Abstract
Background:
Trade-offs between upfront benefits and later risk of revision of unicompartmental knee arthroplasty compared with those of total knee arthroplasty are poorly understood. The purpose of our study was to compare the cost-effectiveness of unicompartmental knee arthroplasty with that of total knee arthroplasty across the age spectrum of patients undergoing knee replacement.
Methods:
Using a Markov decision analytic model, we compared unicompartmental knee arthroplasty with total knee arthroplasty with regard to lifetime costs, quality-adjusted life-years (QALYs), and incremental cost-effectiveness ratios (ICERs) from a societal perspective for patients undergoing surgery at forty-five, fifty-five, sixty-five, seventy-five, or eighty-five years of age. Transition probabilities were estimated from the literature; survival, from the Swedish Knee Arthroplasty Register; and costs, from the literature and the Healthcare Cost and Utilization Project (HCUP) database. Costs and QALYs were discounted at 3.0% annually. We conducted sensitivity analyses to test the robustness of model estimates and threshold analyses.
Results:
For patients sixty-five years of age and older, unicompartmental knee arthroplasty dominated total knee arthroplasty, with lower lifetime costs and higher QALYs. Unicompartmental knee arthroplasty was no longer cost-effective at a $100,000/QALY threshold when total knee arthroplasty rehabilitation costs were reduced by two-thirds or more for these older patients. Lifetime societal savings from utilizing unicompartmental knee arthroplasty in all older patients (sixty-five or older) in 2015 and 2020 were $56 to $336 million and $84 to $544 million, respectively. In the forty-five and fifty-five-year-old age cohorts, total knee arthroplasty had an ICER of $30,300/QALY and $63,000/QALY, respectively. Unicompartmental knee arthroplasty became cost-effective when its twenty-year revision rate dropped from 27.8% to 25.7% for the forty-five-year age group and from 27.9% to 26.7% for the fifty-five-year age group.
Conclusions:
Unicompartmental knee arthroplasty is an economically attractive alternative in patients sixty-five years of age or older, and modest improvements in implant survivorship could make it a cost-effective alternative in younger patients.
Unicompartmental knee arthroplasty, which replaces only the knee compartment affected by osteoarthritis, is an alternative to total knee arthroplasty, a procedure that replaces the entire knee joint. Unicompartmental knee arthroplasty preserves bone tissue that will be valuable if prosthetic revision is needed1,2. In addition, unicompartmental knee arthroplasty has fewer complications, requires less rehabilitation, and may provide a better range of motion and superior function compared with total knee arthroplasty3. Because it is associated with a higher risk of revision compared with that of total knee arthroplasty, unicompartmental knee arthroplasty remains a controversial procedure that may be underutilized. Retrospective studies indicate that 12.0% to 21.0% of patients who undergo total knee arthroplasty were candidates for unicompartmental knee arthroplasty4, whereas <8.0% of knee arthroplasties are unicompartmental5.
Trade-offs between upfront benefits and later risk of revision of unicompartmental knee arthroplasty compared with those of total knee arthroplasty are poorly understood. The few available cost-effectiveness studies of which we are aware were limited to older populations (sixty-five years of age or older)6-8. By 2020, total knee arthroplasty utilization is expected to exceed one million annually9 and, unlike today, approximately half of these procedures will be performed in patients younger than sixty-five years of age10. With changing utilization trends, we compared the cost-effectiveness of unicompartmental knee arthroplasty with that of total knee arthroplasty in patients forty-five through eighty-five years of age in the U.S.
Materials and Methods
We developed a Markov state-transition model (TreeAge Pro; TreeAge Software, Williamstown, Massachusetts) to compare the cost-effectiveness of the two procedures. We expressed cost-effectiveness findings in terms of lifetime arthroplasty-related costs (2012 U.S. dollars), quality-adjusted life-years (QALYs), and incremental cost-effectiveness ratios (ICERs). All costs and QALYs represent a societal perspective and were discounted at 3.0% annually11. We designed five hypothetical cohorts to represent patients choosing either total knee arthroplasty or unicompartmental knee arthroplasty procedures at the age of forty-five, fifty-five, sixty-five, seventy-five, or eighty-five years.
Model Structure
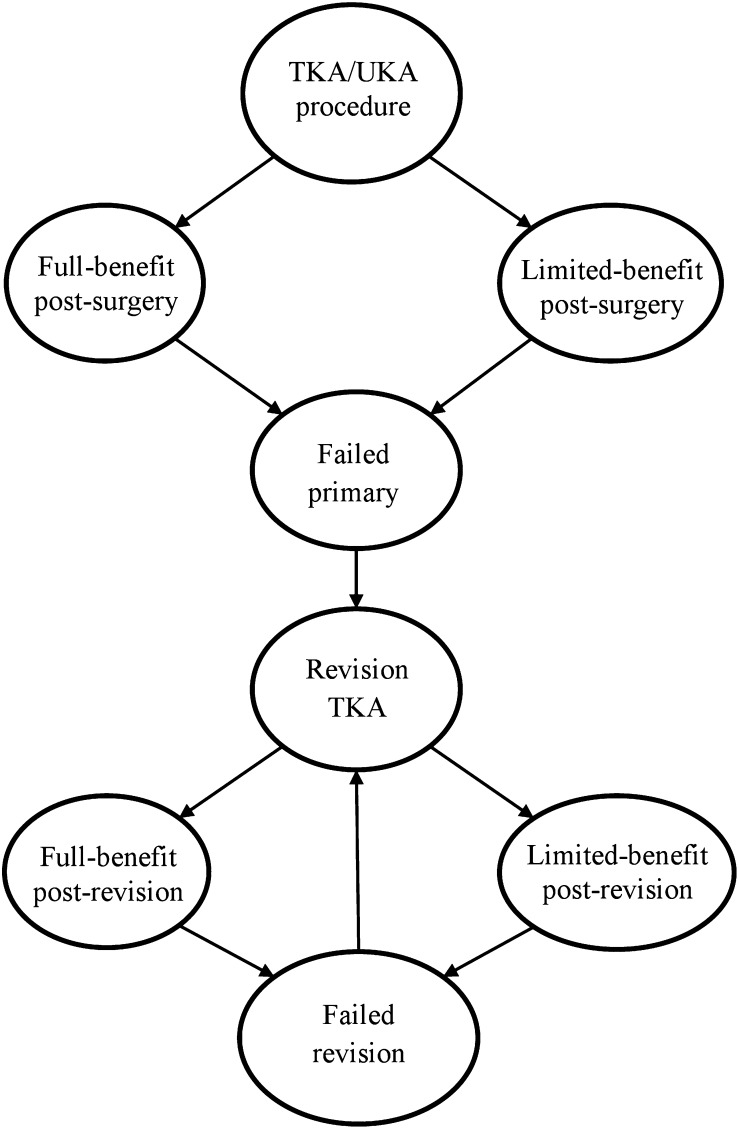
Model health states for both procedures were full-benefit post-surgery, limited-benefit post-surgery, failed primary surgery, revision total knee arthroplasty, full-benefit post-revision, limited-benefit post-revision, failed revision, and death (Fig. 1). A hypothetical patient starts in the total knee arthroplasty or unicompartmental knee arthroplasty surgical state, incurring costs of the initial procedure and associated complications, and moves to either a full-benefit (successful surgery) or limited-benefit (unsuccessful surgery) state. The transition probability is based on his or her Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) score, with a WOMAC score of <60 indicating poor function (the best possible function score is 100) and a transition to a limited-benefit state12,13. Patients in a full-benefit or limited-benefit state are at risk at each cycle for implant failure and may subsequently choose or decline revision total knee arthroplasty. Patients who elect to have a revision stay in the revision state for one cycle and then transition to either a full-benefit or a limited-benefit post-revision state. Patients who decline revision surgery remain in the failed state, accruing costs and reduced quality of life associated with a failed implant. Patients continue to be at risk for implant failure, may undergo more than one revision, and continue through the model until death or the age of 100 years. After the age of ninety years, we assume that revision surgery is not clinically viable and patients who have prosthetic failure remain in the failed state until death.
Fig. 1.
Diagram of health states and transitions. All hypothetical patients are also at risk of death while in each health state in the model. TKA = total knee arthroplasty, and UKA = unicompartmental knee arthroplasty.
Implant Failure and Revision Probabilities
Age-specific probabilities of implant failure and revision were calculated for primary total knee arthroplasty, primary unicompartmental knee arthroplasty, and revision total knee arthroplasty from the Swedish Knee Arthroplasty Register, which has the longest publicly available follow-up data (twenty years) on all unicompartmental and total knee arthroplasties performed in Sweden14,15. From the Swedish Register, we determined revision rates, which we transformed into annual probabilities16, and assumed that 80.0% of failed knee replacements were revised each year13. Age-specific implant failure rates (at younger than sixty-five years, sixty-five to seventy-four years, and more than seventy-four years) were directly available from the Swedish Register for the first ten years post-surgery14,15. We applied age-specific weights from years 1 to 10 to the average implant failure rates for years 11 to 20 in order to estimate age-specific rates. We assumed that the risk of failure after twenty years for each implant type and age cohort was the average failure rate from the previous ten years.
Complication Probabilities
Complications used in this analysis included joint infection, pneumonia, myocardial infarction, sepsis, stiffness or manipulation under anesthesia, and venous thromboembolism (deep vein thrombosis and pulmonary embolism)3,17-19. Unicompartmental knee arthroplasty is associated with a lower probability of joint infection (0.2% compared with 0.8% after total knee arthroplasty in the sixty-five-year-old cohort), stiffness or manipulation under anesthesia (0.4% compared with 5.0%), and venous thromboembolism (0.6% compared with 1.0%) than total knee arthroplasty (see Appendix E-1). The risk of myocardial infarction was found to be similar between unicompartmental knee arthroplasty and total knee arthroplasty17,19, and other systemic complication rates were also assumed to be similar between the procedures.
Mortality-Associated Probabilities
Nonsurgical mortality was estimated from age-specific 2008 U.S. vital statistics20. Mortality in the first year after surgery was assumed to be 2.2 times higher than nonsurgical mortality13.
Rehabilitation Probabilities
Utilization of inpatient rehabilitation services was based on Medicare claims data21. Of all patients who underwent total knee arthroplasty, 33.4% had inpatient rehabilitation, 30.1% had rehabilitation in a skilled-nursing facility, 22.2% had home-health-care rehabilitation, and 14.3% were discharged home with no post-acute care (see Appendix E-1). We assumed in the base case that all patients were discharged home after unicompartmental knee arthroplasty—that is, their utilization of rehabilitation services was similar to that of patients discharged home following total knee arthroplasty (63% of patients had home-health-care rehabilitation following unicompartmental knee arthroplasty and 37% were discharged home with no post-acute care)21.
Costs
We identified medical costs (for the procedure and for surgical complications) and rehabilitation costs (inpatient and outpatient) from national databases using Diagnosis-Related-Group (DRG); International Classification of Diseases, Ninth Revision (ICD-9); Current Procedural Terminology (CPT); and Clinical Classification Software (CCS) codes (see Appendix E-1). Unicompartmental knee arthroplasty, total knee arthroplasty, and revision total knee arthroplasty procedure costs were estimated with use of age-adjusted and severity-adjusted DRG codes (466, 467, 468, 469, and 470) from the Healthcare Cost and Utilization Project (HCUP) national hospital discharge database. Procedure costs were weighted by the frequency of cases with comorbid conditions, major comorbid conditions, or no comorbid conditions22. CPT codes (27446, 27447, and 27487) were used to estimate surgeon costs23. To obtain complication costs, we used the following corresponding ICD-9, CCS, or CPT codes: 996.65 (joint infection), 122 (pneumonia), 100 (myocardial infarction), 038 (sepsis), 718.56 and 27570 (stiffness), and 453.40 (venous thromboembolism). To estimate costs associated with implant failure, we used previously cited estimates that implant failure increased the cost of usual medical care for patients with osteoarthritis by 50.0%13.
Inpatient and home-health-care rehabilitation costs were based on the work by Buntin et al., who used Medicare claims data (see Appendix E-1)21. Other health-care-utilization costs were pharmacotherapy (oral, topical, and injectable agents) and physician, emergency department, and other outpatient visits, including physical therapy and occupational therapy visits24. All costs were adjusted to 2012 U.S. dollars25.
Quality of Life
Patients who have undergone unicompartmental knee arthroplasty have reported somewhat better range-of-motion and health outcomes compared with those who have undergone total knee arthroplasty26. However, we conservatively assumed that quality-of-life values were equivalent after unicompartmental and total knee arthroplasty in each health state in the base case27. We used age-adjusted quality-of-life values from a nationally representative sample for the full-benefit state28. We decreased those values by 9.0% for the limited-benefit state and by an additional 25.0% for the failed and revision health states13.
Sensitivity Analyses
We conducted one-way sensitivity analyses to identify threshold values at which base-case results would change. We varied the rates of unicompartmental knee arthroplasty failure, quality of life in full-benefit states, costs of rehabilitation, proportion of patients discharged home following unicompartmental knee arthroplasty, and costs of complications. We also assigned distributions to parameters with measurable uncertainty and varied these parameters in probabilistic sensitivity analyses to describe overall uncertainty in the model results. For the failure rates we used a beta distribution, for quality of life we used a normal distribution, and for complication and rehabilitation costs we used a gamma distribution13. The probabilistic sensitivity analyses varied these parameters in 10,000 Monte Carlo simulations that simultaneously sampled from each parameter distribution.
Potential Societal Cost Savings
Simulated lifetime costs were used to calculate the total societal cost savings of performing unicompartmental rather than total knee arthroplasties in the years 2015 and 2020, when the number of total knee arthroplasties is projected to reach one million annually9. We assumed that unicompartmental knee arthroplasties currently account for 8.0% of knee arthroplasty procedures5 and could currently account for 10.0% to 21.0%4. We also assumed that 50.0% of the population undergoing knee replacement were sixty-five years of age or older10. Our societal cost-savings calculations excluded the 8.0% of patients who would already have received unicompartmental knee arthroplasty.
Model Validation
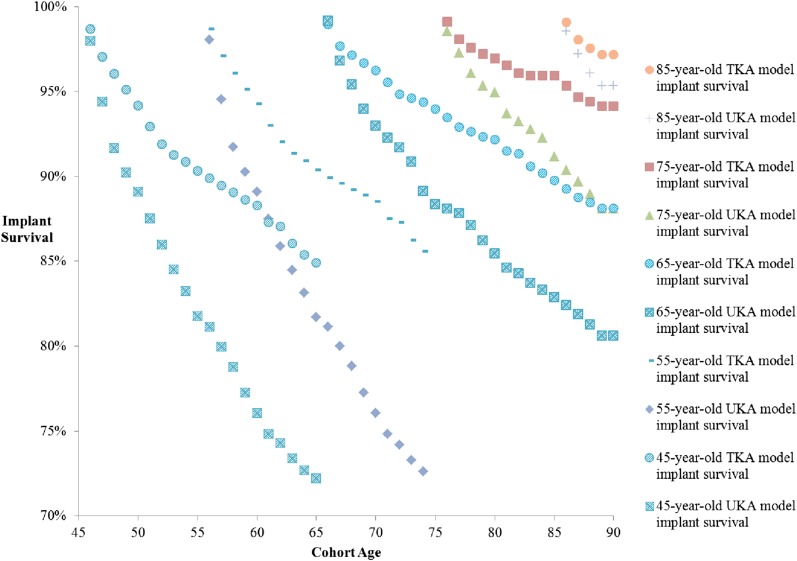
We tested the internal validity of our model, as recommended by the International Society for Pharmacoeconomics and Outcomes Research-Society for Medical Decision Making (ISPOR-SMDM) Modeling Good Research Practices Task Force-729, by comparing simulated revision rates (Fig. 2) against actual Swedish revision rates after twenty years of follow-up. Our simulated revision rates were on average 0.5% to 1.5% higher than actual revision rates reported in the Swedish Registry for each age cohort. However, these differences fell within reported confidence intervals reported by the Swedish Registry (see Appendix E-2)14. We were unable to validate failure rates past twenty years of follow-up because of a lack of longer-term follow-up data from registries.
Fig. 2.
Model output survival curves for total (TKA) and unicompartmental (UKA) knee arthroplasties in each age cohort. All survival curves are truncated at twenty years for simplicity, or at the age of ninety years—when a patient may no longer elect to have revision surgery.
Source of Funding
This study was funded in part by a grant from Mako Surgical Corp. The funding source had no role in the design and conduct of the study; in the collection, analysis, or interpretation of the data; or in the preparation, review, or approval of the study. H.M. Ghomrawi is supported in part by a career development grant from the Eunice Kennedy Shriver National Institute of Child Health & Human Development (K99 HD060686).
Results
The total lifetime costs associated with unicompartmental knee arthroplasty ranged from $35,000 for an eighty-five-year-old to $46,600 for a forty-five-year-old, whereas those for total knee arthroplasty ranged from $42,000 to $47,600, respectively (Table I). For all age groups, lifetime costs were higher for total knee arthroplasty than for unicompartmental knee arthroplasty, and the incremental difference increased with age. Total lifetime QALYs and incremental QALYs gained from total knee arthroplasty compared with those gained from unicompartmental knee arthroplasty decreased with age so that, by the age of sixty-five, unicompartmental knee arthroplasty had gained incrementally more QALYs than total knee arthroplasty. In the forty-five and fifty-five-year-old cohorts, total knee arthroplasty had an ICER of $30,300/QALY and $63,000/QALY, respectively. In the older cohorts, unicompartmental knee arthroplasty dominated total knee arthroplasty (had lower lifetime costs and higher lifetime QALYs compared with total knee arthroplasty and is a cost-effective alternative compared with total knee arthroplasty)30.
TABLE I.
Cost per QALY Gained for Total Knee Arthroplasty Compared with Unicompartmental Knee Arthroplasty According to Age at Time of Surgery*
| Age Cohort/Type of Knee Arthroplasty | Lifetime Costs (2012 U.S.$) | Lifetime QALYs | Incremental Costs (2012 U.S.$) | Incremental QALYs | Incremental Cost-Effectiveness Ratio ($/QALY) |
| Age 45 | |||||
| UKA | 46,600 | 17.240 | — | — | — |
| TKA | 47,600 | 17.272 | 1000 | 0.032 | 30,300 |
| Age 55 | |||||
| UKA | 44,800 | 14.118 | — | — | — |
| TKA | 46,500 | 14.145 | 1700 | 0.027 | 63,000 |
| Age 65 | |||||
| UKA | 38,100 | 10.721 | — | — | — |
| TKA | 43,400 | 10.714 | 5300 | −0.007 | Dominated† |
| Age 75 | |||||
| UKA | 35,500 | 7.114 | — | — | — |
| TKA | 41,600 | 7.109 | 6100 | −0.005 | Dominated† |
| Age 85 | |||||
| UKA | 35,000 | 3.866 | — | — | — |
| TKA | 42,000 | 3.864 | 7000 | −0.002 | Dominated† |
QALY = quality-adjusted life-year, UKA = unicompartmental knee arthroplasty, and TKA = total knee arthroplasty.
Total knee arthroplasty costs more and is less effective; therefore, unicompartmental knee arthroplasty strictly dominates total knee arthroplasty30.
Our base-case results were sensitive to changes in failure rates, quality of life, and rehabilitation costs but not to changes in complication costs (see Appendix E-1). Unicompartmental knee arthroplasty became cost-effective (below the $100,000/QALY willingness-to-pay threshold) for the forty-five-year-old cohort when its annual failure rate was reduced by 9.0% (fell from 18.2% to 16.8% [i.e., 1.5%] by year 10 and from 27.8% to 25.7% [i.e., 2.1%] by year 20) and became cost-effective for the fifty-five-year-old cohort when its annual failure rate was reduced by 4.5% (fell from 18.3% to 17.6% [i.e., 0.7%] by year 10 and from 27.9% to 26.7% [i.e., 1.2%] by year 20). Unicompartmental knee arthroplasty was more effective and less costly than total knee arthroplasty when its annual failure rate was decreased by 22% in the forty-five-year-old cohort (fell to 14.4% by year 10 and to 22.3% by year 20) and when its annual failure rate was decreased by 21% in the fifty-five-year-old cohort (fell to 14.7% by year 10 and to 22.9% by year 20).
In the second threshold analysis, we found that unicompartmental knee arthroplasty had an ICER of <$100,000/QALY when its full-benefit-state utility value was increased by 0.012 per year (a 1.4% increase from the base-case utility value) in the forty-five-year-old cohort and by 0.004 per year (a 0.5% increase from the base-case utility value) in the fifty-five-year-old cohort during the first three years post-surgery. Unicompartmental knee arthroplasty dominated total knee arthroplasty when the full-benefit-state utility value of unicompartmental knee arthroplasty was increased by 0.016 (a 1.8% increase) and 0.013 (1.5% increase) per year for the first three years post-surgery.
We also conducted a threshold analysis in the older cohorts (sixty-five years of age or older) to determine the effect of decreasing inpatient rehabilitation costs for total knee arthroplasty and increasing rehabilitation costs for unicompartmental knee arthroplasty, to reflect some proportion of patients requiring inpatient rehabilitation following unicompartmental knee arthroplasty. Unicompartmental knee arthroplasty was no longer cost-effective (that is, the ICER was >$100,000/QALY) when the rehabilitation costs following total knee arthroplasty were reduced by at least two-thirds of the base-case value of $9400 or when 45% of patients were discharged to inpatient rehabilitation facilities following unicompartmental knee arthroplasty (thereby increasing rehabilitation costs following unicompartmental knee arthroplasty from $2022 to >$8000). Finally, we varied complication costs and rates, but the results were not sensitive to those changes.
In the probabilistic sensitivity analysis, our model was robust to simultaneous changes in the cost of rehabilitation, failure rates, and quality of life. At a willingness-to-pay threshold of $100,000/QALY, total knee arthroplasty was cost-effective 66% and 57% of the time in the forty-five and fifty-five-year-old age groups, respectively. In the sixty-five, seventy-five, and eighty-five-year-old groups, unicompartmental knee arthroplasty was cost-effective 82%, 83%, and 87% of the time, respectively.
Total lifetime societal savings in the year 2015 ranged from $56 to $336 million when we varied the percentage of older patients qualifying as candidates for unicompartmental knee arthroplasty from 10.0% to 21.0%, respectively. These savings increased to $84 to $544 million in 2020. If unicompartmental knee arthroplasty becomes an economically favorable procedure in younger patients, societal savings would nearly double and range from $90 to $582 million in 2015 and from $167 to $1088 million in 2020, respectively.
Discussion
We believe that our study is the first to assess the cost-effectiveness of unicompartmental knee arthroplasty compared with that of total knee arthroplasty across the age spectrum of patients considering knee arthroplasty and indicates that the cost-effectiveness results vary with age. Unicompartmental knee arthroplasty was the dominant choice for patients sixty-five and older, and total knee arthroplasty was the cost-effective alternative for those who were forty-five and fifty-five.
Our results show that performing unicompartmental knee arthroplasty instead of total knee arthroplasty in older patients (sixty-five and older) has important economic implications with little effect on QALY gains, as reported in other studies7,8. Unicompartmental knee arthroplasty was associated with substantial lifetime savings, which were attributed in large part to lower rehabilitation costs. When we lowered the rehabilitation costs of total knee arthroplasty by at least two-thirds, unicompartmental knee arthroplasty was no longer cost-effective for older patients. Rehabilitation costs have been a target for cost containment over the past decade. Medicare has taken several measures to reduce both inpatient and outpatient rehabilitation costs, including the so-called “75% Rule” that limited access to inpatient rehabilitation facilities31 and more recently capping reimbursement for outpatient rehabilitation visits32. In addition, the proposed bundled payment for total knee arthroplasty provides hospitals with a strong incentive to discharge patients home33. These efforts should lower the rehabilitation costs of total knee arthroplasty but may penalize many patients who would otherwise benefit from institutionalized post-acute rehabilitation. Alternatively, our results favor utilizing unicompartmental knee arthroplasty in appropriate older patients who would not require post-acute rehabilitation.
Our base-case results favored total knee arthroplasty in younger patients. Although the lifetime costs of total knee arthroplasty were higher, the incremental difference in QALYs favored total knee arthroplasty (by 0.032 for the forty-five-year-old age group and 0.027 for the fifty-five-year-old age group). However, benefits of unicompartmental knee arthroplasty may appeal to younger patients who are still active and in the workforce, some of whom may feel that the immediate quality-of-life benefits outweigh the increased risk of revision when they are retired and less active. Very few studies have compared quality of life between unicompartmental and total knee arthroplasty at the time of follow-up, and the literature is divided between findings of no difference34,35 and an advantage for unicompartmental knee arthroplasty compared with total knee arthroplasty36.
Sensitivity analyses also suggest that only incremental improvements in implant survivorship are needed for unicompartmental knee arthroplasty to become a favorable choice for younger patients. If this survivorship improves slightly (an average 1.5% drop in the ten-year absolute revision rate) in forty-five-year-olds, unicompartmental knee arthroplasty would become a favorable option. Evidence suggests that the gap in revision rates between unicompartmental and total knee arthroplasty has been narrowing in recent years and is subject to different factors1,37. For example, unicompartmental knee arthroplasties performed in high-volume centers or by high-volume surgeons have been shown to have a six to eightfold decrease in revision rates38. Should third-party payers adopt these findings, reimbursement policies will have to be carefully devised to avoid unintended consequences of unicompartmental knee arthroplasties being performed in low-volume centers or by low-volume surgeons, which would increase revision rates.
Our results are limited by the data available from the Swedish Knee Arthroplasty Register, which provides follow-up rates for twenty years. This follow-up period was not sufficient for age groups in our model requiring more than twenty years of follow-up data, which we had to extrapolate. In addition, the observed difference in failure rates between total and unicompartmental knee arthroplasty may be associated with patient, clinical, and health-system factors that differ between Sweden and the U.S. Both unicompartmental knee arthroplasty and total knee arthroplasty are elective procedures, and in the absence of clear appropriateness criteria for surgery, these factors greatly affect surgical timing and subsequent outcomes39. Finally, our model did not account for comorbidities, which may impact perioperative and postoperative complications.
With the expected rise in utilization of knee arthroplasty, the number of candidates for unicompartmental knee arthroplasty will increase across the age spectrum. Our study shows that performing unicompartmental knee arthroplasty in appropriate older patients will have substantial economic benefits. Total knee arthroplasty remains cost-effective for younger patients who are candidates for either procedure; however, we identified areas of improvement that would make unicompartmental knee arthroplasty the favorable treatment.
Appendix
Tables showing model parameters and threshold analyses for unicompartmental compared with total knee arthroplasty in younger and older patients as well as graphs showing model and Swedish Registry implant survival curves are available with the online version of this article as a data supplement at jbjs.org.
Acknowledgments
Note: The authors thank Dr. Bruce Schackman and Dr. Ankur Pandya for providing assistance with the modeling methods and reviewing a previous version of the manuscript. They also thank Ms. Sophia Paul for assistance with data collection for the study.
Footnotes
Investigation performed at the Weill Cornell Medical College and the Hospital for Special Surgery, New York, NY
Disclosure: One or more of the authors received payments or services, either directly or indirectly (i.e., via his or her institution), from a third party in support of an aspect of this work. In addition, one or more of the authors, or his or her institution, has had a financial relationship, in the thirty-six months prior to submission of this work, with an entity in the biomedical arena that could be perceived to influence or have the potential to influence what is written in this work. No author has had any other relationships, or has engaged in any other activities, that could be perceived to influence or have the potential to influence what is written in this work. The complete Disclosures of Potential Conflicts of Interest submitted by authors are always provided with the online version of the article.
References
- 1.Mckeon BP, Rand JD. Treatment of osteoarthritis of the middle-aged athlete. Sports Med Arthrosc. 2013March;21(1):52-60. [DOI] [PubMed] [Google Scholar]
- 2.Richmond BI, Hadlow SV, Lynskey TG, Walker CG, Munro JT. Proximal tibial bone density is preserved after unicompartmental knee arthroplasty. Clin Orthop Relat Res. 2013May;471(5):1661-9 Epub 2013 Jan 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brown NM, Sheth NP, Davis K, Berend ME, Lombardi AV, Berend KR, Della Valle CJ. Total knee arthroplasty has higher postoperative morbidity than unicompartmental knee arthroplasty: a multicenter analysis. J Arthroplasty. 2012September;27(8)(Suppl):86-90 Epub 2012 May 4. [DOI] [PubMed] [Google Scholar]
- 4.Arno S, Maffei D, Walker PS, Schwarzkopf R, Desai P, Steiner GC. Retrospective analysis of total knee arthroplasty cases for visual, histological, and clinical eligibility of unicompartmental knee arthroplasties. J Arthroplasty. 2011December;26(8):1396-403 Epub 2011 Feb 25. [DOI] [PubMed] [Google Scholar]
- 5.Riddle DL, Jiranek WA, McGlynn FJ. Yearly incidence of unicompartmental knee arthroplasty in the United States. J Arthroplasty. 2008April;23(3):408-12 Epub 2007 Nov 26. [DOI] [PubMed] [Google Scholar]
- 6.Daigle ME, Weinstein AM, Katz JN, Losina E. The cost-effectiveness of total joint arthroplasty: a systematic review of published literature. Best Pract Res Clin Rheumatol. 2012October;26(5):649-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Slover J, Espehaug B, Havelin LI, Engesaeter LB, Furnes O, Tomek I, Tosteson A. Cost-effectiveness of unicompartmental and total knee arthroplasty in elderly low-demand patients. A Markov decision analysis. J Bone Joint Surg Am. 2006November;88(11):2348-55 Epub 2006 Nov 3. [DOI] [PubMed] [Google Scholar]
- 8.Soohoo NF, Sharifi H, Kominski G, Lieberman JR. Cost-effectiveness analysis of unicompartmental knee arthroplasty as an alternative to total knee arthroplasty for unicompartmental osteoarthritis. J Bone Joint Surg Am. 2006September;88(9):1975-82 Epub 2006 Sep 5. [DOI] [PubMed] [Google Scholar]
- 9.Kurtz SM, Ong KL, Lau E, Bozic KJ. Impact of the economic downturn on total joint replacement demand in the United States: updated projections to 2021. J Bone Joint Surg Am. 2014April16;96(8):624-30. [DOI] [PubMed] [Google Scholar]
- 10.Kurtz SM, Lau E, Ong K, Zhao K, Kelly M, Bozic KJ. Future young patient demand for primary and revision joint replacement: national projections from 2010 to 2030. Clin Orthop Relat Res. 2009October;467(10):2606-12 Epub 2009 Apr 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gold MR, Siegel JE, Russell LB, Weinstein MC. Cost effectiveness in health and medicine. Oxford, UK: Oxford University Press; 1996. [Google Scholar]
- 12.Lyman S. Prospective evaluation of the clinical and economic outcomes of total joint replacement: the HSS knee arthroplasty cohort. Hospital for Special Surgery arthroplasty registry. 2013. http://www.hss.edu/research-patient-registries.asp. Accessed 2014 Oct 28.
- 13.Losina E, Walensky RP, Kessler CL, Emrani PS, Reichmann WM, Wright EA, Holt HL, Solomon DH, Yelin E, Paltiel AD, Katz JN. Cost-effectiveness of total knee arthroplasty in the United States: patient risk and hospital volume. Arch Intern Med. 2009June22;169(12):1113-21; discussion 1121-2. Epub 2009 Jun 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Swedish Knee Arthroplasty Register. Annual report 2012. http://www.myknee.se/en/publications/annual-reports. Accessed 2014 Oct 28.
- 15.Hopley CD, Crossett LS, Chen AF. Long-term clinical outcomes and survivorship after total knee arthroplasty using a rotating platform knee prosthesis: a meta-analysis. J Arthroplasty. 2013January;28(1):68-77e1:3. Epub 2012 Sep 21. [DOI] [PubMed] [Google Scholar]
- 16.Sonnenberg FA, Beck JR. Markov models in medical decision making: a practical guide. Med Decis Making. 1993Oct-Dec;13(4):322-38. [DOI] [PubMed] [Google Scholar]
- 17.Cram P, Lu X, Kates SL, Singh JA, Li Y, Wolf BR. Total knee arthroplasty volume, utilization, and outcomes among Medicare beneficiaries, 1991-2010. JAMA. 2012September26;308(12):1227-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Katz JN, Barrett J, Mahomed NN, Baron JA, Wright RJ, Losina E. Association between hospital and surgeon procedure volume and the outcomes of total knee replacement. J Bone Joint Surg Am. 2004September;86(9):1909-16 Epub 2004 Sep 3. [DOI] [PubMed] [Google Scholar]
- 19.Morris MJ, Molli RG, Berend KR, Lombardi AV Jr. Mortality and perioperative complications after unicompartmental knee arthroplasty. Knee. 2013June;20(3):218-20 Epub 2012 Nov 14. [DOI] [PubMed] [Google Scholar]
- 20.Arias E. United States life tables, 2008. Natl Vital Stat Rep. 2012September24;61(3):1-63 http://www.cdc.gov/nchs/data/nvsr/nvsr61/nvsr61_03.pdf. Accessed 2014 Oct 28. [PubMed] [Google Scholar]
- 21.Buntin MB, Deb P, Escarce JJ, Hoverman C, Paddock S, Sood N. Comparison of Medicare spending and outcomes for beneficiaries with lower extremity joint replacements. WR-271-MEDPAC. Santa Monica, CA: RAND Health; 2005.
- 22.Agency for Healthcare Research and Quality. Welcome to H•CUPnet. 2011. http://hcupnet.ahrq.gov/. Accessed 2014 Jan 14.
- 23.Centers for Medicare & Medicaid Services. Physician fee schedule. Details for title: 2012. http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/PhysicianFeeSched/PFS-Relative-Value-Files-Items/RVU12D.html. Accessed 2014 Jan 14.
- 24.Bozic KJ, Stacey B, Berger A, Sadosky A, Oster G. Resource utilization and costs before and after total joint arthroplasty. BMC Health Serv Res. 2012;12:73 Epub 2012 Mar 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.U.S. Department of Labor, Bureau of Labor Statistics. Consumer price index - urban consumers. 2012. http://www.bls.gov/cpi/. Accessed 2014 Jan 14.
- 26.Griffin T, Rowden N, Morgan D, Atkinson R, Woodruff P, Maddern G. Unicompartmental knee arthroplasty for the treatment of unicompartmental osteoarthritis: a systematic study. ANZ J Surg. 2007April;77(4):214-21. [DOI] [PubMed] [Google Scholar]
- 27.Sweeney K, Grubisic M, Marra CA, Kendall R, Li LC, Lynd LD. Comparison of HRQL between unicompartmental knee arthroplasty and total knee arthroplasty for the treatment of osteoarthritis. J Arthroplasty. 2013October;28(9)(Suppl):187-90 Epub 2013 Jul 11. [DOI] [PubMed] [Google Scholar]
- 28.Sullivan PW, Ghushchyan V. Preference-based EQ-5D index scores for chronic conditions in the United States. Med Decis Making. 2006Jul-Aug;26(4):410-20 Epub 2006 Jul 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Eddy DM, Hollingworth W, Caro JJ, Tsevat J, McDonald KM, Wong JB; ISPOR-SMDM Modeling Good Research Practices Task Force. Model transparency and validation: a report of the ISPOR-SMDM Modeling Good Research Practices Task Force-7. Med Decis Making. 2012Sep-Oct;32(5):733-43. [DOI] [PubMed] [Google Scholar]
- 30.Drummond MF, Sculpher MJ, Torrance GW, O’Brien BJ, Stoddart GL. Methods for the economic evaluation of health care programmes. 3rd ed.New York: Oxford University Press; 2005. [Google Scholar]
- 31.Pezzin LE, Roberts BA, Miao H, Dillingham TR. Regulatory policies, the “75% rule,” and post-acute care discharge setting. Am J Phys Med Rehabil. 2011November;90(11):954-8. [DOI] [PubMed] [Google Scholar]
- 32.Center for Medicare & Medicaid Services. Medicare limits on therapy services. 2014. http://www.medicare.gov/Pubs/pdf/10988.pdf. Accessed 2014 Jan 14.
- 33.Sood N, Huckfeldt PJ, Escarce JJ, Grabowski DC, Newhouse JP. Medicare’s bundled payment pilot for acute and postacute care: analysis and recommendations on where to begin. Health Aff (Millwood). 2011September;30(9):1708-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lygre SH, Espehaug B, Havelin LI, Furnes O, Vollset SE. Pain and function in patients after primary unicompartmental and total knee arthroplasty. J Bone Joint Surg Am. 2010December15;92(18):2890-7. [DOI] [PubMed] [Google Scholar]
- 35.Dalury DF, Fisher DA, Adams MJ, Gonzales RA. Unicompartmental knee arthroplasty compares favorably to total knee arthroplasty in the same patient. Orthopedics. 2009April;32(4). [PubMed] [Google Scholar]
- 36.Noticewala MS, Geller JA, Lee JH, Macaulay W. Unicompartmental knee arthroplasty relieves pain and improves function more than total knee arthroplasty. J Arthroplasty. 2012September;27(8)(Suppl):99-105 Epub 2012 May 31. [DOI] [PubMed] [Google Scholar]
- 37.Newman J, Pydisetty RV, Ackroyd C. Unicompartmental or total knee replacement: the 15-year results of a prospective randomised controlled trial. J Bone Joint Surg Br. 2009January;91(1):52-7. [DOI] [PubMed] [Google Scholar]
- 38.Baker P, Jameson S, Critchley R, Reed M, Gregg P, Deehan D. Center and surgeon volume influence the revision rate following unicondylar knee replacement: an analysis of 23,400 medial cemented unicondylar knee replacements. J Bone Joint Surg Am. 2013April17;95(8):702-9. [DOI] [PubMed] [Google Scholar]
- 39.Ghomrawi HM, Schackman BR, Mushlin AI. Appropriateness criteria and elective procedures—total joint arthroplasty. N Engl J Med. 2012December27;367(26):2467-9. [DOI] [PubMed] [Google Scholar]