Abstract
IMPORTANCE
More than 300 000 hip fractures occur each year in the United States. Recent practice guidelines have advocated greater use of regional anesthesia for hip fracture surgery.
OBJECTIVE
To test the association of regional (ie, spinal or epidural) anesthesia vs general anesthesia with 30-day mortality and hospital length of stay after hip fracture.
DESIGN, SETTING, AND PATIENTS
We conducted a matched retrospective cohort study involving patients 50 years or older who were undergoing surgery for hip fracture at general acute care hospitals in New York State between July 1, 2004, and December 31, 2011. Our main analysis was a near-far instrumental variable match that paired patients who lived at different distances from hospitals that specialized in regional or general anesthesia. Supplementary analyses included a within-hospital match that paired patients within the same hospital and an across-hospital match that paired patients at different hospitals.
EXPOSURES
Spinal or epidural anesthesia; general anesthesia.
MAIN OUTCOMES AND MEASURES
Thirty-day mortality and hospital length of stay. Because the distribution of length of stay had long tails, we characterized this outcome using the Huber M estimate with Huber weights, a robust estimator similar to a trimmed mean.
RESULTS
Of 56 729 patients, 15 904 (28%) received regional anesthesia and 40 825 (72%) received general anesthesia. Overall, 3032 patients (5.3%) died. The M estimate of the length of stay was 6.2 days (95% CI, 6.2 to 6.2). The near-far matched analysis showed no significant difference in 30-day mortality by anesthesia type among the 21 514 patients included in this match: 583 of 10 757 matched patients (5.4%) who lived near a regional anesthesia– specialized hospital died vs 629 of 10 757 matched patients (5.8%) who lived near a general anesthesia–specialized hospital (instrumental variable estimate of risk difference, −1.1%; 95% CI, −2.8 to 0.5; P = .20). Supplementary analyses of within and across hospital patient matches yielded mortality findings to be similar to the main analysis. In the near-far match, regional anesthesia was associated with a 0.6-day shorter length of stay than general anesthesia (95% CI, −0.8 to −0.4, P < .001). Supplementary analyses also showed regional anesthesia to be associated with shorter length of stay, although the observed association was smaller in magnitude than in the main analysis.
CONCLUSIONS AND RELEVANCE
Among adults in acute care hospitals in New York State undergoing hip repair, the use of regional anesthesia compared with general anesthesia was not associated with lower 30-day mortality but was associated with a modestly shorter length of stay. These findings do not support a mortality benefit for regional anesthesia in this setting.
Each year, 300 000 hip fractures occur in the United States,1, 2 leading to functional disability3 and mortality.2 Regional anesthesia for hip fracture surgery via spinal or epidural blockade plus sedation may reduce postoperative complications,4-6 and practice guidelines have called for broader use of regional anesthesia for hip fracture surgery.7-9
Most studies assessing the relationship between anesthesia technique and outcomes are observational and not prospective. Recent observational studies regarding the association of anesthesia technique with hip fracture outcomes have shown conflicting results.6,10-13 Typically, clinicians select the anesthesia technique based on their practice style and a variety of patient-related factors. For example, impaired coagulation is a contraindication to spinal and epidural anesthesia.14
Because it is believed there is less morbidity associated with regional anesthesia, patients with hip fracture receiving regional anesthesia tend to be older and sicker than those treated with general anesthesia.13 Consequently, analyses of observational data may be limited because of the nonrandom selection of patients for one form of anesthesia or another. This limitation can potentially be addressed using instrumental variable analysis, which capitalizes on differences in practice patterns across providers or facilities to approximate the structure of a randomized trial within the setting of an observational study.15
We assessed the association of anesthesia technique with 30-day mortality and hospital length of stay among older adults undergoing hip fracture surgery in New York between 2004 and 2011. To go beyond prior observational studies, we used 2 statistical techniques intended to address selection bias, multivariable matching, and instrumental variable analysis. We hypothesized that regional anesthesia would be associated with improved outcomes compared with general anesthesia.
Methods
Data Sources
We obtained data on acute care hospital discharges between January 1, 2004, and December 31, 2011, from New York’s Statewide Planning and Research Cooperative System (SPARCS). Our data set included unique patient identifiers and indicators of 30-day mortality. We obtained hospital characteristics data from the 2006 American Hospital Association Survey and data on zip code area characteristics from census files. The study was approved by the Perelman School of Medicine institutional review board, which waived the requirement for participant informed consent.
Population
Our starting population included adults 50 years or older hospitalized with a hip fracture and a principal procedure of open reduction, internal fixation, hemiarthroplasty, or total hip arthroplasty, which were identified using International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes (eAppendix in the Supplement). We used 50 years as an age cutoff because osteoporotic hip fractures are uncommon among those younger than this age. To allow for examination of hospital discharge data from the 180 days preceding the index admission, we studied hospitalizations between July 1, 2004, and December 31, 2011. For patients with multiple hip fracture admissions, the first admission was the index.
We excluded patients with diagnosis related group codes indicating multiple trauma and patients with secondary ICD-9-CM procedure codes indicating selected other surgeries (eAppendix in the Supplement). We excluded patients who had missing data, who received local anesthesia, who were transferred from another hospital, and who lived outside New York.
Outcomes
Our primary outcome was death at 30 days after admission. Inpatient length of stay in days was our secondary outcome.
Exposure Variable
Hospitals voluntarily report data on anesthesia care to SPARCS. Anesthesia type is recorded as regional, general, local, other, or none. General anesthesia plus another type of anesthesia is coded as general anesthesia. Of 195 hospitals reporting hip fracture discharges over the study period, 36 did not report any data on anesthesia type.
Key Covariates
Data from SPARCS included age, sex, fracture location, surgical procedure, nursing facility residence, and 18 comorbidi-ties identified by ICD-9-CM codes16-18 and present-on-admission indicators for the index admission and hospitalizations in the preceding 180 days. As a proxy for factors related to Medicaid eligibility, we collected data on Medicaid insurance status. Because hip fracture care18 and outcomes19 may differ for black and white patients, we obtained data on patient race, which we coded as white, black, or other. We collected census data on the median income of each patient’s residential zip code, the percentage of residents completing high school or some college, and the percentage below the poverty line. We obtained data from the American Hospital Association survey on hospital bed size, nurse to bed ratio, nurse skill mix (registered nurses plus licensed practical nurses out of all nurses), teaching status, and level I trauma center status.
Near-Far Matching
Prior observational studies of anesthesia for hip fracture have used regression to adjust for observed differences between patients. However, these methods cannot adjust for unobserved factors that may influence anesthesia care, such as illness severity, cognitive impairment, or fracture displacement.
To address this issue, our primary analysis used near-far matching, a matched-pair instrumental variable study design.20-22 Use of regional anesthesia varies across hospitals.11 Because patients seek care for hip fractures at hospitals near their homes, someone who lives closer to a hospital where regional anesthesia is used heavily may be more likely to receive regional anesthesia for hip fracture surgery than someone who lives closer to a hospital where regional anesthesia is avoided. After matching for observed patient factors, proximity to a hospital that often uses regional anesthesia is an instrumental variable if it affects outcomes only by promoting use of regional anesthesia (the so-called exclusion restriction) and if proximity is otherwise unrelated to unmeasured risk factors conditionally given measured risk factors.23 An in strumental variable estimate, such as the Wald estimate, attributes effects of proximity to the greater use of regional anesthesia at some hospitals.23
Our instrumental variable was the difference between the linear distance from each patient’s residence to the nearest in-state hospital that specialized in general anesthesia and the distance from each patient’s residence to the nearest in-state hospital that specialized in regional anesthesia. We classified hospitals as specializing in regional or general anesthesia based on the percentage of their patients with a hip fracture who received regional anesthesia over the full study period. Because the median rate of regional anesthesia across all hospitals was one-third, this value was our cutoff for specialization toward regional vs general anesthesia. Out of 159 hospitals that reported anesthesia data to SPARCS, we classified 63 as regional anesthesia-specialized and 96 as general anesthesia-specialized. Characteristics of study hospitals appear in eTable 1 in the Supplement. Because we lacked patient addresses, distances were calculated from the center of each patient’s residential zip code area.
We paired each patient who lived relatively closer to a regional anesthesia–specialized hospital to a similar patient who lived relatively closer to a general anesthesia– specialized hospital. We matched pairs exactly for sex, fracture type, procedure type, procedure year, and chronic lung disease. We used fine balance24 (a method of constraining 2 groups to be balanced on a particular variable without restricting matching on the variable within individual pairs) for comorbidities, race, Medicaid eligibility, nursing home residence, and hospital trauma center and teaching status. We paired patients who were most similar in terms of measured covariates. Specifically, we minimized the total over pairs of the within-pair distances on covariates. We used the Mahalanobis distance,25,26 which is the difference in covari ate values for patients living near regional anesthesia and patients living near general anesthesia, divided by the covariate’s standard deviation, this quantity squared, summed over the various covariates, with an allowance for correlation among the covariates.
Our distance incorporated all study variables and penalized large distances on a propensity score that we estimated with logit regression using the same variables to predict the likelihood of living closer to a regional anesthesia than to general anesthesia. We used optimal subset matching27 to avoid individually poor matches. Optimal subset matching solves an optimization problem to pick the most similar individuals from treated and control groups, omitting treated subjects without similar control and controls without similar treated subjects. To ensure that paired individuals differed meaning fully in terms of the instrumental variable,20,28 we excluded all patients who resided in zip codes where the absolute value of the instrumental variable was less than 2 miles. Within pairs, we required individual patients to differ by at least 15 miles in their relative proximity to hospitals specializing in regional vs general anesthesia.
Data Analysis
To assess the quality of our match, we used standardized differences, which we calculated for a given variable by dividing the mean difference between matched patients by the pooled standard deviation before matching.29-31 We used a bench mark of 0.10, or one-tenth of a standard deviation, as a maximum acceptable standardized difference.29-32
We first present an unadjusted, unmatched comparison of mortality and length of stay according to anesthesia type among patients who received regional vs general anesthesia. Next, we present the appropriate analysis that controls for measured and unmeasured patient-level confounders through our near-far matched analysis. This analysis used instrumental variable methods to rescale any differences in outcomes between matched patients to account for the difference in rates of actual treatment with regional anesthesia across groups.23 Without use of an instrumental variable estimator, our near-far comparison would estimate the effect of living near a hospital that often uses regional anesthesia, not the effect of actually receiving regional anesthesia. The instrumental variable estimate is a consequence of attributing to use of regional anesthesia any benefit or harm associated with living near a hospital that often uses regional anesthesia.
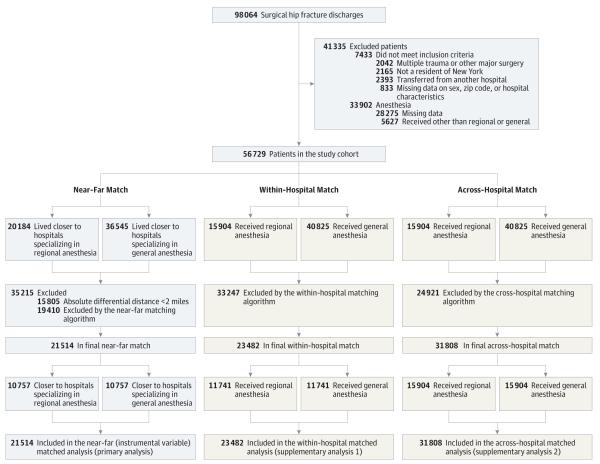
We also present 2 Supplementary analyses. A within-hospital match-paired patients who received regional and general anesthesia within the same hospital as a means of accounting for potential differences between facilities specializing in one or another type of anesthesia. An across-hospital match used standard propensity-score methods to pair patients who received regional and general anesthesia across different hospitals. Details of these matches appear in the eAppendix in the Supplement. Outcomes were examined only after matching was completed.33 An overview of our study design appears in Figure 1.
Figure 1.
Overview of Study Design, Showing the Near-Far Match, the Across-Hospital Match, and the Unadjusted, Unmatched Comparison Our study incorporated 3 matched comparisons. The primary analysis was a “near-far” instrumental variable match that included 10 757 pairs of patients who differed in terms of their residential proximity to hospitals specializing in regional or general anesthesia for hip fracture but were similar in terms of all other observable characteristics. Supplementary analyses included a within-hospital match that paired patients receiving regional vs general anesthesia within the same hospital and an across-hospital match that paired patients receiving regional vs general anesthesia across different hospitals.
We tested for differences in 30-day mortality using the McNemar test for matched pairs and the χ2 statistic for the unmatched comparison. As an outcome, length of stay had long tails, so we used the Huber M estimate with Huber weights,34-36 the standard robust estimator similar to a trimmed mean, to estimate the length of stay within each group and the within-pair difference in length of stay. We used its permutation distribution to obtain confidence intervals for instrumental variable estimates by the standard pivotal method20,37 applied to this permutation distribution.37 For binary outcomes, the pivotal method reports an instrumental variable confidence interval that excludes the null hypothesis of no effect only if the McNemar test rejects no effect when testing the effect of living near a regional hospital.20
All hypothesis tests were 2-sided. We used a significance threshold of P < .05. We conducted sensitivity analyses for all significant findings to assess the magnitude ofbias from unmeasured confounders that would need to be present to alter our conclusions.38,39 Analyses were conducted by R 2.13.1 (R Foundation) and SAS software version 9.3 (SAS Institute Inc), using the R mipmatch package40 and the SAS PROC ASSIGN function.
Results
Unadjusted, Unmatched Comparison
After exclusions (Figure 1), our study cohort included 56 729 patients; 28 275 patients were excluded due to missing anesthesia data (eTable 2 in the Supplement). Compared with patients with available anesthesia data, patients with missing data were more likely to have come from an area with lower educational attainment and greater poverty, to be of black race, to be covered by Medicaid, and to be treated in a trauma center.
Among patients with available anesthesia data, 28% received regional anesthesia (n = 15 904) and 72% received general anesthesia (n = 40 825). Compared with patients receiving general anesthesia, those receiving regional anesthesia were older, more often had chronic lung disease, resided in areas with higher incomes, and were treated in hospitals that were smaller, had less skilled nursing staffs, and were not teaching hospitals or trauma centers (Table 1). Overall, 3032 patients died, for a mortality rate of 5.3%. The M estimate of the length of stay (a robust measure of location similar to a trimmed mean34-36) was 6.2 days (95% CI, 6.2-6.2).
Table 1.
Baseline Characteristics of Patients Receiving Regional and General Anesthesia for Hip Fracture Surgerya
| No. (%) of Patients Receiving Anesthesia |
||||
|---|---|---|---|---|
| Regional (n = 15 904) |
General (n = 40 825) |
Absolute Standardized Differenceb |
P Value |
|
| Demographics, nursing home residence, and Medicaid coverage |
||||
| Age, mean (SD), y | 82.2 (9.5) | 81.1 (10.1) | 0.11 | <.001 |
| Women | 4059 (74.5) | 10 686 (73.8) | 0.01 | .11 |
| Race | ||||
| White | 14 235 (89.5) | 35 945 (88.1) | 0.05 | <.001 |
| Black | 399 (2.5) | 1433 (3.5) | 0.06 | <.001 |
| Other | 1270 (8.0) | 3447 (8.4) | 0.02 | <.001 |
| Nursing home resident | 617 (3.9) | 1517 (3.7) | <0.01 | .36 |
| Medicaid eligible | 2536 (16.0) | 6900 (16.9) | 0.03 | .006 |
| Common comorbidities, present in more than 3% of the study population |
||||
| Dementia | 4060 (25.5) | 10 411 (25.5) | <0.01 | .95 |
| Prior stroke | 1116 (7.0) | 2989 (7.3) | 0.01 | .21 |
| Congestive heart failure | 2546 (16.0) | 6770 (16.6) | 0.02 | .10 |
| Myocardial infarction | 957 (6.0) | 2301 (5.7) | 0.02 | .100 |
| Past cardiac arrhythmia | 3392 (21.3) | 9237 (22.6) | 0.03 | <.001 |
| Cardiac valvular disease | 1861 (11.7) | 5336 (13.1) | 0.04 | <.001 |
| Hypertension | 10 500 (66.0) | 27 521 (67.4) | 0.03 | .002 |
| Chronic lung disease | 3206 (20.2) | 6443 (15.8) | 0.11 | <.001 |
| Renal failure | 127 (7.0) | 485 (8.2) | 0.05 | <.001 |
| Diabetes mellitus | 3218 (20.2) | 8810 (21.6) | 0.03 | <.001 |
| Electrolyte abnormality | 2771 (17.4) | 7298 (17.9) | 0.01 | .21 |
| Thrombocytopenia | 396 (2.5) | 1383 (3.4) | 0.05 | <.001 |
| Cancer | 2117 (13.3) | 5032 (12.3) | 0.03 | .002 |
| Fracture type | ||||
| Femoral neck | 7647 (48.1) | 19 157 (46.9) | 0.02 | .95 |
| Intertrochanteric | 7312 (46.0) | 18 919 (46.3) | <0.01 | .44 |
| Subtrochanteric | 617 (3.9) | 1698 (4.7) | 0.04 | <.001 |
| ≥2 | 328 (2.1) | 838 (2.1) | <0.01 | .01 |
| Procedure | ||||
| Total hip arthroplasty | 596 (3.8) | 1698 (4.2) | 0.02 | .03 |
| Hemiarthroplasty | 5394 (33.9) | 13 184 (32.3) | 0.03 | <.001 |
| Internal fixation | 9914 (62.3) | 25 943 (63.6) | 0.02 | .008 |
| Residential zip code area characteristics, mean (SD) |
||||
| Median income, $ | 53 802 (22 512) |
50 746 (19 770) |
0.14 | <.001 |
| Below poverty, % | 11.0 (7.8) | 11.2 (8.6) | 0.03 | .06 |
| Completing college, % | 29.6 (16.7) | 28.4 (14.9) | 0.08 | .01 |
| Completing high school, % | 82.7 (9.4) | 82.6 (9.4) | 0.02 | .72 |
| Hospital characteristics, mean (SD) | ||||
| No. of beds | 381 (376) | 524 (422) | 0.35 | <.001 |
| Nurse skill mixc | 90.7 (7.2) | 91.7 (7.2) | 0.13 | <.001 |
| Nurse to bed ratiod | 1.56 (0.4) | 1.55 (0.5) | 0.03 | <.001 |
| Teaching hospital, % | 3720 (23.4) | 13 939 (34.1) | 0.24 | <.001 |
| Trauma center, % | 2264 (14.2) | 7239 (17.7) | 0.10 | <.001 |
Data are unadjusted. Selected variables shown; additional results appear in the Appendix.
The standardized difference for each variable is the mean difference between patients in each group as a fraction of the pooled standard deviation across both groups.
Nurse skill mix equals the total number of full-time-employee registered nurses and licensed practical nurses divided by total number of full-time employee nurses.
Nurse to bed ratio calculated as total number of full-time employee nurses divided by total number of hospital beds.
Thirty-day mortality for regional anesthesia was 5.3% and 5.4% for general anesthesia (difference, −0.1%; 95% CI, −0.5 to 0.3; P = .55); regional anesthesia was associated with a shorter unadjusted length-of-stay of 6 days (95% CI, 6.0 to 6.1) vs 6.3 days with general anesthesia (95% CI, 6.2 to 6.3). The difference in length of stay for regional vs general anesthesia was −0.2 days (95% CI, –0.3 to –0.2; P < .001).
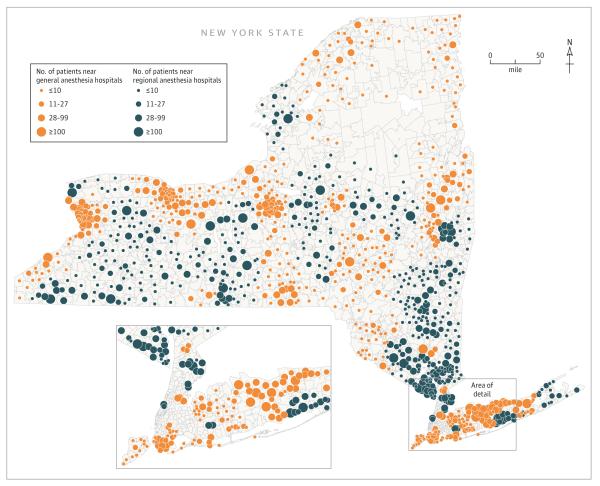
Near-Far Match
Our near-far match comprised 10 757 pairs of patients drawn from across New York State (Figure 2) that were similar in terms of observable factors. Selected variables used in the match appear in Table 2; detailed results appear in eTable 3 in the Supplement. Differential distance was strongly associated with the type of anesthesia received: 53.5% of patients who lived closer to a hospital that specialized in regional anesthesia received it whereas 16.1% of those who lived closer to a hospital that specializedin general anesthesia received regional anesthesia (P < .001).
Figure 2.
Geographic Distribution of Patients Included in the Near-Far Matched Sample Orange circles correspond to patients residing in areas located relatively closer to hospitals that specialized in general anesthesia; blue circles correspond to patients residing in areas located relatively closer to hospitals that specialized in regional anesthesia. The interior borders represent zip code area boundaries.
Table 2.
Characteristics of Patients Included in the Near-Far Matcha
| No. (%) of Patients Receiving Anesthesia |
||||
|---|---|---|---|---|
| Near Regional Anesthesia (n = 10 757) |
Near General Anesthesia (n = 10 757) |
Absolute Standardized Differenceb |
P Value |
|
| Demographics, nursing home residence, and Medicaid coverage |
||||
| Age, mean (SD), y | 81.3 (10.0) | 81.2 (9.9) | 0.02 | .10 |
| Women | 2864 (73.4) | 2864 (73.4) | <0.01 | >.99 |
| Race | ||||
| White | 10 107 (94.0) | 1 107 (94.0) | <0.01 | >.99 |
| Black | 173 (1.6) | 173 (1.6) | <0.01 | >.99 |
| Other | 477 (4.4) | 477 (4.4) | <0.01 | >.99 |
| Nursing home resident | 449 (4.2) | 449 (4.2) | <0.01 | >.99 |
| Medicaid eligible | 1457 (13.5) | 1457 (13.5) | <0.01 | >.99 |
| Common comorbidities, present in more than 3% of the study population |
||||
| Dementia | 2862 (24.9) | 2862 (24.9) | <0.01 | >.99 |
| Prior stroke | 740 (6.9) | 740 (6.9) | <0.01 | >.99 |
| Congestive heart failure | 1680 (15.6) | 1680 (15.6) | <0.01 | >.99 |
| Myocardial infarction | 615 (5.7) | 615 (5.7) | <0.01 | >.99 |
| Past cardiac arrhythmia | 2359 (21.9) | 2359 (21.9) | <0.01 | >.99 |
| Cardiac valvular disease | 1391 (12.9) | 1391 (12.9) | <0.01 | >.99 |
| Hypertension | 7267 (67.6) | 7267 (67.6) | <0.01 | >.99 |
| Chronic lung disease | 2004 (18.6) | 2004 (18.6) | <0.01 | >.99 |
| Renal failure | 738 (6.9) | 738 (6.9) | <0.01 | >.99 |
| Diabetes mellitus | 2268 (21.1) | 2268 (21.1) | <0.01 | >.99 |
| Electrolyte abnormality | 1909 (17.8) | 1909 (17.8) | <0.01 | >.99 |
| Thrombocytopenia | 301 (2.8) | 301 (2.8) | <0.01 | >.99 |
| Cancer | 1377 (12.8) | 1377 (12.8) | <0.01 | >.99 |
| Fracture type | ||||
| Femoral neck | 5307 (49.3) | 5307 (49.3) | <0.01 | >.99 |
| Intertrochanteric | 4810 (44.7) | 4810 (44.7) | <0.01 | >.99 |
| Subtrochanteric | 442 (4.1) | 442 (4.1) | <0.01 | >.99 |
| ≥2 | 198 (1.8) | 198 (1.8) | <0.01 | >.99 |
| Procedure | ||||
| Total hip arthroplasty | 394 (3.7) | 394 (3.7) | <0.01 | >.99 |
| Hemiarthroplasty | 3721 (34.6) | 3721 (34.6) | <0.01 | >.99 |
| Internal fixation | 6642 (61.8) | 6642 (61.8) | <0.01 | >.99 |
| Residential zip code area characteristics, mean (SD) |
||||
| Median income, $ | 49 523 (18 298) | 50 263 (20 549) | 0.04 | .78 |
| Below poverty, % | 10.6 (5.9) | 10.7 (7.6) | 0.02 | <.001 |
| Completing college, % | 25.6 (12.8) | 25.7 (12.4) | 0.02 | .006 |
| Completing high school, % | 83.6 (6.3) | 83.6 (8.0) | <0.01 | <.001 |
| Hospital characteristics | ||||
| No. of beds, mean (SD) | 270 (200) | 269 (167) | <0.01 | <.001 |
| Nurse skill mix, mean (SD)c | 89.0 (7.4) | 89.2 (8.7) | 0.03 | <.001 |
| Nurse to bed ratio, mean (SD)d | 1.5 (0.4) | 1.5 (0.6) | 0.01 | .09 |
| Teaching hospital, % | 471 (8.6) | 471 (8.6) | <0.01 | >.99 |
| Trauma center, % | 925 (4.4) | 925 (4.4) | <0.01 | >.99 |
Selected variables are shown; full match results are presented in the Appendix.
The standardized difference for each variable is the mean difference between patients in each matched group as a fraction of the pooled standard deviation before matching..
Nurse skill mix calculated as total number of full-time-employee registered nurses and licensed practical nurses divided by total number of full-time employee.
Nurses to bed ratio calculated as total number of full-time employee nurses divided by total number of hospital beds.
Before matching, unadjusted 30-day mortality was 5.7% (790 of 13 842) among patients living closer to hospitals that specialized in regional anesthesia vs 5.6% (1527 of 27 082) among those living closer to hospitals that specialized in general anesthesia (P = .79). After matching, mortality was 5.4% among patients living closer to hospitals that specialized in regional anesthesia vs 5.8% among those living closer to hospitals that specialized in general anesthesia, for a difference of −0.4% (95% CI, –1.0 to 0.2; P = .18; Table 3). In the instrumental variable analysis, we did not observe a statistically significant association between anesthesia type and mortality (absolute risk difference, regional vs general anesthesia, −1.1%, 95% CI, −2.8% to 0.5%; P = .18).
Table 3.
Study Outcomes for the Near-Far, Within-Hospital, and Across-Hospital Matches and the Unmatched, Unadjusted Comparisona
| Anesthesia Typeb | Instrumental Variable Estimate, | |||||||
|---|---|---|---|---|---|---|---|---|
| Comparison | Regional Anesth |
General | Risk Difference (95% CI) |
Difference in Days (95% CI) |
P Value |
Risk Difference (95% CI) |
Difference in Days (95% CI) |
P Value |
| Near-far, instrumental variable match |
||||||||
| No. of patients | 10 757 | 10 757 | ||||||
| 30-Day mortality, No. (%) |
583 (5.4) |
629 (5.8) |
−0.4 (−1.0 to 0.2) |
.18 | −1.1 (−2.8 to 0.5) |
.18 | ||
| Hospital length of stay, estimate (95% CI), dc |
5.8 (5.8 to 5.9) |
6.1 (6.1 to 6.2) |
−0.3 (−0.3 to −0.2) |
< .001 | −0.6 (−0.8 to −0.4) |
< .001 | ||
| Within hospital match | ||||||||
| No. of patients | 11 741 | 11 741 | ||||||
| 30-Day mortality, No. (%) |
608 (5.2) |
622 (5.3) |
−0.1 (−0.7 to 0.4) |
.70 | ||||
| Hospital length of stay, estimate (95% CI), dc |
6.1 (6.1 to 6.2) |
6.3 (6.3 to 6.4) |
−0.2 (−0.3 to −0.2) |
< .001 | ||||
| Across hospital match | ||||||||
| No. of patients | 15 904 | 15 904 | ||||||
| 30-Day mortality, No. (%) |
835 (5.3) |
920 (5.8) |
−0.5 (−1.0 to −0.0) |
.03 | ||||
| Hospital length of stay, estimate (95% CI), dc |
6.0 (6.0 to 6.1) |
6.3 (6.3 to 6.4) |
−0.3 (−0.3 to −0.2) |
< .001 | ||||
| Unadjusted, unmatched comparison |
||||||||
| No. of patients | 15 904 | 40 825 | ||||||
| 30-Day mortality, No. (%) |
835 (5.3) |
2197 (5.4) |
−0.1 (−0.5 to 0.3) |
.54 | ||||
| Hospital length of stay, estimate (95% CI), dc |
6.0 (6.0 to 6.1) |
6.3 (6.2 to 6.3) |
−0.2 (−0.3 to −0.2) |
< .001 | ||||
Data are shown on 30-d mortality and hospital length of stay with regional vs general anesthesia from 4 comparisons; please see Methods section for a description of individual comparisons. For the near-far match, we present instrumental variable estimates of the association of regional vs general anesthesia with mortality and length of stay. As is always true, the instrumental variable estimate is larger than the simple between-groups difference, reflecting the fact that only some additional patients received regional anesthesia by virtue of living near hospitals that used it more frequently.
The near-far instrumental variable match compares patients living closer to hospitals specializing in regional anesthesia with patients living closer to hospitals specializing in general anesthesia. The within-hospital match, the across-hospital match, and the unmatched comparison compare patients who received regional anesthesia with patients who received general anesthesia.
Cells show Huber’s M-estimates and 95% confidence intervals for the length of stay among patients receiving regional vs general anesthesia and for the within-pair difference in the length of stay.
The robust estimate of the length of stay among matched patients residing nearer to hospitals that specialized in regional anesthesia was 5.8 days (95% CI, 5.8 to 5.9) vs 6.1 days among patients residing closer to hospitals that specialized in general anesthesia (95% CI, 6.2 to 6.2; difference, −0.3 days; 95% CI, −0.3 to −0.2; P < .001; Table 3). In instrumental variable analysis, regional anesthesia was associated with a 0.6-day shorter length of stay (95% CI, −0.8 to −0.4; P < .001).
Supplementary Analyses
Supplementary analyses were consistent with our near-far match (eTables 4 and 5 in the Supplement and Table 3). Thirty-day mortality was similar among patients receiving regional vs general anesthesia within the same hospital (regional, 5.2%; 95% CI, 4.8% to 5.6% vs general, 5.3% (95% CI, 4.9% to 5.7%; P = .70k), although mortality was lower among patients who received regional vs general anesthesia across different hospitals (regional, 5.3%; 95% CI, 4.9% to 5.6% vs general, 5.8%;95% CI, 5.4% to 6.2%; P = .04). Regional anesthesia was associated with shorter length of stay in the within-hospital match (difference, regional vs general, −0.2 days; 95% CI, −0.3 to −0.2; P < .001) and theacross-hospital match (difference, regional vs general, −0.3 days; 95% CI, −0.3 to −0.2; P < .001).
Sensitivity Analysis
Sensitivity analyses (eTables 6-9 in the Supplement) indicated that the length-of-stay findings from our near-far match would remain statistically significant in the presence of a confounder that increased the odds of both general anesthesia and a longer length of stay by 40%, suggesting that our length of stay findings would not be qualitatively changed by small biases from unmeasured confounders.
Discussion
Among 56 729 patients undergoing hip fracture surgery in New York between 2004 and 2011, we did not observe a statistically significant difference in mortality according to anesthesia technique. Nevertheless, we found regional anesthesia to be associated with hospital length of stay that was shorter by a half day for a representative patient. These findings came from an instrumental variable analysis that accounted for observed and unobserved differences between patients receiving regional vs general anesthesia; we obtained consistent results from Supplementary analyses, including a match that paired similar patients who received regional vs general anesthesia within the same hospital.
Our work adds to previous research on anesthesia for hip fracture. A meta-analysis of 8 small trials published between 1978 and 1998 found equivocal evidence of lower mortality with regional vs general anesthesia and no difference in hospital length of stay.4 The present study includes groups that were excluded from certain trials, such as patients with dementia41,42 and those undergoing hemiarthroplasty or total hip arthroplasty.43 Furthermore because our database extends through 2011, our findings may be more relevant than historical studies to current practice.
Observational studies by our group11 and others6,10 have been conflicted regarding the association of anesthesia technique with hip fracture outcomes, although the interpretation of these studies is limited by their lack of adjustment for potentially important confounders. In contrast to prior observational studies, our near-far analysis compared patients whose anesthesia care varied as a result of their residential proximity to specific types of hospitals instead of a process of clinical selection. This analysis not only adjusted for observed patient factors but also potentially addressed confounding due to unobserved differences among patients who received regional vs anesthesia. As such, our findings suggest an association between regional anesthesia and shorter length-of-stay, which could relate to reductions in complications41,44-46 or more effective rehabilitation.47
Our study has limitations. We examined one state, and could not assess outcomes among patients with missing anesthesia data. The observational design of our study precludes causal conclusions because we cannot fully rule out the possibility of residual confounding. In particular, our main results could be explained by residual confounding if proximity to regional anesthesia is not a perfect instrument. If hospital specialization toward regional anesthesia were associated with other differences in quality, for example, the length-of-stay differences observed in the near-far analysis could reflect such quality differences rather than an effect of regional anesthesia per se. Nevertheless, our observation of consistent findings in our within-hospital match, which explicitly accounted for hospital-level factors, provides reassurance regarding the validity of our main results. Also, as general anesthesia–specialized hospitals in our near-far match had features commonly associated with higher quality, such as higher nurse-to-bed ratios and trauma center designation, we would expect such hospital-level differences to bias our findings toward the null hypothesis. Finally, because we lacked detailed intraoperative data, we could not examine the degree to which regional anesthesia outcomes might vary according to the type of block performed or the depth of sedation.45,48
Our findings may have implications for clinical practice and health policy. Regional anesthesia is used as the primary anesthetic technique in a minority of hip fracture surgeries performed in the United States and in other countries,11,49 and in creasing its use has been proposed as a strategy to improve the quality of hip fracture care.7-9 We found an association between greater use of regional anesthesia and a reduction in length of stay after hip fracture; however, we did not find regional anesthesia to be associated with statistically significant differences in mortality.
Conclusions
Among adults in acute care hospitals in New York State undergoing hip repair, the use of regional anesthesia compared with general anesthesia was not associated with a lower 30-day mortality, but was associated with a modestly shorter length of stay. These findings do not support a mortality benefit for regional anesthesia in this setting.
Supplementary Material
Acknowledgments
Funding/Support: This study was supported by grants to MDN from the Foundation for Anesthesia Education and Research and 1K08AG043548 from the National Institute on Aging (Dr Neuman) and by grant 1260782 the from the National Science Foundation, (Dr Rosenbaum).
Role of the Sponsors: Sponsors had no role in the design or conduct of the study, the collection, management, analysis, or interpretation of data, the preparation, review, or approval of the manuscript, or the decision to submit the manuscript for publication.
Footnotes
Author Contributions: Dr Neuman had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Neuman, Rosenbaum, Zubizarreta, Silber.
Acquisition, analysis, or interpretation of data: Neuman, Rosenbaum, Ludwig, Silber.
Drafting of the manuscript: Neuman, Rosenbaum. Critical revision of the manuscript for important intellectual content: Neuman, Rosenbaum, Ludwig, Zubizarreta, Silber.
Statistical analysis: Neuman, Rosenbaum, Ludwig, Zubizarreta, Silber.
Obtained funding: Neuman.
Administrative, technical, or material support: Neuman.
Study supervision: Neuman.
Conflict of Interest Disclosures: All authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest and none were reported.
Additional Contributions: Maps were created by Jolan Falk, BS, Creative Force, which was paid for his work.
REFERENCES
- 1.Blackman DK, Kamimoto LA, Smith SM. Overview: surveillance for selected public health indicators affecting older adults—United States. MMWR CDC Surveill Summ. 1999;48(8):1–6. [PubMed] [Google Scholar]
- 2.Brauer CA, Coca-Perraillon M, Cutler DM, Rosen AB. Incidence and mortality of hip fractures in the United States. JAMA. 2009;302(14):1573–1579. doi: 10.1001/jama.2009.1462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Magaziner J, Hawkes W, Hebel JR, et al. Recovery from hip fracture in eight areas of function. J Gerontol A Biol Sci Med Sci. 2000;55(9):M498–M507. doi: 10.1093/gerona/55.9.m498. [DOI] [PubMed] [Google Scholar]
- 4.Parker MJ, Handoll HH, Griffiths R. Anaesthesia for hip fracture surgery in adults. Cochrane Database Syst Rev. 2004;(4):CD000521. doi: 10.1002/14651858.CD000521.pub2. [DOI] [PubMed] [Google Scholar]
- 5.UK National Clinical Guideline Centre . The Management of Hip Fracture in Adults. UK National Clinical Guideline Centre; London, England: 2011. [Google Scholar]
- 6.O’Hara DA, Duff A, Berlin JA, et al. The effect of anesthetic technique on postoperative outcomes in hip fracture repair. Anesthesiology. 2000;92(4):947–957. doi: 10.1097/00000542-200004000-00011. [DOI] [PubMed] [Google Scholar]
- 7.Griffiths R, Alper J, Beckingsale A, et al. Association of Anaesthetists of Great Britain and Ireland Management of proximal femoral fractures 2011: Association of Anaesthetists of Great Britain and Ireland. Anaesthesia. 2012;67(1):85–98. doi: 10.1111/j.1365-2044.2011.06957.x. [DOI] [PubMed] [Google Scholar]
- 8.Boulton C, Currie C, Griffiths R, et al. National Hip Fracture Database: Anaesthesia Sprint Audit of Practice. Royal College of Physicians; London, England: 2014. [Google Scholar]
- 9.Scottish Intercollegiate Guidelines Network . Management of Hip Fracture in Older People. Scottish Intercollegiate Guideline Network; Edinburgh, Scottland: 2009. [Google Scholar]
- 10.Radcliff TA, Henderson WG, Stoner TJ, Khuri SF, Dohm M, Hutt E. Patient risk factors, operative care, and outcomes among older community-dwelling male veterans with hip fracture. J Bone Joint Surg Am. 2008;90(1):34–42. doi: 10.2106/JBJS.G.00065. [DOI] [PubMed] [Google Scholar]
- 11.Neuman MD, Silber JH, Elkassabany NM, Ludwig JM, Fleisher LA. Comparative effectiveness of regional versus general anesthesia for hip fracture surgery in adults. Anesthesiology. 2012;117(1):72–92. doi: 10.1097/ALN.0b013e3182545e7c. [DOI] [PubMed] [Google Scholar]
- 12.Regan EA, Radcliff TA, Henderson WG, et al. Improving hip fractures outcomes for COPD patients. COPD. 2013;10(1):11–19. doi: 10.3109/15412555.2012.723072. [DOI] [PubMed] [Google Scholar]
- 13.White SM, Moppett IK, Griffiths R. Outcome by mode of anaesthesia for hip fracture surgery. An observational audit of 65 535 patients in a national dataset. Anaesthesia. 2014;69(3):224–230. doi: 10.1111/anae.12542. [DOI] [PubMed] [Google Scholar]
- 14.Horlocker TT, Wedel DJ, Rowlingson JC, et al. Regional anesthesia in the patient receiving antithrombotic or thrombolytic therapy: American Society of Regional Anesthesia and Pain Medicine Evidence-Based Guidelines (Third Edition) Reg Anesth Pain Med. 2010;35(1):64–101. doi: 10.1097/aap.0b013e3181c15c70. [DOI] [PubMed] [Google Scholar]
- 15.Sheffield KM, Riall TS, Han Y, Kuo YF, Townsend CM, Jr, Goodwin JS. Association between cholecystectomy with vs without intraoperative cholangiography and risk of common duct injury. JAMA. 2013;310(8):812–820. doi: 10.1001/jama.2013.276205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36(1):8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 17.Silber JH, Romano PS, Rosen AK, Wang Y, Even-Shoshan O, Volpp KG. Failure-to-rescue: comparing definitions to measure quality of care. Med Care. 2007;45(10):918–925. doi: 10.1097/MLR.0b013e31812e01cc. [DOI] [PubMed] [Google Scholar]
- 18.Neuman MD, Fleisher LA, Even-Shoshan O, Mi L, Silber JH. Nonoperative care for hip fracture in the elderly: the influence of race, income, and comorbidities. Med Care. 2010;48(4):314–320. doi: 10.1097/mlr.0b013e3181ca4126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Polsky D, Jha AK, Lave J, et al. Short- and long-term mortality after an acute illness for elderly whites and blacks. Health Serv Res. 2008;43(4):1388–1402. doi: 10.1111/j.1475-6773.2008.00837.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Baiocchi M, Small DS, Lorch S, Rosenbaum PR. Building a stronger instrument in an observational study of perinatal care for premature infants. J Am Stat Assoc. 2010;105(492):1285–1296. [Google Scholar]
- 21.Baiocchi M, Small DS, Yang L, Polsky D, Groeneveld PW. Near/far matching: a study design approach to instrumental variables. Health Serv Outcomes Res Methodol. 2012;12:237–253. doi: 10.1007/s10742-012-0091-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lorch SA, Baiocchi M, Ahlberg CE, Small DS. The differential impact of delivery hospital on the outcomes of premature infants. Pediatrics. 2012;130(2):270–278. doi: 10.1542/peds.2011-2820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Angrist JD, Imbens GW, Rubin DB. Identification of causal effects using instrumental variables. J Am Stat Assoc. 1996;91(434):444–455. [Google Scholar]
- 24.Rosenbaum PR, Ross RN, Silber JH. Minimum distance matched sampling with fine balance in an observational study of treatment for ovarian cancer. J Am Stat Assoc. 2007;102(477):75–83. [Google Scholar]
- 25.Mahalanobis P. On the generalised distance in statistics. Proc Nat Inst Sci India. 1936;2(1):49–55. [Google Scholar]
- 26.Rubin DB. Bias reduction using mahalanobis-metric matching. Biometrics. 1980;36(2):293–298. [Google Scholar]
- 27.Rosenbaum PR. Optimal matching of an optimally chosen subset in observational studies. J Comput Graph Stat. 2012;21(1):57–71. [Google Scholar]
- 28.Small DS, Rosenbaum PR. War and wages: the strength of instrumental variables and their sensitivity to unobserved biases. J Am Stat Assoc. 2008;103(483):924–933. [Google Scholar]
- 29.Silber JH, Rosenbaum PR, Trudeau ME, et al. Multivariate matching and bias reduction in the surgical outcomes study. Med Care. 2001;39(10):1048–1064. doi: 10.1097/00005650-200110000-00003. [DOI] [PubMed] [Google Scholar]
- 30.Rosenbaum PR, Rubin DB. Constructing a control-group using multivariate matched sampling methods that incorporate the propensity score. Am Stat. 1985;39(1):33–38. [Google Scholar]
- 31.Cochran WG, Rubin DB. Controlling bias in observational studies. Sankhya-Indian J Stat Ser A. 1973 Dec;35:417–446. [Google Scholar]
- 32.Rosenbaum PR. Design of Observational Studies. Springer; New York, NY: 2010. [Google Scholar]
- 33.Rubin DB. The design versus the analysis of observational studies for causal effects: parallels with the design of randomized trials. Stat Med. 2007;26(1):20–36. doi: 10.1002/sim.2739. [DOI] [PubMed] [Google Scholar]
- 34.Huber PJ. Robust Statistics. John Wiley; New York, NY: 1981. [Google Scholar]
- 35.Huber PJ. Robust estimation of location parameter. Ann Math Stat. 1964;35(1):73–101. [Google Scholar]
- 36.Maritz JS. Distribution-Free Statistical Methods. Chapman & Hall; London, England: 1995. [Google Scholar]
- 37.Imbens GW, Rosenbaum PR. Robust, accurate confidence intervals with a weak instrument: quarter of birth and education. J R Stat Soc Ser A Stat Soc. 2005;168:109–126. [Google Scholar]
- 38.Rosenbaum PR. Sensitivity analysis for M-estimates, tests, and confidence intervals in matched observational studies. Biometrics. 2007;63(2):456–464. doi: 10.1111/j.1541-0420.2006.00717.x. [DOI] [PubMed] [Google Scholar]
- 39.Rosenbaum PR, Silber JH. Amplification of sensitivity analysis in matched observational studies. J Am Stat Assoc. 2009;104(488):1398–1405. doi: 10.1198/jasa.2009.tm08470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zubizarreta JR. Using mixed integer programming for matching in an observational study of kidney failure after surgery. J Am Stat Assoc. 2012;107(500):1360–1371. [Google Scholar]
- 41.Berggren D, Gustafson Y, Eriksson B, et al. Postoperative confusion after anesthesia in elderly patients with femoral neck fractures. Anesth Analg. 1987;66(6):497–504. [PubMed] [Google Scholar]
- 42.Valentin N, Lomholt B, Jensen JS, Hejgaard N, Kreiner S. Spinal or general anaesthesia for surgery of the fractured hip? a prospective study of mortality in 578 patients. Br J Anaesth. 1986;58(3):284–291. doi: 10.1093/bja/58.3.284. [DOI] [PubMed] [Google Scholar]
- 43.Davis FM, McDermott E, Hickton C, et al. Influence of spinal and general anaesthesia on haemostasis during total hip arthroplasty. Br J Anaesth. 1987;59(5):561–571. doi: 10.1093/bja/59.5.561. [DOI] [PubMed] [Google Scholar]
- 44.Scheinin H, Virtanen T, Kentala E, et al. Epidural infusion of bupivacaine and fentanyl reduces perioperative myocardial ischaemia in elderly patients with hip fracture—a randomized controlled trial. Acta Anaesthesiol Scand. 2000;44(9):1061–1070. doi: 10.1034/j.1399-6576.2000.440905.x. [DOI] [PubMed] [Google Scholar]
- 45.Sieber FE, Zakriya KJ, Gottschalk A, et al. Sedation depth during spinal anesthesia and the development of postoperative delirium in elderly patients undergoing hip fracture repair. Mayo Clin Proc. 2010;85(1):18–26. doi: 10.4065/mcp.2009.0469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lee HB, Mears SC, Rosenberg PB, Leoutsakos JM, Gottschalk A, Sieber FE. Predisposing factors for postoperative delirium after hip fracture repair in individuals with and without dementia. J Am Geriatr Soc. 2011;59(12):2306–2313. doi: 10.1111/j.1532-5415.2011.03725.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Foss NB, Kristensen MT, Kristensen BB, Jensen PS, Kehlet H. Effect of postoperative epidural analgesia on rehabilitation and pain after hip fracture surgery: a randomized, double-blind, placebo-controlled trial. Anesthesiology. 2005;102(6):1197–1204. doi: 10.1097/00000542-200506000-00020. [DOI] [PubMed] [Google Scholar]
- 48.Sieber FE, Gottshalk A, Zakriya KJ, Mears SC, Lee H. General anesthesia occurs frequently in elderly patients during propofol-based sedation and spinal anesthesia. J Clin Anesth. 2010;22(3):179–183. doi: 10.1016/j.jclinane.2009.06.005. [DOI] [PubMed] [Google Scholar]
- 49.White SM, Griffiths R, Holloway J, Shannon A. Anaesthesia for proximal femoral fracture in the UK: first report from the NHS Hip Fracture Anaesthesia Network. Anaesthesia. 2010;65(3):243–248. doi: 10.1111/j.1365-2044.2009.06208.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.