Abstract
With an estimated 200,000 anterior cruciate ligament reconstructions performed annually in the United States, there is an emphasis on determining patient-specific information to help educate patients on expected clinically relevant outcomes. The Multicenter Orthopaedic Outcomes Network consortium was created in 2002 to enroll and longitudinally follow a large population cohort of anterior cruciate ligament reconstructions. The study group has enrolled >4,400 anterior cruciate ligament reconstructions from seven institutions to establish the large level I prospective anterior cruciate ligament reconstruction outcomes cohort. The group has become more than a database with information regarding anterior cruciate ligament injuries; it has helped to establish a new benchmark for conducting multicenter, multisurgeon orthopaedic research. The changes in anterior cruciate ligament reconstruction practice resulting from the group include the use of autograft for high school, college, and competitive athletes in their primary anterior cruciate ligament reconstructions. Other modifications include treatment options for meniscus and cartilage injuries, as well as lifestyle choices made after anterior cruciate ligament reconstruction.
Anterior cruciate ligament (ACL) tears are the most common orthopaedic knee ligament injuries, with younger, more active persons at highest risk. These injuries can result in impaired function, especially during high-level competitive sports;1 thus, the standard of care for a ruptured ACL in persons who place a high demand on the ligament is an arthroscopic autograft reconstruction of the damaged ligament.2 It is estimated that 175,000 to 200,000 ACL reconstructions are performed annually in the United States.3 The rationale is to restore knee biomechanics, thus allowing patients to return to cutting and pivoting sports, as well as minimizing the risk of subsequent menisci and articular cartilage damage, and potentially retarding the process of posttraumatic knee joint osteoarthritis. With an increasingly active population and increased numbers of injuries, emphasis needs to be placed on high-quality research related to ACL reconstruction, rehabilitation, and prevention to establish patient-specific predictive models of clinically important outcomes.
The original concept for the Multicenter Orthopaedic Outcomes Network (MOON) was originated in 1993 by the three senior authors (Dr. Parker, Dr. Spindler, Dr. Andrish). This was first known as the Vanderbilt Sports Medicine–Cleveland Clinic Foundation ACL Reconstruction Registry. These early studies identified the following factors as independent predictors of poor outcome at 5 years: an audible pop at the time of injury, a recent weight increase, and a lower number of years of education.4 The initial efforts evolved into the inclusion of seven institutions (Cleveland Clinic Foundation, Vanderbilt Orthopaedic Institute, The Ohio State University, University of Iowa, Washington University, Hospital for Special Surgery, and University of Colorado) with 17 surgeons; >4,400 ACL reconstructions have been registered to establish the largest prospective longitudinal ACL reconstruction cohort in the United States.
Inter-rater Agreement Among Surgeons
In the setting of a multicenter trial with multiple surgeons, it is imperative to have reliable and reproducible arthroscopic evaluation and documentation of the intra-articular pathology. Prior to enrolling patients into the MOON cohort, a validated consensus on pathology definitions, as well as inter-rater agreement tests for meniscal and articular cartilage pathology, was completed. Multi-rater kappa statistics were used to measure agreement among surgeons; kappa represents a chance-adjusted statistic used to evaluate the observed agreement present between raters that is beyond the agreement due to chance alone. Expected agreement (ie, the probability that two surgeons provide the same response to a specific question regarding any given patient) and observed agreement (ie, the probability that two surgeons give the same response to a specific question for a specific patient) contribute to kappa statistics (Table 1):
Table 1.
Criteria to Evaluate Kappa Agreement Statistics
| Κappa Value | Interpretation |
|---|---|
| Below 0.0 | Poor agreement |
| 0.00-0.20 | Slight agreement |
| 0.21-0.40 | Fair agreement |
| 0.41-0.60 | Moderate agreement |
| 0.61-0.80 | Substantial agreement |
| 0.81-1.00 | Almost perfect agreement |
Dunn et al5 validated the classification of meniscal lesions, with seven surgeons reviewing arthroscopic videos of 18 meniscal tears. With an observed agreement of type (73%, κ = 0.63), location (87%, κ = 0.67), and treatment (84%, κ = 0.66) of the meniscal tears, it was concluded that surgeons may grade meniscal tears through the arthroscope reliably and reproducibly. Meanwhile, Marx et al6 studied the validity of articular cartilage pathology, with six surgeons reviewing 53 arthroscopic videos of articular cartilage pathology. Overall, the observed agreement was 80% (κ = 0.47). All medial and lateral articular lesions were in substantial to almost perfect agreement, with the exception of the medial (κ = 0.34) and lateral (κ = 0.51) tibial plateau. The patella had almost perfect agreement and the trochlea had substantial agreement. Therefore, arthroscopic grading of cartilage lesions was reproducible among the different centers with multiple surgeons.
The Use of Patient-reported Outcome Measures
During the last decade in medical outcomes research, a paradigm shift has occurred, changing from a focus on clinician-derived outcome measures to the addition of psychometrically designed patient-reported outcome (PRO) measures. These new tools have been tested and validated and are typically one of two types of measures, general health or disease specific. One of the advantages of PRO measures is that they are self-administered; thus, evaluator bias is eliminated. In the prospective longitudinal cohort design of the MOON group, a series of five validated outcome measures were collected at baseline (within 2 weeks of surgery) and again at follow-up (at a minimum of 2 years and 6 years after ACL reconstruction). The PRO instruments used were administered in the following sequence: the Knee Injury and Osteoarthritis Outcome Score (KOOS, five subscales), the Western Ontario and McMaster Universities (WOMAC) Osteoarthritis Index, the Marx Activity Rating Scale, the Medical Outcomes Study 36-Item Short Form, and the International Knee Documentation Committee subjective knee evaluation form.
The KOOS assesses sports injuries in young and middle-aged athletes. This tool helps to evaluate both short- and long-term effects of the injury and the potential for the development of osteoarthritis.7 The five subscale measures include pain, symptoms, activities of daily living, sports and recreation function, and knee-related quality of life. The most responsive subscale of the KOOS is the knee-related quality of life. The WOMAC is a PRO that is condition-specific for osteoarthritis for the lower extremity. This is the most frequently used PRO for the lower extremity because of its sensitivity to change and efficacy of use.8-11 The WOMAC is completely contained within the KOOS subscales of pain, symptoms, and activities of daily living.
The Marx Activity Rating Scale is an activity assessment that is used in conjunction with joint-specific and general health outcome measures.12 This scale evaluates the level of symptoms and disability of the patient in relation to his or her activity level. The patient is asked about the components of physical function that are common to different sporting activities; the scale consists of four questions that assess the patient’s ability to run, cut, decelerate, and pivot. Each one of these activities is scored on a scale from 0 (performing the task <1 time per month) to 4 (performing the task >4 times per week) for a total of 16 points. The score has been shown to positively correlate with patient activity and returning to pivoting sports and to correlate inversely with age.12,13
The Medical Outcomes Study 36-Item Short Form is a general health PRO measure. This scale may be used to compare musculoskeletal and non-musculoskeletal diseases and conditions across the medical spectrum.14 This is the most frequently used general health outcome measure, and it has an important role in health policy development as well as clinical practice and research.15
The International Knee Documentation Committee is a knee-specific PRO measure. This measure was psychometrically designed as a PRO questionnaire in 1999 by the American Orthopaedic Society of Sports Medicine.16 The strength of this form lies in its simplicity (18 questions) and its ability to assess any knee condition.
Lessons for Clinical Decision Making
Preoperative Factors of Knee Pain
It has been postulated that increased knee pain at the time of ACL reconstruction may predict a more difficult rehabilitation, a prolonged time to pain-free recovery, and/or be associated with more knee pain at 2 years after surgery. Dunn et al17 prospectively investigated in the MOON cohort the effect of various preoperative factors on knee pain at index ACL reconstruction. Of the 525 patients analyzed, 419 patients (80%) presented with a bone bruise on MRI. Bone bruises were present in younger patients with a mechanism not involving jumping; however, bone bruises were not found to have any effect on pain or symptoms. A multivariable analysis was completed; increased pain and symptoms at the time of ACL reconstruction were associated with higher body mass index (BMI), female gender, and concurrent lateral collateral ligament injury.
Concomitant Intra-articular Pathology
During ACL reconstruction, concomitant intra-articular pathologies, such as meniscal tears and articular cartilage injuries, are usually present. Borchers et al18 studied these injuries in the MOON and the Multicenter ACL Revision Study (MARS) prospective cohorts. Five hundred eight patients (taken from the MOON cohort) underwent primary ACL revision (ACLR), and 281 patients (taken from the MARS cohort) underwent revision reconstruction. Meniscal injuries were the most common injury found in both the primary and the revision procedures; lateral meniscal tears were more common in the primary surgery cohort, and the prevalence of medial meniscal tears was similar between the primary and revision groups. This study also confirmed that a history of a previous meniscectomy is a risk factor for future chondral damage in both the medial and the lateral compartments. Previous meniscectomies play a greater role in chondral damage than does an ACL rupture alone in both primary and revision ACL reconstructions.
With the high prevalence of meniscal tears associated with ACL tears, meniscal repairs are a necessary component of the ACL reconstruction procedure to help minimize the potential for posttraumatic osteoarthritis. Toman et al19 retrospectively reviewed a prospective cohort of 437 ACL reconstructions with 82 concomitant meniscal repairs (54 medial and 28 lateral) with a minimum 2-year follow-up. Longitudinal tears were the most common type of meniscal tear present in both the medial and the lateral compartments. Most of these tears were repaired with an all-inside technique (65 of 82 patients [80%]). Overall, regardless of the repair technique, a 96% clinical success rate was seen at 2-year follow-up, defined as no repeat surgery for clinically symptomatic re-tears.
Graft Choice
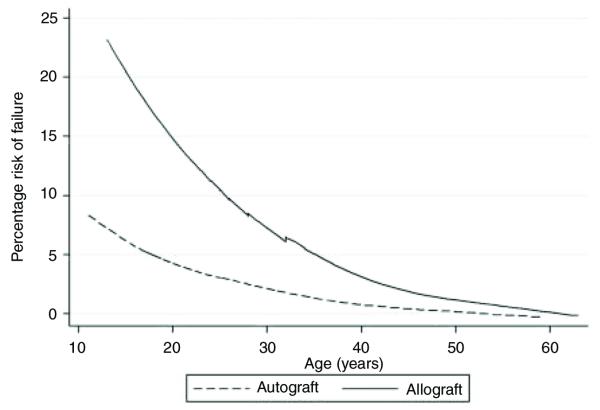
A tear of the reconstructed ACL graft can be a devastating event, with the risk factor for graft failure largely unknown. Kaeding et al20 prospectively investigated predictors of graft failure in a cohort of approximately 1,000 ACLRs. A predictive regression model was created by a single surgeon’s ACL reconstruction collection over a 2-year period. This was then validated with data from the rest of the MOON cohort. Using multivariable analysis, ACL graft choice and patient age were the most predictive variables of graft failure across all surgeons. Reconstruction with an allograft had a rate of failure that was four times higher than that of reconstruction with autograft. Patients who were aged 10 to 19 years had the highest risk of failure. For each 10-year decrease in age, the odds of graft failure increased 2.3 times. Patient characteristics (gender and BMI) and surgical considerations (meniscal pathology and revision ACL) were not associated with an increased risk of graft failure. Figure 1 demonstrates the risk of reinjury in patients with autograft versus allograft reconstructions, as well as the age of the patient at failure.
Figure 1.
Probability of re-tear (in percentage on vertical axis) for autograft versus allograft by age for the combined consortium cohort.
Intraoperative Decision Making
Inappropriate tunnel placement is thought to be the most common technical and preventable cause of ACL reconstruction failure, leading to poor anterior-posterior rotational stability and/or increased graft stress that can be a risk factor for failure. Revision surgery is more technically challenging than primary reconstruction, and the outcomes are significantly poorer.21,22 Thus, preventing these failures is imperative. Several postoperative imaging techniques have been described to analyze tunnel placement accuracy.
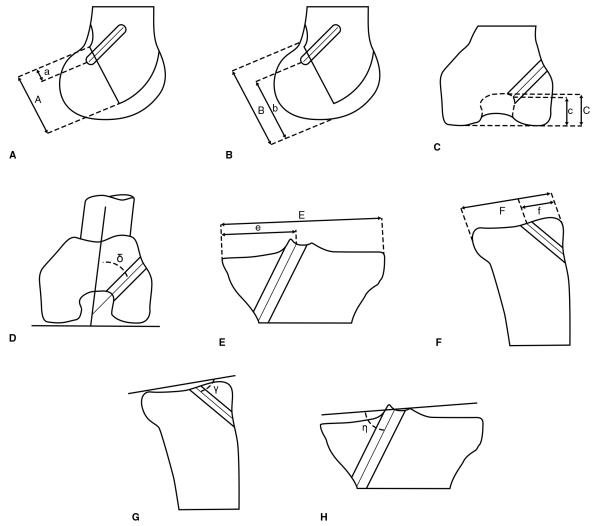
Sullivan et al23 investigated the reliability of various radiographic measurements of ACL tunnels. This was performed by 12 MOON surgeons in 73 cadaver specimens. The measurements included those described by Harner et al,24 Aglietti et al,25 and Jonsson et al26 (Figure 2).
Figure 2.
Illustrations describing each radiographic measurement. A, Harner et al24 (%). B, Aglietti et al25/Jonsson et al26 (%). C, Notch height (%). D, Clock face on Rosenberg view (degrees). E, Tibial medial-lateral position (%). F, Tibial anterior-posterior position (%). G, Tibial sagittal tunnel angle (degrees). H, Tibial coronal tunnel angle (degrees).
Intraclass correlation coefficients were used to determine the reliability of these measurements: excellent, >0.75; good, 0.4 to 0.7; and poor, <0.40. For most of the measurements, the reliability of ACL tunnels measures was good to excellent. Excellent reliability was found for the tibial tunnel angle and tunnel measurement, the clock-face measurement, and the measurements by Aglietti et al25 and Jonsson et al.26
Meanwhile, Wolf et al27 evaluated the MOON intersurgeon and intrasurgeon variability of ACL tunnel placement. Seventy-eight patients who underwent ACL reconstruction by eight MOON surgeons were investigated by means of postoperative CT. These MOON surgeons were relatively consistent with their ACL tunnel placement; 85% of the femoral tunnels and 90% of the tibial tunnels were placed within literature-based guidelines (Figures 3 and 4).
Figure 3.
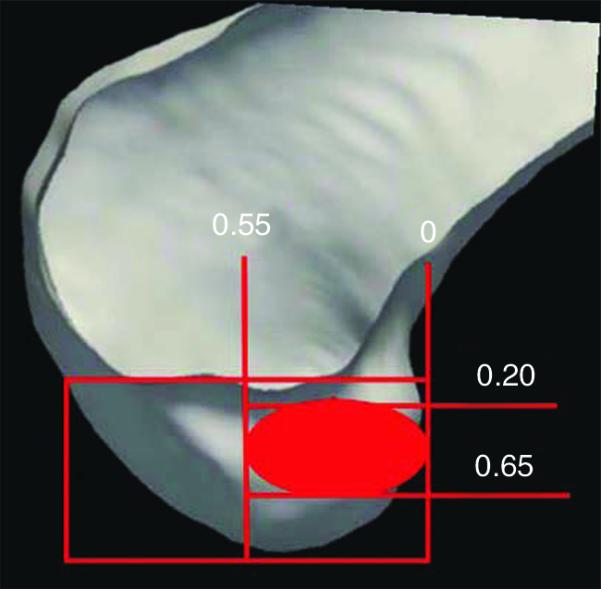
Sagittal three-dimensional CT demonstrating acceptable femoral tunnel placement ranges for depth (c/C) of 0 to 0.55 and height (n/N) of 0.2 to 0.65. The depth was calculated as a percentage of the anterior-to-posterior dimension of the lateral femoral condyle (c/C) with the posterior edge of the condyle as 0%. Tunnel height is the maximal height of the intracondylar notch with the notch apex designated as 0% (n/N).
Figure 4.
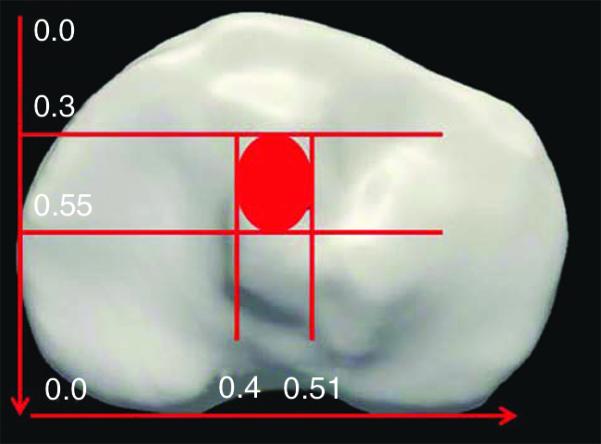
Axial three-dimensional CT demonstrating acceptable tibial tunnel placement ranges for anterior to posterior (a/A) of 0.3 to 0.55 and medial to lateral (m/M) of 0.4 to 0.51. Tibial tunnel aperature location is calculated as a percentage of plateau width from the medial edge of the tibia (m/M). The depth of the tibia plateau is measured from the anterior edge (a/A).
In terms of intrasurgeon variability, consistency between surgeons was evident; however, tunnel placement was variable in regard to condylar depth. This was postulated to be the result of differences in individual surgeons’ tunnel placement preference, but ultimately these differences were not felt to be clinically significant.
Finally, McConkey et al28 investigated arthroscopic agreement of ACL tunnel placement using transtibial, medial portal, or two-incision techniques. This study was performed on a single day in a cadaver wet laboratory with 12 MOON knee surgeons. The surgeons were chosen in a manner to ensure that there was an even distribution of surgeons who performed each of these ACL reconstruction techniques. Additionally, experience level was recorded, and each technique had two surgeons with >9 years of clinical experience after fellowship and two surgeons with <6 years of clinical experience.
Tunnel placement was evaluated arthroscopically by the operating surgeon and an independent reviewing surgeon. Tunnels were also evaluated by three-dimensional (3D) CT imaging. Overall, it was concluded that surgeons do not agree on the appropriate placement of single-bundle ACL tunnels. Operating surgeons were more likely to approve of their tunnels compared with the reviewing surgeon. Meanwhile, the reviewing surgeon was found to provide a more critical evaluation compared with the reports issued based on the 3D CT findings. Finally, it was subjectively concluded that the transtibial technique yielded more poorly placed tunnels.
Rehabilitation
Wright et al29,30 performed a two-part systematic review of the level I and II literature evaluating rehabilitation after ACL reconstruction. To establish evidence-based MOON postoperative ACL reconstruction guidelines, a thorough analysis of the literature resulted in a total of 54 studies for this review. Continuous passive motion was found to have no rehabilitation benefit, with increasing costs to the patient. Early knee range of motion was deemed safe, and its use was felt to prevent arthrofibrosis. Meanwhile, immediate weight bearing was observed to be beneficial and was believed to decrease patellofemoral pain. Any type of postoperative bracing did not offer any rehabilitation advantage compared with no bracing. Home-based rehabilitation was found to be safe, leading to successful ACL reconstruction rehabilitation with no complications.
The second part of this systematic review focused on specific individual aspects of the rehabilitation process.29 Closed-chain exercises were observed to be the appropriate protocol for the first 6 weeks of rehabilitation. High-intensity neuromuscular electrical stimulation was considered safe to implement in the early rehabilitation phase. It is believed that this stimulation may help to improve quadriceps strength, but it was not deemed necessary for a successful rehabilitation. Finally, an accelerated rehabilitation protocol with recovery by 5 to 6 months was found to be safe. The information from both of these systematic reviews, as well as the input of physical therapists, was used to design standardized rehabilitation guidelines for the MOON group.
Postoperative Outcomes and Predictors after Anterior Cruciate Ligament Reconstruction
Dunn et al31 prospectively evaluated the MOON database for predictors of Marx activity level at 2 years following ACL reconstruction. In the MOON cohort, 45% of patients were able to return to the same or higher level of activity. The strongest predictor for return to activity was the patients’ preoperative activity level. An additional factor for return to activity was a low BMI. Factors that were associated with a lower level of activity after surgery were female gender, smoking within 6 months before surgery, and ACLR.
In terms of return to specific sports, the MOON group investigated the return to play in football and soccer athletes within the cohort. McCullough et al32 studied the return to play for high school-level and college-level football. The rate of return to play was similar between the two groups (high school, 63%; college, 69%). When these athletes were interviewed, 43% returned to their previous level of play, 27% returned to a lower level of play, and 30% were not able to return to play. Of the athletes who did not return to play, 50% cited fear of reinjury or further damage as the critical factor for not returning to play at any level of competition.
Meanwhile, Brophy et al33 studied the return to play and future ACL injury risk after ACL reconstruction in soccer athletes. Overall, 72% of these athletes (76% male, 67% female) were able to return to play at an average of 12.2 to 14.3 months following reconstruction. Of this group, 85% were able to return to the same level of play as that before their injury or a higher level of play than that before their injury.
At an average 7-year follow-up, only 36% of the athletes were still playing; older athletes and females were less likely to return to soccer. Within this cohort, there were 12 additional ACL injuries (9 contralateral, 3 ipsilateral), with females more likely to undergo additional ACL surgery. Furthermore, the authors found that athletes who had ACL reconstruction on the nondominant leg had a higher rate of contralateral ACL reconstruction (16%) than did those who had ACL reconstruction on the dominant leg (3.5%).
Hettrich et al34 examined the rate of subsequent surgery at short-term (2 years) and mid-term (6 years) follow-up in 980 patients. At 6-year follow-up, 285 of 905 patients underwent further knee surgery: ipsilateral knee (185 patients, 18.9%) and contralateral knee (100 patients, 10.2%). The rates of ipsilateral ACL graft rupture and contralateral normal ACL tears were similar (7.7% versus 6.4%, respectively). Risk factors for subsequent surgery were younger age at the index reconstruction and the use of allograft.
Complications
Anterior Cruciate Ligament Graft Rupture
The most distressing complication of an ACL reconstruction is a rupture of the reconstructed ACL graft. The graft may fail as a result of traumatic overload, poor surgical technique, undiagnosed concurrent knee injuries, or failure of the graft to biologically incorporate. At a minimum 5-year follow-up, graft rupture rates have been estimated to be 5.8%.35 Wright et al36 found that ACLR reconstructions have worse patient-reported outcomes than do primary reconstructions. The MARS group is a large multicenter (52 sites), multisurgeon (83 participating surgeons), prospective cohort that was developed to determine modifiable predictors of clinical outcome.
The MARS group, consisting of 87 surgeons contributing 460 patients, described the epidemiology of this devastating reinjury.37 The most commonly reported single mode of failure was traumatic reinjury (32%), followed by technical error (24%); femoral tunnel placement was reported as the most common cause of technical failure. Graft choice for the initial reconstruction was autograft (70%), followed by allograft (27%). Meanwhile, for the revision procedure, allograft was the most commonly used graft, followed by autograft. The most frequently used surgical technique for the initial surgery was arthroscopic single incision (81%), followed by arthroscopic two-incision (16%). Articular cartilage and meniscal injuries were very common in this population.
Contralateral Anterior Cruciate Ligament Rupture
Wright et al38 investigated contralateral ACL injury during the first 2 years after ACL reconstruction. In an evaluation of 235 patients, there were 14 ACL injuries that included 7 injuries of the intact contralateral knee (3%) and 7 injuries of the ipsilateral reconstructed knee (3%). Meanwhile, Wright et al38 performed a systematic review of six level I and II prospective studies with a minimum 5-year follow-up of 2,026 patients. The authors’ findings showed the risk of ACL graft rupture in the ipsilateral knee to be half that of the contralateral normal knee (5.8% and 11.8%, respectively).
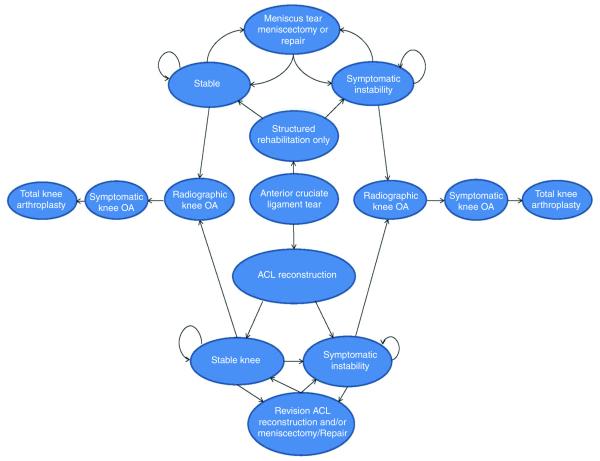
Societal and Economic Impact of Anterior Cruciate Ligament Tears
Mather et al39 investigated the short- and long-term outcomes of ACL injuries and treatment. The cost-effectiveness of ACL reconstruction was compared with patients who were treated with only rehabilitation at 10 weeks or less. A Markov decision model was applied to a cohort of patients from the MOON database to estimate the total societal savings associated with ACL reconstruction (Figure 5). This model compared direct medical costs with indirect costs, such as lost wages from work and disability payment for both the surgical and the nonsurgical groups. Quality-adjusted life years (QALYs) were used to determine treatment effectiveness, with the costs based on the 2012 United States dollar.
Figure 5.
Health state diagram. The diagram demonstrates the clinical pathway of patients within the decision model. Patient health states include either a stable or an unstable knee, and patients can undergo reoperation consisting of meniscal repair, meniscectomy, manipulation under anesthesia, or hardware removal. ACL = anterior cruciate ligament, OA = osteoarthritis.
Short-to-intermediate results found that the mean incremental cost of ACL reconstruction was $4,503 less than that of rehabilitation, with reconstruction providing an incremental QALY gain of 0.18. For a person undergoing ACL reconstruction, long-term outcomes determined that the mean lifetime cost to society was $38,121, compared with $88,538 for a patient who was treated with rehabilitation only, with a QALY gain of 0.72. The authors concluded that limiting ACL reconstruction potentially could be harmful to not only the patient because of the risk of the development of knee osteoarthritis, but also to society because ACL reconstruction demonstrated improved QALY at a lower cost compared with rehabilitation.
MOON Impact on Orthopaedics
The MOON group is not a registry of ACL reconstructions, but rather a hypothesis-driven, prospective, longitudinal population cohort designed to determine prognosis and predictors of ACLR outcomes. The impact has been to provide a model for multicenter, multisurgeon orthopaedic research and comparative effectiveness research in orthopaedics. This challenges the current experience-based physician decision-making model, replacing it with higher-level evidence for physicians to use in discussion with patients about their prognosis, treatment options, and lifestyle choices that affect the knee. For example, the knowledge that failure of ACL reconstruction is age- and allograft-dependent has led to changes in clinical practice; surgeons now avoid the use of allograft in young athletes.
Furthermore, the MOON group has led to several spinoff ventures. Not only has the MARS group for ACLR been launched, but most Meniscal Tear and Osteoarthritis Research (MeTeOR) sites have been established where MOON and MARS study groups are present. MeTeOR is a multicenter randomized controlled trial comparing surgical and nonsurgical management for mild to moderate osteoarthritis with meniscal injury; the results have influenced our treatment algorithms for these patients.40,41 The MOON Shoulder group has also been established. Additionally, the KOOS patient-reported outcome measure is similar to the outcome measures in the Swedish and Norwegian ACL registries, thus allowing for cross-cultural collaboration for discovery of common modifiable predictors to improve ACL reconstruction outcomes42
Future
MOON has laid a foundation on several future fronts. First, the modifiable predictors of ACLR outcomes thus far identified provide opportunities for further investigation (when appropriate) in randomized controlled trials. For example, we expect to perform an ACL prevention trial using neuromuscular training techniques on patients at the highest risk who have been identified within the MOON cohort. Other potential clinical trials include using the latest tissue engineering technology to substitute for meniscus loss or for grade III and IV articular cartilage injuries to determine if outcomes can be improved. Second, the high follow-up rate (approximately 85%) reported with patient-reported outcomes can serve as a model for monitoring clinical practice or for comparative effectiveness in discrete episodes of care, such as an acute injury or surgery. Third, we are currently exploring the relationship between patient-reported outcomes and physical examination and structural measures (eg, radiographs, KT-1000, functional hop testing); these studies should provide interesting insights. Finally, the results thus far suggest that a minimum 10-year follow-up may be required to differentiate the clinically successful ACLR and the avoidance of posttraumatic osteoarthritis from the ACLRs that have poor outcomes with or without osteoarthritis.
Summary
It has been 10 years since the first MOON publication, with more than 40 subsequent publications to date. The investigations that have been identified from this prospective longitudinal cohort will continue to help clarify modifiable and nonmodifiable predictors related to injury, intraoperative decision making and treatment, postoperative rehabilitation, and behavioral characteristics that contribute to a spectrum of clinically relevant outcomes. This has subsequently had a direct impact on providing both the physician and the patient with the highest quality evidence (ie, prospective longitudinal cohort) for decision making, with the goal of improving the outcomes of most ACL reconstructions.
Acknowledgments
The project described was partially funded by Grant Number 5R01 AR053684 (K.P.S.) and Number 5K23 AR052392 (W.R.D.) from the National Institutes of Health/National Institute of Arthritis and Musculoskeletal and Skin Diseases, and by Grant Number 5 U18-HS016075 (R.G.M.) from the Center for Education and Research on Therapeutics (Agency of Health Research and Quality). The initial development of the project was partially funded by a grant from the Orthopaedic Research and Education Foundation, and additional support was provided by the Vanderbilt Sports Medicine Research Fund. Vanderbilt Sports Medicine received unrestricted educational gifts from Smith & Nephew Endoscopy and DonJoy Orthopaedics.
Footnotes
Dr. Parker or an immediate family member has received royalties from Zimmer; is a member of a speakers’ bureau or has made paid presentations on behalf of Smith & Nephew Endoscopy and Zimmer; serves as a paid consultant to Zimmer and Smith & Nephew; and has received research or institutional support from Zimmer. Dr. Andrish or an immediate family member serves as a board member, owner, officer, or committee member of the International Society of Arthroscopy, Knee Surgery, and Orthopaedic Sports Medicine. Dr. Spindler or an immediate family member has received research or institutional support from the Arthritis Foundation and the National Institutes of Health (National Institute of Arthritis and Musculoskeletal and Skin Diseases and the National Institute of Child Health and Human Development), and serves as a board member, owner, officer, or committee member of the American Orthopaedic Society for Sports Medicine, NFL Charities, and the Orthopaedic Research Society. Neither of the following authors nor any immediate family member has received anything of value from or has stock or stock options held in a commercial company or institution related directly or indirectly to the subject of this article: Dr. Lynch and Dr. Patel.
Other contributing authors of the MOON group include: Annunziata Amendola, MD; Robert H. Brophy, MD; Warren R. Dunn, MD, MPH; David C. Flanigan, MD; Laura J. Huston, MS; Morgan H. Jones, MD, MPH; Christopher C. Kaeding, MD; Robert G. Marx, MD, MSc; Matthew J. Matava, MD; Eric C. McCarty, MD; Angela D. Pedroza, MPH; Emily K. Reinke, PhD; Brian R. Wolf, MD, MS; Rick W. Wright, MD.
The Impact of the MOON Research on Anterior Cruciate Ligament Reconstruction and Orthopaedic Practice
T. Sean Lynch, MD, et al
References
Evidence-based Medicine: Levels of evidence are described in the table of contents. In this article, references 13, 26, and 41 are level I studies. References 1, 4, 17, 18, 20, 21, 24, 29-31, and 35-39 are level II studies. References 32-34 are level III studies. References 19, 22, and 25 are level IV studies. References printed in bold type are those published within the past 5 years.
- 1.Lyman S, Koulouvaris P, Sherman S, Do H, Mandl LA, Marx RG. Epidemiology of anterior cruciate ligament reconstruction: Trends, readmissions, and subsequent knee surgery. J Bone Joint Surg Am. 2009;91(10):2321–2328. doi: 10.2106/JBJS.H.00539. Medline. [DOI] [PubMed] [Google Scholar]
- 2.Marx RG, Jones EC, Angel M, Wickiewicz TL, Warren RF. Beliefs and attitudes of members of the American Academy of Orthopaedic Surgeons regarding the treatment of anterior cruciate ligament injury. Arthroscopy. 2003;19(7):762–770. doi: 10.1016/s0749-8063(03)00398-0. Medline. [DOI] [PubMed] [Google Scholar]
- 3.Gottlob CA, Baker CL, Jr, Pellissier JM, Colvin L. Cost effectiveness of anterior cruciate ligament reconstruction in young adults. Clin Orthop Relat Res. 1999;367:272–282. Medline. [PubMed] [Google Scholar]
- 4.Spindler KP, Warren TA, Callison JC, Jr, Secic M, Fleisch SB, Wright RW. Clinical outcome at a minimum of five years after reconstruction of the anterior cruciate ligament. J Bone Joint Surg Am. 2005;87(8):1673–1679. doi: 10.2106/JBJS.D.01842. Medline. [DOI] [PubMed] [Google Scholar]
- 5.Dunn WR, Wolf BR, Amendola A, et al. Multirater agreement of arthroscopic meniscal lesions. Am J Sports Med. 2004;32(8):1937–1940. doi: 10.1177/0363546504264586. Medline. [DOI] [PubMed] [Google Scholar]
- 6.Marx RG, Connor J, Lyman S, et al. Multicenter Orthopaedic Outcomes Network: Multirater agreement of arthroscopic grading of knee articular cartilage. Am J Sports Med. 2005;33(11):1654–1657. doi: 10.1177/0363546505275129. Medline. [DOI] [PubMed] [Google Scholar]
- 7.Roos EM, Roos HP, Lohmander LS, Ekdahl C, Beynnon BD. Knee injury and osteoarthritis outcome score (KOOS): Development of a self-administered outcome measure. J Orthop Sports Phys Ther. 1998;28(2):88–96. doi: 10.2519/jospt.1998.28.2.88. Medline. [DOI] [PubMed] [Google Scholar]
- 8.Ryser L, Wright BD, Aeschlimann A, Mariacher-Gehler S, Stucki G. A new look at the Western Ontario and McMaster Universities Osteoarthritis Index using Rasch analysis. Arthritis Care Res. 1999;12(5):331–335. doi: 10.1002/1529-0131(199910)12:5<331::aid-art4>3.0.co;2-w. Medline. [DOI] [PubMed] [Google Scholar]
- 9.Wolfe F, Kong SX. Rasch analysis of the Western Ontario McMaster questionnaire (WOMAC) in 2205 patients with osteoarthritis, rheumatoid arthritis, and fibromyalgia. Ann Rheum Dis. 1999;58(9):563–568. doi: 10.1136/ard.58.9.563. Medline. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Angst F, Aeschlimann A, Stucki G. Smallest detectable and minimal clinically important differences of rehabilitation intervention with their implications for required sample sizes using WOMAC and SF-36 quality of life measurement instruments in patients with osteoarthritis of the lower extremities. Arthritis Rheum. 2001;45(4):384–391. doi: 10.1002/1529-0131(200108)45:4<384::AID-ART352>3.0.CO;2-0. Medline. [DOI] [PubMed] [Google Scholar]
- 11.Angst F, Ewert T, Lehmann S, Aeschlimann A, Stucki G. The factor subdimensions of the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) help to specify hip and knee osteoarthritis: A prospective evaluation and validation study. J Rheumatol. 2005;32(7):1324–1330. Medline. [PubMed] [Google Scholar]
- 12.Marx RG, Stump TJ, Jones EC, Wickiewicz TL, Warren RF. Development and evaluation of an activity rating scale for disorders of the knee. Am J Sports Med. 2001;29(2):213–218. doi: 10.1177/03635465010290021601. Medline. [DOI] [PubMed] [Google Scholar]
- 13.Gobbi A, Francisco R. Factors affecting return to sports after anterior cruciate ligament reconstruction with patellar tendon and hamstring graft: A prospective clinical investigation. Knee Surg Sports Traumatol Arthrosc. 2006;14(10):1021–1028. doi: 10.1007/s00167-006-0050-9. Medline. [DOI] [PubMed] [Google Scholar]
- 14.Keller SD, Ware JE, Jr, Hatoum HT, Kong SX. The SF-36 Arthritis-Specific Health Index (ASHI): II. Tests of validity in four clinical trials. Med Care. 1999;37(suppl 5):MS51–MS60. doi: 10.1097/00005650-199905001-00005. Medline. [DOI] [PubMed] [Google Scholar]
- 15.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36): I. Conceptual framework and item selection. Med Care. 1992;30(6):473–483. [PubMed] [Google Scholar]
- 16.Irrgang JJ, Anderson AF, Boland AL, et al. Development and validation of the international knee documentation committee subjective knee form. Am J Sports Med. 2001;29(5):600–613. doi: 10.1177/03635465010290051301. Medline. [DOI] [PubMed] [Google Scholar]
- 17.Dunn WR, Spindler KP, Amendola A, et al. MOON ACL Investigation Which preoperative factors, including bone bruise, are associated with knee pain/symptoms at index anterior cruciate ligament reconstruction (ACLR)? A Multicenter Orthopaedic Outcomes Network (MOON) ACLR Cohort Study. Am J Sports Med. 2010;38(9):1778–1787. doi: 10.1177/0363546510370279. Medline. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Borchers JR, Kaeding CC, Pedroza AD, Huston LJ, Spindler KP, Wright RW, MOON Consortium and the MARS Group Intra-articular findings in primary and revision anterior cruciate ligament reconstruction surgery: A comparison of the MOON and MARS study groups. Am J Sports Med. 2011;39(9):1889–1893. doi: 10.1177/0363546511406871. Medline. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Toman CV, Dunn WR, Spindler KP, et al. Success of meniscal repair at anterior cruciate ligament reconstruction. Am J Sports Med. 2009;37(6):1111–1115. doi: 10.1177/0363546509337010. Medline. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kaeding CC, Aros B, Pedroza A, et al. Allograft versus autograft anterior cruciate ligament reconstruction: Predictors of failure from a MOON prospective longitudinal cohort. Sports Health. 2011;3(1):73–81. doi: 10.1177/1941738110386185. Medline. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wright RW, Dunn WR, Amendola A, et al. MOON Cohort: Anterior cruciate ligament revision reconstruction: Two-year results from the MOON cohort. J Knee Surg. 2007;20(4):308–311. doi: 10.1055/s-0030-1248066. Medline. [DOI] [PubMed] [Google Scholar]
- 22.Battaglia MJ, II, Cordasco FA, Hannafin JA, et al. Results of revision anterior cruciate ligament surgery. Am J Sports Med. 2007;35(12):2057–2066. doi: 10.1177/0363546507307391. Medline. [DOI] [PubMed] [Google Scholar]
- 23.Sullivan JP, Matava MJ, Flanigan DC, et al. MOON Group Reliability of tunnel measurements and the quadrant method using fluoroscopic radiographs after anterior cruciate ligament reconstruction. Am J Sports Med. 2012;40(10):2236–2241. doi: 10.1177/0363546512458086. Medline. [DOI] [PubMed] [Google Scholar]
- 24.Harner CD, Marks PH, Fu FH, Irrgang JJ, Silby MB, Mengato R. Anterior cruciate ligament reconstruction: Endoscopic versus two-incision technique. Arthroscopy. 1994;10(5):502–512. doi: 10.1016/s0749-8063(05)80004-0. Medline. [DOI] [PubMed] [Google Scholar]
- 25.Aglietti P, Buzzi R, Giron F, Simeone AJ, Zaccherotti G. Arthroscopic-assisted anterior cruciate ligament reconstruction with the central third patellar tendon: A 5-8-year follow-up. Knee Surg Sports Traumatol Arthrosc. 1997;5(3):138–144. doi: 10.1007/s001670050041. Medline. [DOI] [PubMed] [Google Scholar]
- 26.Jonsson H, Elmqvist LG, Kärrholm J, Tegner Y. Over-the-top or tunnel reconstruction of the anterior cruciate ligament? A prospective randomised study of 54 patients. J Bone Joint Surg Br. 1994;76(1):82–87. Medline. [PubMed] [Google Scholar]
- 27.Wolf BR, Ramme AJ, Wright RW, et al. MOON Knee Group Variability in ACL tunnel placement: Observational clinical study of surgeon ACL tunnel variability. Am J Sports Med. 2013;41(6):1265–1273. doi: 10.1177/0363546513483271. Medline. [DOI] [PubMed] [Google Scholar]
- 28.McConkey MO, Amendola A, Ramme AJ, et al. MOON Knee Group: Arthroscopic agreement among surgeons on anterior cruciate ligament tunnel placement. Am J Sports Med. 2012;40(12):2737–2746. doi: 10.1177/0363546512461740. Medline. [DOI] [PubMed] [Google Scholar]
- 29.Wright RW, Preston E, Fleming BC, et al. A systematic review of anterior cruciate ligament reconstruction rehabilitation: part II: Open versus closed kinetic chain exercises, neuromuscular electrical stimulation, accelerated rehabilitation, and miscellaneous topics. J Knee Surg. 2008;21(3):225–234. doi: 10.1055/s-0030-1247823. Medline. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wright RW, Preston E, Fleming BC, et al. A systematic review of anterior cruciate ligament reconstruction rehabilitation: part I: Continuous passive motion, early weight bearing, postoperative bracing, and home-based rehabilitation. J Knee Surg. 2008;21(3):217–224. doi: 10.1055/s-0030-1247822. Medline. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Dunn WR, Spindler KP, MOON Consortium Predictors of activity level 2 years after anterior cruciate ligament reconstruction (ACLR): A Multicenter Orthopaedic Outcomes Network (MOON) ACLR cohort study. Am J Sports Med. 2010;38(10):2040–2050. doi: 10.1177/0363546510370280. Medline. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.McCullough KA, Phelps KD, Spindler KP, et al. MOON Group Return to high school- and college-level football after anterior cruciate ligament reconstruction: A Multicenter Orthopaedic Outcomes Network (MOON) cohort study. Am J Sports Med. 2012;40(11):2523–2529. doi: 10.1177/0363546512456836. Medline. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Brophy RH, Schmitz L, Wright RW, et al. Return to play and future ACL injury risk after ACL reconstruction in soccer athletes from the Multicenter Orthopaedic Outcomes Network (MOON) group. Am J Sports Med. 2012;40(11):2517–2522. doi: 10.1177/0363546512459476. Medline. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hettrich CM, Dunn WR, Reinke EK, Spindler KP, MOON Group The rate of subsequent surgery and predictors after anterior cruciate ligament reconstruction: Two- and 6-year follow-up results from a multicenter cohort. Am J Sports Med. 2013;41(7):1534–1540. doi: 10.1177/0363546513490277. Medline. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wright RW, Magnussen RA, Dunn WR, Spindler KP. Ipsilateral graft and contralateral ACL rupture at five years or more following ACL reconstruction: A systematic review. J Bone Joint Surg Am. 2011;93(12):1159–1165. doi: 10.2106/JBJS.J.00898. Medline. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wright R, Spindler K, Huston L, et al. Revision ACL reconstruction outcomes: MOON cohort. J Knee Surg. 2011;24(4):289–294. doi: 10.1055/s-0031-1292650. Medline. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wright RW, Huston LJ, Spindler KP, et al. MARS Group Descriptive epidemiology of the Multicenter ACL Revision Study (MARS) cohort. Am J Sports Med. 2010;38(10):1979–1986. doi: 10.1177/0363546510378645. Medline. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wright RW, Dunn WR, Amendola A, et al. Risk of tearing the intact anterior cruciate ligament in the contralateral knee and rupturing the anterior cruciate ligament graft during the first 2 years after anterior cruciate ligament reconstruction: A prospective MOON cohort study. Am J Sports Med. 2007;35(7):1131–1134. doi: 10.1177/0363546507301318. Medline. [DOI] [PubMed] [Google Scholar]
- 39.Mather RC, III, Koenig L, Kocher MS, et al. MOON Knee Group Societal and economic impact of anterior cruciate ligament tears. J Bone Joint Surg Am. 2013;95(19):1751–1759. doi: 10.2106/JBJS.L.01705. Medline. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Katz JN, Chaisson CE, Cole B, et al. The MeTeOR trial (Meniscal Tear in Osteoarthritis Research): Rationale and design features. Contemp Clin Trials. 2012;33(6):1189–1196. doi: 10.1016/j.cct.2012.08.010. Medline. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Katz JN, Brophy RH, Chaisson CE, et al. Surgery versus physical therapy for a meniscal tear and osteoarthritis. N Engl J Med. 2013;368(18):1675–1684. doi: 10.1056/NEJMoa1301408. Medline. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Magnussen RA, Granan LP, Dunn WR, et al. Cross-cultural comparison of patients undergoing ACL reconstruction in the United States and Norway. Knee Surg Sports Traumatol Arthrosc. 2010;18(1):98–105. doi: 10.1007/s00167-009-0919-5. Medline. [DOI] [PMC free article] [PubMed] [Google Scholar]