Abstract
Introduction
The patterning of the HIV epidemic within young key populations (YKPs) highlights disproportionate burden by mental disorders in these populations. The mental wellbeing of YKPs is closely associated with biological predispositions and psychosocial factors related to YKPs’ sexual and gender identities and socio-economic status. The purpose of this paper is to highlight sources of risk and resilience, as well as identify treatment and supports for mental health disorders (MHDs) among YKPs.
Discussion
This paper utilizes Bronfenbrenner's Bioecological Systems Theory and the Social Stress Model to explore the risk and protective factors for MHDs across YKPs’ ecological systems, and identify current gaps in treatment and support for MHDs among these youth. We emphasize the fluidity and intersections across these categorizations which reinforce the vulnerability of these populations, the lack of concrete data to inform mental health interventions among YKPs, and the need to ground YKP interventions and programmes with human rights principles stipulated in the convention on the rights of a child.
Conclusions
We put forth recommendations for future research and strategies to address the mental wellbeing of YKPs, including the need for integrated interventions that address the multiplicity of risk factors inherent in the multiple group membership, rather than single-focus interventions whilst addressing the unique needs or challenges of YKPs.
Keywords: youth, adolescents, psychiatric disorders, psychosocial, HIV/AIDS, treatment, programmes
Introduction
HIV infection disproportionately affects youth [1–3] , and the patterning of the HIV epidemic within young key populations (YKPs) underscores the role of mental health disorders (MHDs) in structuring vulnerability of these populations to HIV. For the purposes of this article, YKPs will be defined as sexual minority youth (including gay, bisexual, and lesbian youth and young men who have sex with men regardless of their sexual orientation identity); gender minority youth (specifically transgender and gender non-conforming youth); youth who inject drugs; youth involved in sex work; runaway and homeless youth; and detained or incarcerated youth.
MHDs may increase YKPs’ vulnerability to HIV, and/or alter the course of infection among those already living with HIV [4–6]. Among YKPs, MHDs have been linked to HIV risk behaviours such as early sexual debut, high numbers of sexual partners, low condom use, transactional sex, needle sharing, and drug/alcohol use [4–13]; lower uptake, adherence to, and retention in HIV care [14,15]; and increased risk of AIDS mortality [16]. Moreover, HIV infection also increases the risk of MHDs among YKPs [17,18].
Epidemiology of MHDs among YKPs
Although adolescence and emerging adulthood is a time of relative positive physical health as measured by traditional indicators such as rates of mortality, chronic disease burden and hospitalizations, it is also a peak time for developing MHDs [19–21] and health-related challenges stemming from participation in high risk behaviours [22,23]. Studies have consistently reported higher rates of MHDs such as major depression, anxiety, conduct disorder, attention-deficit/hyperactivity disorder (ADHD), substance use disorder, alcohol dependence and abuse, suicide, and post-traumatic stress disorder (PTSD) among sexual minority youth [24–28], gender minority youth [25,27,29,30], youth who inject drugs [20,31], detained or incarcerated youth [32–36], runaway and homeless youth [37–39] and youth involved in sex work [40–42], relative to comparable youth populations. It is important to note that the higher rates of MHDs among YKPs are not due to any inherent dysfunction within these youth, but are closely associated with their membership in socially stigmatized minority groups that experience excessive stress in the form of prejudice-related stressful life events, discrimination, rejection and violence [43–45] .
Sexual minority adult populations have a two-fold excess in suicide attempts, and rates of depression, anxiety and substance use disorders are almost twice as high among sexual minorities compared to heterosexual populations [28]. Among sexual minority youth, a review of MHDs found that one third of participants met the criteria for any MHD including 17% for conduct disorder, 15% for major depression and 9% for PTSD [25]. Studies have reported even higher rates of MHDs among gender minority youth relative to comparable youth populations. A cross-sectional study of 515 gender minority persons found that 60% of participants were depressed; the prevalence of attempted suicide in this sample was 32% [29]. A cross-sectional study of 55 transgender youth found that 45% of participants had seriously considered suicide and 26% had attempted suicide [46], while another study of 571 male-to-female transgender persons in New York found that the lifetime prevalence of major depression among youth in this study was 54.7% [47].
More than two thirds of runaway and homeless youth meet the criteria for two or more MHDs including depression, conduct disorders, ADHD and PTSD [48–52]. Rates of attempted suicide among runaway and homeless youth who self-identify as sexual minorities range between 2 and 42% [26]. Detained or incarcerated youth are 10 times more likely to suffer from psychosis and depression compared to youth in the general population [32]. A nationwide review of 57 juvenile justice agencies (N=9, 819) found that 51.9% of youth met the criteria for a MHD; one third met the criteria for more than one disorder and about a quarter met the criteria for multiple clusters disorders. In this study, 20.4% reported anxiety, 27% reported disruptive behaviour disorder, 14% reported lifetime suicide attempts and 7.9% reported affective disorders [53]. Data on the mental health of youth involved in sex work are rare, but a study in Goa, India, found that 41.5% of female sex workers under 20 years of age had attempted suicide in the past three months [40]. Rates of physical and sexual violence among youth involved in sex work are high, ranging between 18 and 67% [54,55].
Current data point to sex/gender differences in prevalence of MHDs among YKPs. Gay/bisexual male youth have higher rates of panic and depression disorders, while lesbian/bisexual female youth have higher rates of substance abuse [56]. A study of sexual and gender minority youth found that transgender youth had a lower prevalence of all MHDs compared to gay/bisexual youth [25]. Among runaway and homeless youth, rates of drug abuse among were 10 times higher among male youth and 17 times higher among female youth as compared to youth in a nationally representative sample, and alcohol abuse was significantly higher among male youth [52]. Almost twice as many female runaway and homeless youth (25%) had attempted suicide at least once compared to male runaway and homeless youth (14%) [26]. Among detained or incarcerated youth, rates of major depression were twice as high among female youth compared to male youth (29% vs. 10.6%), while young men reported higher rates of psychotic illness (3.3% vs. 2.7%) [32]. These sex/gender differences underscore the diversity in experiences and needs within specific YKPs, which may have significant implications for intervention development. However, more studies are needed to elaborate on these differences.
Cross-cutting issues
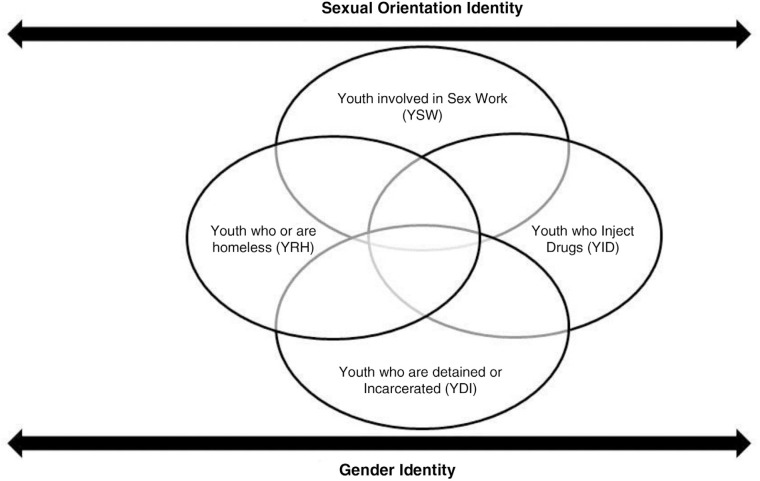
The needs and challenges of YKPs vary with their age, sex, race/ethnicity, gender identity, sexual identity, socio-economic status and geographic region. However, YKPs also share a host of socio-ecological experiences, broadly engendered by their sexual orientation and gender identities, which confer selective risks and vulnerabilities for MHDs and HIV. The categorizations of YKPs are not mutually exclusive (see Figure 1): there is high fluidity and intersections across these categories [57,58]. For example, approximately 30–45% of clients served in homeless youth services are sexual minority youth [59]; compared to heterosexual female youth, lesbian and bisexual youth are over-represented among detained or incarcerated youth [60,61]; homelessness is associated with greater risks for substance abuse [62]; and runaway and homeless youth who also self-identify as gay are more likely to report being tested or treated for HIV compared to bisexual or heterosexual youth [58,63] and are also more likely to engage in substance and alcohol abuse [64].
Figure 1.
Intersection of group membership and identities among young key populations.
This intersectionality of oppressed identities and multiple memberships among YKP categories that experience social marginalization may increase the presence of MHDs. This is supported by the syndemic production theory, which posits that for some marginalized groups (e.g. sexual minority youth), there is a syndemic process of interacting physical and psychosocial challenges (e.g. HIV, substance use, depression, violence) that cause poor health outcomes within these populations [65,66]. For this reason, we emphasize the importance of developing interventions that address the intersectionality of social and cultural identities possessed by YKPs and the multiplicity of risk and resilience factors that may accompany membership in these various groups, rather than single-focus interventions.
Discussion
Theoretical framework
This paper utilizes two theoretical frameworks based on diathesis-stress models, to situate the epidemiology of MHDs among YKPs: Bronfenbrenner's Bioecological Systems Theory (BST) [67,68], and the Social Stress Model (SST) [69–71]. Generally, diathesis-stress models assert that all people have some level of pre-disposing risk factors (biological diathesis) for any given MHD, and that stress activates a diathesis, transforming the potential pre-disposition into an MHD [72–74]. BST is useful in understanding the linkages between biological factors and psychosocial factors in the development of MHDs among YKPs [69,70]. It proposes that an individual is continually impacted by four successive and interconnected levels of influence (i.e. microsystem, mesosystem, exosystem and macrosystem) over their life course; the biological diatheses and ecological stressors may act directly or synergistically to increase an individual's risk for MHDs. SST posits that one's disadvantaged position in the social hierarchy leads to more stressful conditions and fewer resources to counteract these stressors, resulting in greater rates of MHDs.
The microsystem comprises the complex relations between the developing person and the environments in the immediate settings containing the person. The mesosystem is a set of microsystems constituting an individual's developmental niche within a given period of development; mesosystems are more challenging to quantify and represent the assumption that microsystems do not function independently. The exosystem is composed of contexts that do not directly involve the developing person but have an influence on the person's behaviour and development. The macrosystem is the super ordinate ecological level of human development, involving culture, macro-institutions and public policy [75].
BST also provides a useful theoretical framework for understanding nested ecological system factors that influence the mental health and HIV risk/protective behaviours of YKPs, and the reciprocal relationships between youth and their environments. Both the BST and SST enable examination of youth within their social contexts, thereby allowing identification of contextually relevant cultural and developmental risk and protective factors.
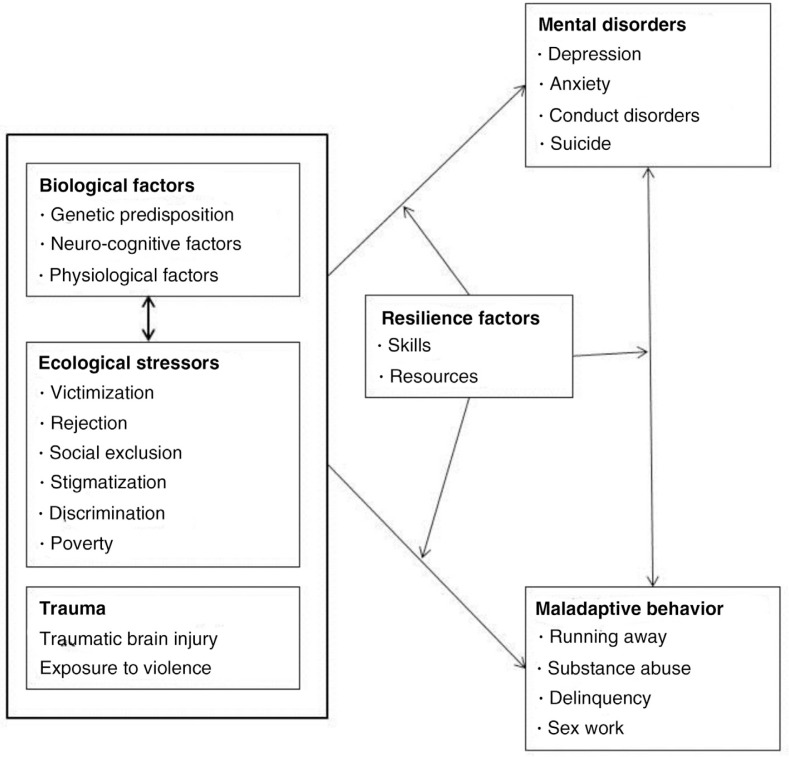
Figure 2 illustrates the adaptation of the SST to MHDs among YKPs. We argue that MHDs among YKPs result from their disadvantaged positions in the social hierarchy within their ecological systems, and this positioning is closely linked to their sexual orientation identity, gender identity and/or socio-economic status [76,77]. Consistent with our diathesis-stress framework, we argue that biological predispositions and ecological stressors may act independently, additively or synergistically to create MHDs and maladaptive HIV risk behaviours, and these pathways may be moderated by resilience factors [78]. This model highlights the reciprocal relationship between maladaptive behaviours and MHDs, which is also moderated by resilience factors.
Figure 2.
A framework using the Social Stress Theory to depict evolution of mental disorders among young key populations.
Risk factors
Microsystem factors could be sub-divided into intrapersonal and interpersonal factors. Intrapersonal factors include biological or cognitive factors that contribute toward certain abnormal states or conditions including genetic factors, inherited traits, neurological anomalies and patterns of psycho-physiological stress responses [73,74,79]. HIV may affect central nervous system structures involved in the regulation of emotion and behaviour, thereby increasing youth's risk of MHDs [80,81]. Additionally, normative developmental processes such as identity development and increased propensity for risk-taking, psychosocial distress manifested by self-esteem, poor self-image, hopelessness, helplessness and internalized homophobia may increase MHDs and HIV risk behaviours among YKPs [45,82–86]. Adolescence is a peak time for traumatic injuries, which, in turn, increase the risk of MHDs and HIV risk behaviours among youth [87,88]. MHDs such as depression, conduct disorder and PTSD and related dimensions of behaviour including coping strategies have been linked to diatheses such as genetic factors, depressogenic cognitive structures, traumatic brain injury and ecological stressors [72,73,87–89].
Interpersonal factors include experiences of victimization, family conflict, family/peer rejection, social isolation, poverty and housing instability [24,42,45,90–98]. Studies have found high rates of childhood maltreatment (physical and sexual abuse) among youth involved in sex work and runaway and homeless youth [99–102]. Childhood maltreatment, especially childhood sexual abuse, has been associated with alcohol use, delinquency and sexual risk behaviour [103–106] and MHDs such as depression and PTSD [107–109]. The pathways through which childhood physical and sexual abuse result in MHDs and HIV risk behaviours are not clearly elucidated but several authors hypothesize that these traumas could influence the development of maladaptive coping skills, maladaptive social information processing, and feelings of hopelessness, vulnerability and loneliness [110,111], leading to MHDs and HIV risk behaviours.
Exosystem factors include school and neighbourhood safety, neighbourhood poverty, stereotypes and representation of YKPs in communities, absence of caring adults, negative experiences with service providers, dearth of trained mental health providers, and geographical and financial barriers to accessing comprehensive and sensitive mental health services [85,112–116]. Exposure to violence, including war and civil strife, contributes significantly to MHDs, especially among youth in low-income countries [117,118]. The macrosystem factors include stigma, discrimination, social and economic marginalization, criminalizing or disenfranchising public policies, and cost of health care services.
All of these systems of influence act individually or synergistically to heighten YKPs’ risk for MHDs and HIV risk behaviours [42,45,112,119–122]. Different types of stressors (acute or chronic) may play different roles in the aetiology of MHDs and HIV risk behaviours. However, within the current research, there is a lack of theoretical attention to the nature and quality of the stressors, and the complex interactions through which biological diatheses and ecological factors influence the development of MHDs among YKPs.
Resilience factors
Despite the host of powerful negative forces, not all YKPs have MHDs or engage in HIV risk behaviours. Many have multiple resilience factors – personal traits or characteristics of their social environment that protect young people from harm and reduce the likelihood of MHDs among vulnerable youth [123–125]. Intrapersonal resilience factors include high self-esteem, positive self-image, positive coping strategies, spirituality/religiosity, hopefulness, positive future expectations and participation in support or advocacy networks [85,90,98,123,126,127]. Interpersonal factors such as family and peers play an important role in youth development. Social support is generally hypothesized to be a protective factor that buffers individuals against the potential negative consequences of stressful events [128]. However, social support from family and peers may have differential effects for YKPs, including positive effects [129–133] or no effects at all [91,96,134]. For example, parental support may be more predictive of future MHDs than peer support [135,136]. Family connectedness and positive family acceptance have also been associated with positive mental health outcomes, particularly for sexual and gender minority youth who are grappling with issues of sexual orientation and gender identity [64,85,93,137–140]. Strong peer group affiliations may enhance risky health behaviours such as substance abuse and survival sex among runaway and homeless youth [141–143].
Exosystem factors include the availability of support from caring adults including teachers, case managers, programme facilitators and health providers; access to comprehensive youth-friendly social services with trained providers; non-discriminatory and anti-bullying policies in schools, homeless shelters and detention facilities; and child protection policies. These factors prevent MHDs, increase access to and utilization of health services, and promote YKPs’ ability to desist HIV risk behaviours [63,85,112,122,127,129,144]. Within the exosystem, organizations such as schools, churches, youth centres and health facilities are well positioned to provide safe environments and prevent MHDs among YKPs. For example, health providers could prepare youth and their families for changes related to pubertal development, understand and accept the gender and sexual identity of their children, provide parents/guardians with the skills needed to fully support YKPs and facilitate family re-integration (when appropriate). Schools, detentions centres, homeless shelters and foster homes can institute policies to prevent victimization of YKPs in these environments and advocate for the rights of YKPs. However, the success of these preventive actions requires providers who are knowledgeable and sensitive to the specific needs of YKPs.
Programmes and interventions
Interventions to prevent or improve MHDs and HIV risk behaviours among YKPs are critical to addressing the HIV epidemic among youth. MHDs among youth are addressed through treatment with pharmacological agents or psychosocial interventions [145]. Current treatment guidelines discourage use of pharmacotherapy among children and adolescents [146]; rather pharmacological agents should only be prescribed if psychosocial interventions prove ineffective. However, compared to adults, the evidence base for management of MHDs and HIV risk behaviours among youth is less established. For example, depression and PTSD are some of the most common MHDs among YKPs [147], but evidence for the effectiveness of medications for treatment of these MHDs among adolescents remains elusive [146,148,149].
Globally, there is a paucity of programmes addressing MHDs and HIV risk among YKPs, and even fewer of these programmes exist in low- and middle-income countries [150]. Psychosocial interventions for management of MHDs among YKPs include interpersonal psychotherapy, cognitive behavioural therapy, behavioural therapy, psychodynamic therapy, structured physical activity programmes, relaxation training, problem-solving therapy and motivational interviewing. Within the adult literature, there is an extensive body of knowledge on the effectiveness of these psychosocial interventions [151] but even so, understanding the exact mechanisms by which these interventions achieve their effects and consensus over the relative effectiveness of different psychosocial therapies is lacking [145,152,153].
There is a paucity of interventions to prevent MHDs among YKPs. Universal and targeted prevention programmes have been developed to address alcohol and substance use and HIV risk behaviours among YKPs [154–156] , but results from systematic reviews of these interventions indicate that the majority do not obtain significantly better mental health outcomes compared to controls [150], and reductions in HIV risk behaviours, if realized, are often short-lived [150,154,157–160] . These findings suggest a need to re-consider strategies for engaging and promoting sustainability of behavioural gains among YKPs.
The persistent fragmentation of services, often with single-focus programmes targeting specific YKPs or MHDs, disregards the co-occurrence of MHDs among YKPs [161] and multiplicity of needs across these intersecting populations, thus limiting the efficacy of these interventions. Commonly cited components of integrated MHD services include comprehensive screening for all MHDs, development of a common treatment plan addressing all conditions, a multi-disciplinary team that includes a specialist in co-occurring disorders and psychosocial and pharmacological interventions, and services such as assertive outreach, coordinated care and supported employment [162].
The World Health Organization advocates for treatment of mental and psychosocial problems within primary care settings, but several concerns abound with this strategy including lack of organizational resources and expertise, gaps in provider knowledge regarding the developmental and mental health needs of YKPs, and lack of cultural competency in addressing needs of YKPs [163,164] . Additionally, YKPs may have significant challenges in accessing services within primary care settings, due to lack of health insurance coverage and concerns about confidentiality and privacy.
Conclusions
Promoting the wellbeing of YKPs requires culturally and developmentally appropriate primary prevention interventions to eliminate or reduce risk factors for MHDs and HIV risk behaviours, and foster resilience factors throughout YKPs’ ecological environment. In addition, culturally and developmentally appropriate HIV care and mental health services are needed for youth living with HIV and/or MHDs, as well as secondary prevention interventions that promote healthy functioning and life course development for affected YKPs. All youth programmes and services need to address the intersectionality of marginalized identities and group membership often found among YKPs. They should be grounded in the latest theoretical and empirical data related to risk reduction and health promotion, and attend to the cultural and developmental needs of these youth.
While there is a growing body of knowledge regarding MHDs in some YKPs (e.g. sexual minority youth, runaway and homeless youth, detained or incarcerated youth), the literature on other populations such as gender minority youth and youth involved in sex work as well as YKPs in low-income countries continues to lag behind. The majority of studies on YKPs have been conducted in the United States; less is known about the psychosocial challenges or burden of MHDs among YKPs outside of the United States. This challenge is exacerbated by the lack of consistency in how MHDs are conceptualized and measured across countries and cultures [165–168], and differences in how adolescence is defined as a developmental period across settings [169,170]. Future research should focus on developing and validating mental health measures for non-US based populations and assessing the efficacy of these interventions in both US and non-US populations, keeping in mind the importance of tailoring interventions to local contexts.
Additional research is needed to increase understanding of key issues that influence the MHDs and HIV-related behaviours of YKPs, and to inform the development of effective interventions to address the unique needs of these young people. Of particular importance are studies elaborating on the complex pathways through which biological and ecological diatheses influence the development of MHDs and HIV risk behaviours among YKPs, the relative effects of the different types of stressors and appropriate strategies for management of MHDs in young people.
Interventions and research among YKPs would benefit from utilizing a BST framework for understanding the range of ecological factors that impact the MHDs and HIV-related risk and resilience of YKPs and in developing culturally and developmentally appropriate MHD and HIV-focused primary and secondary prevention interventions for YKPs. More research is needed to better understand the burden of MHDs in YKPs (especially outside of the US) and the interaction of MHDs and HIV-related risk and resilience. Such research should be sensitive to the multiple group membership of YKPs in often marginalized populations, addressing the multiplicity of risk and resilience factors across YKPs.
Given the high levels of stigma and discrimination experienced by YKPs globally, we argue that youth interventions should be rooted in the key human rights principles advanced in the convention on the rights of a child [171] including: (1) protection from physical and mental harm and exploitation; (2) utilization of evidence-based practices in establishing programmes and services for children; (3) provision of secure conditions that ensure dignity and promote self-reliance and (4) participation in decision-making processes taken in their regard. These human rights principles should supersede any social, cultural, political and other hegemonic ideologies, which may serve to oppress YKPs.
Below, we provide recommendations for practitioners and researchers on the best practices to promote the mental health and reduce HIV risk behaviours among YKPs:
Consolidate youth services to address the multiplicity of risk factors, and resulting MHDs and HIV risk behaviours. Develop partnerships across public, private and civil organizations to address the multiplicity of risk factors and special needs within YKPs, whilst attending to the individual needs of each youth. Such services should promote YKPs’ access to and sustained engagement in mental health services, HIV continuum of care and youth development programmes.
Tailor programmes and interventions to biological, cognitive, social and identity development stage of YKPs because there are wide variations in developmental differences between adolescents and young adults within YKPs.
Expand training for providers in mental health, particularly in low- and middle-income countries with a dearth of trained clinicians. This training should equip providers with the knowledge and skills to promote positive adolescent development and address the needs of YKPs through affirmative and respectful approaches.
Create supportive environments within programmes and services, and foster positive youth development by strengthening family, peers, school and community support systems. Family-centred interventions that enhance parent's/guardian's ability to connect with and support youth grappling with various psychosocial issues especially gender and sexual identity, and prevent risk factors such as family abuse, rejection and poor parent-youth communication and support are critical to preventing MHDs and HIV risk behaviours among YKPs.
Develop youth capabilities and critical consciousness by equipping youth with knowledge, skills and resources to counter their varied challenges [172] and provide opportunities for YKPs to participate in their socio-political environments.
Develop and enforce formal child protection systems, policies and guidelines in institutions such as schools and juvenile justice systems to prevent re-victimization of YKPs, and ensure access to mental health and HIV care services as well as positive youth development programmes within these contexts.
Acknowledgements
The authors would like to thank the faculty and staff at the Center for Sexuality and Health Disparities for their support during the preparation of the manuscript.
Competing interests
The authors do not have any competing interests to declare.
Authors' contributions
All authors contributed equally in the preparation of this manuscript.
References
- 1.Hall HI, Song R, Rhodes P, Prejean J, An Q, Lee LM, et al. Estimation of HIV incidence in the United States. JAMA. 2008;300(5):520–9. doi: 10.1001/jama.300.5.520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention (CDC) HIV surveillance – United States, 1981–2008. MMWR. 2011;60:689–93. [PubMed] [Google Scholar]
- 3.UNICEF. Monitoring the situation of children and women. 2014. [cited 2014 Sep 15]. Available from: http://data.unicef.org/hiv-aids/adolescents-young-people.
- 4.Donenberg GR. Youths and HIV/AIDS: psychiatry's role in a changing epidemic. J Am Acad Child Adolesc Psychiatry. 2005;44(8):728–47. doi: 10.1097/01.chi.0000166381.68392.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brown LK, Danovsky MB, Lourie KJ, DiClemente RJ, Ponton LE. Adolescents with psychiatric disorders and the risk of HIV. J Am Acad Child Adolesc Psychiatry. 1997;36(11):1609–17. doi: 10.1016/S0890-8567(09)66573-4. [DOI] [PubMed] [Google Scholar]
- 6.DiClemente RJ, Ponton LE. HIV-related risk behaviors among psychiatrically hospitalized adolescents and school-based adolescents. Am J Psychiatry. 1993;150(2):324–5. doi: 10.1176/ajp.150.2.324. [DOI] [PubMed] [Google Scholar]
- 7.Rotheram-Borus MJ, Koopman C. Sexual risk behaviors, AIDS knowledge, and beliefs about AIDS among runaways. Am J Public Health. 1991;81(2):208–10. doi: 10.2105/ajph.81.2.208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tubman JG, Gil AG, Wagner EF, Artigues H. Patterns of sexual risk behaviors and psychiatric disorders in a community sample of young adults. J Behav Med. 2003;26(5):473–500. doi: 10.1023/a:1025776102574. [DOI] [PubMed] [Google Scholar]
- 9.Stewart AJ, Theodore-Oklota C, Hadley W, Brown LK, Donenberg G, DiClemente R, et al. Mania symptoms and HIV-risk behavior among adolescents in mental health treatment. J Clin Child Adolesc Psychol. 2012;41(6):803–10. doi: 10.1080/15374416.2012.675569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Elkington KS, Bauermeister JA, Zimmerman MA. Psychological distress, substance use, and HIV/STI risk behaviors among youth. J Youth Adolesc. 2010;39(5):514–27. doi: 10.1007/s10964-010-9524-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lehrer JA, Shrier LA, Gortmaker S, Buka S. Depressive symptoms as a longitudinal predictor of sexual risk behaviors among US middle and high school students. Pediatrics. 2006;118(1):189–200. doi: 10.1542/peds.2005-1320. [DOI] [PubMed] [Google Scholar]
- 12.Tolou-Shams M, Brown LK, Houck C, Lescano CM. The association between depressive symptoms, substance use, and HIV risk among youth with an arrest history. J Stud Alcohol Drugs. 2007;69(1):58. doi: 10.15288/jsad.2008.69.58. [DOI] [PubMed] [Google Scholar]
- 13. Teplin LA, Elkington KS, McClelland GM, Abram KM, Mericle AA, Washburn JJ. Major mental disorders, substance use disorders, comorbidity, and HIV-AIDS risk behaviors in juvenile detainees. Psychiatr Serv. 2005;56(7):823–8. doi: 10.1176/appi.ps.56.7.823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Naar-King S, Templin T, Wright K, Frey M, Parsons JT, Lam P. Psychosocial factors and medication adherence in HIV-positive youth. AIDS Patient Care STDs. 2006;20(1):44–7. doi: 10.1089/apc.2006.20.44. [DOI] [PubMed] [Google Scholar]
- 15.Hosek SG, Harper GW, Domanico R. Predictors of medication adherence among HIV-infected youth. Psychol Health Med. 2005;10(2):166–79. doi: 10.1080/1354350042000326584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Leserman J. HIV disease progression: depression, stress, and possible mechanisms. Biol Psychiatry. 2003;54(3):295–306. doi: 10.1016/s0006-3223(03)00323-8. [DOI] [PubMed] [Google Scholar]
- 17.Fielden S, Sheckter L, Chapman G, Alimenti A, Forbes J, Sheps S, et al. Growing up: perspectives of children, families and service providers regarding the needs of older children with perinatally-acquired HIV. AIDS Care. 2006;18(8):1050–3. doi: 10.1080/09540120600581460. [DOI] [PubMed] [Google Scholar]
- 18.Mellins CA, Malee KM. Understanding the mental health of youth living with perinatal HIV infection: lessons learned and current challenges. J Int AIDS Soc. 2013;16(1):18593. doi: 10.7448/IAS.16.1.18593. doi: http://dx.doi.org/10.7448/IAS.16.1.18593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of dsm-iv disorders in the national comorbidity survey replication. Arch Gen Psychiatry. 2005;62(6):593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- 20.Merikangas KR, He JP, Burstein M, Swanson SA, Avenevoli S, Cui L, et al. Lifetime prevalence of mental disorders in US adolescents: results from the National Comorbidity Survey Replication Adolescent Supplement (NCS-A) J Am Acad Child Adolesc Psychiatry. 2010;49(10):980–9. doi: 10.1016/j.jaac.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kessler RC, Angermeyer M, Anthony JC, de Graaf R, Demyttenaere K, Gasquet I, et al. Lifetime prevalence and age-of-onset distributions of mental disorders in the World Health Organization's World Mental Health Survey Initiative. World Psychiatry. 2007;6(3):168. [PMC free article] [PubMed] [Google Scholar]
- 22.Millstein SG, Petersen AC, Nightingale EO. Promoting the health of adolescents: new directions for the twenty-first century. Oxford: Oxford University Press; 1993. [Google Scholar]
- 23.Rivara FP, Park MJ, Irwin CE, Jr, DiClemente R, Santelli J, Crosby R. Trends in adolescent and young adult morbidity and mortality. In: Ralph J. DiClemente, John S. Santelli, Richard A. Crosby., editors. Adolescent health: understanding and preventing risk behaviors. San Francisco, CA: Jossey-Bass; 2009. pp. 7–29. [Google Scholar]
- 24.Hatzenbuehler ML. The social environment and suicide attempts in lesbian, gay, and bisexual youth. Pediatrics. 2011;127(5):896–903. doi: 10.1542/peds.2010-3020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mustanski BS, Garofalo R, Emerson EM. Mental health disorders, psychological distress, and suicidality in a diverse sample of lesbian, gay, bisexual, and transgender youths. Am J Public Health. 2010;100(12):2426–32. doi: 10.2105/AJPH.2009.178319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Leslie MB, Stein JA, Rotheram-Borus MJ. Sex-specific predictors of suicidality among runaway youth. J Clin Child Adolesc Psychol. 2002;31(1):27–40. doi: 10.1207/S15374424JCCP3101_05. [DOI] [PubMed] [Google Scholar]
- 27.Almeida J, Johnson RM, Corliss HL, Molnar BE, Azrael D. Emotional distress among LGBT youth: the influence of perceived discrimination based on sexual orientation. J Youth Adolesc. 2009;38(7):1001–14. doi: 10.1007/s10964-009-9397-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.King M, Semlyen J, Tai SS, Killaspy H, Osborn D, Popelyuk D, et al. A systematic review of mental disorder, suicide, and deliberate self harm in lesbian, gay and bisexual people. BMC Psychiatry. 2008;8(1):70. doi: 10.1186/1471-244X-8-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Clements-Nolle K, Marx R, Katz M. Attempted suicide among transgender persons: the influence of gender-based discrimination and victimization. J Homosex. 2006;51(3):53–69. doi: 10.1300/J082v51n03_04. [DOI] [PubMed] [Google Scholar]
- 30.Wallien MS, Swaab H, Cohen-Kettenis PT. Psychiatric comorbidity among children with gender identity disorder. J Am Acad Child Adolesc Psychiatry. 2007;46(10):1307–14. doi: 10.1097/chi.0b013e3181373848. [DOI] [PubMed] [Google Scholar]
- 31.Conway KP, Compton W, Stinson FS, Grant BF. Lifetime comorbidity of DSM-IV mood and anxiety disorders and specific drug use disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. 2006;67(2):247–57. doi: 10.4088/jcp.v67n0211. [DOI] [PubMed] [Google Scholar]
- 32.Fazel S. Mental disorders among adolescents in juvenile detention and correctional facilities: a systematic review and metaregression analysis of 25 surveys. J Am Acad Child Adolesc Psychiatry. 2008;47(9):1010–9. doi: 10.1097/CHI.ObO13e31817eecf3. [DOI] [PubMed] [Google Scholar]
- 33.Colins O, Vermeiren R, Vreugdenhil C, van den Brink W, Doreleijers T, Broekaert E. Psychiatric disorders in detained male adolescents: a systematic literature review. Can J Psychiatry. 2010;55(4):255–63. doi: 10.1177/070674371005500409. [DOI] [PubMed] [Google Scholar]
- 34.Quinn MM, Osher DM, Poirier JM, Rutherford RB, Leone PE. Youth with disabilities in juvenile corrections: a national survey. Except Child. 2005;71(3):339–45. [Google Scholar]
- 35.Krezmien MP, Mulcahy CA, Leone PE. Detained and committed youth: examining differences in achievement, mental health needs, and special education status. Educ Treat Children. 2008;31(4):445–64. [Google Scholar]
- 36.Teplin LA, Abram KM, McClelland GM, Dulcan MK, Mericle AA. Psychiatric disorders in youth in juvenile detention. Arch Gen Psychiatry. 2002;59(12):1133–43. doi: 10.1001/archpsyc.59.12.1133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kirst MJ, Erickson P, Strike C. Poly-substance use among male and female street youth in Toronto, Canada. Int J Soc Inq. 2009;2(2):123–39. [Google Scholar]
- 38.Cleverley K, Kidd SA. Resilience and suicidality among homeless youth. J Adolesc. 2011;34(5):1049–54. doi: 10.1016/j.adolescence.2010.11.003. [DOI] [PubMed] [Google Scholar]
- 39.Johnson KD, Whitbeck LB, Hoyt DR. Substance abuse disorders among homeless and runaway adolescents. J Drug Issues. 2005;35(4):799–816. doi: 10.1177/002204260503500407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Shahmanesh M, Wayal S, Cowan F, Mabey D, Copas A, Patel V. Suicidal behavior among female sex workers in Goa, India: the silent epidemic. Am J Public Health. 2009;99(7):1239. doi: 10.2105/AJPH.2008.149930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Burgos M, Richter DL, Reininger B, Coker AL, Saunders R, Alegria M, et al. Street based female adolescent Puerto Rican sex workers: contextual issues and health needs. Fam Community Health. 1999;22(2):59–71. [Google Scholar]
- 42.Silverman JG. Adolescent female sex workers: invisibility, violence and HIV. Arch Dis Child. 2011;96(5):478–81. doi: 10.1136/adc.2009.178715. [DOI] [PubMed] [Google Scholar]
- 43.Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychol Bull. 2003;129(5):674. doi: 10.1037/0033-2909.129.5.674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Institute of Medicine. Washington, DC: National Academies Press; 2011. The health of lesbian, gay, bisexual, and transgender people: building a foundation for better understanding. [PubMed] [Google Scholar]
- 45.Harper GW, Schneider M. Oppression and discrimination among lesbian, gay, bisexual, and transgendered people and communities: a challenge for community psychology. Am J Community Psychol. 2003;31(3–4):243–52. doi: 10.1023/a:1023906620085. [DOI] [PubMed] [Google Scholar]
- 46.Grossman AH, D'Augelli AR. Transgender youth and life-threatening behaviors. Suicide Life Threat Behav. 2007;37(5):527–37. doi: 10.1521/suli.2007.37.5.527. [DOI] [PubMed] [Google Scholar]
- 47.Nuttbrock L, Hwahng S, Bockting W, Rosenblum A, Mason M, Macri M, et al. Psychiatric impact of gender-related abuse across the life course of male-to-female transgender persons. J Sex Res. 2010;47(1):12–23. doi: 10.1080/00224490903062258. [DOI] [PubMed] [Google Scholar]
- 48.Adlaf EM, Zdanowicz YM. A cluster-analytic study of substance problems and mental health among street youths. Am J Drug Alcohol Abuse. 1999;25(4):639–60. doi: 10.1081/ada-100101884. [DOI] [PubMed] [Google Scholar]
- 49.Merscham C, Van Leeuwen JM, McGuire M. Mental health and substance abuse indicators among homeless youth in Denver, Colorado. Child Welfare. 2008;88(2):93–110. [PubMed] [Google Scholar]
- 50.Slesnick N, Prestopnik J. Dual and multiple diagnosis among substance using runaway youth. Am J Drug Alcohol Abuse. 2005;31(1):179–201. doi: 10.1081/ADA-200047916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Whitbeck LB, Hoyt DR, Bao WN. Depressive symptoms and co-occurring depressive symptoms, substance abuse, and conduct problems among runaway and homeless adolescents. Child Dev. 2000;71(3):721–32. doi: 10.1111/1467-8624.00181. [DOI] [PubMed] [Google Scholar]
- 52.Whitbeck LB, Johnson KD, Hoyt DR, Cauce AM. Mental disorder and comorbidity among runaway and homeless adolescents. J Adolesc Health. 2004;35(2):132–40. doi: 10.1016/j.jadohealth.2003.08.011. [DOI] [PubMed] [Google Scholar]
- 53.Wasserman GA, McReynolds LS, Schwalbe CS, Keating JM, Jones SA. Psychiatric disorder, comorbidity, and suicidal behavior in juvenile justice youth. Crim Justice Behav. 2010;37(12):1361–76. [Google Scholar]
- 54.Decker MR, McCauley HL, Phuengsamran D, Janyam S, Silverman JG. Sex trafficking, sexual risk, sexually transmitted infection and reproductive health among female sex workers in Thailand. J Epidemiol Community Health. 2010;65(4):334–9. doi: 10.1136/jech.2009.096834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Beattie TS, Bhattacharjee P, Ramesh B, Gurnani V, Anthony J, Isac S, et al. Violence against female sex workers in Karnataka state, south India: impact on health, and reductions in violence following an intervention program. BMC Public Health. 2010;10(1):476. doi: 10.1186/1471-2458-10-476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Haas AP, Eliason M, Mays VM, Mathy RM, Cochran SD, D'Augelli AR, et al. Suicide and suicide risk in lesbian, gay, bisexual, and transgender populations: review and recommendations. J Homosex. 2010;58(1):10–51. doi: 10.1080/00918369.2011.534038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Frederick T. Diversity at the margins: the interconnections between homelessness, sex work, mental health, and substance use in the lives of sexual minority homeless young people. In: Dana Peterson, Vanessa R. Panfill., editors. Handbook of LGBT communities, crime, and justice. New York: Springer; 2014. pp. 473–501. [Google Scholar]
- 58.Garofalo R, Deleon J, Osmer E, Doll M, Harper GW. Overlooked, misunderstood and at-risk: exploring the lives and HIV risk of ethnic minority male-to-female transgender youth. J Adolesc Health. 2006;38(3):230–6. doi: 10.1016/j.jadohealth.2005.03.023. [DOI] [PubMed] [Google Scholar]
- 59.Durso LE, Gates GJ. Serving our youth: findings from a national survey of service providers working with lesbian, gay, bisexual, and transgender youth who are homeless or at risk of becoming homeless. Los Angeles, CA: Williams Institute, with True Colors Fund and Palette Fund; 2012. [Google Scholar]
- 60. Belknap J, Holsinger K, Little JS. Lesbian, gay, and bisexual youth incarcerated in delinquent facilities. In: Dana Peterson, Vanessa R. Panfill., editors. Handbook of LGBT communities, crime, and justice. New York: Springer; 2014. pp. 207–28. [Google Scholar]
- 61.Himmelstein KE, Brackner H. Criminal-justice and school sanctions against nonheterosexual youth: a national longitudinal study. Pediatrics. 2011;127(1):49–57. doi: 10.1542/peds.2009-2306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Rosario M, Schrimshaw EW, Hunter J. Homelessness among lesbian, gay, and bisexual youth: implications for subsequent internalizing and externalizing symptoms. J Youth Adolesc. 2012;41(5):544–60. doi: 10.1007/s10964-011-9681-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Rew L. Caring for and connecting with homeless adolescents. Fam Community Health. 2008;31:S42–51. doi: 10.1097/01.FCH.0000304017.13255.12. [DOI] [PubMed] [Google Scholar]
- 64.Friedman CK, Morgan EM. Comparing sexual-minority and heterosexual young womens’ friends and parents as sources of support for sexual issues. J Youth Adolesc. 2009;38(7):920–36. doi: 10.1007/s10964-008-9361-0. [DOI] [PubMed] [Google Scholar]
- 65.Stall R, Friedman M, Catania JA. Interacting epidemics and gay men's health: a theory of syndemic production among urban gay men. In: Wolitski RJ, Stall R, Valdiserri RO, editors. Unequal opportunity: health disparities affecting gay and bisexual men in the United States. New York: Oxford University Press; 2008. pp. 251–74. [Google Scholar]
- 66.Bruce D, Harper GW. Operating without a safety net: gay male adolescents and emerging adults’ experiences of marginalization and migration, and implications for theory of syndemic production of health disparities. Health Educ Behav. 2011;38(4):367–78. doi: 10.1177/1090198110375911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Bronfenbrenner U. Developmental ecology through space and time: a future perspective. In: Phyllis Moen, Glenn H. Elder, Kurt Luscher., editors. Examining lives in context: perspectives on the ecology of human development. Washington, DC: American Psychological Association; 1995. pp. 619–647. [Google Scholar]
- 68.Bronfenbrenner U. Making human beings human: bioecological perspectives on human development. Thousand Oaks, CA: SAGE Publications Inc; 2005. [Google Scholar]
- 69.Horwitz AV. The sociological study of mental illness. In: Carol S. Aneshensel, Jo C. Phelan, Alex Bierman., editors. Handbook of the sociology of mental health. Dordrecht: Springer; 1999. pp. 57–78. [Google Scholar]
- 70.Miranda J, McGuire T, Williams D, Wang P. Mental health in the context of health disparities. Am J Psychiatry. 2008;165(9):1102–8. doi: 10.1176/appi.ajp.2008.08030333. [DOI] [PubMed] [Google Scholar]
- 71.Schwartz S, Meyer IH. Mental health disparities research: the impact of within and between group analyses on tests of social stress hypotheses. Soc Sci Med. 2010;70(8):1111–8. doi: 10.1016/j.socscimed.2009.11.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.McKeever VM, Huff ME. A diathesis-stress model of posttraumatic stress disorder: ecological, biological, and residual stress pathways. Rev Gen Psychol. 2003;7(3):237. [Google Scholar]
- 73.Rende R, Plomin R. Diathesis-stress models of psychopathology: a quantitative genetic perspective. Appl Prev Psychol. 1992;1(4):177–82. [Google Scholar]
- 74.Monroe SM, Simons AD. Diathesis-stress theories in the context of life stress research: implications for the depressive disorders. Psychol Bull. 1991;110(3):406. doi: 10.1037/0033-2909.110.3.406. [DOI] [PubMed] [Google Scholar]
- 75.Bronfenbrenner U. Toward an experimental ecology of human development. Am Psychol. 1977;32(7):513. [Google Scholar]
- 76.Reisner SL, Greytak EA, Parsons JT, Ybarra ML. Gender minority social stress in adolescence: disparities in adolescent bullying and substance use by gender identity. J Sex Res. 2014;17:1–14. doi: 10.1080/00224499.2014.886321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Noell JW, Ochs LM. Relationship of sexual orientation to substance use, suicidal ideation, suicide attempts, and other factors in a population of homeless adolescents. J Adolesc Health. 2001;29(1):31–6. doi: 10.1016/s1054-139x(01)00205-1. [DOI] [PubMed] [Google Scholar]
- 78.Moskowitz A, Stein JA, Lightfoot M. The mediating roles of stress and maladaptive behaviors on self-harm and suicide attempts among runaway and homeless youth. J Youth Adolesc. 2013;42(7):1015–27. doi: 10.1007/s10964-012-9793-4. [DOI] [PubMed] [Google Scholar]
- 79.Dodge KA, Pettit GS. A biopsychosocial model of the development of chronic conduct problems in adolescence. Dev Psychol. 2003;39(2):349. doi: 10.1037//0012-1649.39.2.349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Sowell ER, Peterson BS, Thompson PM, Welcome SE, Henkenius AL, Toga AW. Mapping cortical change across the human life span. Nat Neurosci. 2003;6(3):309–15. doi: 10.1038/nn1008. [DOI] [PubMed] [Google Scholar]
- 81.Sharer LR. Pathology of HIV-1 infection of the central nervous system. A review. J Neuropathol Exp Neurol. 1992;51(1):3–11. doi: 10.1097/00005072-199201000-00002. [DOI] [PubMed] [Google Scholar]
- 82.Arnett J. Reckless behavior in adolescence: a developmental perspective. Dev Rev. 1992;12(4):339–73. [Google Scholar]
- 83.Arnett JJ. Adolescent storm and stress, reconsidered. Am Psychol. 1999;54(5):317. doi: 10.1037//0003-066x.54.5.317. [DOI] [PubMed] [Google Scholar]
- 84.Greene K, Krcmar M, Walters LH, Rubin DL, Hale L. Targeting adolescent risk-taking behaviors: the contributions of egocentrism and sensation-seeking. J Adolesc. 2000;23(4):439–61. doi: 10.1006/jado.2000.0330. [DOI] [PubMed] [Google Scholar]
- 85.Fenaughty J, Harré N. Life on the seesaw: a qualitative study of suicide resiliency factors for young gay men. J Homosex. 2003;45(1):1–22. doi: 10.1300/J082v45n01_01. [DOI] [PubMed] [Google Scholar]
- 86.Herbert SE. Female-to-male transgender adolescents. Child Adolesc Psychiatr Clin N Am. 2011;20(4):681–8. doi: 10.1016/j.chc.2011.08.005. [DOI] [PubMed] [Google Scholar]
- 87.Mackelprang JL, Harpin SB, Grubenhoff JA, Rivara FP. Adverse outcomes among homeless adolescents and young adults who report a history of traumatic brain injury. Am J Public Health. 2014;104(10):1986–92. doi: 10.2105/AJPH.2014.302087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Huw Williams W, Cordan G, Mewse AJ, Tonks J, Burgess CN. Self-reported traumatic brain injury in male young offenders: a risk factor for re-offending, poor mental health and violence? Neuropsychol Rehabil. 2010;20(6):801–12. doi: 10.1080/09602011.2010.519613. [DOI] [PubMed] [Google Scholar]
- 89.Lewinsohn PM, Joiner TE, Jr, Rohde P. Evaluation of cognitive diathesis-stress models in predicting major depressive disorder in adolescents. J Abnorm Psychol. 2001;110(2):203. doi: 10.1037//0021-843x.110.2.203. [DOI] [PubMed] [Google Scholar]
- 90.Grossman AH, D'augelli AR, Frank JA. Aspects of psychological resilience among transgender youth. J LGBT Youth. 2011;8(2):103–15. [Google Scholar]
- 91.Hershberger SL, D'Augelli AR. The impact of victimization on the mental health and suicidality of lesbian, gay, and bisexual youths. Dev Psychol. 1995;31(1):65. [Google Scholar]
- 92.Van Bergen DD, Bos HM, van Lisdonk J, Keuzenkamp S, Sandfort TG. Victimization and suicidality among Dutch lesbian, gay, and bisexual youths. Am J Public Health. 2013;103(1):70–2. doi: 10.2105/AJPH.2012.300797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Ryan C, Huebner D, Diaz RM, Sanchez J. Family rejection as a predictor of negative health outcomes in White and Latino Lesbian, Gay, and bisexual young adults. Pediatrics. 2009;123(1):346–52. doi: 10.1542/peds.2007-3524. [DOI] [PubMed] [Google Scholar]
- 94.Russell ST, Ryan C, Toomey RB, Diaz RM, Sanchez J. Lesbian, gay, bisexual, and transgender adolescent school victimization: implications for young adult health and adjustment. J School Health. 2011;81(5):223–30. doi: 10.1111/j.1746-1561.2011.00583.x. [DOI] [PubMed] [Google Scholar]
- 95.Kidd SA. Youth homelessness and social stigma. J Youth Adolesc. 2007;36(3):291–9. doi: 10.1007/s10964-006-9100-3. [DOI] [PubMed] [Google Scholar]
- 96.Kidd SA, Carroll MR. Coping and suicidality among homeless youth. J Adolesc. 2007;30(2):283–96. doi: 10.1016/j.adolescence.2006.03.002. [DOI] [PubMed] [Google Scholar]
- 97.Keuroghlian AS, Shtasel D, Bassuk EL. Out on the street: a public health and policy agenda for lesbian, gay, bisexual, and transgender youth who are homeless. Am J Orthopsychiatry. 2014;84(1):66. doi: 10.1037/h0098852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Mc Elroy S, Hevey D. Relationship between adverse early experiences, stressors, psychosocial resources and wellbeing. Child Abuse Neglect. 2014;38(1):65–75. doi: 10.1016/j.chiabu.2013.07.017. [DOI] [PubMed] [Google Scholar]
- 99.Wilson HW, Widom CS. The role of youth problem behaviors in the path from child abuse and neglect to prostitution: a prospective examination. J Res Adolesc. 2010;20(1):210–36. doi: 10.1111/j.1532-7795.2009.00624.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Simons RL, Whitbeck LB. Sexual abuse as a precursor to prostitution and victimization among adolescent and adult homeless women. J Family Issues. 1991;12(3):361–79. [Google Scholar]
- 101.Rosario M, Schrimshaw EW, Hunter J. Risk factors for homelessness among lesbian, gay, and bisexual youths: a developmental milestone approach. Child Youth Serv Rev. 2012;34(1):186–93. doi: 10.1016/j.childyouth.2011.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Tyler KA, Melander LA. Child abuse, street victimization, and substance use among homeless young adults. Youth Society. 2013:1–18. doi: 10.1177/0044118X12471354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Wilson HW, Widom CS. An examination of risky sexual behavior and HIV in victims of child abuse and neglect: a 30-year follow-up. Health Psychol. 2008;27(2):149. doi: 10.1037/0278-6133.27.2.149. [DOI] [PubMed] [Google Scholar]
- 104.Jones DJ, Runyan DK, Lewis T, Litrownik AJ, Black MM, Wiley T, et al. Trajectories of childhood sexual abuse and early adolescent HIV/AIDS risk behaviors: the role of other maltreatment, witnessed violence, and child gender. J Clin Child Adolesc Psychol. 2010;39(5):667–80. doi: 10.1080/15374416.2010.501286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Lansford JE, Miller-Johnson S, Berlin LJ, Dodge KA, Bates JE, Pettit GS. Early physical abuse and later violent delinquency: a prospective longitudinal study. Child Maltreat. 2007;12(3):233–45. doi: 10.1177/1077559507301841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Jespersen AF, Lalumière ML, Seto MC. Sexual abuse history among adult sex offenders and non-sex offenders: a meta-analysis. Child Abuse Negl. 2009;33(3):179–92. doi: 10.1016/j.chiabu.2008.07.004. [DOI] [PubMed] [Google Scholar]
- 107.Trickett PK, Noll JG, Putnam FW. The impact of sexual abuse on female development: lessons from a multigenerational, longitudinal research study. Dev Psychopathol. 2011;23(02):453–76. doi: 10.1017/S0954579411000174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Trickett PK, Negriff S, Ji J, Peckins M. Child maltreatment and adolescent development. J Res Adolesc. 2011;21(1):3–20. [Google Scholar]
- 109.Noll JG, Haralson KJ, Butler EM, Shenk CE. Childhood maltreatment, psychological dysregulation, and risky sexual behaviors in female adolescents. J Pediatr Psychol. 2011;36(7):743–52. doi: 10.1093/jpepsy/jsr003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Engel CC, Engel AL, Campbell SJ, McFall ME, Russo J, Katon W. Posttraumatic stress disorder symptoms and precombat sexual and physical abuse in Desert Storm veterans. J Nerv Ment Dis. 1993;181(11):683–8. doi: 10.1097/00005053-199311000-00006. [DOI] [PubMed] [Google Scholar]
- 111.Dodge KA, Pettit GS, Bates JE, Valente E. Social information-processing patterns partially mediate the effect of early physical abuse on later conduct problems. J Abnorm Psychol. 1995;104(4):632. doi: 10.1037//0021-843x.104.4.632. [DOI] [PubMed] [Google Scholar]
- 112.Thompson SJ, McManus H, Lantry J, Windsor L, Flynn P. Insights from the street: perceptions of services and providers by homeless young adults. Eval Program Plann. 2006;29(1):34–43. [Google Scholar]
- 113.Cummings JR, Wen H, Druss BG. Improving access to mental health services for youth in the United States. JAMA. 2013;309(6):553–4. doi: 10.1001/jama.2013.437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Kieling C, Baker-Henningham H, Belfer M, Conti G, Ertem I, Omigbodun O, et al. Child and adolescent mental health worldwide: evidence for action. Lancet. 2011;378(9801):1515–25. doi: 10.1016/S0140-6736(11)60827-1. [DOI] [PubMed] [Google Scholar]
- 115.Solorio MR, Milburn NG, Andersen RM, Trifskin S, Rodríguez MA. Emotional distress and mental health service use among urban homeless adolescents. J Behav Health Serv Res. 2006;33(4):381–93. doi: 10.1007/s11414-006-9037-z. [DOI] [PubMed] [Google Scholar]
- 116.Ensign J, Bell M. Illness experiences of homeless youth. Qual Health Res. 2004;14(9):1239–54. doi: 10.1177/1049732304268795. [DOI] [PubMed] [Google Scholar]
- 117.Ribeiro WS, Andreoli SB, Ferri CP, Prince M, Mari JJ. Exposure to violence and mental health problems in low and middle-income countries: a literature review. Rev Bras Psiquiatr. 2009;31:S49–57. doi: 10.1590/s1516-44462009000600003. [DOI] [PubMed] [Google Scholar]
- 118.Amone-P'Olak K, Jones PB, Abbott R, Meiser-Stedman R, Ovuga E, Croudace TJ. Cohort profile: mental health following extreme trauma in a northern Ugandan cohort of War-Affected Youth Study (The WAYS Study) SpringerPlus. 2013;2(1):1–11. doi: 10.1186/2193-1801-2-300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Corliss HL, Belzer M, Forbes C, Wilson EC. An evaluation of service utilization among male to female transgender youth: qualitative study of a clinic-based sample. J LGBT Health Res. 2008;3(2):49–61. doi: 10.1300/J463v03n02_06. [DOI] [PubMed] [Google Scholar]
- 120.Castaneda H. Structural vulnerability and access to medical care among migrant street-based male sex workers in Germany. Soc Sci Med. 2013;84:94–101. doi: 10.1016/j.socscimed.2013.02.010. [DOI] [PubMed] [Google Scholar]
- 121.Shannon K, Rusch M, Shoveller J, Alexson D, Gibson K, Tyndall MW. Mapping violence and policing as an environmental-structural barrier to health service and syringe availability among substance-using women in street-level sex work. Int J Drug Policy. 2008;19(2):140–7. doi: 10.1016/j.drugpo.2007.11.024. [DOI] [PubMed] [Google Scholar]
- 122.Christiani A, Hudson AL, Nyamathi A, Mutere M, Sweat J. Attitudes of homeless and drug-using youth regarding barriers and facilitators in delivery of quality and culturally sensitive health care. J Child Adolesc Psychiatr Nurs. 2008;21(3):154–63. doi: 10.1111/j.1744-6171.2008.00139.x. [DOI] [PubMed] [Google Scholar]
- 123.Fergus S, Zimmerman MA. Adolescent resilience: a framework for understanding healthy development in the face of risk. Annu Rev Public Health. 2005;26:399–419. doi: 10.1146/annurev.publhealth.26.021304.144357. [DOI] [PubMed] [Google Scholar]
- 124.Resnick MD, Bearman PS, Blum RW, Bauman KE, Harris KM, Jones J, et al. Protecting adolescents from harm: findings from the National Longitudinal Study on Adolescent Health. JAMA. 1997;278(10):823–32. doi: 10.1001/jama.278.10.823. [DOI] [PubMed] [Google Scholar]
- 125.Borowsky IW, Ireland M, Resnick MD. Violence risk and protective factors among youth held back in school. Ambul Pediatr. 2002;2(6):475–84. doi: 10.1367/1539-4409(2002)002<0475:vrapfa>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 126.Kidd S, Shahar G. Resilience in homeless youth: the key role of self-esteem. Am J Orthopsychiatry. 2008;78(2):163–72. doi: 10.1037/0002-9432.78.2.163. [DOI] [PubMed] [Google Scholar]
- 127.Tevendale HD, Lightfoot M, Slocum SL. Individual and environmental protective factors for risky sexual behavior among homeless youth: an exploration of gender differences. AIDS Behav. 2009;13(1):154–64. doi: 10.1007/s10461-008-9395-z. [DOI] [PubMed] [Google Scholar]
- 128.Yap MB, Devilly GJ. The role of perceived social support in crime victimization. Clin Psychol Rev. 2004;24(1):1–14. doi: 10.1016/j.cpr.2003.09.007. [DOI] [PubMed] [Google Scholar]
- 129.Eisenberg ME, Resnick MD. Suicidality among gay, lesbian and bisexual youth: the role of protective factors. J Adolesc Health. 2006;39(5):662–8. doi: 10.1016/j.jadohealth.2006.04.024. [DOI] [PubMed] [Google Scholar]
- 130.Sheets RL, Jr, Mohr JJ. Perceived social support from friends and family and psychosocial functioning in bisexual young adult college students. J Couns Psychol. 2009;56(1):152. [Google Scholar]
- 131.Doty ND, Willoughby BL, Lindahl KM, Malik NM. Sexuality related social support among lesbian, gay, and bisexual youth. J Youth Adolesc. 2010;39(10):1134–47. doi: 10.1007/s10964-010-9566-x. [DOI] [PubMed] [Google Scholar]
- 132.Williams T, Connolly J, Pepler D, Craig W. Peer victimization, social support, and psychosocial adjustment of sexual minority adolescents. J Youth Adolesc. 2005;34(5):471–82. [Google Scholar]
- 133.Vincke J, van Heeringen K. Confidant support and the mental wellbeing of lesbian and gay young adults: a longitudinal analysis. J Community Appl Soc Psychol. 2002;12(3):181–93. [Google Scholar]
- 134.Szymanski DM. Examining potential moderators of the link between heterosexist events and gay and bisexual men's psychological distress. J Couns Psychol. 2009;56(1):142–51. [Google Scholar]
- 135.Stice E, Ragan J, Randall P. Prospective relations between social support and depression: differential direction of effects for parent and peer support? J Abnorm Psychol. 2004;113(1):155. doi: 10.1037/0021-843X.113.1.155. [DOI] [PubMed] [Google Scholar]
- 136.Lewinsohn PM, Roberts RE, Seeley JR, Rohde P, Gotlib IH, Hops H. Adolescent psychopathology: II. Psychosocial risk factors for depression. J Abnorm Psychol. 1994;103(2):302. doi: 10.1037//0021-843x.103.2.302. [DOI] [PubMed] [Google Scholar]
- 137.Needham BL, Austin EL. Sexual orientation, parental support, and health during the transition to young adulthood. J Youth Adolesc. 2010;39(10):1189–98. doi: 10.1007/s10964-010-9533-6. [DOI] [PubMed] [Google Scholar]
- 138.Simons L, Schrager SM, Clark LF, Belzer M, Olson J. Parental support and mental health among transgender adolescents. J Adolesc Health. 2013;53(6):791–3. doi: 10.1016/j.jadohealth.2013.07.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Nesmith AA, Burton DL, Cosgrove TJ. Gay, lesbian, and bisexual youth and young adults: social support in their own words. J Homosex. 1999;37(1):95–108. doi: 10.1300/J082v37n01_07. [DOI] [PubMed] [Google Scholar]
- 140.Rothman EF, Sullivan M, Keyes S, Boehmer U. Parents’ supportive reactions to sexual orientation disclosure associated with better health: results from a population-based survey of LGB adults in Massachusetts. J Homosex. 2012;59(2):186–200. doi: 10.1080/00918369.2012.648878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Wright ER, Perry BL. Sexual identity distress, social support, and the health of gay, lesbian, and bisexual youth. J Homosex. 2006;51(1):81–110. doi: 10.1300/J082v51n01_05. [DOI] [PubMed] [Google Scholar]
- 142.McMorris BJ, Tyler KA, Whitbeck LB, Hoyt DR. Familial and on-the-street risk factors associated with alcohol use among homeless and runaway adolescents. J Stud Alcohol Drugs. 2002;63(1):34. [PubMed] [Google Scholar]
- 143.Ennett ST, Bailey SL, Federman EB. Social network characteristics associated with risky behaviors among runaway and homeless youth. J Health Soc Behav. 1999;40:63–78. [PubMed] [Google Scholar]
- 144.Darwich L, Hymel S, Waterhouse T. School avoidance and substance use among lesbian, gay, bisexual, and questioning youths: the impact of peer victimization and adult support. J Educ Psychol. 2012;104(2):381. [Google Scholar]
- 145.Chernoff M, Nachman S, Williams P, Brouwers P, Heston J, Hodge J, et al. Mental health treatment patterns in perinatally HIV-infected youth and controls. Pediatrics. 2009;124(2):627–36. doi: 10.1542/peds.2008-2441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.World Health Organization. mhGAP Intervention Guide for mental, neurological and substance use disorders in non-specialized health settings. 2014. [cited 2014 Sep 15]. Available from: http://www.paho.org/mhgap/en/depression.html. [PubMed]
- 147.Costello JE, Erkanli A, Angold A. Is there an epidemic of child or adolescent depression? J Child Psychol Psychiatry. 2006;47(12):1263–71. doi: 10.1111/j.1469-7610.2006.01682.x. [DOI] [PubMed] [Google Scholar]
- 148.Goodyer IM, Croudace T, Dudbridge F, Ban M, Herbert J. Polymorphisms in BDNF (Val66Met) and 5-HTTLPR, morning cortisol and subsequent depression in at-risk adolescents. Br J Psychiatry. 2010;197(5):365–71. doi: 10.1192/bjp.bp.110.077750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Hetrick SE, Purcell R, Garner B, Parslow R. Combined pharmacotherapy and psychological therapies for post traumatic stress disorder (PTSD) Cochrane Database Syst Rev. 2010;7(7):CD007316. doi: 10.1002/14651858.CD007316.pub2. [DOI] [PubMed] [Google Scholar]
- 150.Coren E, Hossain R, Pardo Pardo J, Veras MM, Chakraborty K, Harris H, et al. Interventions for promoting reintegration and reducing harmful behaviour and lifestyles in street-connected children and young people. Cochrane Database Syst Rev. 2013;2:CD009823. doi: 10.1002/14651858.CD009823.pub2. [DOI] [PubMed] [Google Scholar]
- 151.Johnson WD, Diaz RM, Flanders WD, Goodman M, Hill AN, Holtgrave D, et al. Behavioral interventions to reduce risk for sexual transmission of HIV among men who have sex with men. Cochrane Database Syst Rev. 2008;3:CD001230. doi: 10.1002/14651858.CD001230.pub2. [DOI] [PubMed] [Google Scholar]
- 152.Bower P, Knowles S, Coventry PA, Rowland N. Counselling for mental health and psychosocial problems in primary care. Cochrane Database Syst Rev. 2011;9:CD001025. doi: 10.1002/14651858.CD001025.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Cleary M, Hunt G, Matheson S, Siegfried N, Walter G. Psychosocial interventions for people with both severe mental illness and substance misuse. Cochrane Database Syst Rev. 2008;1:CD001088. doi: 10.1002/14651858.CD001088.pub2. [DOI] [PubMed] [Google Scholar]
- 154.McCambridge J, Gates S, Smith LA, Foxcroft DR. Interventions for prevention of drug use by young people delivered in non-school settings. Cochrane Database Syst Rev. 2004:CD005030. doi: 10.1002/14651858.CD005030. [DOI] [PubMed] [Google Scholar]
- 155.Goldberg E, Millson P, Rivers S, Manning SJ, Leslie K, Read S, et al. A human immunodeficiency virus risk reduction intervention for incarcerated youth: a randomized controlled trial. J Adolesc Health. 2009;44(2):136–45. doi: 10.1016/j.jadohealth.2008.07.021. [DOI] [PubMed] [Google Scholar]
- 156.St Lawrence JS, Crosby RA, Belcher L, Yazdani N, Brasfield TL. Sexual risk reduction and anger management interventions for incarcerated male adolescents: a randomized controlled trial of two interventions. J Sex Educ Ther. 1999;24(1–2):9–17. [Google Scholar]
- 157.Stanton BF, Li X, Ricardo I, Galbraith J, Feigelman S, Kaljee L. A randomized, controlled effectiveness trial of an AIDS prevention program for low-income African-American youths. Arch Pediatr Adolesc Med. 1996;150(4):363–72. doi: 10.1001/archpedi.1996.02170290029004. [DOI] [PubMed] [Google Scholar]
- 158.Cox GR, Callahan P, Churchill R, Hunot V, Merry SN, Parker AG, et al. Psychological therapies versus antidepressant medication, alone and in combination for depression in children and adolescents. Cochrane Database Syst Rev. 2012;11:CD008324. doi: 10.1002/14651858.CD008324.pub2. [DOI] [PubMed] [Google Scholar]
- 159.Foxcroft DR, Tsertsvadze A. Cochrane review: Universal school-based prevention programs for alcohol misuse in young people. Evid Based Child Health. 2012;7(2):450–575. doi: 10.1002/14651858.CD009113. [DOI] [PubMed] [Google Scholar]
- 160.Gates S, McCambridge J, Smith LA, Foxcroft D. Interventions for prevention of drug use by young people delivered in non-school settings. Cochrane Database Syst Rev. 2006;1:CD005030. doi: 10.1002/14651858.CD005030.pub2. [DOI] [PubMed] [Google Scholar]
- 161.McGovern MP, Lambert-Harris C, Gotham HJ, Claus RE, Xie H. Dual diagnosis capability in mental health and addiction treatment services: an assessment of programs across multiple state systems. Adm Policy Ment Health. 2014;41(2):205–14. doi: 10.1007/s10488-012-0449-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Foster S, LeFauve C, Kresky-Wolff M, Rickards LD. Services and supports for individuals with co-occurring disorders and long-term homelessness. J Behav Health Serv Res. 2010;37(2):239–51. doi: 10.1007/s11414-009-9190-2. [DOI] [PubMed] [Google Scholar]
- 163.Drake RE, Essock SM, Shaner A, Carey KB, Minkoff K, Kola L, et al. Implementing dual diagnosis services for clients with severe mental illness. Psychiatr Serv. 2001;52(4):469–76. doi: 10.1176/appi.ps.52.4.469. [DOI] [PubMed] [Google Scholar]
- 164.Mitchell AJ, Malone D, Doebbeling CC. Quality of medical care for people with and without comorbid mental illness and substance misuse: systematic review of comparative studies. Br J Psychiatry. 2009;194(6):491–9. doi: 10.1192/bjp.bp.107.045732. [DOI] [PubMed] [Google Scholar]
- 165.Mutumba M, Tomlinson M, Tsai AC. Psychometric properties of instruments for assessing depression among African youth: a systematic review. J Child Adolesc Mental Health. 2014;26(2):139–56. doi: 10.2989/17280583.2014.907169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Tomlinson M, Swartz L, Kruger L-M, Gureje O. Manifestations of affective disturbance in sub-Saharan Africa: key themes. J Affect Disord. 2007;102(1):191–8. doi: 10.1016/j.jad.2006.09.029. [DOI] [PubMed] [Google Scholar]
- 167.Ventevogel P, Jordans M, Reis R, de Jong J. Madness or sadness? Local concepts of mental illness in four conflict-affected African communities. Confl Health. 2013;7:3. doi: 10.1186/1752-1505-7-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Bebbington P. Transcultural aspects of affective disorders. Int Rev Psychiatry. 1993;5(2–3):145–56. [Google Scholar]
- 169.Caldwell JC, Caldwell P, Caldwell BK, Pieris I. The construction of adolescence in a changing world: implications for sexuality, reproduction, and marriage. Stud Fam Plann. 1998 Jun;29(2):137–53. [PubMed] [Google Scholar]
- 170.Fatusi AO, Hindin MJ. Adolescents and youth in developing countries: health and development issues in context. J Adolesc. 2010;33(4):499–508. doi: 10.1016/j.adolescence.2010.05.019. [DOI] [PubMed] [Google Scholar]
- 171.United Nations Human Rights (UNHR) Convention on the rights of the child. 1989. [cited 2014 Jul 25]. Available from: http://www.ohchr.org/en/professionalinterest/pages/crc.aspx.
- 172.Diemer MA, Li CH. Critical consciousness development and political participation among marginalized youth. Child Dev. 2011;82(6):1815–33. doi: 10.1111/j.1467-8624.2011.01650.x. [DOI] [PubMed] [Google Scholar]