Abstract
HIV stigma as a barrier to retention in HIV care has not been well-studied outside the United States. We conducted a case-control study in Lima, Peru to examine this issue. Cases were out-of-care for ≥12 months (n=66) and controls were recruited from patients in active care presenting for a clinic visit (n=110). A previously validated HIV stigma scale with four domains was used. Associations between being out-of-care and each stigma domain were assessed using multivariable logistic regression. Stigma scores were highest for disclosure concerns. Modest associations were found for greater disclosure concerns (OR=1.16; 95% CI: 0.99, 1.36) and concerns with public attitudes (OR=1.20; 95% CI: 1.03, 1.40). Enacted stigma and negative self-image showed non-linear associations with being out-of-care that plateaued or declined, respectively, at higher levels of stigma. The threshold effect for enacted stigma warrants further exploration, while disclosure concerns may be especially amenable to intervention in this population.
Keywords: HIV, Stigma, Retention in care, Peru
Introduction
Retention in HIV care is essential for maximizing favorable health outcomes among people living with HIV (PLHIV).(1) Guidelines emphasize the importance of remaining in care in addition to adhering to antiretroviral treatment (ART).(2) The availability of ART has transformed HIV infection into a chronic, manageable condition.(3, 4) Thus, successful management requires prompt diagnosis, access to ART, and excellent adherence, but, above all, adequate and continuous HIV care.(5) Poor retention in care has been associated with delayed initiation of ART(6) and increased mortality compared to patients who did not miss visits.(7, 8) While prevention of adverse clinical outcomes is the primary goal of HIV care, continuous care may also decrease secondary HIV transmission within the community.(5, 9) HIV has been stigmatized since the beginning of the epidemic and remains a barrier to HIV prevention and care.(10-14) HIV stigma, as with other health-related stigmas, is a multi-dimensional construct that includes both structural- and individual-level aspects and requires a power dynamic between those who are infected and those who are not.(15-17) From the perspective of PLHIV, stigma can be conceptualized as enacted stigma (experiencing discrimination because of HIV status), anticipated stigma (anticipated or perceived prejudice or discrimination in the community), and internalized stigma (feeling shame or blame because of HIV status).(18-20) This three-domain framework retains the multi-domain construct of HIV stigma while providing a simplified operational definition that facilitates measurement. Because patient-based interventions are critical for HIV prevention and care, it is necessary to understand how HIV stigma affects a patient's retention in care and, indirectly, affects risk of further HIV transmission.
Evidence for associations between HIV stigma and retention in HIV care primarily come from qualitative studies(10, 11, 21, 22) and by extension from stigma's association with access to care and treatment adherence(13, 14, 23-27). Only a few studies, all conducted within the United States (US), have quantitatively addressed HIV stigma and retention in care(27-30) using validated HIV stigma scales.(18) Given the expansion of therapy for persons in resource limited settings,(31) the relationship between HIV stigma and retention in care in international settings warrants investigation.
Poor retention in care and its impact on HIV transmission, morbidity, and mortality were of particular concern to staff at the study clinic in Lima, Peru where we planned this study. While the adult HIV prevalence is low in Latin America in general (0.4%) and Peru specifically (0.4%), it is concentrated among urban men who have sex with men (MSM) with HIV estimates as high as 12.4% among MSM in Peru.(32, 33) Furthermore, the number of women living with HIV has been increasing over the last 10 years.(32) Globally, the Central and South America regions are one of the few regions not experiencing a decline in new HIV infections over the last decade, with an estimated 4,600 new infections occurring in Peru during 2012.(32) To further explore the impact HIV stigma has on retention in HIV care in a low-resource country with an ongoing HIV epidemic, we conducted a case-control study to evaluate the association between HIV stigma and retention in HIV care among HIV-infected Peruvians.
Methods
Study location and population
We conducted the study between April 2011 and January 2012 at the Department of Infectious, Tropical, and Dermatologic Diseases at the Hospital Nacional Cayetano Heredia (HNCH), a national referral center for HIV diagnosis and clinical care supported by the Ministry of Health to provide free ART to HIV-positive individuals. A multi-disciplinary team (nurse, psychologist, social worker, etc) provides social evaluations and “training” to the patients about the importance of retention in care, but there is a lack of personnel for follow-up activities of these patients. For this reason, the clinic was particularly interested in patients who were lost to care. Since May 2004, >4,800 patients have been diagnosed and approximately 2,240 patients initiated HIV care at HNCH, comprising the clinical cohort within the Programa de Control de Enfermedades de Transmision Sexual y SIDA.
From this cohort, all patients diagnosed and/or initiating HIV care at HNCH by having at least one provider visit between January 1, 2005 and March 31, 2010 were identified. Acknowledging variability in definitions of retention and loss to follow-up,(34, 35) eligible cases were patients currently out-of-care, defined as not having a provider visit for >12 months as of March 31, 2011 (last recorded visit occurring before March 31, 2010). Eligible controls were patients currently in care, defined as having ≥ 2 documented medical care visits per year since initiating care, with the most recent visit occurring <12 months before March 31, 2011.
Participant Selection and Enrollment
We sought to sample cases from eligible out-of-care patients. Initially, we assigned a random number to each eligible patient and they were contacted by telephone. We discovered, however, that most patients could not be contacted due to incorrect or missing telephone numbers. We then used home visits to contact participants, resulting in a convenience sample of as many persons as we could find. Home visits constitute a routine part of the HNCH follow up care and the presence of the research interviewers did not draw additional attention to, or risk, the confidentiality of the patients. The research interviewer contacted eligible patients via telephone or home visit using a discrete script to ensure confidentiality. All questionnaires were completed in person at, or near, the home, regardless of whether the patient was initially contacted by telephone or home visit. Participation in the study concluded upon completion of the questionnaire.
We sampled controls from eligible in-care patients. We reviewed daily clinic appointment schedules each morning to identify eligible patients. Patients were approached discretely by a research interviewer while checking in for their appointment, informed of the study, and invited to participate. Participants completed an interviewer-assisted questionnaire in a private location and the study concluded once the questionnaire was completed.
Data collection
The interviewer-assisted questionnaire gathered data on socio-demographic information, HIV disclosure, actual or perceived barriers to receiving HIV care at HNCH, transportation, HIV stigma, HIV knowledge, social support, and depression.
HIV stigma was measured using a modified, Spanish-language version of the Berger HIV Stigma Scale previously validated in Peru.(36, 37) The modified version is a 20-item scale used to quantify the multiple domains of HIV stigma as experienced and perceived by patients within their communities: community enacted stigma (e.g., “People appear to be scared of me because I have HIV”), disclosure concerns (e.g., “Telling someone I have HIV is risky”), negative self-image (e.g., “I feel like I am not as good as others because I have HIV”), and concern with public attitudes (e.g., “Most people believe that a person with HIV is dirty”). Each domain is measured using a sub-scale with 5 items that participants respond to using a 4-point Likert scale ranging from “strongly disagree” to “strongly agree”. Responses were coded 0-3, with higher scores indicating higher stigma (sub-scale scores range from 0-15). Cronbach's alpha, a measure of internal reliability, ranged from 0.64 to 0.82 for each of the sub-scales.
HIV knowledge was measured using an index modified from Carey et al.(38) and contained 24 True/False questions relating to the prevention, transmission, and treatment of HIV. Social support was measured using seven items from the O'Brien social support scale(39) that asked about perceived availability of support. Depression was measured using eight items from the Spanish version of the PHQ-9 (excluding the final question about hurting yourself or wishing you were dead).(40) For these measures, items were reverse coded as needed to obtain a single score each for knowledge, social support, and depression, with higher scores indicating higher levels of each factor. Cronbach's alpha ranged from 0.71 to 0.81 for all three scales.
Date of HIV diagnosis, date and value of latest CD4+ cell count prior to March 31, 2010, and ART status were obtained from patient medical records.
Data analysis
Data were analyzed using Stata/SE 12® (StataCorp, College Station, TX). Socio-demographic and clinical dataare presented categorically in Table 1 but age, income, time since HIV diagnosis and CD4+ cell count were analyzed as continuous variables. Differences in mean stigma scores between the in-care and out-of-care groups were assessed using t-tests.
Table 1.
Socio-demographic, clinical, and psychosocial characteristics of in-care and out-of-care HIV patients, Lima, Peru, 2011-2012 (N=176).
| In-care (N=110) | Out-of-care (N=66) | |||
|---|---|---|---|---|
| N | % | N | % | |
| Age | ||||
| 18-25 | 13 | 11.8 | 10 | 15.2 |
| 26-35 | 41 | 37.3 | 28 | 42.4 |
| 36-45 | 26 | 23.6 | 20 | 30.3 |
| 46+ | 30 | 27.3 | 8 | 12.1 |
| Sex | ||||
| Male | 75 | 68.2 | 31 | 47.0 |
| Female | 35 | 31.8 | 35 | 53.0 |
| Incomea | ||||
| 0-500 soles | 25 | 22.7 | 17 | 27.0 |
| 501-1000 soles | 50 | 44.5 | 30 | 47.6 |
| 1001-1500 soles | 16 | 14.6 | 3 | 4.8 |
| >1500 soles | 19 | 17.3 | 13 | 20.6 |
| Missing | 0 | 3 | ||
| Travel time to HNCHb | ||||
| 0-30 minutes | 28 | 25.5 | 20 | 31.3 |
| 30-60 minutes | 45 | 40.9 | 36 | 56.3 |
| ≥60 minutes | 37 | 33.6 | 8 | 12.5 |
| Missing | 0 | 2 | ||
| Time since HIV diagnosis | ||||
| 0-11 months | 31 | 39.2 | 3 | 4.8 |
| 12-35 months | 29 | 36.7 | 23 | 37.1 |
| 36-59 months | 10 | 12.7 | 23 | 37.1 |
| >60 months | 9 | 11.4 | 13 | 21.0 |
| Missing | 31 | 4 | ||
| Last CD4+ cell countc | ||||
| <100 | 9 | 12.0 | 7 | 16.3 |
| 100-249 | 16 | 21.3 | 10 | 23.3 |
| 250-349 | 15 | 20.0 | 9 | 21.0 |
| 350-499 | 16 | 21.3 | 6 | 14.0 |
| >500 | 19 | 25.3 | 11 | 25.6 |
| Missing | 35 | 23 | ||
| Receiving ART therapy | ||||
| No | 49 | 44.6 | 54 | 81.8 |
| Yes | 61 | 55.5 | 12 | 18.2 |
| Received HIV care elsewhere in past year | ||||
| No | 101 | 91.8 | 28 | 43.8 |
| Yes | 9 | 8.2 | 36 | 56.3 |
| Missing | 0 | 2 | ||
| Mean | SD | Mean | SD | |
| HIV knowledge (range: 0-24) | 18.9 | 3.7 | 19.2 | 2.4 |
| Social support (range: 0-21) | 16.3 | 3.7 | 15.7 | 5.0 |
| Depression (range: 0-24) | 6.7 | 4.7 | 8.1 | 6.2 |
| HIV stigma | ||||
| Enacted (range: 0-15) | 5.5 | 3.1 | 7.2 | 2.7 |
| Disclosure concerns (range: 0-15) | 9.5 | 2.7 | 10.3 | 2.3 |
| Negative self-image (range: 0-15) | 5.3 | 2.5 | 6.3 | 2.3 |
| Concern with public attitudes (range: 0-15) | 8.9 | 2.8 | 10.0 | 2.4 |
1 nuevo soles ≈ $0.36 USD
Hospital National Cayetano Heredia
As of March 31, 2010 for in-care participants or last clinic visit for out-of-care participants
Crude and adjusted odds ratios (OR and aOR) and 95% confidence intervals (95% CI) were estimated using logistic regression. Four separate regression models were used to model the relationship between the four stigma domains and odds of being out-of-care. Confounders for the adjusted models were selected a priori based on variables previously reported to be associated with both HIV stigma and being out-of-care, while not adjusting for intermediates (e.g., depression).(6, 27-29, 41-46) These included age, gender, income, travel time to HNCH, time since HIV diagnosis, CD4+ cell count, ART status, HIV knowledge, and social support. Due to a substantial amount of missing data on time since diagnosis and CD4+ cell count, these were not included in the multivariable analyses. Preliminary analyses indicate that excluding these covariates changes the aOR by <5%.
Linearity between stigma scores and odds of being out-of-care was assessed by comparing models using a single, linear stigma term with models using a restricted cubic spline with three knots (10th, 50th, and 90th percentiles) or four knots (5th, 35th, 65th, and 95th percentiles). Restricted cubic splines allow for a flexible and non-linear relationship while using a linear relationship at the upper and lower ends of the continuous variable.(47) Likelihood ratio tests were used to compare models using a spline with models using a linear term. When P<0.05, indicating a non-linear relationship, stigma was modeled using a spline to relax linearity assumptions. Due to the relatively small sample size a spline with three knots was preferred over one with four knots unless the likelihood ratio test comparing the two was also P<0.05). In all other instances, a linear term was used. As with HIV stigma, all continuous covariates were assessed for linearity. Time since HIV diagnosis, HIV knowledge, and social support were modeled using a restricted cubic spline. Age, income, and CD4+ cell count were modeled using a linear term.
The Institutional Review Boards of the Vanderbilt University Medical Center and HNCH approved this study and written informed consent was obtained from all participants.
Results
Among 736 eligible out-of-care participants identified in the database, 66 (9%) were successfully approached and enrolled; 11 (1%) were in care elsewhere and refused to participate, 40 (5%) had died, and 619 (84%) could not be located. Of the 619 who could not be located, 185 (30%) had incomplete contact information or lived outside the service area of HNCH, 134 (22%) could not be contacted via phone (wrong number or did not answer) and no address was available, 60 (10%) were not at home when the study personnel made the home visit, 83 (13%) gave false addresses where the individual had never resided, 75 (12%) were correct addresses but the individual had moved away, and 82 (13%) were non-existent addresses. We enrolled 111 in-care participants, representing 86% participation among those approached in the clinic. Of the 177 participants enrolled in the study, one was missing data on one or more of the HIV stigma items and was excluded from the analysis resulting in a final sample of 176 participants (66 out-of-care and 110 in-care), 78.2% of the intended sample size of 225.
Out-of-care participants were slightly younger and more often female, and lived closer to the clinic (Table 1). Out-of-care participants had been living with HIV longer, but were less likely to be on ART even though CD4+ counts were similar between the two groups. Slightly more than half (56%) of out-of-care participants reported receiving HIV care elsewhere during the previous year. HIV knowledge and social support were high and similar among both groups of participants. Depression was uncommon in the study sample but was slightly higher among out-of-care participants.
All stigma scores were normally distributed (histograms in Figure 1) and there was considerable variation in scores for the four domains, each of which had a possible range of 0 to 15 (Table 1). Stigma scores were higher for the out-of-care participants on all four domains compared to the in-care patients. In general, however, scores were low (out of a possible score of 15) for enacted stigma (5.5 for in-care and 7.2 for out-of-care, p<0.001) and negative self-image (5.3 and 6.4, p=0.007), but high for disclosure concerns (9.5 for in-care and 10.3 for out-of-care, p=0.049) and concern with public attitudes (8.9 and 10.0, p=0.008).
Figure 1.
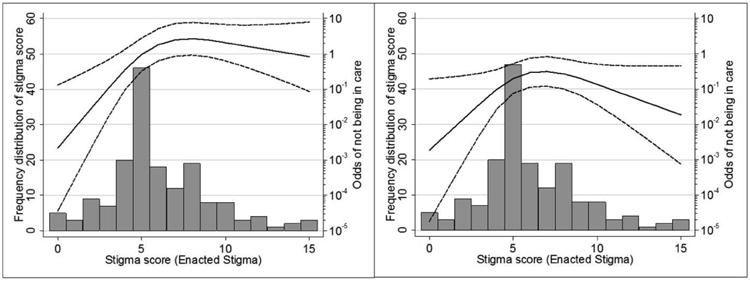
Frequency distribution of enacted stigma scores and adjusted association with being out-of-care among HIV patients, Lima, Peru, 2011-2012, in the primary analysis (left panel) and re-classified analysis (right panel)a.
a Predicted odds (solid line) and 95% confidence interval (dashed line) for enacted stigma were obtained by fixing all other covariates at their median. Likelihood ratio test for linearity of the stigma term: primary analysis, p<0.001; re-classified analysis, p=0.006.
Thirty-six (56%) out-of-care participants received HIV care at a non-HNCH clinic during the period that defined them as out-of-care from HNCH. A sensitivity analysis was conducted to assess how re-classifying these 36 participants as “in-care” would affect the observed results. Compared with out-of-care participants who did not receive care elsewhere, out-of-care participants who did receive care elsewhere had slightly higher scores for enacted stigma (7.8 vs. 6.7; P=0.11), similar scores for disclosure concerns (10.6 vs. 10.0; P=0.30) and negative self-image (6.2 vs. 6.5; P=0.68), and higher scores for concern with public attitudes (10.8 vs. 9.3; P=0.01).
Crude and adjusted odds ratios for a linear association between HIV stigma and being out-of-care are shown in Table 2. While the largest association is seen for enacted stigma (aOR=1.27; 95% CI: 1.10, 1.48), there was evidence that this was truly a non-linear relationship (Likelihood ratio test “LRT” P<0.001). The association between negative self-image and being out-of-care also demonstrated a non-linear relationship (LRT P=0.02). Only disclosure concerns (aOR=1.16; 95% CI: 0.99, 1.36) and concern with public attitudes (aOR=1.20; 95% CI: 1.03, 1.40) demonstrated a linear relationship with being out-of-care, where a one-point increase in the stigma score was associated with a 16% and 20% increase, respectively, in the odds of being out-of-care.
Table 2.
Crude and adjusted odds ratios for the linear associations between HIV stigmaa and being out-of-care among HIV patients, Lima, Peru, 2011-2012.
| Primary outcome of being out-of-care (>12 months since HNCH visit) | Sensitivity analysis reclassifying out-of-care patients attending other clinics in previous 12 months as in-care | |||||||
|---|---|---|---|---|---|---|---|---|
| Crude | Adjustedb | Crude | Adjustedc | |||||
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Enacted stigmad | 1.22 | 1.09, 1.36 | 1.27 | 1.10, 1.48 | 1.06 | 0.94, 1.20 | 1.04 | 0.86, 1.22 |
| Disclosure concerns | 1.13 | 1.00, 1.28 | 1.16 | 0.99, 1.36 | 1.02 | 0.87, 1.19 | 1.04 | 0.87, 1.24 |
| Negative Self-imagee | 1.19 | 1.04, 1.36 | 1.16 | 0.97, 1.39 | 1.16 | 0.99, 1.35 | 1.15 | 0.93, 1.42 |
| Concern with Public Attitudesf | 1.17 | 1.04, 1.32 | 1.20 | 1.03, 1.40 | 0.98 | 0.85, 1.13 | 0.94 | 0.80, 1.11 |
Modeled as a simple, linear term where the OR reflects the relative change in odds of being out-of-care for each one point increase in the HIV stigma score.
Adjusted for age, gender, income, travel time to HNCH, social support, knowledge of HIV, and ART status
Adjusted for age, gender, income, social support, knowledge of HIV, and ART status (no adjustment for travel time to HNCH)
Evidence of a non-linear association with being out-of-care in both the primary and re-classified analyses; see results from Table 3 and Figure 1.
The non-linear relationships for both enacted stigma and negative self-image are shown in Table 3, Figure 1, and Figure 2. For lower scores between zero and seven, a one-point increase in enacted stigma had much stronger associations with being out-of-care than initially apparent from the linear association, with statistically significant aORs ranging from 1.37 to 2.71 at various points along the curve (Table 3 and Figure 1). At higher scores, the relationship flattens out (e.g., no association) and possibly declines (e.g., inverse association). Negative self-image showed a slightly different non-linear relationship, with lower scores showing no association with being out-of-care, followed by a strong association as scores increased between four and seven, at which point the association flattens again and possibly declines (Table 3 and Figure 2).
Table 3.
Crude and adjusted odds ratios for the non-linear associations between HIV stigmaa and being out-of-care among HIV patients, Lima, Peru, 2011-2012.
| Primary outcome of being out-of-care (>12 months since HNCH visit) | Sensitivity analysis reclassifying out-of-care patients attending other clinics in previous 12 months as in-care | |||||||
|---|---|---|---|---|---|---|---|---|
| Crude | Adjustedb | Crude | Adjustedc | |||||
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Enacted stigmad | ||||||||
| Stigma score of 5 vs. 4 | 2.19 | 1.43, 3.33 | 2.71 | 1.47, 4.98 | 1.86 | 1.10, 3.12 | 2.06 | 1.04, 4.12 |
| Stigma score of 6 vs. 5 | 1.67 | 1.28, 2.17 | 1.89 | 1.30, 2.75 | 1.42 | 1.03, 1.95 | 1.47 | 0.98, 2.20 |
| Stigma score of 7 vs. 6 | 1.31 | 1.14, 1.52 | 1.37 | 1.12, 1.68 | 1.11 | 0.92, 1.34 | 1.08 | 0.85, 1.36 |
| Stigma score of 8 vs. 7 | 1.10 | 0.97, 1.24 | 1.08 | 0.89, 1.30 | 0.93 | 0.76, 1.13 | 0.86 | 0.65, 1.13 |
| Stigma score of 9 vs. 8 | 0.97 | 0.83, 1.14 | 0.92 | 0.71, 1.18 | 0.82 | 0.64, 1.07 | 0.73 | 0.51, 1.07 |
| Negative Self-imagee | ||||||||
| Stigma score of 4 vs. 3 | 1.13 | 0.76, 1.68 | 1.11 | 0.70, 1.75 | No evidence of a non-linear association, see results for linear association in Table 2. | |||
| Stigma score of 5 vs. 4 | 1.51 | 1.19, 1.93 | 1.60 | 1.17, 2.18 | ||||
| Stigma score of 6 vs. 5 | 1.99 | 1.29, 3.05 | 2.20 | 1.24, 3.90 | ||||
| Stigma score of 7 vs. 6 | 1.51 | 1.14, 1.99 | 1.42 | 1.00, 2.01 | ||||
| Stigma score of 8 vs. 7 | 1.08 | 0.89, 1.30 | 0.86 | 0.61, 1.21 | ||||
| Concern with Public Attitudesf | ||||||||
| Stigma score of 6 vs. 5 | No evidence of a non-linear association, see results for linear association in Table 2. | 1.61 | 1.06, 2.46 | 1.46 | 0.94, 2.27 | |||
| Stigma score of 7 vs. 6 | 1.59 | 1.05, 2.40 | 1.44 | 0.94, 2.22 | ||||
| Stigma score of 8 vs. 7 | 1.45 | 1.02, 2.07 | 1.33 | 0.92, 1.93 | ||||
| Stigma score of 9 vs. 8 | 1.21 | 0.93, 1.58 | 1.13 | 0.85, 1.50 | ||||
| Stigma score of 10 vs. 9 | 0.92 | 0.74, 1.16 | 0.88 | 0.69, 1.14 | ||||
Modeled as a restricted cubic spline; the OR no longer reflects a constant relative change in odds of being out-of-care for each one point increase in the HIV stigma score.
Adjusted Model 1 adjusted for age, gender, income, travel time to HNCH, social support, knowledge of HIV, and ART status
Adjusted Model 2 adjusted for all covariates in Model 1 and time since HIV diagnosis
Likelihood ratio test for the non-linear stigma term: primary analysis, p<0.001; re-classified analysis, p=0.006
Likelihood ratio test for the non-linear stigma term: primary analysis, p=0.02; re-classified analysis, p=0.39
Likelihood ratio test for the non-linear stigma term: primary analysis, p=0.50; re-classified analysis, p=0.006
Figure 2.
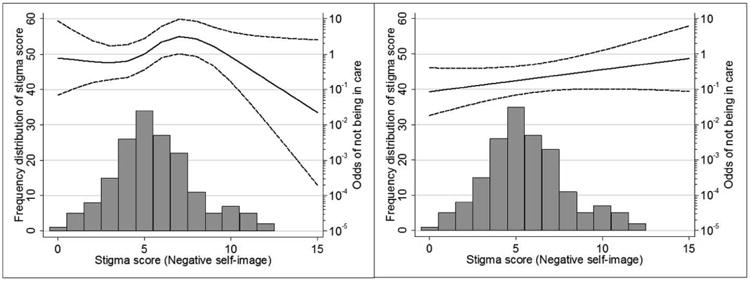
Frequency distribution of negative self-image scores and adjusted association with being out-of-care among HIV patients, Lima, Peru, 2011-2012, in the primary analysis (left panel) and re-classified analysis (right panel)a.
aPredicted odds (solid line) and 95% confidence interval (dashed line) for negative self-image were obtained by fixing all other covariates at their median. Likelihood ratio test for linearity of the stigma term: primary analysis, p=0.02; re-classified analysis, p=0.39.
Associations from the sensitivity analysis were attenuated slightly with decreased precision due to only 30 participants remaining classified as out-of-care (Table 3). Enacted stigma retained its non-linear association with being out-of-care (LRT P=0.006). However, negative self-image changed to a linear association (LRT P=0.39; aOR=1.15; 95% CI: 0.93, 1.42) while concern with public attitudes changed to a non-linear association (LR P=0.006). For scores between zero and eight, a one-point increase in concern with public attitudes scores was associated with a 33% to 46% increase in the odds of being out-of-care, after which the association flattens and begins to decline (Table 3 and Figure 3).
Figure 3.
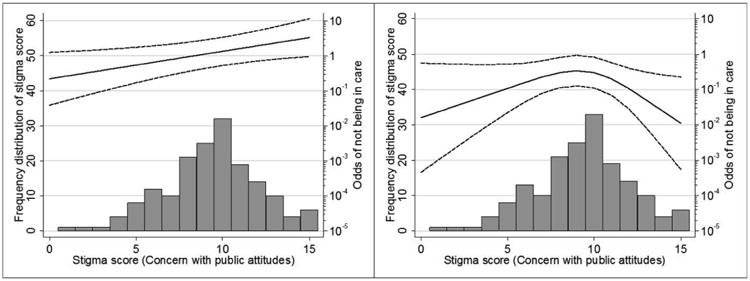
Frequency distribution of concern with public attitude scores and adjusted association with being out-of-care among HIV patients, Lima, Peru, 2011-2012, in the primary analysis (left panel) and re-classified analysis (right panel)a.
a Predicted odds (solid line) and 95% confidence interval (dashed line) for concern with public attitudes were obtained by fixing all other covariates at their median. Likelihood ratio test for linearity of the stigma term: primary analysis, p=0.50; re-classified analysis, p=0.006.
Discussion
We quantitatively measured HIV stigma and assessed its association with retention in HIV care in Lima, Peru. On average, stigma scores were low for enacted stigma (discrimination) and negative self-image (internalized stigma), but higher for disclosure concerns and concerns with public attitudes (anticipated/perceived stigma). Disclosure concerns and concerns with public attitudes both had modest, linear associations with being out-of-care. A surprising finding, however, was the observed non-linear associations, with an initial increase in the odds of being out-of-care for enacted stigma that then plateaued at higher levels of stigma. Similar non-linear relationships were seen for negative self-image and concern for public attitudes, but these were not consistent between the primary and sensitivity analyses. The non-linear relationship for enacted stigma and poor retention in HIV care remained even after reclassifying some out-of-care patients as being in-care (see Table 3 and Figure 1). Furthermore, it has important implications for interventions. If the non-linear association is true (e.g., confirmed by prospective studies), it suggests that for individuals reporting high levels of enacted stigma, interventions must achieve a much larger reduction in stigma to improve retention outcomes, whereas individuals with moderate levels of stigma would see improved outcomes with only a minor reduction.
Four prior studies from the US found no association between HIV stigma and other measures of retention including: 1) clinic appointment attendance among 178 adolescent and young women,(29) 2) completing two or more clinic appointments in the past six months among 398 minority men,(28) 3) longer gaps in medical care among 95 adults,(30) and 4) lacking a regular source of HIV care among 202 adults.(27) The latter study by Sayles et al. found an elevated odds ratio for the association between high levels of stigma and not having a regular source of HIV care that is comparable to some of our results, but with very wide confidence intervals (OR=2.25, 95% CI: 0.69, 7.32). The current study is therefore one of the first studies to demonstrate statistically significant associations between HIV stigma and poor retention in care, defined here as going ≥12 months since the last documented clinic visit. It is possible that HIV stigma is not associated with other, less extreme forms of poor retention reported by the other studies, such as missing one or more (but not all) clinic visits over a period of time.(28, 29)
The associations observed here between HIV stigma domains and retention in care reinforce the complex nature of HIV stigma and the multifaceted approaches that must be taken to reduce HIV stigma to improve retention in HIV care, ART adherence, and other outcomes.(48) Nachega et al. suggest that combination anti-stigma interventions/approaches that address the three major domains of HIV stigma should include community education, support groups, advocacy, and/or legal approaches.(48) Nevertheless, there are few quality interventions that have proven efficacious, particularly for reducing structural, rather than individual, drivers of stigma.(49, 50) Furthermore, while interventions have been shown to reduce HIV stigma, these interventions were not designed to assess if improvements in HIV-related behavioral outcomes occurred following the reductions in stigma.(50) While all aspects of HIV stigma are important to address, interventions targeting internalized stigma among PLHIV (measured in the current study as negative self-image) may prove more feasible for improving retention than community-based stigma interventions to reduce enacted and anticipated stigma, and have the added benefit of reducing depression among PLHIV as well.(51-54) Our findings suggest this could have some impact on improving retention, though not as much as reducing enacted stigma. To this end, recent studies on the beneficial role of spirituality and counseling to aid with coping and reduction of internalized stigma are promising.(52, 55)
In this study, it was unclear how best to interpret the non-linear associations that either plateau at moderate levels of stigma (enacted stigma) or suggest a lower odds of being out-of-care at higher levels of stigma. One suggestion is that PLHIV reporting high levels of stigma due to their HIV may become highly motivated to appear as “normal” as possible by concealing their condition so as to avoid future discrimination or to prove they are not any different from those not infected with HIV. Remaining in care and adhering to ART are measures that can be taken to remain healthy and appear uninfected. A similar suggestion has been made in the context of tuberculosis, where higher levels of perceived tuberculosis and HIV stigma were associated with shorter delay times in seeking tuberculosis treatment among women.(56) These observed results for negative self-image and concern with public attitudes should be interpreted with caution, however, since they were highly susceptible to misclassification of being out-of-care. We could not verify whether participants who received care elsewhere were truly “in-care” or simply attended another clinic once or twice. Nevertheless, this could help explain the observation that out-of-care patients lived closer to the HNCH clinic than the in-care patients. This may be due, in part, to the resource limitations of actively seeking out-of-care patients too far from the clinic, but it was also observed that the 36 out-of-care patients who were re-classified as in-care elsewhere had the highest levels of stigma. This study was not designed to further explore this, but one possible explanation is that the desire to appear normal by remaining in care and on treatment was strong enough to overcome any challenges of travelling further to receive care in an effort to avoid being seen by someone who knows them at or near the HNCH clinic.
A final explanation for our non-linear findings could be selection bias, as a very high proportion of eligible out-of-care participants could not be located for this study. Perhaps the level of HIV stigma reported by out-of-care participants in the study is underestimated, and an unbiased out-of-care sample would have resulted in a linear association similar to that seen for the other domains of stigma. Yet for this bias to truly exist, it suggests that selection bias only occurred among participants reporting higher enacted stigma and negative self-image (or concern with public attitudes in the sensitivity analysis), but not the other domains. Furthermore a subsequent analysis comparing out-of-care participants who could be located to those who could not be located showed no differences in demographic characteristics, CD4+ cell count, viral load, or ART status, suggesting the out-of-care participants enrolled in our study are not very different from those who could not be located in terms of measured characteristics.(57) If HIV stigma is higher among out-of-care participants who could not be located, however, it likely means the true association between stigma and retention in HIV care is underestimated in our study.
Two final limitations are worth noting. First, the temporal relationship between measured stigma levels and retention in care cannot be determined. It is possible that the higher levels of stigma reported by out-of-care patients is a result of being out-of-care, and that these same patients would have reported lower levels of stigma prior to falling out-of-care. This limitation can only be addressed through a prospective study. Second, findings from this study only apply to retention defined as 12 months or longer without documented HIV care. Other, less extreme forms of poor retention such as short gaps, intermittent care, or missed visits may have different associations with HIV stigma. Nevertheless, patients who leave care represent a distinct and important group for which efforts to prevent attrition are important.
An important finding from our study is the strong and robust non-linear relationship between enacted stigma and poor retention in care. This warrants further exploration because it suggests that different interventions may be required depending on the level of stigma reported: those with moderate stigma may have improved outcomes with only minor reductions in stigma, while, those reporting higher stigma might require interventions capable of drastically reducing stigma in order to see the improvement. In addition to enacted stigma, we also report modest associations for three HIV stigma domains (negative self-image, disclosure concerns, and concern with public attitudes) and poor retention in HIV care, and a that warrants further exploration. Which aspects of HIV stigma to address via interventions remains another important question, though disclosure concerns and negative self-image (internalized stigma) are perhaps a more accessible target than community attitudes. Regardless of these caveats, our study does suggest that HIV stigma is associated with poor retention in HIV care. While prospective studies are needed to confirm these findings, specifically addressing enacted stigma (i.e., discrimination) through community outreach or patient-oriented interventions may improve adherence to HIV care and treatment.
Acknowledgments
We thank the dedicated research and support staff at HNCH and Vanderbilt Institute for Global Health. Funding and support for this study came from the Vanderbilt Institute for Clinical and Translational Research (grant UL1 TR000445 from the National Center for Advancing Translational Sciences at the National Institutes of Health); Vanderbilt Emphasis Program, Tinker Field Research Grant, and the Infectious Disease Society of America Medical Scholars Program (to C Valenzuela); Instituto de Medicina Tropical Alexander Von Humboldt, Universidad Peruana Cayetano Heredia, Peru, ICOHRTA Network for AIDS/TB Research Training (NIH Grant 1U2RTW007368-01A1- Fogarty International Center, Lima Peru) (to C Ugarte and J Paz).
Footnotes
The final publication is available at Springer via http://dx.doi.org/10.1007/s10461-014-0908-7.
References
- 1.Mugavero MJ, Davila JA, Nevin CR, Giordano TP. From access to engagement: measuring retention in outpatient HIV clinical care. AIDS Patient Care STDS. 2010;24(10):607–13. doi: 10.1089/apc.2010.0086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Thompson MA, Mugavero MJ, Amico KR, et al. Guidelines for Improving Entry Into and Retention in Care and Antiretroviral Adherence for Persons With HIV: Evidence-Based Recommendations From an International Association of Physicians in AIDS Care Panel. Ann Intern Med. 2012;156(11):817–33. doi: 10.7326/0003-4819-156-11-201206050-00419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Walensky RP, Paltiel AD, Losina E, et al. The survival benefits of AIDS treatment in the United States. J Infect Dis. 2006;194(1):11–9. doi: 10.1086/505147. [DOI] [PubMed] [Google Scholar]
- 4.Wada N, Jacobson LP, Cohen M, French A, Phair J, Munoz A. Cause-Specific Life Expectancies After 35 Years of Age for Human Immunodeficiency Syndrome-Infected and Human Immunodeficiency Syndrome-Negative Individuals Followed Simultaneously in Long-term Cohort Studies, 1984-2008. Am J Epidemiol. 2013;177(2):116–25. doi: 10.1093/aje/kws321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Burns DN, Dieffenbach CW, Vermund SH. Rethinking prevention of HIV type 1 infection. Clin Infect Dis. 2010;51(6):725–31. doi: 10.1086/655889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ulett KB, Willig JH, Lin HY, et al. The therapeutic implications of timely linkage and early retention in HIV care. AIDS Patient Care STDS. 2009;23(1):41–9. doi: 10.1089/apc.2008.0132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mugavero MJ, Lin HY, Willig JH, et al. Missed visits and mortality among patients establishing initial outpatient HIV treatment. Clin Infect Dis. 2009;48(2):248–56. doi: 10.1086/595705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tripathi A, Youmans E, Gibson JJ, Duffus WA. The impact of retention in early HIV medical care on viro-immunological parameters and survival: a statewide study. AIDS Res Hum Retroviruses. 2011;27(7):751–8. doi: 10.1089/AID.2010.0268. [DOI] [PubMed] [Google Scholar]
- 9.Granich RM, Gilks CF, Dye C, De Cock KM, Williams BG. Universal voluntary HIV testing with immediate antiretroviral therapy as a strategy for elimination of HIV transmission: a mathematical model. Lancet. 2009;373(9657):48–57. doi: 10.1016/S0140-6736(08)61697-9. [DOI] [PubMed] [Google Scholar]
- 10.Mugavero MJ. Improving engagement in HIV care: what can we do? Top HIV Med. 2008;16(5):156–61. [PubMed] [Google Scholar]
- 11.Kempf MC, McLeod J, Boehme AK, et al. A qualitative study of the barriers and facilitators to retention-in-care among HIV-positive women in the rural southeastern United States: implications for targeted interventions. AIDS Patient Care STDS. 2010;24(8):515–20. doi: 10.1089/apc.2010.0065. [DOI] [PubMed] [Google Scholar]
- 12.Herek GM, Capitanio JP. Public reactions to AIDS in the United States: a second decade of stigma. Am J Public Health. 1993;83(4):574–7. doi: 10.2105/ajph.83.4.574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chesney MA, Smith AW. Critical Delays in HIV Testing and Care: The Potential Role of Stigma. Am Behav Sci. 1999;42(7):1162–74. [Google Scholar]
- 14.Golin C, Isasi F, Bontempi JB, Eng E. Secret pills: HIV-positive patients' experiences taking antiretroviral therapy in North Carolina. AIDS Educ Prev. 2002;14(4):318–29. doi: 10.1521/aeap.14.5.318.23870. [DOI] [PubMed] [Google Scholar]
- 15.Parker R, Aggleton P. HIV and AIDS-related stigma and discrimination: a conceptual framework and implications for action. Soc Sci Med. 2003;57(1):13–24. doi: 10.1016/s0277-9536(02)00304-0. [DOI] [PubMed] [Google Scholar]
- 16.Deacon H. Towards a sustainable theory of health-related stigma: lessons from the HIV/AIDS literature. J Community Appl Soc Psychol. 2006;16:418–25. [Google Scholar]
- 17.Link BG, Phelan JC. Conceptualizing Stigma. Annu Rev Sociol. 2001;27:363–85. [Google Scholar]
- 18.Earnshaw VA, Chaudoir SR. From conceptualizing to measuring HIV stigma: a review of HIV stigma mechanism measures. AIDS Behav. 2009;13(6):1160–77. doi: 10.1007/s10461-009-9593-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nyblade LC. Measuring HIV stigma: existing knowledge and gaps. Psychol Health Med. 2006;11(3):335–45. doi: 10.1080/13548500600595178. [DOI] [PubMed] [Google Scholar]
- 20.Steward WT, Herek GM, Ramakrishna J, et al. HIV-related stigma: Adapting a theoretical framework for use in India. Soc Sci Med. 2008;67(8):1225–35. doi: 10.1016/j.socscimed.2008.05.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rajabiun S, Mallinson RK, McCoy K, et al. “Getting me back on track”: the role of outreach interventions in engaging and retaining people living with HIV/AIDS in medical care. AIDS Patient Care STDS. 2007;21(Suppl 1):S20–9. doi: 10.1089/apc.2007.9990. [DOI] [PubMed] [Google Scholar]
- 22.Bogart LM, Chetty S, Giddy J, et al. Barriers to care among people living with HIV in South Africa: contrasts between patient and healthcare provider perspectives. AIDS Care. 2013;25(7):843–53. doi: 10.1080/09540121.2012.729808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ware NC, Wyatt MA, Tugenberg T. Social relationships, stigma and adherence to antiretroviral therapy for HIV/AIDS. AIDS Care. 2006;18(8):904–10. doi: 10.1080/09540120500330554. [DOI] [PubMed] [Google Scholar]
- 24.Wolitski RJ, Pals SL, Kidder DP, Courtenay-Quirk C, Holtgrave DR. The effects of HIV stigma on health, disclosure of HIV status, and risk behavior of homeless and unstably housed persons living with HIV. AIDS Behav. 2009;13(6):1222–32. doi: 10.1007/s10461-008-9455-4. [DOI] [PubMed] [Google Scholar]
- 25.Peltzer K, Friend-du Preez N, Ramlagan S, Anderson J. Antiretroviral treatment adherence among HIV patients in KwaZulu-Natal, South Africa. BMC Public Health. 2010;10:111. doi: 10.1186/1471-2458-10-111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rintamaki LS, Davis TC, Skripkauskas S, Bennett CL, Wolf MS. Social stigma concerns and HIV medication adherence. AIDS Patient Care STDS. 2006;20(5):359–68. doi: 10.1089/apc.2006.20.359. [DOI] [PubMed] [Google Scholar]
- 27.Sayles JN, Wong MD, Kinsler JJ, Martins D, Cunningham WE. The association of stigma with self-reported access to medical care and antiretroviral therapy adherence in persons living with HIV/AIDS. J Gen Intern Med. 2009;24(10):1101–8. doi: 10.1007/s11606-009-1068-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wohl AR, Galvan FH, Myers HF, et al. Do social support, stress, disclosure and stigma influence retention in HIV care for Latino and African American men who have sex with men and women? AIDS Behav. 2011;15(6):1098–110. doi: 10.1007/s10461-010-9833-6. [DOI] [PubMed] [Google Scholar]
- 29.Dietz E, Clum GA, Chung Se, et al. Adherence to scheduled appointments among HIV-infected female youth in five U.S. cities. J Adolesc Health. 2010;46(3):278–83. doi: 10.1016/j.jadohealth.2009.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Earnshaw VA, Smith LR, Chaudoir SR, Amico KR, Copenhaver MM. HIV stigma mechanisms and well-being among PLWH: a test of the HIV stigma framework. AIDS Behav. 2013;17(5):1785–95. doi: 10.1007/s10461-013-0437-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.WHO. Global HIV/AIDS response: epidemic update and health sector progress towards universal access: progress report 2011. Geneva, Switzerland: World Health Organization; 2011. [Google Scholar]
- 32.UNAIDS. Global report: UNAIDS report on the global AIDS epidemic 2013. Geneva, Switzerland: Joint United Nations Programme on HIV/AIDS (UNAIDS); 2013. Contract No.: UNAIDS / JC2502/1/E. [Google Scholar]
- 33.Bastos FI, Caceres C, Galvao J, Veras MA, Castilho EA. AIDS in Latin America: assessing the current status of the epidemic and the ongoing response. Int J Epidemiol. 2008;37(4):729–37. doi: 10.1093/ije/dyn127. [DOI] [PubMed] [Google Scholar]
- 34.Chi BH, Yiannoutsos CT, Westfall AO, et al. Universal definition of loss to follow-up in HIV treatment programs: a statistical analysis of 111 facilities in Africa, Asia, and Latin America. PLoS Med. 2011;8(10):e1001111. doi: 10.1371/journal.pmed.1001111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Shepherd BE, Blevins M, Vaz LME, et al. Impact of definitions of loss to follow-up on estimates of retention, disease progression, and mortality: Application to an HIV program in Mozambique. Am J Epidemiol. 2013;178(5):819–28. doi: 10.1093/aje/kwt030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Berger BE, Ferrans CE, Lashley FR. Measuring stigma in people with HIV: psychometric assessment of the HIV stigma scale. Res Nurs Health. 2001;24(6):518–29. doi: 10.1002/nur.10011. [DOI] [PubMed] [Google Scholar]
- 37.Franke MF, Muñoz M, Finnegan K, et al. Validation and abbreviation of an HIV stigma scale in an adult spanish-speaking population in urban Peru. AIDS Behav. 2010;14(1):189–99. doi: 10.1007/s10461-008-9474-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Carey MP, Morrison-Beedy D, Johnson BT. The HIV-Knowledge Questionnaire: Development and Evaluation of a Reliable, Valid, and Practical Self-Administered Questionnaire Journal Name: AIDS and Behavior. AIDS Behav. 1997;1(1):61–74. [Google Scholar]
- 39.O'Brien K, Wortman CB, Kessler RC, Joseph JG. Social relationships of men at risk for AIDS. Soc Sci Med. 1993;36(9):1161–7. doi: 10.1016/0277-9536(93)90236-w. [DOI] [PubMed] [Google Scholar]
- 40.Diez-Quevedo C, Rangil T, Sanchez-Planell L, Kroenke K, Spitzer RL. Validation and utility of the patient health questionnaire in diagnosing mental disorders in 1003 general hospital Spanish inpatients. Psychosom Med. 2001;63(4):679–86. doi: 10.1097/00006842-200107000-00021. [DOI] [PubMed] [Google Scholar]
- 41.Logie C, Gadalla TM. Meta-analysis of health and demographic correlates of stigma towards people living with HIV. AIDS Care. 2009;21(6):742–53. doi: 10.1080/09540120802511877. [DOI] [PubMed] [Google Scholar]
- 42.Emlet CA, Brennan DJ, Brennenstuhl S, et al. Protective and risk factors associated with stigma in a population of older adults living with HIV in Ontario, Canada. AIDS Care. 2013;25(10):1330–9. doi: 10.1080/09540121.2013.774317. [DOI] [PubMed] [Google Scholar]
- 43.Fleishman JA, Yehia BR, Moore RD, Korthuis PT, Gebo KA. Establishment, Retention, and Loss to Follow-Up in Outpatient HIV Care. J Acquir Immune Defic Syndr. 2012;60(3):249–59. doi: 10.1097/QAI.0b013e318258c696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Giordano TP, Visnegarwala F, White AC, Jr, et al. Patients referred to an urban HIV clinic frequently fail to establish care: factors predicting failure. AIDS Care. 2005;17(6):773–83. doi: 10.1080/09540120412331336652. [DOI] [PubMed] [Google Scholar]
- 45.Howe CJ, Cole SR, Napravnik S, Eron JJ. Enrollment, retention, and visit attendance in the University of North Carolina Center for AIDS Research HIV clinical cohort, 2001-2007. AIDS Res Hum Retroviruses. 2010;26(8):875–81. doi: 10.1089/aid.2009.0282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gardner LI, Metsch LR, Anderson-Mahoney P, et al. Efficacy of a brief case management intervention to link recently diagnosed HIV-infected persons to care. AIDS. 2005;19(4):423–31. doi: 10.1097/01.aids.0000161772.51900.eb. [DOI] [PubMed] [Google Scholar]
- 47.Greenland S. Introduction to Regression Models. In: Rothman KJ, Greenland S, Lash TL, editors. Modern Epidemiology. 3rd. Philadelphia: Lippincott Williams & Wilkins; 2008. [Google Scholar]
- 48.Nachega JB, Morroni C, Zuniga JM, et al. HIV-Related Stigma, Isolation, Discrimination, and Serostatus Disclosure: A Global Survey of 2035 HIV-Infected Adults. JInt Assoc Physicians AIDS Care. 2012;11(3):172–8. doi: 10.1177/1545109712436723. [DOI] [PubMed] [Google Scholar]
- 49.Sengupta S, Banks B, Jonas D, Miles MS, Smith GC. HIV interventions to reduce HIV/AIDS stigma: a systematic review. AIDS Behav. 2011;15(6):1075–87. doi: 10.1007/s10461-010-9847-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Stangl AL, Lloyd JK, Brady LM, Holland CE, Baral S. A systematic review of interventions to reduce HIV-related stigma and discrimination from 2002 to 2013: how far have we come? J Int AIDS Soc. 2013;16(3 Suppl 2):18734. doi: 10.7448/IAS.16.3.18734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hatzenbuehler ML, O'Cleirigh C, Mayer KH, Mimiaga MJ, Safren SA. Prospective associations between HIV-related stigma, transmission risk behaviors, and adverse mental health outcomes in men who have sex with men. Ann Behav Med. 2011;42(2):227–34. doi: 10.1007/s12160-011-9275-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Logie C, James L, Tharao W, Loutfy M. Associations Between HIV-Related Stigma, Racial Discrimination, Gender Discrimination, and Depression Among HIV-Positive African, Caribbean, and Black Women in Ontario, Canada. AIDS Patient Care STDS. 2013;27(2):114–22. doi: 10.1089/apc.2012.0296. [DOI] [PubMed] [Google Scholar]
- 53.Tanney MR, Naar-King S, MacDonnel K. Depression and stigma in high-risk youth living with HIV: a multi-site study. J Pediatr Health Care. 2012;26(4):300–5. doi: 10.1016/j.pedhc.2011.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Wohl AR, Galvan FH, Carlos JA, et al. A Comparison of MSM Stigma, HIV Stigma and Depression in HIV-Positive Latino and African American Men who have Sex with Men (MSM) AIDS Behav. 2012 doi: 10.1007/s10461-012-0385-9. [DOI] [PubMed] [Google Scholar]
- 55.Chaudoir SR, Norton WE, Earnshaw VA, Moneyham L, Mugavero MJ, Hiers KM. Coping with HIV stigma: do proactive coping and spiritual peace buffer the effect of stigma on depression? AIDS Behav. 2012;16(8):2382–91. doi: 10.1007/s10461-011-0039-3. [DOI] [PubMed] [Google Scholar]
- 56.Pungrassami P, Kipp AM, Stewart PW, Chongsuvivatwong V, Strauss RP, Van Rie A. Tuberculosis and AIDS stigma among patients who delay seeking care for tuberculosis symptoms. Int J Tuberc Lung Dis. 2010;14(2):181–7. [PMC free article] [PubMed] [Google Scholar]
- 57.Paz J, Ugarte-Gil C, Valenzuela C, et al. Challenges in finding HIV patients who have dropped out of care after diagnosis at an HIV reference service in Lima, Peru. American Society for Topical Medicine and Hygiene Annual Meeting; November 14-16; Washington, DC. 2013. [Google Scholar]


