Abstract
Objective
Changes in insulin sensitivity (IS) and insulin secretion occur with perturbations in energy balance and glycemic load (GL) of the diet that may precede the development of insulin resistance and hyperinsulinemia. Determinants of changes in IS and insulin secretion with weight cycling in non-obese healthy subjects remain unclear.
Methods
In a 6wk controlled 2-stage randomized dietary intervention 32 healthy men (26±4y, BMI: 24±2kg/m2) followed 1wk of overfeeding (OF), 3wks of caloric restriction (CR) containing either 50% or 65% carbohydrate (CHO) and 2wks of refeeding (RF) with the same amount of CHO but either low or high glycaemic index at ±50% energy requirement. Measures of IS (basal: HOMA-index, postprandial: Matsuda-ISI), insulin secretion (early: Stumvoll-index, total: tAUC-insulin/tAUC-glucose) and potential endocrine determinants (ghrelin, leptin, adiponectin, thyroid hormone levels, 24h-urinary catecholamine excretion) were assessed.
Results
IS improved and insulin secretion decreased due to CR and normalized upon RF. Weight loss-induced improvements in basal and postprandial IS were associated with decreases in leptin and increases in ghrelin levels, respectively (r = 0.36 and r = 0.62, p<0.05). Weight regain-induced decrease in postprandial IS correlated with increases in adiponectin, fT3, TSH, GL of the diet and a decrease in ghrelin levels (r-values between -0.40 and 0.83, p<0.05) whereas increases in early and total insulin secretion were associated with a decrease in leptin/adiponectin-ratio (r = -0.52 and r = -0.46, p<0.05) and a decrease in fT4 (r = -0.38, p<0.05 for total insulin secretion only). After controlling for GL associations between RF-induced decrease in postprandial IS and increases in fT3 and TSH levels were no longer significant.
Conclusion
Weight cycling induced changes in IS and insulin secretion were associated with changes in all measured hormones, except for catecholamine excretion. While leptin, adiponectin and ghrelin seem to be the major endocrine determinants of IS, leptin/adiponectin-ratio and fT4 levels may impact changes in insulin secretion with weight cycling.
Trial Registration
ClinicalTrials.gov NCT01737034
Introduction
Insulin resistance and hyperinsulinemia are early symptoms of metabolic dysfunction that precede the onset of type 2 diabetes. Even short-term overfeeding with modest weight gain contributes to decreased insulin sensitivity and compensatory increased insulin secretion [1,2]. Weight loss counteracts the negative consequences of a positive energy balance [3,4]; however, losses are rarely maintained, leading to recurrent weight cycling that has been associated with worsened metabolic and cardiovascular outcomes [5–7].
In addition, high glycemic index and glycemic load diets were independently associated with an increased risk of type 2 diabetes [8]. Because a diet high in rapidly absorbed carbohydrates and low in cereal fiber augments postprandial glycemia and insulin secretion it may contribute to glucotoxicity as well as increased insulin demand and eventually the development of insulin resistance.
To understand the etiology of early changes in IS and insulin secretion with perturbations in energy balance it is important to investigate healthy non-obese subjects, because a chronic disturbance in energy balance may increase visceral and liver fat and thus lead to impaired hepatic insulin clearance [9], chronic low grade inflammation [10] and elevated FFA levels [11] associated with IR and pathological hyperinsulinemia. Early determinants of changes in insulin sensitivity and insulin secretion that precede the development of ectopic fat accumulation could thus facilitate the identification of novel strategies for prevention of type 2 diabetes.
Several appetite-regulating hormones that fluctuate in response to changes in energy balance are known to potentially influence insulin levels or insulin sensitivity (e.g. leptin, ghrelin, GLP-1). Activation of proopiomelanocortin neurons by leptin has been shown to enhance insulin secretion [12] and degree of insulin resistance and β-cell function are associated with leptin in patients with Type 2 diabetes [13]. It is suggested that ghrelin has central and peripheral effects on glucose regulation and insulin level in humans [14,15] and GLP-1 has been shown to increase insulin secretion in a glucose-dependent manner [16]. However, changes in IS and insulin secretion with overfeeding and caloric restriction were accompanied by an unchanged GLP-1 response to oral glucose [4]. Moreover adiponectin [3], thyroid hormones and catecholamine excretion [17] change with body weight and might impact associated changes in IS or insulin secretion [18–20].
Early determinants of changes in IS and insulin secretion with weight loss and regain using different glycemic loads of the diet remain unclear. In a controlled dietary intervention, we therefore investigated the associations between changes in basal and OGTT-derived IS or insulin secretion with levels of ghrelin, leptin, adiponectin, thyroid hormones and catecholamine excretion during a weight cycle in 32 healthy men.
Subjects and Methods
This paper focuses on a secondary aim of a previously published trial investigating the effect of carbohydrate intake and glycemic index on resting energy expenditure and substrate oxidation [21]. The study protocol was approved by the ethical committee of the Medical Faculty of the Christian-Albrechts-University of Kiel in November 2010. All participants provided informed written consent before participation according to the Declaration of Helsinki. No changes were made to the registered protocol. CONSORT checklist is available as supporting information; see S1 CONSORT Checklist.
Subjects and methods of this study have been described in more detail elsewhere [21,22]. Recruitment started in February 2011 and follow-up was finished in September 2012. Recruitment and final sample size for the analysis was 32 healthy men aged 20–37 years who were recruited at the University of Kiel campus. All subjects completed a medical history and physical examination to assess health status. Subjects did not use any medication on a daily basis and had a normal ECG-recording. Exclusion criteria for enrollment included smoking, unstable weight (>2 kg over the past 12 months, self-reported), family history of type 2 diabetes, food allergies, special diets (e.g. vegetarian) or being an athlete (i.e. >2h exercise per week or participation in competitive sports).
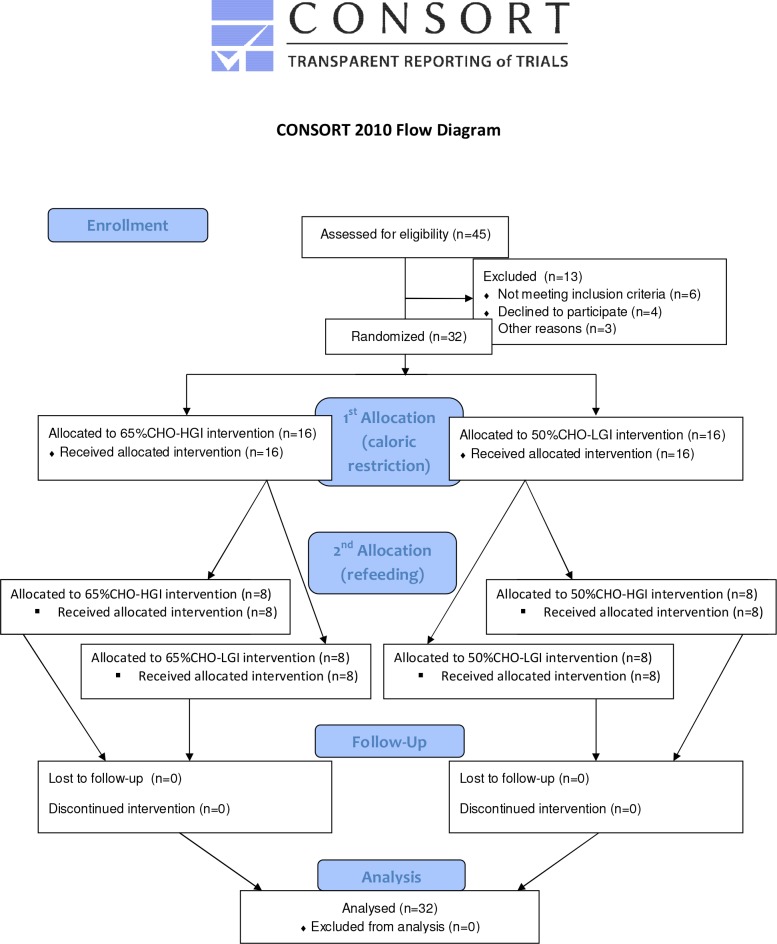
CONSORT flow chart (Fig. 1) shows the passage of participants through the different stages of the present trial including enrollment, allocation to the interventions, follow-up, and analysis.
Fig 1. CONSORT flow chart, showing the passage of participants through the different stages of the present trial: enrollment, first allocation after OF to the 65%CHO and 50%CHO intervention and second allocation after CR to 65%CHO-HGI, 65%CHO-LGI, 50%CHO-HGI and 50%CHO-LGI intervention, follow-up, and analysis.
OF, overfeeding; CR, caloric restriction; CHO: carbohydrate, HGI, high glyceamic index; LGI, low glyceamic index
More detailed information of the study protocol is available as supporting information; see S1 Protocol.
Study protocol
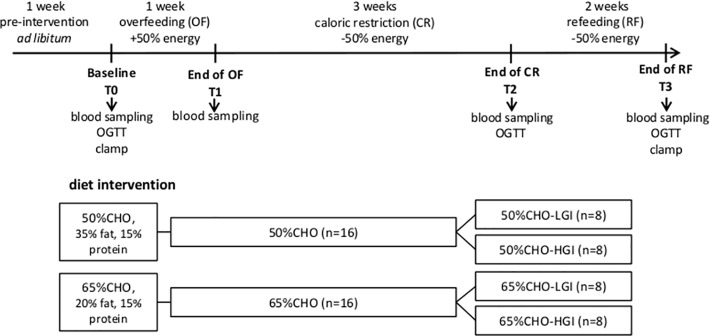
6-week strictly controlled dietary intervention was carried out at the Institute of Human Nutrition and Food Science at the Christian-Albrechts-University of Kiel. An outline of the study protocol is shown in Fig. 2. All subjects underwent an initial 1-week of overfeeding (OF, +50% of energy requirement), followed by 3-weeks of caloric restriction (CR, -50% of energy requirement) and subsequent 2-weeks of refeeding (RF, +50% of energy requirement). Energy requirement of each subject was defined by multiplying resting energy expenditure (measured by indirect calorimetry, Vmax Spectra 29n, SensorMedics, Viasys Healthcare, Bilthoven, Netherlands) by a sedentary physical activity level of 1.4 that resembles sedentary behavior [23]. Physical activity was checked throughout the study using Senswear activity monitors (SMT medical, Würzburg, Germany) (Mean values for PAL at baseline: 1.43 ±0.17; OF: 1.38 ±0.14; CR: 1.49 ±0.14; RF: 1.41 ±0.15).
Fig 2. Schematic overview of the study protocol.
OGTT, oral glucose tolerance test, CHO, carbohydrate; LGI, low glycaemic index; HGI, high glycaemic index
Fasting blood samples were taken at baseline and at the end of each intervention period. An oral glucose tolerance test (OGTT) was conducted at baseline, as well as after CR and RF. Body weight was measured daily. Physical activity was monitored by step counters. Participants were informed that physical activity should not exceed 5,000 steps a day.
Diet intervention
At the end of OF, subjects were randomized into a normal CHO intake (50% CHO, 35% fat, 15% protein) and a high CHO-intake group (65% CHO-HGI, 20% fat, 15% protein). After CR, both intervention-groups were further stratified into groups receiving a low glycaemic index (LGI) or a high glycaemic index (HGI) diet: 50%CHO-LGI, 50%CHO-HGI, 65%CHO-LGI and 65%CHO-HGI (Fig. 2). Details of the randomization process as well as basal characteristics of the study population stratified by intervention groups are given in our previous publication [22].
GL was calculated by multiplying the GI by the amount of CHO in grams provided by the food and dividing the total by 100 [24]. Mean values of dietary GL differed between the diet groups in both phases (CR: 50%CHO: 62 ±7; 65%CHO: 154 ±18, p<0.05; RF: 50%CHO-LGI: 213 ±16, 50%CHO-HGI: 356 ±57, 65%CHO-LGI: 259 ±33 and 65%CHO-HGI: 495 ±59, p<0.05).
Weight status, body composition
Body weight was measured to the nearest 0.5 kg on a calibrated scale (seca 285, seca GmbH & Co.KG, Hamburg, Germany). Height was measured to the nearest 0.1 cm by stadiometer (seca 285, seca GmbH & Co.KG, Hamburg, Germany). Measurements were performed in underwear, without shoes after voiding. Fat-free mass and fat mass were measured by Quantitative Magnetic Resonance (QMR, EchoMRI-AH, Echo Medical Systems, Houston, Texas, USA).
Blood sampling and analytical methods
Fasting blood samples were collected after an overnight fast (≥10h) at baseline and at the end of each intervention period. Glucose was measured using glucose oxidase method (BIOSEN C-Line, EKF-diagnostics, Texas, USA). Serum insulin was determined by electrochemiluminescence immunoassay (Elecsys, Roche diagnotics, Mannheim, Germany). Leptin, adiponectin, ghrelin and thyroid hormone levels (TSH, fT3, fT4) were measured by radioimmunoassay (RIA 125 Tube Kit, LINCO Research, St Charles, Missouri and Abott Diagnostics, Wiesbaden, Germany). Ghrelin secretion was shown to be inhibited by oral glucose administration [25], therefore ghrelin levels were measured at baseline and during OGTT. 24-h urinary catecholamine excretion (epinephrine and norepinephrine) was measured by HPLC according to Hollenbach et al, 1998 [26]. Because plasma norepinephrine and epinephrine have a circadian and ultradian rhythm 24h urinary catecholmine excretion was chosen as a more integrated measure of diurnal SNS activity.
Oral glucose tolerance test
Participants underwent a standard OGTT (intake of 75 g glucose) at baseline as well as after CR and RF. Venous blood was sampled 0, 30, 90 and 120 minutes after glucose intake. Insulin, glucose and ghrelin responses were determined and calculated as incremental AUC (iAUC) and total AUC (tAUC) using the trapezoid rule [27].
Hyperinsulinaemic-euglycaemic clamp
Whole-body IS at baseline and at the end of RF was assess by the hyperinsulinemic-euglycemic clamp technique according to DeFronzo et al [28], as previously described (1). M-value, expressed as mg/kg body weight/min, was determined during the last 20 min of the hyperinsulinemic glucose clamp as steady state glucose disposal rate calculated from the mean rate of exogenous glucose infusion corrected for glucose space.
Calculations of fasting and postprandial IS and insulin secretion
Fasting IS was assessed using HOMA-index: fasting glucose (mmol/l) x fasting insulin (μU/l) /22.5 [29]. Postprandial IS was calculated by Matsuda whole-body IS Index (Matsuda-ISI): 10000/(√ (fasting glucose x fasting insulin) x (mean glucose x mean insulin during OGTT)) [30]. 1st-phase insulin secretion was estimated by Stumvoll-index: 1.283+1.829 x insulin30min—138.7 x glucose30min + 3.772 x fasting insulin [31]. tAUC-insulin/tAUC-glucose was estimated to assess overall glucose-stimulated insulin secretion during OGTT [32].
Statistical analysis
Data are presented as means ±SD. Analyses were performed using SPSS version 21.0 (SPSS Inc., Chicago, Illinois). Normal distribution was assessed by Kolmogorov-Smirnov test. Parameters liver fat and GL did not meet the criteria of normal distribution and were log transformed before correlation analyses. Repeated measures ANOVA was used to observe differences across the intervention periods followed by Bonferroni post hoc tests. Differences between diet groups (time x GI, time x CHO, time x GI x CHO, GI x CHO) were assessed by mixed-design ANOVA and Bonferroni post hoc tests. Associations between changes in fasting insulin, IS or insulin secretion and potential endocrine determinants were tested using Pearson’s correlation, whereas partial correlation analyses controlling for GL or liver fat were performed between RF-induced changes in Matsuda-ISI and changes in endocrine determinants. P-values <0.05 were considered statistically significant.
Results
Baseline characteristics of the subjects and changes in body weight and fat mass during the intervention are summarized in Table 1. At baseline, seven subjects were overweight (BMI 25.6–29.3 kg/m2). Body weight and fat mass significantly increased due to OF (BW: 1.8 ±0.7 kg, p<0.001; FM: 0.8 ±0.6 kg, p<0.001), decreased with CR and increased again upon RF (all p<0.001). At the end of RF, mean body weight (p<0.05) and fat mass (p<0.001) were significantly lower compared to baseline. Changes in body weight and fat mass did not differ between diet groups except for the RF period. Weight regain was affected by CHO (<0.01) and GI x CHO interaction (p<0.05). Results of changes in body weight and fat mass by intervention groups on the same database are previously published [21]. In brief, weight regain was affected by CHO (<0.01) and GI x CHO interaction (p<0.05). Compared to the group with 50%CHO diet, subjects with 65%CHO diet gained more body weight (50%CHO: 3.0 ±1.2 kg; 65%CHO: 4.0 ±1.0 kg; p<0.05) particularly with HGI meals (50%CHO-LGI: 3.4 ±1.1 kg; 50%CHO-HGI: 2.5 ±1.1 kg; 65%CHO-LGI: 3.6 ±1.0 kg; 65%CHO-HGI: 4.4 ±0.6 kg; p<0.01) and fat mass regain was 60–70% higher in the 65%CHO-HGI group [21].
Table 1. Subject characteristics at baseline of the whole study population, and changes in body weight and fat mass during intervention periods, and changes of body weight and fat mass during CR and RF by intervention group.
| Baseline (T0) | OF (T1) | CR (T2) | RF (T3) | ΔCR (T2-T0) | ΔRF (T3-T2) | |
|---|---|---|---|---|---|---|
| age (years) | 25.5 ±3.9 | |||||
| height (cm) | 181.8 ±6.9 | |||||
| weight (kg) | 77.7 ±7.6 | 79.4 ±7.8 ††† | 73.5 ±7.4 | 76.9 ±7.9 | -4.2 ±0.9 ††† | 3.5 ±1.2*** |
| FM (kg) | 13.8 ±5.1 | 14.6 ±5.3 ††† | 12.0 ±5.0 | 13.2 ±5.0 | -1.8 ±0.5 ††† | 1.2 ±0.6*** |
| FM (%) | 17.8 ±5.9 | 18.4 ±5.8 ††† | 16.3 ±6.0 | 17.2 ±5.7 | -1.5 ±0.7 ††† | 0.8 ±0.8*** |
Values are means ±SD, n = 32.
†††p<0.001 significantly different from baseline
***p<0.001 significantly different from previous period; Repeated measures ANOVA with Bonferroni adjustments
OF, overfeeding; CR, caloric restriction; RF, refeeding; FM, fat mass; CHO, carbohydrate; GI, glycemic index
At baseline, fasting insulin levels ranged from 1.3 to 22.4 mU/l and mean values of IS were in the normal range according to cut-off values by Radikova et al. (HOMA-IR <2.3 and Matsuda >5.0) [33], while three study participants had HOMA-IR values >2.3 and Matsuda indices <5.0 together with an increased FM (>23% FM). M-values were significantly associated with HOMA-index and Matsuda-ISI [22](r = -0.43 and r = 0.42, both p<0.05) at baseline as well as after RF with Matsuda-ISI (r = 0.55, p<0.05), while association with HOMA-IR tended to be associated (r = -0.34, p = 0.06).
Changes in fasting insulin, IS, insulin secretion and potential endocrine determinants with overfeeding
Due to OF, fasting insulin levels and HOMA-index significantly increased (insulin: 4.05 ±4.83 mU/l, p<0.001; HOMA: 0.83 ±1.00, p<0.01) whereas glucose levels remained unchanged (Table 2). By contrast, no OF-induced changes in potential endocrine determinants were observed except for an increase in adiponectin (1.11 ±1.53 μg/ml, p<0.01) and a decrease in fT4 (-0.66 ±1.04 ng/l, p<0.01) (Table 3). No associations were observed between changes in fasting insulin levels or HOMA-index and potential endocrine determinants due to OF. Our discussion will therefore focus on the results of CR and RF.
Table 2. Changes in insulin secretion and IS due to overfeeding (OF) caloric restriction (CR) and refeeding (RF) (values are means ±SD).
| n | baseline (T0) | OF (T1) | CR (T2) | RF (T3) | ∆CR (T2-T0) | ∆RF (T3-T2) | |
|---|---|---|---|---|---|---|---|
| insulin secretion | |||||||
| insulin-tAUC/glucose-tAUC | 30 | 9.43 ±5.68 | 7.77 ±4.14 | 10.25 ±7.25 | -1.55 ±2.97 † | 2.34 ±4.22* | |
| Stumvoll-index | 30 | 1642 ±846 | 1300 ±512 | 1914 ±1114 | -321 ±555 †† | 576 ±840** | |
| fasting IS | |||||||
| insulin (mU/l) | 32 | 7.94 ±4.15 | 11.99 ±6.26 ††† | 5.59 ±3.69 | 8.13 ±4.36 | -2.36 ±2.86 ††† | 2.54 ±2.27*** |
| glucose (mmol/l) | 32 | 4.27 ±0.26 | 4.26 ±0.30 | 4.00 ±0.29 | 3.97 ±0.29 | -0.27 ±0.34 ††† | -0.02 ±0.33 |
| HOMA-index | 32 | 1.48 ±1.10 | 2.39 ±1.27 †† | 0.84 ±0.44 | 1.43 ±0.74 | -0.63 ±0.93 †† | 0.58 ±0.56*** |
| OGTT-derived IS | |||||||
| insulin-iAUC (mU/l per 2h) | 30 | 104.2 ±50.0 | 98.0 ±50.1 | 116.6 ±89.5 | -6.2 ±35.9 | 18.7 ±56.0 | |
| glucose-iAUC (mmol/l per 2h) | 30 | 2.24 ±1.72 | 3.30 ±1.54 | 2.38 ±1.21 | 1.07 ±2.06 † | -0.92 ±1.65* | |
| Matsuda-ISI | 30 | 9.17 ±4.44 | 12.13 ±6.37 | 8.45 ±3.46 | 2.95 ±3.23 ††† | -3.67 ±4.44*** | |
| ∆RF-baseline (T3-T0) | |||||||
| M-value (mg/kg/min) | 31 | 9.0 ±2.9 | 8.7 ±2.2 | -0.3 ±2.5 |
†p<0.05
††p<0.01
†††p<0.001 significantly different from baseline
*p<0.05
**p<0.01
***p<0.001 significantly different from previous period; Repeated measures ANOVA with Bonferroni adjustments
IS, insulin sensitivity; HOMA-index, homeostasis model assessment of insulin resistance; OGTT, oral glucose tolerance test; iAUC, incremental area under the curve; tAUC, total area under the curve; Matsuda-ISI, Mastsuda insulin sensitivity index
Table 3. Changes in endocrine parameters due to overfeeding (OF) caloric restriction (CR) and refeeding (RF) (values are means ±SD).
| Baseline (T0) | OF (T1) | CR (T2) | RF (T3) | ΔCR (T2-T0) | ΔRF (T3-T2) | ||
|---|---|---|---|---|---|---|---|
| adipokines | |||||||
| leptin (ng/ml) | 32 | 4.07 ±2.96 | 4.04 ±2.75 | 2.24 ±1.82 | 4.03 ±2.58 | -1.83 ±2.40 ††† | 1.79 ±1.47*** |
| leptin/FM | 32 | 0.27 ±0.12 | 0.26 ±0.10 | 0.18 ±0.11 | 0.29 ±0.11 | -0.09 ±0.17 † | 0.11 ±0.11*** |
| adiponectin (μg/ml) | 32 | 8.16 ±3.20 | 9.26 ±3.07 †† | 4.71 ±1.90 | 9.70 ±3.23 | -3.45 ±2.18 ††† | 4.99 ±2.89*** |
| leptin/adiponectin | 32 | 0.63 ±0.63 | 0.54 ±0.58 | 0.59 ±0.62 | 0.50 ±0.43 | -0.04 ±0.51 | -0.10 ±0.39 |
| ghrelin (pg/l) | 16 | 803 ±298 | 683 ±212 | 945 ±451 | 683 ±165 | 144 ±246 | -262 ±356* |
| ghrelin-iAUC (pg/l per 2h) | 16 | -208 ±216 | -91 ±113 | 117 ±206* | |||
| thyroid hormones | |||||||
| fT3 (ng/l) | 32 | 3.07 ±0.36 | 3.00 ±0.40 | 2.80 ±0.40 | 3.18 ±0.41 | -0.27 ±0.42 †† | 0.38 ±0.35*** |
| fT4 (ng/l) | 32 | 9.97 ±1.24 | 9.31 ±1.37 †† | 10.42 ±1.17 | 9.04 ±1.05 | 0.45 ±1.09 | -1.38 ±1.04*** |
| TSH (mU/l) | 32 | 2.07 ±1.06 | 1.86 ±0.90 | 1.51 ±0.74 | 2.21 ±0.94 | -0.55 ±0.68 ††† | 0.70 ±0.46*** |
| catecholamines | |||||||
| epinephrine (IU) | 32 | 4.65 ±2.30 | 5.25 ±2.71 | 5.11 ±2.38 | 5.78 ±2.85 | 0.46 ±2.35 | 0.68 ±2.72 |
| norepinephrine (IU) | 32 | 40.5 ±12.3 | 38.8 ±8.5 | 26.5 ±7.9 | 38.2 ±9.9 | -13.2 ±10.55 ††† | 11. 6 ±7.8*** |
†p<0.05
††p<0.01
†††p<0.001 significantly different from baseline
*p<0.05
**p<0.01
***p<0.001 significantly different from previous period; Repeated measures ANOVA with Bonferroni adjustments
OGTT, oral glucose tolerance test; iAUC, incremental area under the curve
Impact of the diet groups on changes in IS, insulin secretion and potential endocrine determinants
No time x CHO x GI interaction in changes of IS, insulin secretion or potential endocrine determinants between the diet groups were observed, except for a lower RF-induced reduction in Matsuda-ISI in the LGI groups compared to the HGI groups (LGI: -1.45 ±2.43; HGI: -5.90 ±4.92, p<0.05). Concomitantly, the increase in adiponectin with RF was higher in the HGI compared with the LGI group (HGI: 6.1 ±3.1 μg/ml; LGI: 3.9 ±2.3 μg/ml, p<0.05). GL was inversely associated with RF-induced decrease in Matsuda-ISI (r = -0.51; p<0.01).
Changes in fasting insulin, IS, insulin secretion and potential endocrine determinants with CR and RF
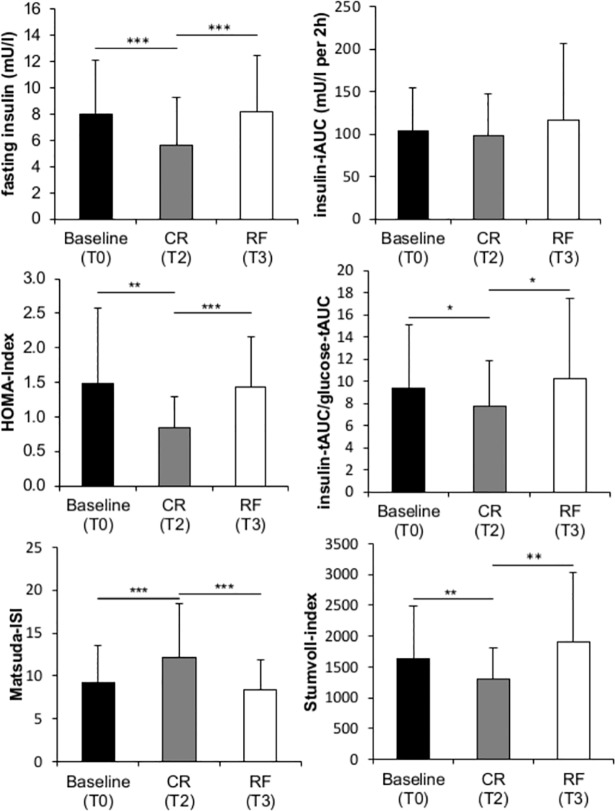
Hyperinsulinaemic euglycemic clamp (M-value) revealed normal insulin sensitivity at baseline for all participants that remained unchanged after the weight cycle (Table 2). As shown in Fig. 3, due to CR, IS (HOMA-index, Matsuda-ISI) improved and fasting insulin as well as insulin secretion (insulin-tAUC/glucose-tAUC and Stumvoll-Index) decreased. All parameters normalized again upon RF (Fig. 3; Table 2). Fasting glucose levels decreased due to CR and remained unchanged upon RF (Table 2). Levels of leptin, leptin/FM, adiponectin, fT3, TSH as well as norepinephrine excretion significantly decreased with CR (Table 3). All parameters inversely changed upon RF. Fasting and postprandial ghrelin (ghrelin-iAUC) improved with RF. Whereas fT4 decreased with RF, leptin/adiponectin-ratio and epinephrine excretion remained unchanged during all intervention periods.
Fig 3. Comparison between fasting insulin level, IS (HOMA-index and Matsuda-ISI) as well as insulin secretion (insulin-iAUC, insulin-tAUC/glucose-tAUC, Stumvoll-index) at baseline (T0), after caloric restriction (CR, T2) and refeeding (RF, T3).
*p<0.05, **p<0.01, ***p<0.001; Repeated measures ANOVA with Bonferroni adjustments. HOMA, homeostasis model assessment; ISI, insulin sensitivity index, iAUC, incremental area under the curve; tAUC, total area under the curve
Associations between changes in IS or insulin secretion and potential endocrine determinants with CR and RF
Improved IS due to CR correlated with the decrease in leptin (r = 0.36, p<0.01, for HOMA-index only) and the increase in ghrelin (r = 0.62, p<0.01, for Matsuda-ISI only). The decrease in postprandial IS upon RF was associated with the decrease in ghrelin (r = 0.83, r<0.001) as well as the increases in adiponectin (r = -0.38, p<0.05), fT3 (r = -0.40, r<0.05) and TSH (r = -0.38, r<0.05) levels. However, partial correlation analysis controlling for GL revealed that associations between the RF-induced decrease in Matsuda-ISI and increases in fT3 and TSH levels were no longer significant (fT3: r = -0.24; TSH: r = -0.32, both p>0.05).
The increase in insulin secretion upon RF (Stumvoll-index, insulin-tAUC/glucose-tAUC) was inversely associated with leptin/adiponectin-ratio (Stumvoll-index: r = -0.52; insulin-tAUC/glucose-tAUC: r = -0.46; both p<0.01) and fT4 levels (insulin-tAUC/glucose-tAUC: r = -0.38, p<0.05).
The decrease in fT3 and the increase in fT4 levels due to CR as well as inverse changes in these parameters with RF (Table 3) were positively associated with each other (CR: r = 0.39, p<0.05; RF: r = 0.39, p<0.05). Increases in fT3 and TSH levels upon RF were also correlated (r = 0.44, p<0.05).
Pearson's correlation coefficients (r) showing main interactions between changes in IS or insulin secretion and potential endocrine determinants are summarized in S1 Table.
Discussion
In line with our hypothesis, weight loss and regain led to changes in IS and insulin secretion that were partly explained by concomitant changes in leptin, adiponectin, leptin/adiponectin-ratio, ghrelin, fT3 and fT4 levels, while the associations were not affected by different diet groups. Although the observed correlations need not necessarily be causal, our findings are supported by evidence from mechanistic, in vitro, animal or patient studies discussed below.
Impact of leptin or leptin/adiponectin-ratio on IS or insulin secretion
The association between the decrease in leptin and the improvement in HOMA-index with CR (see results) was also shown with weight loss in obese patients [34]. Our results therefore indicate that even in mostly lean or slightly overweight subjects a diet-induced decrease in leptin is associated with improved insulin sensitivity. There is evidence for an adipoinsular axis in which insulin stimulates leptin production in adipocytes and leptin inhibits the production of insulin in human beta-cells [35]. We did however not find an inhibitory effect of leptin on insulin secretion during the weight cycle.
The ratio of leptin to adiponectin has been repeatedly suggested as an index of IS [36–38] whereas in our study we could not confirm an association between changes in leptin/adiponectin-ratio and IS. Adiponectin may however respond differently to caloric restriction in healthy non-obese insulin sensitive subjects compared to obese patients. While we found a decrease in adiponectin with a negative energy balance (Table 3) an increase in adiponectin with weight loss was observed in obese patients who also had lower baseline adiponectin levels [39]. Whereas the increase in adiponectin with weight loss in obese patients was associated with improved IS [40] in our study the decrease in adiponectin with caloric restriction was accompanied by an improvement in IS and vice versa upon RF (Table 2 and 3). The proposed insulin sensitizing effect of adiponectin [41] therefore needs further investigation. The observed changes in adiponectin are in line with other studies in lean healthy men [42,43] that imply that the coincidence of changes in adiponectin and IS may not be causal in non-obese healthy subjects.
Although it was shown that adiponectin increased insulin secretion in human pancreatic β-cells [44] we found no association between changes in adiponectin and increased insulin secretion during refeeding. This may be due to the observation that adiponectin exerts its effect on insulin secretion by the activation of lipid oxidation [44] that is suppressed with hypercaloric refeeding.
Impact of ghrelin on IS or insulin secretion
Increases in ghrelin levels with caloric restriction were associated with an improvement in Matsuda-ISI. Likewise reduced ghrelin levels with RF were associated with a decrease in Matsuda-ISI. These findings are consistent with cross-sectional data from two studies that found circulating ghrelin levels to be associated with lower insulin resistance (assessed by HOMA-index) [45,46]. In line with a potential positive effect of ghrelin on glucose homeostasis, fasting ghrelin is lower in obese insulin resistant adolescents with polycystic ovary syndrome [45] and type 2 diabetic patients [47]. The insulin sensitizing effect of ghrelin remains controversial because IS measured by the gold standard euglycemic hyperinsulinemic clamp, was not associated with plasma ghrelin in a Swedish population of healthy men [48]. Moreover, an acute administration of exogenous ghrelin has been found to decrease glucose stimulated insulin secretion in healthy humans [14,49,50], an effect that could be mediated by increased AMPK phosphorylation and UCP2 mRNA expression [51]. However, we found no association between changes in ghrelin levels and insulin secretion in response to weight loss or weight regain.
Impact of thyroid hormones on IS or insulin secretion
In contrast to normal thyroid regulation TSH and fT3 did not change in opposite directions but showed a joint decrease due to CR and increase upon RF (with inverse changes in fT4 levels), respectively (Table 3). These findings are in line with the observation of low levels of fT3 and TSH in underweight patients [52,53] and elevated levels of both hormones in obese patients [54,55]. We found that the changes in fT3 and fT4 due to CR and RF were correlated (see results). This may be explained by impaired (CR) and increased (RF) extrathyroidal monodeiodination of T4 into T3 that was observed in underweight and overweight subjects, respectively [56]. Low fT3 in underweight and high levels in overweight subjects have been suggested to reflect metabolic adaptation to the altered nutritional status to spare energy consumption in starvation or increase energy expenditure in overfeeding [57].Our data support this hypothesis and show that even short-term perturbations in energy balance are associated with adaptations of thyroid hormone levels.
Increases in fT3 and TSH with RF were associated with a decrease in postprandial IS assessed by Matsuda-ISI (Table 3). Similar findings have also been shown in subjects with elevated TSH or fT3 levels [19]. Nevertheless, associations between thyroid hormones and IS remain controversial since not only hyperthyroidism but also hypothyroidism was associated with insulin resistance [57]. Explanations for the underlying mechanisms mostly refer to the insulin antagonistic effect of thyroid hormones in the liver or insulin agonistic effects in the muscle, found in animal models [58]. However, these results were obtained in hyper- or hypothyroidism and cannot be compared to our results in healthy humans with changes in thyroid hormones in a normal euthyroid range. Ortega et al. found a positive association between insulin secretion and fT3 in euthyroid humans [20]. Although we found an inverse correlation between refeeding-induced changes in fT4 and insulin secretion (assessed by tAUC-insulin/tAUC-glucose) a decrease in fT4 with refeeding correlated with an increase in fT3 levels (see results) and imply an increased T4-T3 conversion that might facilitate a higher insulin secretion.
Associations between changes in Matsuda-ISI and thyroid hormones with RF were no longer significant using partial correlation analysis adjusting for GL (see results). This suggests that the decrease in IS with refeeding is not explained by an increase in fT3 but is due to the increase in GL of the diet that has been shown to contribute to increased fT4 to fT3 conversion in rats [59]. In line with this interpretation, it was shown that fT3 levels increased 21% during three weeks of carbohydrate overfeeding [60].
Impact of catecholamine excretion on IS or insulin secretion
Norepinephrine excretion decreased with CR and increased again after RF (with a concomittant increase in epinephrine). No associations were observed between changes in catecholamine excretion and changes in IS or insulin secretion. It has however long been known from isolated beta cells in a rat model that epinephrine and norepinephrine inhibit insulin secretion [61–63]. It was also shown, that euglycaemic hyperinsulinemia during a clamp leads to an increase in norepinephrine release indicating an increase in SNS activity [64] and thus contributes to impaired IS [65]. Since it is assumed that only chronic or sustained SNS activation contribute to insulin resistance [66], short-term changes in SNS-activity during two weeks of hypercaloric refeeding may not be long enough to impair IS.
Strengths and limitations of the study
A major advantage of our study is the controlled dietary intervention in healthy subjects that allows an intraindividual comparison of early determinants of changes in insulin sensitivity or insulin secretion with weight loss and regain.
There are also some limitations that need to be discussed. (i) Deterioration in IS and secretion with RF may not only be explained by endocrine determinants but may also be due to an increase in ectopic lipid storage. In a previous publication on the same database, liver fat increased with RF above baseline values [22]. We now observed that liver fat after RF was positively associated with RF-induced changes in HOMA-IR and insulin secretion (HOMA-IR: r = 0.55; Stumvoll-index: r = 0.65 and insulin-tAUC/glucose-tAUC: r = 0.70, all p<0.05). Using partial correlation adjusting for liver fat, associations between RF-induced changes in Matsuda-ISI and thyroid hormones or insulin secretion and thyroid hormones as well as leptin/adiponectin-ratio were no longer significant (data not shown). (ii) Indirect methods were used to assess IS (HOMA-index, Matsuda-ISI). Although surrogate measures of insulin sensitivity are preferred because they are less expensive, invasive and challenging to perform they should be used with caution in longitudinal study designs because they showed less correlation with reference methods of IS in a an intervention study [67]. (iii) Although we did not measure GLP-1, a recent study showed no changes in basal or postprandial GLP-1 after overfeeding for 35 days and subsequent caloric restriction in healthy men [4]. By contrast, undercarboxylated osteocalcin and cortisol may be better determinants of changes in IS and insulin secretion with weight loss and regain. Of notice, recent studies showed a correlation between serum/plasma osteocalcin and insulin secretion in lean subjects [68] and the weight-loss induced increase in osteocalcin was associated with improved glucose homeostasis [69]. In obese children, weight-loss induced reduction in cortisol correlates with improvement in IS. Serum testosterone may also be an important determinant of changes in IS during weight cycling. Short-term starvation decreased serum testosterone levels by approximately 40% in lean healthy men [70] and low serum testosterone levels have been shown to be associated with insulin resistance [71]. Further studies focusing insulin secretion should also address arterial natriuretic peptide (ANP) since recent studies found increased insulin levels during ANP infusion in human subjects [72].(iv) Because our intervention involved changes in energy balance as well as diet composition this may limit the power of our analysis. As a measure of effect size, i.e. the practical meaningfulness of main effects and diet interactions, we used SPSS-derived partial eta squared, to describe effect sizes in our ANOVA. Mean partial eta squared for all main effects (caloric restriction and refeeding per se) was 0.52, and partial eta squared for all time x diet interactions (glycemic index and carbohydrate content) averaged 0.07. According to Cohen (1988, cited by Westermann R, 2000 [73]) these partial eta squared values are of large (>0.1) and medium size (0.06–0.1), respectively. This shows that the energy deficit or surplus alone has a much stronger impact on changes in outcome variables and may override some effects of the diet composition.
Conclusion
Even in non-obese healthy men changes in leptin contribute to changes in IS after weight loss. We could not confirm that leptin/adiponectin-ratio is an important determinant of IS during weight loss or regain. By contrast, it is suggested that adiponectin and ghrelin affect IS during weight cycling. Changes in thyroid hormones might reflect early adaptations in energy balance. While leptin, ghrelin and adiponectin seem to be the major endocrine determinants of changes in IS, leptin/adiponectin-ratio and fT4 levels may impact changes in insulin secretion with weight cycling. Catecholamine excretion does not seem to be involved in early changes in IS or insulin secretion with short-term perturbations in energy balance.
Supporting Information
(DOC)
(DOC)
(DOC)
Acknowledgments
The authors would like to thank Wiebke Braun, Maike Johannsen and Ulrike Preuß for their excellent technical assistance.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
The study was funded by a grant of the Germany Ministry of Education and Research (BMBF 0315681), the German Research Foundation (DFG Bo 3296/1-1) and the BMBF Kompetenznetz Adipositas, Core domain “Body composition” (Körperzusammensetzung; FKZ 01GI1125). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. Adochio RL, Leitner JW, Gray K, Draznin B, Cornier M-A (2009) Early responses of insulin signaling to high-carbohydrate and high-fat overfeeding. Nutr Metab (Lond) 6: 37 10.1186/1743-7075-6-37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Lagerpusch M, Bosy-Westphal A, Kehden B, Peters A, Müller MJ (2012) Effects of brief perturbations in energy balance on indices of glucose homeostasis in healthy lean men. Int J Obes 36: 1094–1101. 10.1038/ijo.2011.211 [DOI] [PubMed] [Google Scholar]
- 3. Lagerpusch M, Enderle J, Later W, Eggeling B, Pape D, et al. (2013) Impact of glycaemic index and dietary fibre on insulin sensitivity during the refeeding phase of a weight cycle in young healthy men. Br J Nutr 109: 1606–1616. 10.1017/S000711451200462X [DOI] [PubMed] [Google Scholar]
- 4.Brands M, Swat M (2013) Effects of a hypercaloric diet on β‐cell responsivity in lean healthy men. Clin Endocrinol (Oxf). [DOI] [PubMed]
- 5. Hamm P, Shekelle RB, Stamler J (1989) Large fluctuations in body weight during young adulthood and twenty-five-year risk of coronary death in men. Am J Epidemiol 129: 312–318. [DOI] [PubMed] [Google Scholar]
- 6. Folsom AR, French SA, Zheng W, Baxter JE, Jeffery RW (1996) Weight variability and mortality: the Iowa Women’s Health Study. Int J Obes Relat Metab Disord 20: 704–709. [PubMed] [Google Scholar]
- 7. Olson MB, Kelsey SF, Bittner V, Reis SE, Reichek N, et al. (2000) Weight cycling and high-density lipoprotein cholesterol in women: evidence of an adverse effect. J Am Coll Cardiol 36: 1565–1571. [DOI] [PubMed] [Google Scholar]
- 8. Barclay AW, Petocz P, McMillan-Price J, Flood VM, Prvan T, et al. (2008) Glycemic index, glycemic load, and chronic disease risk—a meta-analysis of observational studies. Am J Clin Nutr 87: 627–637. [DOI] [PubMed] [Google Scholar]
- 9. Kotronen A, Juurinen L, Tiikkainen M, Vehkavaara S, Yki-Järvinen H (2008) Increased liver fat, impaired insulin clearance, and hepatic and adipose tissue insulin resistance in type 2 diabetes. Gastroenterology 135: 122–130. 10.1053/j.gastro.2008.03.021 [DOI] [PubMed] [Google Scholar]
- 10. Kolb H, Mandrup-Poulsen T (2010) The global diabetes epidemic as a consequence of lifestyle-induced low-grade inflammation. Diabetologia 53: 10–20. 10.1007/s00125-009-1573-7 [DOI] [PubMed] [Google Scholar]
- 11. Lam TKT, Carpentier A, Lewis GF, van de Werve G, Fantus IG, et al. (2003) Mechanisms of the free fatty acid-induced increase in hepatic glucose production. Am J Physiol Endocrinol Metab 284: E863–E873. [DOI] [PubMed] [Google Scholar]
- 12. Chandra R, Liddle RA (2013) Modulation of pancreatic exocrine and endocrine secretion. Curr Opin Gastroenterol 29: 517–522. 10.1097/MOG.0b013e3283639326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Wauters M, Considine RV, Yudkin JS, Peiffer F, De Leeuw I, et al. (2003) Leptin levels in type 2 diabetes: associations with measures of insulin resistance and insulin secretion. Horm Metab Res 35: 92–96. [DOI] [PubMed] [Google Scholar]
- 14. Broglio F, Arvat E, Benso A (2001) Ghrelin, a natural GH secretagogue produced by the stomach, induces hyperglycemia and reduces insulin secretion in humans. J Clin Endocrinol Metab. 86:5083–6 [DOI] [PubMed] [Google Scholar]
- 15. Sun Y, Asnicar M, Smith RG (2007) Central and peripheral roles of ghrelin on glucose homeostasis. Neuroendocrinology 86: 215–228. [DOI] [PubMed] [Google Scholar]
- 16. Meloni AR, DeYoung MB, Lowe C, Parkes DG (2013) GLP-1 receptor activated insulin secretion from pancreatic β-cells: mechanism and glucose dependence. Diabetes Obes Metab 15: 15–27. 10.1111/j.1463-1326.2012.01663.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Rosenbaum M, Hirsch J, Murphy E, Leibel RL (2000) Effects of changes in body weight on carbohydrate metabolism, catecholamine excretion, and thyroid function. Am J Clin Nutr 71: 1421–1432. [DOI] [PubMed] [Google Scholar]
- 18. Galofré JC, Pujante P, Abreu C, Santos S, Guillen-Grima F, et al. (2008) Relationship between thyroid-stimulating hormone and insulin in euthyroid obese men. Ann Nutr Metab 53: 188–194. 10.1159/000172981 [DOI] [PubMed] [Google Scholar]
- 19. Lambadiari V, Mitrou P, Maratou E, Raptis AE, Tountas N, et al. (2011) Thyroid hormones are positively associated with insulin resistance early in the development of type 2 diabetes. Endocrine 39: 28–32. 10.1007/s12020-010-9408-3 [DOI] [PubMed] [Google Scholar]
- 20. Ortega E, Koska J, Pannacciulli N (2008) Free triiodothyronine plasma concentrations are positively associated with insulin secretion in euthyroid individuals. Eur J Endocrinol. 158:217–21 10.1530/EJE-07-0592 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Kahlhöfer J, Lagerpusch M, Enderle J, Eggeling B, Braun W, et al. (2014) Carbohydrate intake and glycemic index affect substrate oxidation during a controlled weight cycle in healthy men. Eur J Clin Nutr. 68:1060–6 10.1038/ejcn.2014.132 [DOI] [PubMed] [Google Scholar]
- 22. Lagerpusch M, Enderle J, Eggeling B, Braun W, Johannsen M, et al. (2013) Carbohydrate quality and quantity affect glucose and lipid metabolism during weight regain in healthy men. J Nutr 143: 1593–1601. 10.3945/jn.113.179390 [DOI] [PubMed] [Google Scholar]
- 23. Hills AP, Mokhtar N, Byrne NM (2014) Assessment of Physical Activity and Energy Expenditure: An Overview of Objective Measures. Front Nutr 1: 1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Liu S, Willett WC, Stampfer MJ, Hu FB, Franz M, et al. (2000) A prospective study of dietary glycemic load, carbohydrate intake, and risk of coronary heart disease in US women. Am J Clin Nutr 71: 1455–1461. [DOI] [PubMed] [Google Scholar]
- 25. Broglio F, Gottero C, Prodam F, Destefanis S, Gauna C, et al. (2004) Ghrelin secretion is inhibited by glucose load and insulin-induced hypoglycaemia but unaffected by glucagon and arginine in humans. Clin Endocrinol (Oxf) 61: 503–509. [DOI] [PubMed] [Google Scholar]
- 26. Hollenbach E, Schulz C, Lehnert H (1998) Rapid and sensitive determination of catecholamines and the metabolite 3-methoxy-4-hydroxyphen-ethyleneglycol using HPLC following novel extraction procedures. Life Sci 63: 737–750. [DOI] [PubMed] [Google Scholar]
- 27. Matthews JN, Altman DG, Campbell MJ, Royston P (1990) Analysis of serial measurements in medical research. BMJ 300: 230–235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. DeFronzo R, Tobin J, Andres R (1979) Glucose clamp technique: a method for quantifying insulin secretion and resistance. Am J Physiol Endocrinol Metab 237: E214–E223. [DOI] [PubMed] [Google Scholar]
- 29. Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, et al. (1985) Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28: 412–419. [DOI] [PubMed] [Google Scholar]
- 30. Matsuda M, DeFronzo R (1999) Insulin sensitivity indices obtained from oral glucose tolerance testing: comparison with the euglycemic insulin clamp. Diabetes Care 22:1462–70 [DOI] [PubMed] [Google Scholar]
- 31. Stumvoll M, Mitrakou a, Pimenta W, Jenssen T, Yki-Järvinen H, et al. (2000) Use of the oral glucose tolerance test to assess insulin release and insulin sensitivity. Diabetes Care 23: 295–301. [DOI] [PubMed] [Google Scholar]
- 32. Albareda M, Murugo M, Leiva A De, Corcoy R (2000) Assessment of insulin sensitivity and beta-cell function from measurements in the fasting state and during an oral glucose tolerance test. Diabetologia. 43:1507–11. [DOI] [PubMed] [Google Scholar]
- 33. Radikova Z, Koska J, Huckova M, Ksinantova L, Imrich R, et al. (2006) Insulin sensitivity indices: a proposal of cut-off points for simple identification of insulin-resistant subjects. Exp Clin Endocrinol Diabetes 114: 249–256. [DOI] [PubMed] [Google Scholar]
- 34. Wang T-N, Chang W-T, Chiu Y-W, Lee C-Y, Lin K-D, et al. (2013) Relationships between changes in leptin and insulin resistance levels in obese individuals following weight loss. Kaohsiung J Med Sci 29: 436–443. 10.1016/j.kjms.2012.08.041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Seufert J, Kieffer TJ, Leech C a, Holz GG, Moritz W, et al. (1999) Leptin suppression of insulin secretion and gene expression in human pancreatic islets: implications for the development of adipogenic diabetes mellitus. J Clin Endocrinol Metab 84: 670–676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Oda N, Imamura S, Fujita T, Uchida Y, Inagaki K, et al. (2008) The ratio of leptin to adiponectin can be used as an index of insulin resistance. Metabolism 57: 268–273. 10.1016/j.metabol.2007.09.011 [DOI] [PubMed] [Google Scholar]
- 37.Inoue M, Yano M, Yamakado M, Maehata E, Suzuki S (2006) Relationship between the adiponectin-leptin ratio and parameters of insulin resistance in subjects without hyperglycemia. Metabolism. [DOI] [PubMed]
- 38. Finucane FM, Luan J, Wareham NJ, Sharp SJ, O’Rahilly S, et al. (2009) Correlation of the leptin:adiponectin ratio with measures of insulin resistance in non-diabetic individuals. Diabetologia 52: 2345–2349. 10.1007/s00125-009-1508-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Arita Y, Kihara S, Ouchi N, Takahashi M, Maeda K, et al. (1999) Paradoxical decrease of an adipose-specific protein, adiponectin, in obesity. 1999. Biochem Biophys Res Commun 425: 560–564. [DOI] [PubMed] [Google Scholar]
- 40.Weyer C, Funahashi T, Tanaka S, Hotta K, Matsuzawa Y, et al. (2013) Hypoadiponectinemia in Obesity and Type 2 Diabetes: Close Association with Insulin Resistance and Hyperinsulinemia. [DOI] [PubMed]
- 41. Wang C, Mao X, Wang L, Liu M, Wetzel MD, et al. (2007) Adiponectin sensitizes insulin signaling by reducing p70 S6 kinase-mediated serine phosphorylation of IRS-1. J Biol Chem 282: 7991–7996. [DOI] [PubMed] [Google Scholar]
- 42. Knudsen S, Hansen L (2012) Changes in insulin sensitivity precede changes in body composition during 14 days of step reduction combined with overfeeding in healthy young men. J Appl Physiol 113:7–15. 10.1152/japplphysiol.00189.2011 [DOI] [PubMed] [Google Scholar]
- 43. Brøns C, Jensen CB, Storgaard H, Hiscock NJ, White A, et al. (2009) Impact of short-term high-fat feeding on glucose and insulin metabolism in young healthy men. J Physiol 587: 2387–2397. 10.1113/jphysiol.2009.169078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Patané G, Caporarello N, Marchetti P, Parrino C, Sudano D, et al. (2013) Adiponectin increases glucose-induced insulin secretion through the activation of lipid oxidation. Acta Diabetol 50: 851–857. 10.1007/s00592-013-0458-x [DOI] [PubMed] [Google Scholar]
- 45. Rahmanpour H, Jamal L, Mousavinasab SN, Esmailzadeh A, Azarkhish K (2012) Association between polycystic ovarian syndrome, overweight, and metabolic syndrome in adolescents. J Pediatr Adolesc Gynecol 25: 208–212. 10.1016/j.jpag.2012.02.004 [DOI] [PubMed] [Google Scholar]
- 46. Amini P, Wadden D, Cahill F, Randell E, Vasdev S, et al. (2012) Serum acylated ghrelin is negatively correlated with the insulin resistance in the CODING study. PLoS One 7: e45657 10.1371/journal.pone.0045657 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Poykko SM, Kellokoski E, Horkko S, Kauma H, Kesaniemi YA, et al. (2003) Low Plasma Ghrelin Is Associated With Insulin Resistance, Hypertension, and the Prevalence of Type 2 Diabetes. Diabetes 52: 2546–2553. [DOI] [PubMed] [Google Scholar]
- 48. Fagerberg B, Hultén LM, Hulthe J (2003) Plasma ghrelin, body fat, insulin resistance, and smoking in clinically healthy men: the atherosclerosis and insulin resistance study. Metabolism 52: 1460–1463. [DOI] [PubMed] [Google Scholar]
- 49. Vestergaard ET, Gormsen LC, Jessen N, Lund S, Hansen TK, et al. (2008) Ghrelin Infusion in Humans Induces Acute Insulin Resistance and Lipolysis Independent of Growth Hormone Signaling. 57: 3205–3210. d 10.2337/db08-0025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Tong J, Prigeon RL, Davis HW, Bidlingmaier M, Kahn SE, et al. (2010) Ghrelin suppresses glucose-stimulated insulin secretion and deteriorates glucose tolerance in healthy humans. Diabetes 59: 2145–2151. 10.2337/db10-0504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Wang Y, Nishi M, Doi A, Shono T, Furukawa Y, et al. (2010) Ghrelin inhibits insulin secretion through the AMPK-UCP2 pathway in beta cells. FEBS Lett 584: 1503–1508. 10.1016/j.febslet.2010.02.069 [DOI] [PubMed] [Google Scholar]
- 52. Reinehr T, Isa A, de Sousa G, Dieffenbach R, Andler W (2008) Thyroid hormones and their relation to weight status. Horm Res 70: 51–57. 10.1159/000129678 [DOI] [PubMed] [Google Scholar]
- 53. Onur S, Haas V, Bosy-Westphal A, Hauer M, Paul T, et al. (2005) L-tri-iodothyronine is a major determinant of resting energy expenditure in underweight patients with anorexia nervosa and during weight gain. Eur J Endocrinol 152: 179–184. [DOI] [PubMed] [Google Scholar]
- 54. Moulin de Moraes CM, Mancini MC, de Melo ME, Figueiredo DA, Villares SMF, et al. (2005) Prevalence of subclinical hypothyroidism in a morbidly obese population and improvement after weight loss induced by Roux-en-Y gastric bypass. Obes Surg 15: 1287–1291. [DOI] [PubMed] [Google Scholar]
- 55. Reinehr T, de Sousa G, Andler W (2006) Hyperthyrotropinemia in obese children is reversible after weight loss and is not related to lipids. J Clin Endocrinol Metab 91: 3088–3091. [DOI] [PubMed] [Google Scholar]
- 56. Reinehr T (2010) Obesity and thyroid function. Mol Cell Endocrinol 316: 165–171. 10.1016/j.mce.2009.06.005 [DOI] [PubMed] [Google Scholar]
- 57. Wang C (2013) The relationship between type 2 diabetes mellitus and related thyroid diseases. J Diabetes Res. 2013:390534 10.1155/2013/390534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Brenta G (2011) Why can insulin resistance be a natural consequence of thyroid dysfunction? J Thyroid Res 2011: 152850 10.4061/2011/152850 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Gavin LA, Moeller M, McMahon FA, Castle JN, Gulli R, et al. (1988) Carbohydrate feeding increases total body and specific tissue 3,5,3’-triiodothyronine neogenesis in the rat. Endocrinology 123: 1075–1081. [DOI] [PubMed] [Google Scholar]
- 60. Welle S, O’Connell M, Danforth E, Campbell R (1984) Decreased free fraction of serum thyroid hormones during carbohydrate overfeeding. Metabolism 33: 837–839. [DOI] [PubMed] [Google Scholar]
- 61. Malaisse W, Malaisse-Lagae F, Wright PH, Ashmore J (1967) Effects of adrenergic and cholinergic agents upon insulin secretion in vitro. Endocrinology 80: 975–978. [DOI] [PubMed] [Google Scholar]
- 62. Porte D (1969) Sympathetic Regulation of Insulin Secretion. Arch Intern Med 123: 252 [PubMed] [Google Scholar]
- 63. Robertson RP, Porte D (1973) Adrenergic modulation of basal insulin secretion in man. Diabetes 22: 1–8. [DOI] [PubMed] [Google Scholar]
- 64. Berne C, Fagius J, Pollare T, Hjemdahl P (1992) The sympathetic response to euglycaemic hyperinsulinaemia. Evidence from microelectrode nerve recordings in healthy subjects. Diabetologia 35: 873–879. [DOI] [PubMed] [Google Scholar]
- 65. Canale MP, Manca di Villahermosa S, Martino G, Rovella V, Noce A, et al. (2013) Obesity-related metabolic syndrome: mechanisms of sympathetic overactivity. Int J Endocrinol 2013: 865965 10.1155/2013/865965 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Lambert GW, Straznicky NE, Lambert EA, Dixon JB, Schlaich MP (2010) Sympathetic nervous activation in obesity and the metabolic syndrome—causes, consequences and therapeutic implications. Pharmacol Ther 126: 159–172. 10.1016/j.pharmthera.2010.02.002 [DOI] [PubMed] [Google Scholar]
- 67. Xiang a H, Watanabe RM, Buchanan T a (2014) HOMA and Matsuda indices of insulin sensitivity: poor correlation with minimal model-based estimates of insulin sensitivity in longitudinal settings. Diabetologia 57: 334–338. 10.1007/s00125-013-3121-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Fernández-Real JM, Izquierdo M, Ortega F, Gorostiaga E, Gómez-Ambrosi J, et al. (2009) The relationship of serum osteocalcin concentration to insulin secretion, sensitivity, and disposal with hypocaloric diet and resistance training. J Clin Endocrinol Metab 94: 237–245. 10.1210/jc.2008-0270 [DOI] [PubMed] [Google Scholar]
- 69. Hinton PS, Thyfault JP, Thomas TR (2011) Weight loss-induced increases in osteocalcin are associated with improvements in glucose homeostasis. Endocrinol Metab Syndr 01 10.4172/2161-1017 [DOI] [Google Scholar]
- 70. Chan JL, Heist K, DePaoli AM, Veldhuis JD, Mantzoros CS (2003) The role of falling leptin levels in the neuroendocrine and metabolic adaptation to short-term starvation in healthy men. J Clin Invest 111: 1409–1421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Pitteloud N, Mootha VK, Dwyer AA, Hardin M, Lee H, et al. (2005) Relationship between testosterone levels, insulin sensitivity, and mitochondrial function in men. Diabetes Care 28: 1636–1642. [DOI] [PubMed] [Google Scholar]
- 72. Uehlinger D (1986) Increase in circulating insulin induced by atrial natriuretic peptide in normal humans. J Cardiovasc Pharmacol. 8:1122–9. [DOI] [PubMed] [Google Scholar]
- 73.Westermann R (2000) Wissenschaftstheorie und Experimentalmethodik: Ein Lehrbuch zur Psychologischen Methodenlehre. p.357
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOC)
(DOC)
(DOC)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.