Abstract
In humans, ingested inorganic arsenic is metabolized to monomethylarsenic (MMA) then to dimethylarsenic (DMA), although this process is not complete in most people. The trivalent form of MMA is highly toxic in vitro and previous studies have identified associations between the proportion of urinary arsenic as MMA (%MMA) and several arsenic-related diseases. To date, however, relatively little is known about its role in lung cancer, the most common cause of arsenic-related death, or about its impacts on people drinking water with lower arsenic concentrations (e.g., <200 μg/L). In this study, urinary arsenic metabolites were measured in 94 lung and 117 bladder cancer cases and 347 population-based controls from areas in northern Chile with a wide range of drinking water arsenic concentrations. Lung cancer odds ratios adjusted for age, sex, and smoking by increasing tertiles of %MMA were 1.00, 1.91 (95% confidence interval (CI), 0.99–3.67), and 3.26 (1.76–6.04) (p-trend <0.001). Corresponding odds ratios for bladder cancer were 1.00, 1.81 (1.06–3.11), and 2.02 (1.15–3.54) (p-trend <0.001). In analyses confined to subjects only with arsenic water concentrations <200 μg/L (median=60 μg/L), lung and bladder cancer odds ratios for subjects in the upper tertile of %MMA compared to subjects in the lower two tertiles were 2.48 (1.08–5.68) and 2.37 (1.01–5.57), respectively. Overall, these findings provide evidence that inter-individual differences in arsenic metabolism may be an important risk factor for arsenic-related lung cancer, and may play a role in cancer risks among people exposed to relatively low arsenic water concentrations.
Keywords: Arsenic, cancer, methylation, lung, bladder, water
INTRODUCTION
Millions of people worldwide are exposed to arsenic in their drinking water (Nordstrom 2002), and ingested arsenic is an established cause of bladder, lung, and skin cancer (IARC 2012; IARC. 2004). In addition to cancer, arsenic in water has also been associated with cardiovascular disease, skin lesions, diabetes, reproductive disorders, cognitive deficits in children, and other health effects (Naujokas et al. 2013; NRC 1999). The cancer risks from arsenic in drinking water may be high. The National Research Council (NRC) has estimated that the excess cancer risk associated with lifetime exposures to arsenic at the US regulatory drinking water standard of 10 μg/L may be close to 1 in 300 (NRC 2001). This is about 30 to 300 times higher than the cancer risks estimated for exposure to all other known drinking water carcinogens at concentrations equal to their current US regulatory standards (Smith et al. 2002). Risks may be even higher in susceptible groups, and marked variation in susceptibility to arsenic-related disease appears to exist (Smith and Steinmaus 2009). Importantly, these risks are estimated based on extrapolations from studies where many people had arsenic water concentrations well above 200 μg/L. As such, the true cancer risks and the impacts of various susceptibility factors at arsenic water concentrations <200 μg/L are mostly unknown (Celik et al. 2008; Gibb et al. 2011). This is important, since many people in the US and worldwide have arsenic in their water at these lower concentrations.
The primary metabolic pathway of ingested inorganic arsenic (iAs) in humans is methylation (Vahter 2002). Once ingested, iAs is methylated to monomethylarsonic acid (MMA5), which is reduced to monomethylarsonous acid (MMA3). MMA3 is then methylated to dimethylarsinic acid (DMA5), a small amount of which is then reduced to dimethylarsinous acid (DMA3). In humans, this process is not complete, and some arsenic remains as iAs and MMA (MMA3 and MMA5) (Hopenhayn-Rich et al. 1993). Almost all ingested arsenic is excreted through the urine and the relative distribution of arsenic metabolites in urine is commonly used as a biomarker of how well an individual can fully methylate ingested iAs (NRC 1999). Typically, ingested iAs is excreted as 10–20% iAs, 10–15% MMA, and 60–75% DMA. However, large inter-individual variations exist.
In the past, methylation of iAs was thought to be primarily a detoxification pathway since the methylated species most commonly found in human urine, MMA5 and DMA5, are more water soluble, more readily excreted, and less acutely toxic than iAs (Gebel 2002). However, MMA3 is much more toxic in vitro than its pentavalent form, and may be more toxic than iAs (Mass et al. 2001; Styblo et al. 2002). MMA3 is highly unstable and rapidly oxidized to MMA5 in urine, and is therefore extremely difficult to measure in field studies (Kalman et al. 2013). However, epidemiological studies have reported associations between the proportion of total MMA (MMA3 plus MMA5) in urine (%MMA), and the risks of several arsenic-related diseases including bladder cancer, skin cancer, and arsenic-caused skin lesions (Smith and Steinmaus 2009). As a whole, these studies provide a highly consistent body of evidence linking methylation capacity and %MMA to arsenic-related disease risks. Currently, however, relatively little data is available for lung cancer. This is important since lung cancer is the number one cause of arsenic-related death (Smith et al. 1998).
In this study, we investigated the association between arsenic methylation capacity and lung and bladder cancer by collecting detailed information of past arsenic exposure and potential confounders like smoking and occupation, and measuring urinary arsenic metabolites in 94 lung and 117 bladder cancer cases, and 347 population-based controls from regions in northern Chile with a wide range of arsenic drinking water concentrations. Because of its dry climate, small number of individual water sources, and availability of historic arsenic water concentration records for all cities and towns with many dating back 50 years or more, this area offers one of the best areas in the world to investigate the long-term health effects of arsenic exposure. Using the same subjects that are used in the analyses presented here, we recently reported major increases in both bladder and lung cancer related to arsenic water concentrations in this area, although data on methylation were not reported (Steinmaus et al. 2013).
METHODS
The participants of this study were a subgroup of subjects from a recently completed case-control study of arsenic and cancer, and detailed methods are provided elsewhere (Steinmaus et al. 2013). Briefly, the study area comprised two contiguous regions (Regions I, II) in northern Chile with a total population of 922,579 (Instituto Nacional de Estadisticas 2012). These regions include cities with a wide range of arsenic water concentrations but with similar socio-demographic characteristics (Smith et al. 2012). The cancer cases in the original study included all people who: 1. Had primary lung or bladder cancer first diagnosed between October 2007 and December 2010; 2. Lived in the study area at the time of diagnosis; 3. Were over age 25 years at the time of diagnosis; and 4. Were able to provide interview data or had a close relative who could. Cases were ascertained from all pathologists, hospitals, and radiologists in the study area. Relatively few long-term residents leave the study area for all of their medical care, since the nearest large medical facilities are in Santiago, 675 miles away. Most cases were histologically confirmed (98% for bladder cancer and 72% for lung cancer), with the remaining diagnoses based on a combination of radiologic (computed tomography) and physician’s clinical findings. Controls, frequency matched to cases by sex and five-year age groups, were randomly selected from computerized voter registration lists for the study area. These lists contained >95% of people over age 50 years compared to the Chile national census. For the methylation portion of the study, subjects had to be alive at the time of the interview and able to provide a urine sample. This study was approved by ethical review boards in the US and Chile, and informed consent was obtained from all participants.
All participants were interviewed using a standardized questionnaire. Participants were asked to provide all residences lived in ≥6 months, all jobs held ≥6 months, and information on specific exposure to agents linked to lung and bladder cancer, including asbestos, silica, and other workplace carcinogens. Questions regarding tobacco covered age when smoking began, periods quit, total years smoked, packs smoked per week, as well as secondhand smoke exposure as a child and adult. Questions regarding body-mass index included height and typical weight currently, 20, and 40 years ago. Subjects were also asked about all medical conditions and medications. Subjects were asked their typical drinking water intake currently, 20, and 40 years ago, including tap water used for coffee and tea. However, because the range in arsenic water concentrations in the study area (<10 to >800 μg/L) was much greater than the range in drinking water intakes, drinking water intake data had little impact on categorizing exposure so were not used in the analyses presented here.
Lifetime arsenic exposure in water was assessed as follows: For each subject, each city or town of residence was linked to a water arsenic measurement so that an arsenic concentration could be assigned to each year of the subject’s life. These yearly concentrations were then used to develop several metrics of exposure, including lifetime maximum, lifetime average, highest average for any contiguous five-year period, and cumulative exposure (calculated by summing the yearly averages). Exposure metrics using various lag periods (e.g., 5, 20, and 40 year lags) were also assessed. Arsenic water measurements from government agencies, research studies, and other sources were available for >97% of the study area and >90% of all subject residences. Until recently, few people drank bottled water or used water filters, and few people obtained water from a private well. Water arsenic concentrations were also available for all large cities in Chile outside the study area, and these were also linked to residences, although almost all involved arsenic concentrations <10 μg/L. Residences for which water records were not available were all in areas not known to have high arsenic levels, so were assigned a value of zero.
A single first morning urine sample was collected from each subject by study personnel during home visits. A previous study has shown that a moderately strong correlation exists between arsenic concentrations in single first morning samples and samples collected over 24 hours (Calderon et al. 1999). Urine samples were kept frozen in field laboratories at −20° C for 2–4 weeks, then transported to the main study office in Chile for longer-term storage at −80° C. Most samples were stored frozen for one to four months before analysis. Samples were then transported on dry ice to the University of Washington, Seattle, where urinary concentrations of iAs and its metabolites were measured using high performance liquid chromatography and inductively-coupled mass spectrometry (HPLC-ICP/MS). Urinary metabolites were measured in the first 558 subjects from the original study that provided urine. Quantitation limits were: MMA3, 0.5 μg/L; iAs3, 1 μg/L; DMA5, 5 μg/L; MMA5, 1 μg/L; iAs5, 2.5 μg/L; total arsenic, 1 μg/L; and arsenobetaine, 1 μg/L. Further details of the laboratory methods are described elsewhere (Kalman, Dills 2013). We attempted to measure MMA3 in all samples using the methods described previously (Kalman et al. 2013). However, MMA3 was only found in a few subjects’ urine, despite continual low temperature and other measures meant to prevent or minimize oxidation of this inherently unstable metabolite. For this reason, our data analyses focused on total MMA (MMA3 + MMA5).
The proportion of arsenic in each species in urine (%iAs, %MMA, and %DMA) was calculated by dividing the concentration of arsenic in each species by the sum of the concentrations of iAs, MMA, and DMA. Because MMA3 appears to be highly toxic in vitro and because previous studies have linked %MMA to risks of other arsenic-related diseases, the focus of our analyses was on %MMA, although results for %iAs and %DMA are also presented. Lung and bladder cancer odds ratios (OR) for various categories of %iAs, %MMA, and %DMA were calculated using unconditional logistic regression. In order to more readily compare our results to those of other studies, subjects in the upper tertile of %MMA or %iAs were initially compared to subjects in the lower two tertiles combined, although ORs for each tertile individually and for %MMA as a continuous variable are also presented. Variables entered into logistic regression models included sex, age (as a continuous variable), and smoking (highest cigarettes per week) (Lubin et al. 2007). Entering other variables such as mining work, current body-mass index (BMI) (above or below 30 kg/m2), secondhand smoke exposure, and tertiles of socioeconomic status (SES) scores, or entering smoking as pack-years, BMI as a continuous variable, or BMI from 20 or 40 years ago had little impact on results. Adjusting for arsenic water concentrations (entered as either average, highest, or cumulative exposure) also had little impact on results. In order to evaluate the effects of arsenic metabolism in subjects exposed to lower arsenic water concentrations, analyses were stratified by the subjects highest five-year contiguous average arsenic water concentration, excluding the five years before cancer diagnosis (cases) or interview (controls). A cut-off point of 200 μg/L was chosen for this stratification since this divided the subjects into two approximately equal sized groups. All data analyses were done using STATA statistical software program (version 12.1, STATACorp LP, College Station, TX). All p-values are two-tailed.
RESULTS
For this study, 94 lung cancer cases, 117 bladder cancer cases, and 347 control subjects were selected from the 937 living subjects in the original case-control study. Participants in the methylation portion of the study were similar to non-participants in terms of age, gender distribution, SES, smoking, lifetime average arsenic concentration in water, and other factors (Table 1S). Table 1 shows the socio-demographic characteristics and arsenic exposure information of the lung and bladder cancer cases and controls in this study. Cases tended to be smokers (the percentages of ever-smokers among controls, bladder, and lung cancer cases were 64, 79, and 81%, respectively) and have higher arsenic exposures than controls (the percentages of subjects with highest 5-year average arsenic water concentrations >200 μg/L among controls, bladder, and lung cancer cases was 16, 38, and 38%, respectively). Controls tended to be older than bladder and lung cancer cases (38, 32, and 28% over age 70 years, respectively), were more likely to be of non-European descent (27, 10, and 13% non-European descent, respectively), and were more likely to be women than bladder cancer cases (31 and 21%, respectively).
Table 1.
Socio-demographic characteristics of lung and bladder cancer cases and controls.
| Lung cancer
|
Bladder cancer
|
Controls
|
||||
|---|---|---|---|---|---|---|
| No. | % | No. | % | No. | % | |
| Total | 94 | 100 | 117 | 100 | 347 | 100 |
| Age (years) | ||||||
| <60 | 29 | 31 | 36 | 31 | 101 | 29 |
| 60–70 | 39 | 41 | 43 | 37 | 116 | 33 |
| >70 | 26 | 28 | 38 | 32 | 130 | 38 |
| Race | ||||||
| European | 82 | 87 | 105 | 90 | 253 | 73 |
| Other | 12 | 13 | 12 | 10 | 94 | 27 |
| Gender | ||||||
| Female | 29 | 31 | 24 | 21 | 109 | 31 |
| Male | 65 | 69 | 93 | 79 | 238 | 69 |
| Obesitya | ||||||
| Yes | 9 | 10 | 18 | 15 | 68 | 20 |
| No | 85 | 90 | 99 | 85 | 279 | 80 |
| Socioeconomic status | ||||||
| Low | 35 | 37 | 32 | 27 | 121 | 35 |
| High | 59 | 63 | 85 | 73 | 226 | 65 |
| Smoking | ||||||
| Ever | 76 | 81 | 92 | 79 | 222 | 64 |
| Never | 18 | 19 | 25 | 21 | 125 | 36 |
| Secondhand tobacco smokeb | ||||||
| Yes | 59 | 63 | 77 | 66 | 185 | 53 |
| No | 35 | 37 | 40 | 34 | 162 | 47 |
| Drinking water arsenic (μg/L)c | ||||||
| ≤10 | 11 | 12 | 10 | 9 | 56 | 16 |
| 10.1–200 | 47 | 50 | 62 | 53 | 235 | 68 |
| >200 | 36 | 38 | 45 | 38 | 56 | 16 |
Defined as a body mass index ≥30 kg/m2.
Includes self-reported exposure > 6 months as a child or adult.
Highest contiguous five-year average arsenic concentration in drinking water over a subject’s lifetime, excluding the five years before cancer diagnosis or interview.
The mean proportions of each arsenic species stratified by case status, gender, smoking, age, and urinary arsenic concentration are shown in Table 2 (all subjects) and Table 7S (controls only). In all subjects, mean %MMA values were higher in lung and bladder cancer cases than in controls. The mean %MMA in controls, lung, and bladder cancer cases were 10.2, 12.6, and 11.2%, respectively (p-values <0.05). The mean %MMA for men and women were 11.2 and 9.8%, respectively (p=0.001). A small correlation was seen between total urinary arsenic concentration (the sum of iAs, MMA, and DMA) and %iAs (R=0.10, p=0.02), but not %MMA or %DMA and not in analyses restricted to controls (Table 7S).
Table 2.
Mean proportions (standard deviations) of each arsenic species.
| Variable | N | % | %iAs | %MMA | %DMA |
|---|---|---|---|---|---|
| All | 558 | 100 | 9.6 (6.3) | 10.8 (4.8) | 80.0 (8.3) |
| Cancer status | |||||
| Controls | 347 | 62 | 10.4 (6.6) | 10.2 (4.3) | 79.4 (8.4) |
| Lung cancera | 94 | 17 | 10.0 (5.9) | 12.6 (5.4) | 77.4 (8.6) |
| p=0.58 | p<0.001 | p=0.05 | |||
| Bladder cancera | 117 | 21 | 6.9 (5.0) | 11.2 (5.3) | 81.9 (7.3) |
| p<0.001 | p=0.04 | p=0.005 | |||
| Genderb | |||||
| Women | 162 | 31 | 9.0 (5.9) | 9.8 (4.5) | 81.2 (7.9) |
| Men | 396 | 69 | 9.8 (6.5) | 11.2 (4.8) | 78.9 (8.4) |
| p=0.18 | p=0.001 | p=0.004 | |||
| Smokingb | |||||
| Ever | 390 | 70 | 9.3 (6.1) | 11.1 (4.9) | 79.5 (8.3) |
| Never | 168 | 30 | 10.1 (6.9) | 10.1 (4.6) | 79.8 (8.5) |
| p=0.19 | p=0.02 | p=0.75 | |||
| Age (years)c | |||||
| <60 | 166 | 32 | 10.8 (6.1) | 10.3 (4.5) | 78.9 (8.1) |
| 60–70 | 198 | 35 | 8.9 (6.4) | 11.0 (5.2) | 80.1 (8.9) |
| >70 | 194 | 33 | 9.2 (6.4) | 11.1 (4.6) | 79.7 (8.0) |
| R = − 0.15 | R=0.08 | R=0.05 | |||
| p< 0 .001 | p=0.08 | p=0.16 | |||
| Urinary arsenicc,d | |||||
| Low tertile | 183 | 33 | 8.9 (6.7) | 11.0 (4.9) | 80.2 (8.2) |
| Medium tertile | 191 | 34 | 9.9 (5.9) | 11.0 (4.7) | 79.1 (8.1) |
| High tertile | 184 | 33 | 9.9 (6.4) | 10.5 (4.8) | 79.6 (8.8) |
| R=0.10 | R=−0.05 | R=−0.02 | |||
| p=0.02 | p=0.20 | p=0.61 |
p-values comparing cancer cases to controls calculated using the Wilcoxon rank-sum test.
p-values comparing men to women or ever to never smokers calculated using the Wilcoxon rank-sum test.
Spearman correlation coefficients (R) and their p-values.
Sum of urinary concentrations of iAs, MMA, and DMA. The tertile cutoff points are 14.5 and 28.5 μg/L.
Tables 3 and 4 display the unadjusted and adjusted ORs for the association between lung and bladder cancer and urinary %MMA. The lung cancer OR adjusted for age, gender, and smoking for subjects with a %MMA in the upper tertile compared to subjects in the lower two tertiles was 2.32 (95% confidence interval (CI), 1.42–3.77, p<0.001). For bladder cancer, the corresponding OR was 1.41 (95% CI, 0.89–2.23, p=0.14). With additional adjustment for arsenic water concentrations (highest five-year contiguous average) these ORs were 2.32 (95% CI, 1.40–3.87) for lung cancer and 1.53 (95% CI, 0.94–2.49) for bladder cancer (not shown in tables). In analyses stratified by sex and smoking, ORs are somewhat higher in females than males and never-smokers than ever-smokers, although the differences were not statistically significant (Figure 1).
Table 3.
Lung cancer odds ratios (OR) for low and high levels of %MMA.a
| Cases | Controls | Crude
|
Adjustedb
|
|||
|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | |||
| All subjects | ||||||
| %MMA < 12.5% | 49 | 251 | 1.00 | Ref | 1.00 | Ref |
| %MMA ≥ 12.5% | 45 | 96 | 2.40 | 1.46–3.93 | 2.32 | 1.42–3.77 |
| Water arsenic < 200 μg/Lc | ||||||
| %MMA < 12.5% | 14 | 138 | 1.00 | Ref | 1.00 | Ref |
| %MMA ≥ 12.5% | 14 | 52 | 2.65 | 1.18–5.94 | 2.48 | 1.08–5.68 |
| Water arsenic ≥ 200 μg/Lc,d | ||||||
| %MMA < 12.5% | 35 | 113 | 3.05 | 1.56–5.95 | 3.16 | 1.59–6.32 |
| %MMA ≥ 12.5% | 31 | 44 | 6.94 | 3.39–14.22 | 6.81 | 3.24–14.31 |
A %MMA of 12.5% divides the upper from the two lower tertiles.
Odds ratios adjusted for age, gender, and smoking.
Highest contiguous five-year average arsenic water concentration, excluding the five years before cancer diagnosis or interview.
Subjects with arsenic water concentrations < 200 μg/L and %MMA < 12.5% are used as the reference group to calculate these ORs.
Abbreviations: CI, confidence interval; OR, odds ratio; Ref, reference group; %MMA, the proportion of inorganic arsenic excreted in urine as MMA.
Table 4.
Bladder cancer odds ratios (OR) for low and high levels of %MMA.a
| Cases | Controls | Crude
|
Adjustedb
|
|||
|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | |||
| All subjects | ||||||
| %MMA < 12.5% | 75 | 251 | 1.00 | Ref | 1.00 | Ref |
| %MMA ≥ 12.5% | 42 | 96 | 1.46 | 0.91–2.33 | 1.41 | 0.89–2.23 |
| Water arsenic < 200 μg/Lc | ||||||
| %MMA < 12.5% | 14 | 138 | 1.00 | Ref | 1.00 | Ref |
| %MMA ≥ 12.5% | 13 | 52 | 2.46 | 1.09–5.59 | 2.37 | 1.01–5.57 |
| Water arsenic ≥ 200 μg/Lc,d | ||||||
| %MMA < 12.5% | 61 | 113 | 5.32 | 2.82–10.01 | 6.42 | 3.29–12.53 |
| %MMA ≥ 12.5% | 29 | 44 | 6.50 | 3.15–13.38 | 6.96 | 3.27–14.79 |
A %MMA of 12.5% divides the upper from the two lower tertiles.
Odds ratios adjusted for age, gender, and smoking.
Highest contiguous five-year average arsenic water concentration, excluding the five years before cancer diagnosis or interview.
Subjects with arsenic water concentrations < 200 μg/L and %MMA < 12.5% are used as the reference group to calculate these ORs.
Abbreviations: CI, confidence interval; OR, odds ratio; Ref, reference group; %MMA, the proportion of inorganic arsenic excreted in urine as MMA.
Figure 1.
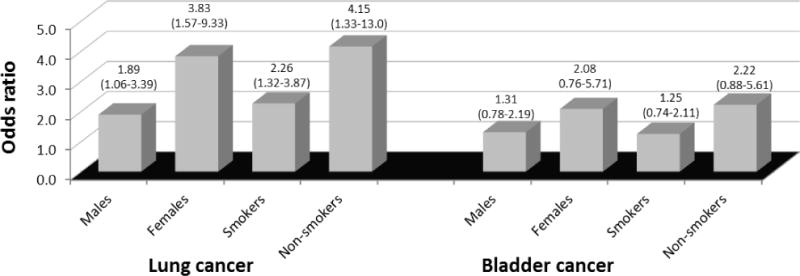
Lung and bladder cancer odds ratios (OR) for low and high levels of %MMA in analyses stratified by sex and smoking (ever-smokers vs. never smokers)a
aCancer odd ratios comparing subjects with %MMA levels in the upper tertile (≥ 12.5%) to subjects in the lower two tertiles.
Tables 3 and 4 also show the lung and bladder cancer ORs, comparing subjects in the upper tertile of %MMA to those in the lower two tertiles, stratified by highest 5-year average arsenic water concentrations. The reference group in these calculations were subjects who had a %MMA value in the lower two tertiles and who had a highest 5-year average arsenic drinking water concentration <200 μg/L. For lung cancer, those with a %MMA in the upper tertile and arsenic water concentrations <200 µg/L had a lung cancer OR of 2.48 (95% CI, 1.08–5.68), while those with a %MMA in the upper tertile who had arsenic water concentrations >200 µg/L had a lung cancer OR of 6.81 (95% CI, 3.24–14.31). For bladder cancer, those with a %MMA in the upper tertile and who had arsenic water concentrations <200 μg/L had an OR of 2.37 (95% CI, 1.01–5.57), while those with a %MMA in the upper tertile and who had arsenic water concentrations >200 μg/L had a bladder cancer OR of 6.96 (95% CI, 3.27–14.79). Similar results were seen in analyses stratified by highest known, lifetime average, and cumulative arsenic exposure (Tables 8S–13S). Median arsenic water concentrations in subjects in these analyses with arsenic water concentrations above and below 200 μg/L were approximately 850 and 60 μg/L, respectively (Table 2S).
Table 5 shows lung and bladder cancer ORs for each tertile of %MMA, using subjects in the lower tertile as the reference group. Evidence of dose-response patterns with increasing %MMA were seen for both cancers. The adjusted ORs for lung cancer for the middle and upper tertiles of %MMA were 1.91 (95% CI, 0.99–3.67) and 3.26 (95% CI, 1.76–6.04), respectively (Table 5) (p-trend <0.001). The corresponding ORs for bladder cancer were 1.81 (95% CI, 1.06–3.11) and 2.02 (95% CI, 1.15–3.54), respectively (p-trend <0.001). In analyses entering %MMA as a continuous variable, each one percent increase in %MMA (e.g., from 10% to 11%) was associated with an 11% (95% CI, 5–17%) and 4% (95% CI, 0–9%) increase in lung and bladder cancer ORs, respectively (Table 5).
Table 5.
Lung and bladder cancer odds ratios (ORs) by tertile of %MMA in all subjects.a
| Cases | Controls | Crude
|
Adjustedb
|
|||
|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | |||
| Lung cancer | ||||||
| Lower tertile | 20 | 134 | 1.00 | Ref | 1.00 | Ref |
| Medium tertile | 29 | 117 | 1.66 | 0.89–3.09 | 1.91 | 0.99–3.67 |
| Upper tertile | 45 | 96 | 3.14 | 1.74–5.66 | 3.26 | 1.76–6.04 |
| Continuousc | 94 | 347 | 1.11 | 1.06–1.17 | 1.11 | 1.05–1.17 |
| Bladder cancer | ||||||
| Lower tertile | 29 | 134 | 1.00 | Ref | 1.00 | Ref |
| Medium tertile | 46 | 117 | 1.82 | 1.07–3.08 | 1.81 | 1.06–3.11 |
| Upper tertile | 42 | 96 | 2.02 | 1.16–3.43 | 2.02 | 1.15–3.54 |
| Continuousc | 117 | 347 | 1.05 | 1.00–1.10 | 1.04 | 1.00–1.09 |
The upper and lower tertile cutoffs for %MMA are 12.5% and 8.5%, respectively.
Odds ratios adjusted for age, gender, and smoking.
Logistic regression entering %MMA as a continuous variable. The values given are the OR and its 95% CI for each 1% increase in %MMA.
Abbreviations: CI, confidence interval; OR, odds ratio; Ref, reference group; %MMA, the proportion of inorganic arsenic excreted in urine as MMA.
Elevated ORs remained after further adjustments for potential confounders other than sex, age, and smoking. For example, the sex, age, and smoking adjusted lung cancer OR for the upper tertile of %MMA was 2.32 (95% CI, 1.42–3.77), while the corresponding OR adjusted for age, sex, smoking, body mass index (obese vs. non-obese), SES score (lower tertile), secondhand tobacco smoke, race, and self-reported silica and asbestos exposure was 2.21 (95% CI, 1.32–3.69, p=0.002).
Analyses evaluating %iAs and %DMA are shown in Supplementary Tables 3S–6S. The bladder cancer OR for subjects with a %iAs in the upper tertile compared to subjects in the two lower tertiles was 0.27 (95% CI, 0.15–0.46). In subjects with 5-year highest average water concentrations <200 μg/L, this OR was 0.38 (95% CI, 0.15–1.02) (Table 4S). MMA3 was assessed in all samples but only above detection (>0.1 μg/L) in two lung cancer cases (mean=0.22 μg/L; standard deviation (SD)=0.41 μg/L), two bladder cancer cases (mean = 0.25 μg/L; SD=0.44 μg/L), and five controls (mean =0.19 μg/L; SD= 0.11 μg/L).
DISCUSSION
Overall, the elevated lung and bladder cancer ORs identified in subjects with higher %MMA values in this study provides evidence that people who are less effective at methylating MMA to DMA are at greater risk of arsenic-related cancer than others. In addition, the lung and bladder cancer ORs of 2.48 (1.08–5.68) and 2.37 (1.01–5.57), respectively, that we identified in subjects with %MMA in the upper tertile but with arsenic water concentrations <200 μg/L, suggests that arsenic metabolism plays an important role in susceptibility even in people exposed to lower drinking water arsenic concentrations. These latter findings are important since most previous evidence linking ingested arsenic to cancer have involved arsenic water concentrations >200 μg/L (Celik et al. 2008; Gibb et al. 2011; NRC 1999). Overall, the low p-values, the presence of dose-response relationships, and the consistency with other studies, all suggest that these findings are not due to chance and represent real associations.
Our findings are consistent with a growing body of evidence that elevations in %MMA or MMA/DMA ratio are associated with increased risks various arsenic-related diseases (Smith and Steinmaus 2009). In several studies from parts of Taiwan and Bangladesh with historic arsenic concentrations >200 μg/L, people with higher %MMA or MMA/DMA ratios have had relative risks of arsenic-caused skin lesions, skin cancer, or bladder cancer that were 2–5 times higher than people with lower levels of these factors (Ahsan et al. 2007; Huang et al. 2008; Lindberg et al. 2008; McCarty et al. 2007; Pu et al. 2007). To date, only two studies have examined arsenic metabolism and lung cancer. In a case-control study involving only 45 lung cancer cases and 75 controls from an arsenic-exposed region in Argentina, our research group identified a lung cancer OR of 3.09 (95% CI, 1.08–8.81) in subjects with %MMA in the upper tertile compared to those in the lower two tertiles (Steinmaus et al. 2010). In a prospective cohort study from an area in Taiwan with high arsenic water concentrations in the distant past, mortality hazard ratios (HR) for bladder cancer were above 1.0 in subjects with elevated %iAs (HR=3.53; 95% CI, 1.16–10.77) and %MMA (HR=1.77; 95% CI, 0.72–4.36), but HRs for lung cancer were lower (HR=0.85; 95% CI, 0.41–1.76 for %MMA ≥ 15.31% and HR=1.43; 95% CI, 0.66–3.14 for %iAs ≥ 7.86%) (Chung et al. 2013). However, the data on past arsenic exposure in this study was ecologic and limited, and clear associations between arsenic water concentrations and lung cancer were not seen (e.g., lung cancer HR = 1.04; 95% CI, 0.43–2.48 for average arsenic water concentrations ≥710 μg/L). This is different from our study in that we collected detailed individual information on lifetime exposure, and clear arsenic-lung cancer associations were identified (i.e., lung cancer OR = 4.32; 95% CI, 2.60–7.17, for arsenic water concentrations >335 μg/L) (Steinmaus et al. 2013).
Additional data supporting the biological plausibility of our findings comes from laboratory research showing that MMA3 is more acutely toxic in vitro than MMA5, DMA, and iAs (Styblo et al. 2002). These data, combined with the human data linking %MMA to arsenic-related health effects (Smith and Steinmaus 2009), provide some evidence that MMA, specifically MMA3, may be the primary toxic species of ingested inorganic arsenic. In our study, we were unable to assess the specific effects of MMA3 since it is rapidly oxidized to MMA5 and difficult to measure in field studies. This is consistent with a recent analysis of MMA3 in highly exposed children in Bangladesh, where urine MMA3 concentrations above 1 μg/L were only detected in 2 of 643 urine samples despite fairly high overall urine arsenic concentrations (mean = 80.9 μg/L; SD =134 μg/L), sample freezing at −70°C, and attempted binding with an arsenic chelating agent (Kalman et al. 2013). Because MMA3 levels were low in our study, we assessed total MMA, that is, MMA3 and MMA5 combined. It is possible that total MMA is an accurate surrogate for MMA3, and that the associations we saw with cancer for total MMA are due to MMA3. If this is the case, any inaccuracies involved in using total MMA as a surrogate for MMA3 would likely bias ORs towards the null and the true ORs may actually be higher than those found in our study. To date, the degree to which total urinary MMA may be an accurate marker of MMA3 concentrations is unknown. Regardless, the in vitro evidence showing that MMA3 is highly toxic supports our findings linking MMA to increased cancer risks.
Our lung cancer findings are also supported by the large body of evidence showing that the human lung is a major target site of arsenic. Several studies have shown that arsenic accumulates in the lungs to a greater extent than in most other organs (Marafante et al. 1981; Vahter and Marafante 1983). This could be related to the high concentration of sulfhydrl groups found in lung tissue which are known to bind arsenic (NRC 1999). Ingested arsenic is an established cause of lung cancer and many studies have also linked it to adverse non-malignant effects in the lung, including respiratory symptoms, bronchiectasis, and decrements in pulmonary function (Dauphine et al. 2011; Guha Mazumder et al. 2005; Milton and Rahman 2002; Parvez et al. 2008). With regards to the bladder, ingested arsenic is excreted in the urine through the bladder and is an established cause of bladder cancer. As a whole, these findings all provide evidence that ingested arsenic not only reaches the target organ sites we assessed but also causes toxicity there.
The ORs in our study changed relatively little after adjustments for various potential confounding factors. Residual confounding is possible but major confounding is not likely since we evaluated most of the more prevalent and important risk factors for lung and bladder cancer, including smoking and workplace exposures. Some dietary variables may be associated with both arsenic metabolism and lung cancer, but the impacts are generally small and unlikely to cause the 2–3-fold increases in risk we identified here (Cho et al. 2006; Gamble et al. 2005; Hsueh et al. 1997; C. Steinmaus et al. 2005; Steinmaus et al. 1998). In this study, and most other studies of arsenic metabolism and disease, urinary methylation patterns were assessed after disease diagnosis and assumed to be representative of subject’s past methylation patterns. Several studies have assessed changes in methylation patterns in the same individuals over time, and most suggest that these patterns remain fairly stable over time (Chen et al. 2013; Concha et al. 2002; Huang et al. 2009; Navas-Acien et al. 2009; C Steinmaus et al. 2005). In addition, evidence suggests that stable genetic factors play a more important role in determining inter-individual differences in methylation patterns than do factors that are likely to have greater day to day variability such as diet or smoking (Chung et al. 2002). Despite this, some intra-individual variability in methylation patterns likely occurs and this could lead to some misclassification of past methylation patterns. However, because we collected and analyzed metabolites from cases and controls using the same protocols, the resulting bias would most likely be non-differential and towards the null, not towards the positive associations identified. Errors in our estimates of past arsenic exposure may have also occurred. However, as discussed above, there are few water sources in the study area, almost everyone lives in one of the cities and towns, and arsenic water concentrations are available for these cities and towns for the last 40 years or more. As such, past exposures can be accurately estimated simply by knowing the cities and towns in which the subject lived, information that is likely to be recalled with fairly good accuracy.
The assessment of methylation after cancer diagnosis also raises concerns about the temporal relationship between disease and methylation capacity. That is, the effects seen in our study and in most other studies of arsenic metabolism and disease might not be due to the impact of methylation patterns on disease, but rather, due to the impact of disease or disease treatment on methylation patterns. Currently, no data are available on the impact of severe chronic non-arsenic-related diseases on arsenic metabolism. However, several of the studies linking %MMA to arsenic susceptibility involve non-melanoma skin cancer, benign skin lesions, or chromosomal aberrations (Maki-Paakkanen et al. 1998; Smith and Steinmaus 2009), none of which would be expected to have significant systemic effects on metabolism. In addition, a few prospective cohort studies have assessed urine arsenic metabolic patterns before disease diagnosis, and have reported associations between %MMA and heart disease (Chen et al. 2013) and bladder cancer (Huang et al. 2008). Overall, the consistency of our findings with these studies and other data on biologic plausibility suggest our results represent the effects of %MMA on lung cancer risks, although the possibility that lung cancer affects %MMA can not be completely ruled out. A longitudinal cohort study with accurate data on past %MMA might be better able to establish temporality, although this type of study would be incredibly difficult given the 30 to 40 year (or longer) latency of arsenic-caused cancer (Marshall et al. 2007).
In conclusion, millions of people are exposed to arsenic worldwide and these exposures may be associated with high cancer risks. Our results add to a gradually expanding body of evidence that inter-individual differences in arsenic metabolism play an important role in arsenic-related disease, including lung cancer. Our findings also add new evidence that arsenic drinking water concentrations <200 μg/L may be associated with significantly increased cancer risks, especially in people who methylate arsenic poorly. Although the design of this study prevents us from confirming the temporal relationship between %MMA and lung cancer, the biologic plausibility of our results and their consistency with a variety of other research is evidence that our findings represent a true impact of MMA on lung cancer risks. Data such as these are important in identifying susceptible subpopulations who may need specific regulatory protection. Information on the particular toxic species of ingested arsenic may also help elucidate the mechanisms of arsenic-caused disease, which are currently unknown.
Supplementary Material
Highlights.
Urine arsenic metabolites were measured in cancer cases and controls from Chile.
Higher urine %MMA values were associated with increased lung and bladder cancer.
%MMA-cancer associations were seen at drinking water arsenic levels <200 ug/L.
Acknowledgments
Funding: This work was supported by grants R01 ES014032 and P42 ES04705 from the US National Institute of Environmental Health Sciences (NIEHS).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The views expressed are those of the authors and do not necessarily represent those of the Office of Environmental Health Hazard Assessment, the California Environmental Protection Agency, or the State of California.
Conflict of Interest: The authors declare there are no conflicts of interest.
References
- Ahsan H, Chen Y, Kibriya MG, Slavkovich V, Parvez F, Jasmine F, et al. Arsenic metabolism, genetic susceptibility, and risk of premalignant skin lesions in bangladesh. Cancer Epidemiol Biomarkers Prev. 2007;16:1270–1278. doi: 10.1158/1055-9965.EPI-06-0676. [DOI] [PubMed] [Google Scholar]
- Calderon R, Hudgens E, Le XC, Schreinmachers D, Thomas DJ. Excretion of arsenic in urine as a function of exposure to arsenic in drinking water. Environ Health Perspect. 1999;107:663–667. doi: 10.1289/ehp.99107663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Celik I, Gallicchio L, Boyd K, Lam TK, Matanoski G, Tao X, et al. Arsenic in drinking water and lung cancer: A systematic review. Environmental Research. 2008;108:48–55. doi: 10.1016/j.envres.2008.04.001. [DOI] [PubMed] [Google Scholar]
- Chen Y, Wu F, Liu M, Parvez F, Slavkovich V, Eunus M, et al. A prospective study of arsenic exposure, arsenic methylation capacity, and risk of cardiovascular disease in bangladesh. Environ Health Perspect. 2013;121:832–838. doi: 10.1289/ehp.1205797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cho E, Hunter DJ, Spiegelman D, Albanes D, Beeson WL, van den Brandt PA, et al. Intakes of vitamins a, c and e and folate and multivitamins and lung cancer: A pooled analysis of 8 prospective studies. Int J Cancer. 2006;118:970–978. doi: 10.1002/ijc.21441. [DOI] [PubMed] [Google Scholar]
- Chung CJ, Huang YL, Huang YK, Wu MM, Chen SY, Hsueh YM, et al. Urinary arsenic profiles and the risks of cancer mortality: A population-based 20-year follow-up study in arseniasis-endemic areas in taiwan. Environ Res. 2013;122:25–30. doi: 10.1016/j.envres.2012.11.007. [DOI] [PubMed] [Google Scholar]
- Chung JS, Kalman DA, Moore LE, Kosnett MJ, Arroyo AP, Beeris M, et al. Family correlations of arsenic methylation patterns in children and parents exposed to high concentrations of arsenic in drinking water. Environ Health Perspect. 2002;110:729–733. doi: 10.1289/ehp.02110729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Concha G, Volger G, Nermell B, Vahter M. Intra-individual variation in the metabolism of inorganic arsenic. Int Arch Occup Environ Health. 2002;75:576–580. doi: 10.1007/s00420-002-0361-1. [DOI] [PubMed] [Google Scholar]
- Dauphine DC, Ferreccio C, Guntur S, Yuan Y, Hammond SK, Balmes J, et al. Lung function in adults following in utero and childhood exposure to arsenic in drinking water: Preliminary findings. Int Arch Occup Environ Health. 2011;84:591–600. doi: 10.1007/s00420-010-0591-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gamble MV, Liu X, Ahsan H, Pilsner R, Ilievski V, Slavkovich V, et al. Folate, homocysteine, and arsenic metabolism in arsenic-exposed individuals in bangladesh. Environ Health Perspect. 2005;113:1683–1688. doi: 10.1289/ehp.8084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gebel TW. Arsenic methylation is a process of detoxification through accelerated excretion. Int J Hyg Environ Health. 2002;205:505–508. doi: 10.1078/1438-4639-00177. [DOI] [PubMed] [Google Scholar]
- Gibb H, Haver C, Gaylor D, Ramasamy S, Lee JS, Lobdell D, et al. Utility of recent studies to assess the national research council 2001 estimates of cancer risk from ingested arsenic. Environ Health Perspect. 2011;119:284–290. doi: 10.1289/ehp.1002427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guha Mazumder DN, Steinmaus C, Bhattacharya P, von Ehrenstein OS, Ghosh N, Gotway M, et al. Bronchiectasis in persons with skin lesions resulting from arsenic in drinking water. Epidemiology. 2005;16:760–765. doi: 10.1097/01.ede.0000181637.10978.e6. [DOI] [PubMed] [Google Scholar]
- Hopenhayn-Rich C, Smith AH, Goeden HM. Human studies do not support the methylation threshold hypothesis for the toxicity of inorganic arsenic. Environ Res. 1993;60:161–177. doi: 10.1006/enrs.1993.1024. [DOI] [PubMed] [Google Scholar]
- Hsueh YM, Chiou HY, Huang YL, Wu WL, Huang CC, Yang MH, et al. Serum beta-carotene level, arsenic methylation capability, and incidence of skin cancer. Cancer Epidemiol Biomarkers Prev. 1997;6:589–596. [PubMed] [Google Scholar]
- Huang YK, Huang YL, Hsueh YM, Yang MH, Wu MM, Chen SY, et al. Arsenic exposure, urinary arsenic speciation, and the incidence of urothelial carcinoma: A twelve-year follow-up study. Cancer Causes Control. 2008;19:829–839. doi: 10.1007/s10552-008-9146-5. [DOI] [PubMed] [Google Scholar]
- Huang YK, Huang YL, Hsueh YM, Wang JT, Yang MH, Chen CJ. Changes in urinary arsenic methylation profiles in a 15-year interval after cessation of arsenic ingestion in southwest taiwan. Environ Health Perspect. 2009;117:1860–1866. doi: 10.1289/ehp.0900560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- IARC. A review of human carcinogens: Arsenic, metals, fibres, and dusts. 100c. Lyon; 2012. [Google Scholar]
- IARC. Some drinking-water disinfectants and contaminants, including arsenic. Vol. 84. Lyon; 2004. [PMC free article] [PubMed] [Google Scholar]
- Instituto Nacional de Estadisticas. Resultados preliminares del censo 2012. 2012 Available: http://www.censo.cl/
- Kalman DA, Dills RL, Steinmaus C, Yunus M, Khan AF, Prodhan MM, et al. Occurrence of trivalent monomethyl arsenic and other urinary arsenic species in a highly exposed juvenile population in bangladesh. J Expo Sci Environ Epidemiol. 2013 doi: 10.1038/jes.2013.14. [DOI] [PubMed] [Google Scholar]
- Lindberg AL, Rahman M, Persson LA, Vahter M. The risk of arsenic induced skin lesions in bangladeshi men and women is affected by arsenic metabolism and the age at first exposure. Toxicol Appl Pharmacol. 2008;230:9–16. doi: 10.1016/j.taap.2008.02.001. [DOI] [PubMed] [Google Scholar]
- Lubin JH, Caporaso N, Wichmann HE, Schaffrath-Rosario A, Alavanja MC. Cigarette smoking and lung cancer: Modeling effect modification of total exposure and intensity. Epidemiology. 2007;18:639–648. doi: 10.1097/EDE.0b013e31812717fe. [DOI] [PubMed] [Google Scholar]
- Maki-Paakkanen J, Kurttio P, Paldy A, Pekkanen J. Association between the clastogenic effect in peripheral lymphocytes and human exposure to arsenic through drinking water. Environ Mol Mutagen. 1998;32:301–313. doi: 10.1002/(sici)1098-2280(1998)32:4<301::aid-em3>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- Marafante E, Rade J, Sabbioni E. Intracellular interaction and metabolic fate of arsenite in the rabbit. Clinical Toxicol. 1981;18:1335–1341. doi: 10.3109/00099308109035074. [DOI] [PubMed] [Google Scholar]
- Marshall G, Ferreccio C, Yuan Y, Bates MN, Steinmaus C, Selvin S, et al. Fifty-year study of lung and bladder cancer mortality in chile related to arsenic in drinking water. J Natl Cancer Inst. 2007;99:920–928. doi: 10.1093/jnci/djm004. [DOI] [PubMed] [Google Scholar]
- Mass MJ, Tennant A, Roop BC, Cullen WR, Styblo M, Thomas DJ, et al. Methylated trivalent arsenic species are genotoxic. Chem Res Toxicol. 2001;14:355–361. doi: 10.1021/tx000251l. [DOI] [PubMed] [Google Scholar]
- McCarty KM, Chen YC, Quamruzzaman Q, Rahman M, Mahiuddin G, Hsueh YM, et al. Arsenic methylation, gstt1, gstm1, gstp1 polymorphisms, and skin lesions. Environ Health Perspect. 2007;115:341–345. doi: 10.1289/ehp.9152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milton AH, Rahman M. Respiratory effects and arsenic contaminated well water in bangladesh. Int J Environ Health Res. 2002;12:175–179. doi: 10.1080/09603120220129346. [DOI] [PubMed] [Google Scholar]
- Naujokas MF, Anderson B, Ahsan H, Aposhian HV, Graziano JH, Thompson C, et al. The broad scope of health effects from chronic arsenic exposure: Update on a worldwide public health problem. Environ Health Perspect. 2013;121:295–302. doi: 10.1289/ehp.1205875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Navas-Acien A, Umans JG, Howard BV, Goessler W, Francesconi KA, Crainiceanu CM, et al. Urine arsenic concentrations and species excretion patterns in american indian communities over a 10-year period: The strong heart study. Environ Health Perspect. 2009;117:1428–1433. doi: 10.1289/ehp.0800509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nordstrom DK. Public health. Worldwide occurrences of arsenic in ground water. Science. 2002;296:2143–2145. doi: 10.1126/science.1072375. [DOI] [PubMed] [Google Scholar]
- NRC. Arsenic in drinking water. Washington, DC: Subcommittee on Arsenic in Drinking Water. National Research Council; 1999. [Google Scholar]
- NRC. Arsenic in drinking water 2001 update. Washington, DC: Subcommittee to Update the 1999 Arsenic in Drinking Water Report. National Research Council; 2001. [Google Scholar]
- Parvez F, Chen Y, Brandt-Rauf PW, Bernard A, Dumont X, Slavkovich V, et al. Nonmalignant respiratory effects of chronic arsenic exposure from drinking water among never-smokers in bangladesh. Environ Health Perspect. 2008;116:190–195. doi: 10.1289/ehp.9507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pu YS, Yang SM, Huang YK, Chung CJ, Huang SK, Chiu AW, et al. Urinary arsenic profile affects the risk of urothelial carcinoma even at low arsenic exposure. Toxicol Appl Pharmacol. 2007;218:99–106. doi: 10.1016/j.taap.2006.09.021. [DOI] [PubMed] [Google Scholar]
- Smith A, Lopipero P, Bates M, Steinmaus C. Arsenic epidemiology and drinking water standards. Science. 2002;296:2145–2146. doi: 10.1126/science.1072896. [DOI] [PubMed] [Google Scholar]
- Smith AH, Goycolea M, Haque R, Biggs ML. Marked increase in bladder and lung cancer mortality in a region of northern chile due to arsenic in drinking water. Am J Epidemiol. 1998;147:660–669. doi: 10.1093/oxfordjournals.aje.a009507. [DOI] [PubMed] [Google Scholar]
- Smith AH, Steinmaus CM. Health effects of arsenic and chromium in drinking water: Recent human findings. Annu Rev Public Health. 2009;30:107–122. doi: 10.1146/annurev.publhealth.031308.100143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith AH, Marshall G, Liaw J, Yuan Y, Ferreccio C, Steinmaus C. Mortality in young adults following in utero and childhood exposure to arsenic in drinking water. Environ Health Perspect. 2012;120:1527–1531. doi: 10.1289/ehp.1104867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinmaus C, Carrigan K, Kalman D, Atallah R, Yuan Y, Smith AH. Dietary intake and arsenic methylation in a u.S. Population. Environ Health Perspect. 2005;113:1153–1159. doi: 10.1289/ehp.7907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinmaus C, Yuan Y, Kalman D, Atallah R, Smith A. Intra-individual variability in arsenic methylation in a us population. Cancer Epidemiol Biomarkers Prev. 2005;14:919–924. doi: 10.1158/1055-9965.EPI-04-0277. [DOI] [PubMed] [Google Scholar]
- Steinmaus C, Yuan Y, Kalman D, Rey OA, Skibola CF, Dauphine D, et al. Individual differences in arsenic metabolism and lung cancer in a case-control study in cordoba, argentina. Toxicol Appl Pharmacol. 2010;247:138–145. doi: 10.1016/j.taap.2010.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinmaus CM, Nunez S, Smith AH. Diet and bladder cancer: A meta-analysis of six dietary variables. Am J Epidemiol. 1998;151:693–702. doi: 10.1093/oxfordjournals.aje.a010264. [DOI] [PubMed] [Google Scholar]
- Steinmaus CM, Ferreccio C, Acevedo Romo J, Yuan Y, Cortes S, Marshall G, et al. Drinking water arsenic in northern chile: High cancer risks 40 years after exposure cessation. Cancer Epidemiol Biomarkers Prev. 2013;22:623–630. doi: 10.1158/1055-9965.EPI-12-1190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Styblo M, Drobna Z, Jaspers I, Lin S, Thomas DJ. The role of biomethylation in toxicity and carcinogenicity of arsenic: A research update. Environ Health Perspect. 2002;110(suppl 5):S767–S771. doi: 10.1289/ehp.110-1241242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vahter M, Marafante E. Intracellular interaction and metabolic fate of arsenite and arsenate in mice and rabbits. Chem Biol Interact. 1983;47:29–44. doi: 10.1016/0009-2797(83)90145-x. [DOI] [PubMed] [Google Scholar]
- Vahter M. Mechanisms of arsenic biotransformation. Toxicology. 2002;181:211–217. doi: 10.1016/s0300-483x(02)00285-8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


