD patients.
Methods
14 GERD patients undertook two 3.5-hour high-resolution manometry/pH-impedance studies during which they ate a standardized meal. In a double-blinded randomized crossover design they then took Gaviscon or CVS brand antacid, each with ~18 mmol/l acid neutralizing capacity. The primary outcome was distal esophageal acid exposure; secondary outcomes were number of reflux events, proximal extent of reflux, nadir pH of the refluxate, mechanism of reflux, and reflux symptoms scored with a validated instrument.
Results
10 patients completed the study. Gaviscon studies had significantly less distal esophageal acid exposure and greater nadir refluxate pH in the 30–150 minute postprandial period than antacid studies. There were no differences in the number of reflux events (acid or weakly acidic) or the number of proximal reflux events (15–17 cm above the LES) with either study medication.
Conclusions
Gaviscon Double Action Liquid was more effective than an antacid without alginate in controlling postprandial esophageal acid exposure. However, the number and spatial distribution of reflux events within the esophagus were similar. This suggests that Gaviscon main effectiveness related to its co-localization with and displacement/neutralization of the post-prandial acid pocket, rather than preventing reflux.
Keywords: Gastro-esophageal reflux disease, antacid, alginate
INTRODUCTION
Heartburn is a cardinal symptom of gastro-esophageal reflux disease (GERD) and is among the most common patient complaints encountered by Internists and Gastroenterologists. A nationwide telephone survey of 21,000 representative US adults found that 6.3% of respondents experienced heartburn on at least a twice-weekly basis 1. In most instances, heartburn is experienced postprandially. A seeming paradox of postprandial heartburn is that it occurs during the period that one might expect gastric acid to be buffered by the meal. That paradox was partially resolved with the description of the ‘acid pocket’, the phenomenon by which newly secreted gastric acid layers on top of, rather than mixing with, the ingested meal 2, 3. This puts acid in close proximity to the gastro-esophageal junction as soon as 17 minutes after eating 4. Investigations using either technetium labelled acid and scintigraphic monitoring 5 or high-resolution postprandial pH recordings 4 have confirmed that the acid pocket is the source of postprandial acid reflux. Furthermore, the acid pocket tends to localize within a hiatal hernia, when present 5, and to facilitate the migration of acid across the squamocolumnar junction in patients with hernias or GERD 5, 6. Hence, selectively targeting the acid pocket becomes an attractive therapeutic approach for the management of postprandial heartburn.
Consistent with the central role of gastric acid in the genesis of reflux symptoms and mucosal pathology, the inhibition of gastric acid secretion has been the mainstay of the medical management of GERD 7. Proton pump inhibitors (PPIs) are particularly potent and have proven to be extremely effective treatment for esophagitis. Not surprisingly, PPIs have also been shown to both decrease the size of and the acidity within the acid pocket 8, 9. However, PPI therapy has limitations. Many patients have an incomplete symptom response and others, either because of general unease with open-ended pharmacotherapy or because of the intermittent nature of reflux symptoms, prefer to address reflux symptoms with prn medication. The problem has been the limited efficacy of this approach; antacids neutralize gastric acid in a short timeframe after ingestion but the effect is soon overcome by meal-stimulated acid secretion. Alternatively, an alginate-antacid combination creates a ‘raft’ floating on top of the ingested chyme that co-localizes in the region of the acid pocket, potentially offering more effective targeted therapy 10. This study compared the effect of Gaviscon Double Action Liquid (Reckitt Benckiser Healthcare, Hull, UK) to a store-brand antacid in controlling postprandial acid reflux in GERD patients.
METHODS
Study subjects
Typical GERD patients with past or present LA A or B esophagitis and/or abnormal pH monitoring study (>5% distal esophageal acid exposure on Bravo pH monitoring) along with a significant frequency-severity of typical gastroesophageal reflux symptoms gauged by the GerdQ instrument (score ≥8) were recruited from a pool of patients referred to the Northwestern Medical Faculty Foundation (NMFF) Gastroenterology outpatient practice or the gastrointestinal diagnostic laboratory at Northwestern Memorial Hospital from August 2011 to March 2013. Those with prior gastrointestinal surgery, or significant cardiopulmonary, renal, neurologic, or psychiatric disorders were excluded. Study participants were asked to refrain from taking any proton pump inhibitors or H2-receptor antagonists for 7 days prior to their study sessions. Acid neutralizing medications were allowed as needed except for the day of the study. All subjects gave written informed consent and the Northwestern University Institutional Review Board (IRB) approved the study protocol.
Study medications
Gaviscon Double Action Liquid (sodium alginate-bicarbonate) is an oral liquid suspension that belongs in the pharmacotherapeutic group A02BX (other drugs for peptic ulcer and gastro-esophageal reflux disease). Its mode of action is local, not depending on absorption into the circulation. The medication is a combination of two antacids (calcium carbonate and sodium bicarbonate) and sodium alginate. Each 20 ml dose contains 1000 mg sodium alginate, 426 mg sodium bicarbonate, and 650 mg calcium carbonate with an acid neutralizing capacity of approximately 18.1 mmol/l. Antacid Supreme (CVS brand Antacid Liquid Supreme) is an oral liquid suspension that contains calcium carbonate 400 mg and magnesium hydroxide 135 mg in each 5 ml dose. Each 10 ml dose has acid neutralizing capacity of approximately 25.2 mmol/l. The volumes used were 20 ml of Gaviscon Double Action Liquid and 7.5 mL of CVS antacid, each with ~18 mmol/l acid neutralizing capacity.
High-resolution manometry
High-resolution manometry data were obtained using a solid-state assembly (4.2 mm outer diameter) with 36 circumferential sensors spaced at 1-cm intervals (Given Imaging, Duluth, GA), the recording characteristics of which have been described previously 11. Studies were performed after at least a 6-hour fast in a sitting position. Pressure transducers were calibrated at 0 and 300 mmHg using externally applied pressure prior to the study. Pressure topography data were analyzed using Manoview analysis software (Given Imaging, Duluth, GA).
pH-impedance Measurement
After manometric localization of the lower esophageal sphincter (LES), an intraluminal pH-impedance catheter (Sandhill Scientific, Highlands Ranch, CO or Medical Measurement Systems (MMS), Enshede, Netherlands) was positioned trans-nasally into the esophagus such that the esophageal pH sensor was 5 cm above the proximal margin of the LES. Intraluminal impedance was continuously measured from six impedance-recording segments; the middle of each impedance segment was located at 3, 5, 7, 9, 15 and 17 cm above the proximal border of the OGJ as previously determined by HRM. Impedance signals were recorded on a portable digital data logger (Sandhill Scientific or MMS).
Study protocol
The protocol consisted of two 3.5-hour study sessions, at least 4 days apart. The GerdQ instrument was administered to assess symptom severity for the 7 days prior to each session during which time they were taking no acid-suppressive medications. The HRM and pH-impedance catheters were placed and recording begun. Participants then consumed a standardized meal consisting of a McDonald’s double quarter pounder with cheese and small fries (970 kcal) within about 15 minutes. Five minutes after completion of the meal, one of the two medications was administered by syringe into the subject’s mouth, the identity of which was blinded to the patient. The sequence of medication was allocated according to an on-line computerized randomization site (www.randomizer.org). Postprandial pH-impedance and HRM recordings continued for 180 minutes, during which the patients were asked to complete a modified GerdQ each 30 minutes. At the completion of the recording period, both catheters were removed and the subjects were discharged.
Data analysis
The primary outcome of the study was the time that the distal esophageal pH was <4 in the three-hour postprandial period. Secondary outcomes were number of reflux events, acid reflux events, proximal reflux events (15–17 cm proximal to the LES), nadir pH of the refluxate, and postprandial symptoms experienced. Manometric tracings were also analyzed for the mechanism of reflux associated with each reflux event. Criteria used to define transient lower esophageal sphincter relaxations (TLESRs) were adapted from those proposed by Roman et al for pressure topography studies 12 in line with the evolving recommendations of a multicenter expert panel focused on this topic. All studies were reviewed by two investigators (SR and AdR); discrepancies in interpretation were resolved by discussion inclusive of PJK. The investigators were unaware of the medication given.
Statistical analysis
Data were expressed as median and interquartile range (IQR) if nonparametric or mean ± SEM if parametric. The Wilcoxon Rank Sum test and the Kruskal–Wallis test were used to compare differences in non-parametric metrics between groups. A paired t-test was used to compare parametric results. All p-values were two-tailed with the level of significance defined at 0.05. The study was IRB approved to enroll a maximum of 20 subjects based on the objective of detecting a 50% difference in acid exposure time between study conditions and experiencing a high number of anticipated dropouts owing to the rigors of the study.
RESULTS
Ten patients successfully completed both test sessions with good quality recordings. Two subjects completed only one session, declining to participate further, one subject’s recording in one arm of the study was lost after 2 hours of recording, and one subject’s recordings were corrupted and unusable. Table 1 details the demographics and entry characteristics of the completed patients.
Table 1.
Demographics and clinical features of 10 completed patients
| Patient characteristic (n=11) | Value |
|---|---|
| Age in years (SD); gender | 48 (11.6) 5 male |
| Weight in kg (SD) | 90.4 (15.4) |
| Number enrolled based on history of LA A esophagitis | 4 (40%) |
| Number enrolled based on history of LA B esophagitis | 4 (40%) |
| Number enrolled based on abnormal acid exposure on 48-hr pH study | 2 (20%) |
| Mean entry GerdQ score | 9.5 (SD 1.2) |
All patients had typical GERD symptoms, evident by all abnormal GerdQ scores prior to the first study day. Most of them (80%) were enrolled on the basis of having had the recent demonstration of low-grade (LA A or B) esophagitis on a recent endoscopy and the remaining 20% had pathological acid exposure on pH monitoring performed while not taking a PPI.
Postprandial esophageal acid exposure
Evident in Table 2, the primary outcome of the study, distal esophageal acid exposure, was significantly less following Gaviscon compared to antacid.
Table 2.
Postprandial acid exposure and reflux data. Gaviscon Double Action Liquid vs antacid.
| Gaviscon | Antacid | p | |
|---|---|---|---|
| Distal acid exposure: median % [IQR] | 0.7% [0–28.2] | 8.0% [0 – 7.2] | .001 |
| Number of acid reflux events: mean ± SEM | 8.7± 3.0 | 12.4 ± 2.7 | 0.06 |
| Total reflux events: mean ± SEM | 22.5± 4.9 | 25.1 ± 7.3 | 0.54 |
| Proximal reflux events: mean ± SEM | 8.7 ± 4.4 | 6.4 ± 3.7 | 0.29 |
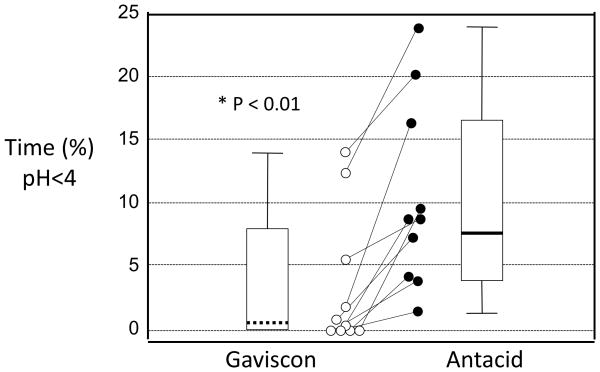
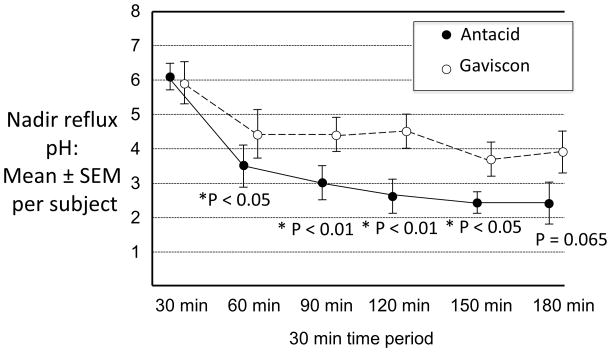
Figure 1 illustrates the median, IQR, range and paired esophageal acid exposure data for each study participant, showing reasonable consistency in the effect among study subjects. Figure 2 illustrates the mean nadir pH for each 30-minute postprandial study period. Evident in the Figure, after the first 30-minute period the nadir pH was significantly greater in the Gaviscon studies and this effect persisted until 150 minutes postprandially. Logically, the decreased esophageal acid exposure observed during the Gaviscon studies was related to the decreased acidity of the refluxate during these periods.
Figure 1.
Median, IQR, range (box plots) and paired (dots) acid exposure times for study subjects during Gaviscon Double Action Liquid (left, dashed line, white dots) and antacid (right, black line, black dots) studies. A consistent decrease was observed with Gaviscon compared to the antacid with corresponding significant decrease in the median (p<0.01).
Figure 2.
Comparison of the mean nadir pH of refluxate during each 30-minute postprandial period during Gaviscon Double Action Liquid (white dots) and antacid (black dots) studies. After the first 30 minutes, the nadir pH of refluxate was significantly less acidic during the Gaviscon studies and this effect persisted until 150 minutes (p<0.05, paired t-test).
Quantitative and qualitative characteristics of reflux events
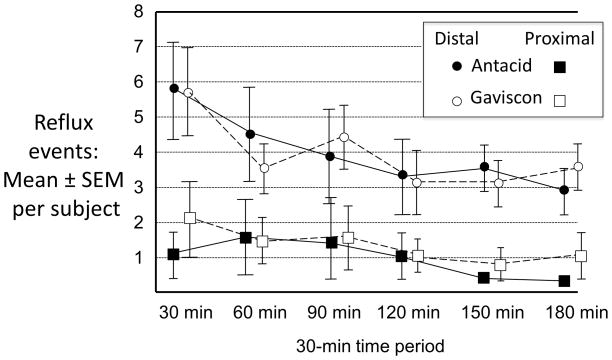
Despite the decreased acidity of refluxate throughout most of the postprandial period, the number of acid reflux events marginally failed to reach significance overall (Table 2). In all likelihood, this was related to small sample size. On the other hand, total reflux events (acid and weakly acidic) were quite similar between study conditions. Impedance data, also summarized in Table 2, show similar numbers of reflux events during Gaviscon and antacid studies. Similarly, there was no difference in the number of proximal reflux events (15–17 cm proximal to the LES). These observations were uniform throughout all 30-minute periods of the study protocol suggesting no differences in either the propensity for reflux or the distribution of reflux in the esophagus between study paradigms.
Mechanisms of reflux and reflux symptoms
When analyzed by mechanism, most reflux events occurred by transient LES relaxation (Table 3) with no difference observed between study conditions.
Table 3.
Mechanisms of reflux. No significant differences were seen between study paradigms. TLESR was the dominant mechanism with both medications. Data expressed as mean±SEM
| Reflux mechanism | Gaviscon | Antacid | P value |
|---|---|---|---|
| TLESR | 10.9 ± 2.0 | 11.5 ± 1.2 | 0.6 |
| Strain | 8.8 ± 4.9 | 10.8 ± 7.8 | 0.3 |
| Swallow | 1.1 ± 0.5 | 1.6 ± 0.7 | 1.0 |
| Hypotensive LES | 1.7 ± 1.4 | 1.0 ± 0.6 | 0.6 |
Subjects reported relatively few reflux symptoms during the studies, again with no systematic differences between study conditions. It should, however, be noted that subjects were somewhat uncomfortable during the studies consequent of having two naso-esophageal tubes in place, perhaps masking reflux-related symptoms.
DISCUSSION
This investigation compared the effectiveness of Gaviscon Double Action Liquid (alginate & antacid) to an equally potent antacid without alginate in controlling postprandial acid reflux in GERD patients. Two 3-hour postprandial impedance pH recordings combined with HRM were done on each study participant in a double-blind crossover design. The major findings of the study were that Gaviscon was associated with significantly less distal esophageal acid exposure than antacid and that this was related to a greater pH of the refluxate rather than to a decrease in the number of reflux events recorded in each study condition. The results suggest that the primary mechanism of efficacy for Gaviscon related to its demonstrated characteristic of localizing with and displacing (or neutralizing) the postprandial acid pocket rather than serving as a mechanical barrier to reflux.
Although the acid pocket was described long ago 13, its relevance to reflux disease is only now coming to light 3. The initial observation was that the minimal pH of esophageal reflux was lower than the concomitant pH recorded from within the stomach 2. Ultimately this paradox was resolved with the description of the acid pocket, the pool of newly secreted acid in the postprandial period that layers on top of ingested chyme rather than mixing with it and serves as the reservoir for postprandial acid reflux events within as little as 17 minutes of eating 4. Subsequent observations were that ingested alginate co-localized with the acid pocket 10 and could displace or even neutralize it 14. The current investigation adds to this with the demonstration that the effect of an alginate-antacid combination was above and beyond that of antacid after the first 30 minutes and persisted for at least 2.5 hours after the meal. These observations support the persistence of the rafting effect of alginate also observed with 3D MRI imagery 15.
An alternative mechanism of action proposed for alginates is of forming a barrier to reflux 15–17. The hypothesis is that through molecular cross-linking, the polysaccharides form a cap over the gastric content and contains it within the stomach 16. If this were the operant mechanism, one would anticipate a lesser number of reflux events in the Gaviscon condition than in the antacid condition. In the current study we observed only a trend in acidic reflux events number decrease likely due to the small sample size. One interesting finding of our study was a shift in the content of the refluxate to being less acidic suggesting that by displacing the acid pocket, it was now the alginate raft that was refluxing rather than gastric secretions. Comparing the Gaviscon to the antacid studies, no differences were seen in either the number of reflux events or in the number of reflux events that reached the proximal esophagus. Furthermore, there was no difference in the mechanism of reflux, in each paradigm being dominated by transient LES relaxation. Nonetheless, there was substantially less esophageal exposure on account of the increased pH of the refluxate during the Gaviscon studies.
Even though they had objectively less acid reflux, we observed no difference in the symptoms experienced by subjects during the Gaviscon studies. In fact, subjects reported relatively few symptoms with either treatment. This outcome is not surprising considering the complex instrumentation and multiple naso-esophageal intubations. The experimental setup does not lend itself to detecting potentially subtle differences in reflux symptoms given the level of discomfort imposed by the experimental setup itself. A better experimental design to assess the impact of the medications on symptoms would be a simple crossover comparison done without any instrumentation with the outcome solely dependent on scoring a questionnaire such as the GerdQ. Such a study was recently conducted comparing Gaviscon Double Action Liquid to placebo finding substantial decrease in heartburn and regurgitation after Gaviscon administration 18.
Limitations of the current study include the immobility imposed on the study subjects by the experimental setup and, as already mentioned, the inherent discomfort of the instrumentation that probably negated our ability to analyze symptoms. Immobility potentially influences the outcome in that it makes it significantly less likely that reflux would occur by any mechanism other than transient LES relaxation and it may be that the alginate effect would be different with strain-induced or swallow-induced reflux 19. Testing that hypothesis would, however, require an ambulatory manometry study, equipment that we do not have at our disposal.
In conclusion, we conducted a physiological study to compare the effectiveness of Gaviscon Double Action Liquid, an alginate-antacid combination, to antacid in controlling postprandial acid reflux in a group of well-defined GERD patients. We found that Gaviscon decreased postprandial acid exposure in the distal esophagus and increased the nadir pH of the refluxate. The effect persisted for at least 2.5 hours. Gaviscon did not, however, decrease the number of reflux events or the proximal extent of reflux within the esophagus. These findings suggest that the dominant mechanism of action for the alginate-antacid combination is to displace and or neutralize the post-prandial acid pocket rather than mechanically constraining it. Nonetheless, the observations suggest a mechanism of action for the alginate-antacid combination uniquely suited to addressing postprandial acid reflux.
Figure 3.
Comparison of the number of reflux events (acid and weakly acidic) observed during the Gaviscon Double Action Liquid (distal events white dots and proximal events white squares) and antacid (distal events black dots and proximal events black square) studies. Similar numbers total and proximal events were observed throughout the duration of the recordings.
Acknowledgments
Financial support: This work was supported by an unrestricted grant from Reckitt Benckiser Group plc and grants DK56033 (PJK) and R01 DK092217 (JEP) from the United States Public Health Service.
Abbreviations
- LES
lower esophageal sphincter
- EGJ
esophago-gastric junction
- GERD
gastro-esophageal reflux disease
- PPI
proton pump inhibitor
Footnotes
Potential competing interests: PJ Kahrilas serves as a paid consultant for AstraZeneca, EndoGastric Solutions, Ironwood Pharmaceuticals, Reckitt Benckiser, and Torax. John E. Pandolfino serves as a paid consultant for AstraZeneca. Sabine Roman serves as a paid consultant for Given Imaging. Annemijn De Ruigh and Joan Chen declare no potential competing interests.
Guarantor of the article: Peter J Kahrilas, MD.
Specific author contributions: Peter J Kahrilas coordinated drafting of the manuscript; all authors contributed to the writing, provided critical revision of the manuscript, and approved the submitted draft.
References
- 1.Camilleri M, Dubois D, Coulie B, et al. Prevalence and socioeconomic impact of upper gastrointestinal disorders in the United States: results of the US Upper Gastrointestinal Study. Clinical gastroenterology and hepatology : the official clinical practice journal of the American Gastroenterological Association. 2005;3(6):543–52. doi: 10.1016/s1542-3565(05)00153-9. [DOI] [PubMed] [Google Scholar]
- 2.Fletcher J, Wirz A, Young J, Vallance R, McColl KE. Unbuffered highly acidic gastric juice exists at the gastroesophageal junction after a meal. Gastroenterology. 2001;121(4):775–83. doi: 10.1053/gast.2001.27997. [DOI] [PubMed] [Google Scholar]
- 3.Kahrilas PJ, McColl K, Fox M, et al. The acid pocket: a target for treatment in reflux disease? The American journal of gastroenterology. 2013;108(7):1058–64. doi: 10.1038/ajg.2013.132. [DOI] [PubMed] [Google Scholar]
- 4.Clarke AT, Wirz AA, Seenan JP, Manning JJ, Gillen D, McColl KE. Paradox of gastric cardia: it becomes more acidic following meals while the rest of stomach becomes less acidic. Gut. 2009;58(7):904–9. doi: 10.1136/gut.2008.161927. [DOI] [PubMed] [Google Scholar]
- 5.Beaumont H, Bennink RJ, de Jong J, Boeckxstaens GE. The position of the acid pocket as a major risk factor for acidic reflux in healthy subjects and patients with GORD. Gut. 2010;59(4):441–51. doi: 10.1136/gut.2009.178061. [DOI] [PubMed] [Google Scholar]
- 6.Pandolfino JE, Zhang Q, Ghosh SK, Post J, Kwiatek M, Kahrilas PJ. Acidity surrounding the squamocolumnar junction in GERD patients: “acid pocket” versus “acid film”. The American journal of gastroenterology. 2007;102(12):2633–41. doi: 10.1111/j.1572-0241.2007.01488.x. [DOI] [PubMed] [Google Scholar]
- 7.Kahrilas PJ, Shaheen NJ, Vaezi MF, et al. American Gastroenterological Association Medical Position Statement on the management of gastroesophageal reflux disease. Gastroenterology. 2008;135(4):1383–1391. 1391 e1–5. doi: 10.1053/j.gastro.2008.08.045. [DOI] [PubMed] [Google Scholar]
- 8.Rohof WO, Bennink RJ, Boeckxstaens GE. Proton Pump Inhibitors Reduce the Size and Acidity of the Acid Pocket in the Stomach. Clinical gastroenterology and hepatology : the official clinical practice journal of the American Gastroenterological Association. 2014 doi: 10.1016/j.cgh.2014.04.003. Epub ahead of print. [DOI] [PubMed]
- 9.Vo L, Simonian HP, Doma S, Fisher RS, Parkman HP. The effect of rabeprazole on regional gastric acidity and the postprandial cardia/gastro-oesophageal junction acid layer in normal subjects: a randomized, double-blind, placebo-controlled study. Alimentary pharmacology & therapeutics. 2005;21(11):1321–30. doi: 10.1111/j.1365-2036.2005.02489.x. [DOI] [PubMed] [Google Scholar]
- 10.Rohof WO, Bennink RJ, Smout AJ, Thomas E, Boeckxstaens GE. An alginate-antacid formulation localizes to the acid pocket to reduce acid reflux in patients with gastroesophageal reflux disease. Clinical gastroenterology and hepatology : the official clinical practice journal of the American Gastroenterological Association. 2013;11(12):1585–91. doi: 10.1016/j.cgh.2013.04.046. quiz e90. [DOI] [PubMed] [Google Scholar]
- 11.Pandolfino JE, Ghosh SK, Zhang Q, Jarosz A, Shah N, Kahrilas PJ. Quantifying EGJ morphology and relaxation with high-resolution manometry: a study of 75 asymptomatic volunteers. American journal of physiology Gastrointestinal and liver physiology. 2006;290(5):G1033–40. doi: 10.1152/ajpgi.00444.2005. [DOI] [PubMed] [Google Scholar]
- 12.Roman S, Zerbib F, Belhocine K, des Varannes SB, Mion F. High resolution manometry to detect transient lower oesophageal sphincter relaxations: diagnostic accuracy compared with perfused-sleeve manometry, and the definition of new detection criteria. Alimentary pharmacology & therapeutics. 2011;34(3):384–93. doi: 10.1111/j.1365-2036.2011.04728.x. [DOI] [PubMed] [Google Scholar]
- 13.Cannon WB. The Movements of the stomach, studied by means of the Rontgen Rays. Boston Soc Med Sci. 1898;2:59–66. [Google Scholar]
- 14.Kwiatek MA, Roman S, Fareeduddin A, Pandolfino JE, Kahrilas PJ. An alginate-antacid formulation (Gaviscon Double Action Liquid) can eliminate or displace the postprandial ‘acid pocket’ in symptomatic GERD patients. Alimentary pharmacology & therapeutics. 2011;34(1):59–66. doi: 10.1111/j.1365-2036.2011.04678.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sweis R, Kaufman E, Anggiansah A, et al. Post-prandial reflux suppression by a raft-forming alginate (Gaviscon Advance) compared to a simple antacid documented by magnetic resonance imaging and pH-impedance monitoring: mechanistic assessment in healthy volunteers and randomised, controlled, double-blind study in reflux patients. Alimentary pharmacology & therapeutics. 2013;37(11):1093–102. doi: 10.1111/apt.12318. [DOI] [PubMed] [Google Scholar]
- 16.Hampson FC, Farndale A, Strugala V, Sykes J, Jolliffe IG, Dettmar PW. Alginate rafts and their characterisation. International journal of pharmaceutics. 2005;294(1–2):137–47. doi: 10.1016/j.ijpharm.2005.01.036. [DOI] [PubMed] [Google Scholar]
- 17.Zentilin P, Dulbecco P, Savarino E, et al. An evaluation of the antireflux properties of sodium alginate by means of combined multichannel intraluminal impedance and pH-metry. Alimentary pharmacology & therapeutics. 2005;21(1):29–34. doi: 10.1111/j.1365-2036.2004.02298.x. [DOI] [PubMed] [Google Scholar]
- 18.Thomas E, Wade A, Crawford G, Jenner B, Levinson N, Wilkinson J. Randomised clinical trial: relief of upper gastrointestinal symptoms by an acid pocket-targeting alginate-antacid (Gaviscon Double Action) - a double-blind, placebo-controlled, pilot study in gastro-oesophageal reflux disease. Alimentary pharmacology & therapeutics. 2014;39(6):595–602. doi: 10.1111/apt.12640. [DOI] [PubMed] [Google Scholar]
- 19.van Herwaarden MA, Samsom M, Smout AJ. Excess gastroesophageal reflux in patients with hiatus hernia is caused by mechanisms other than transient LES relaxations. Gastroenterology. 2000;119(6):1439–46. doi: 10.1053/gast.2000.20191. [DOI] [PubMed] [Google Scholar]