Abstract
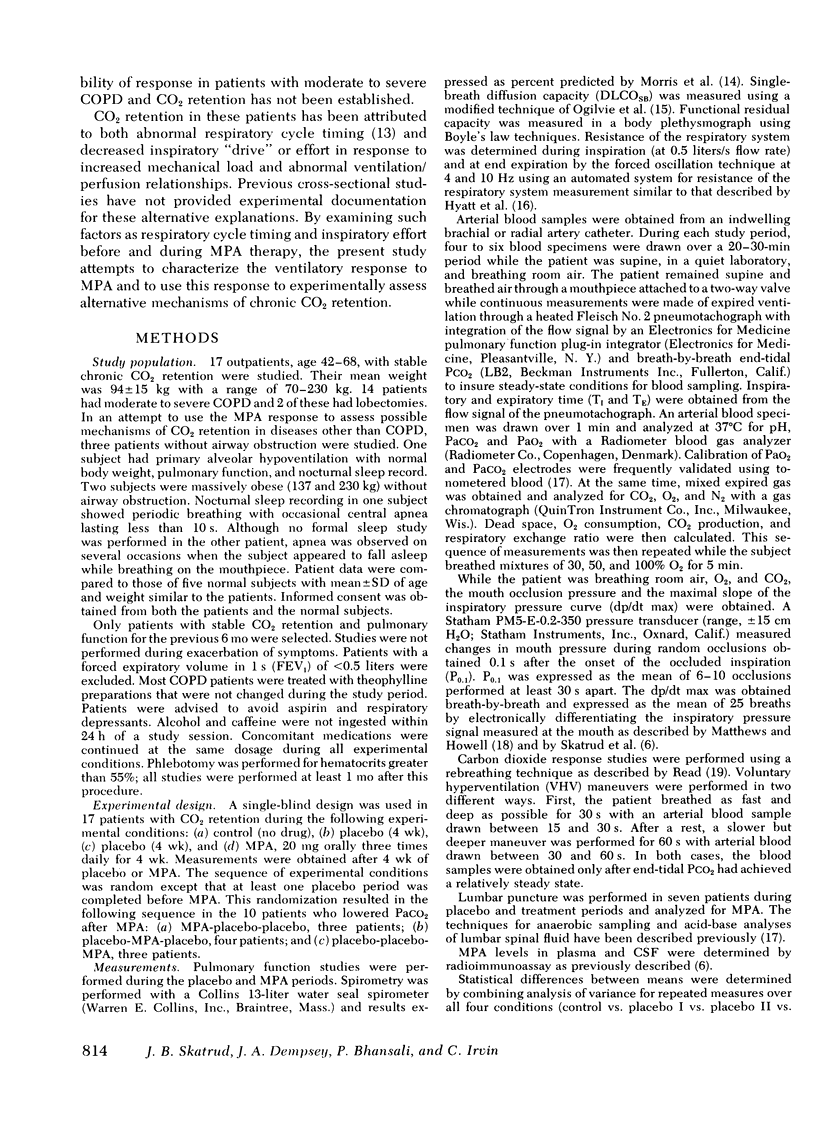
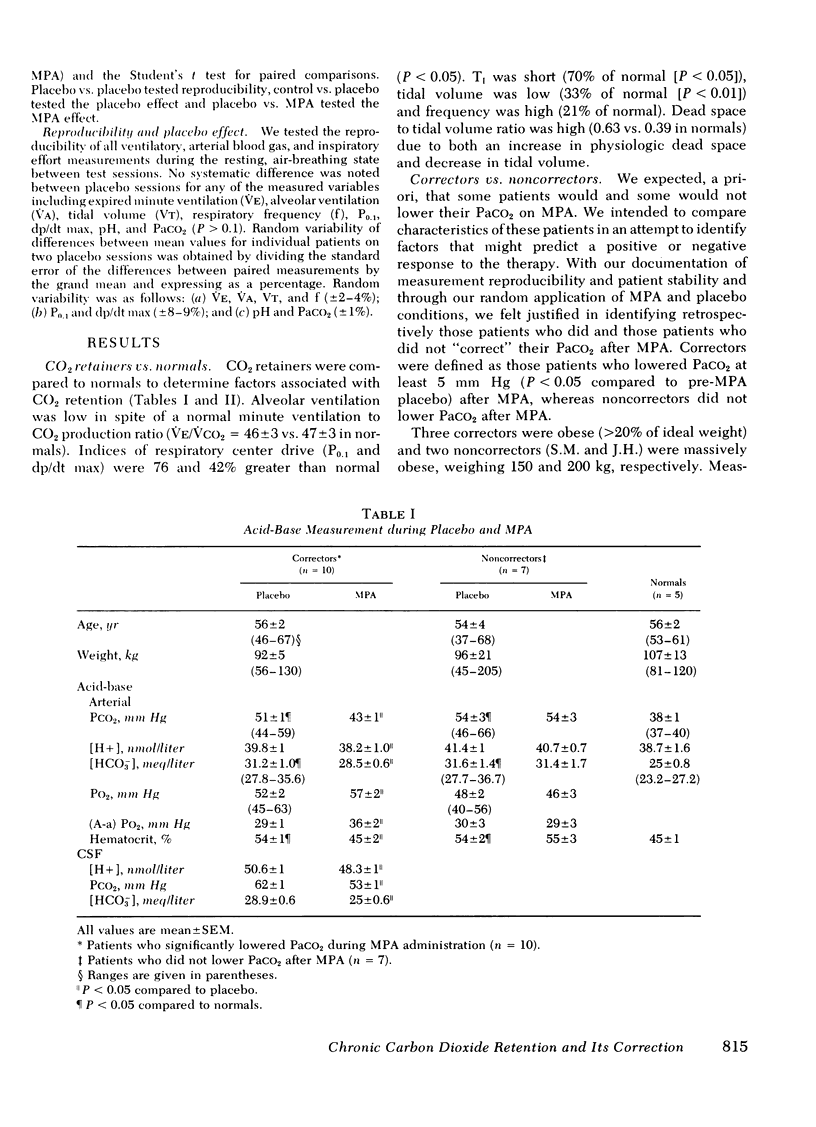
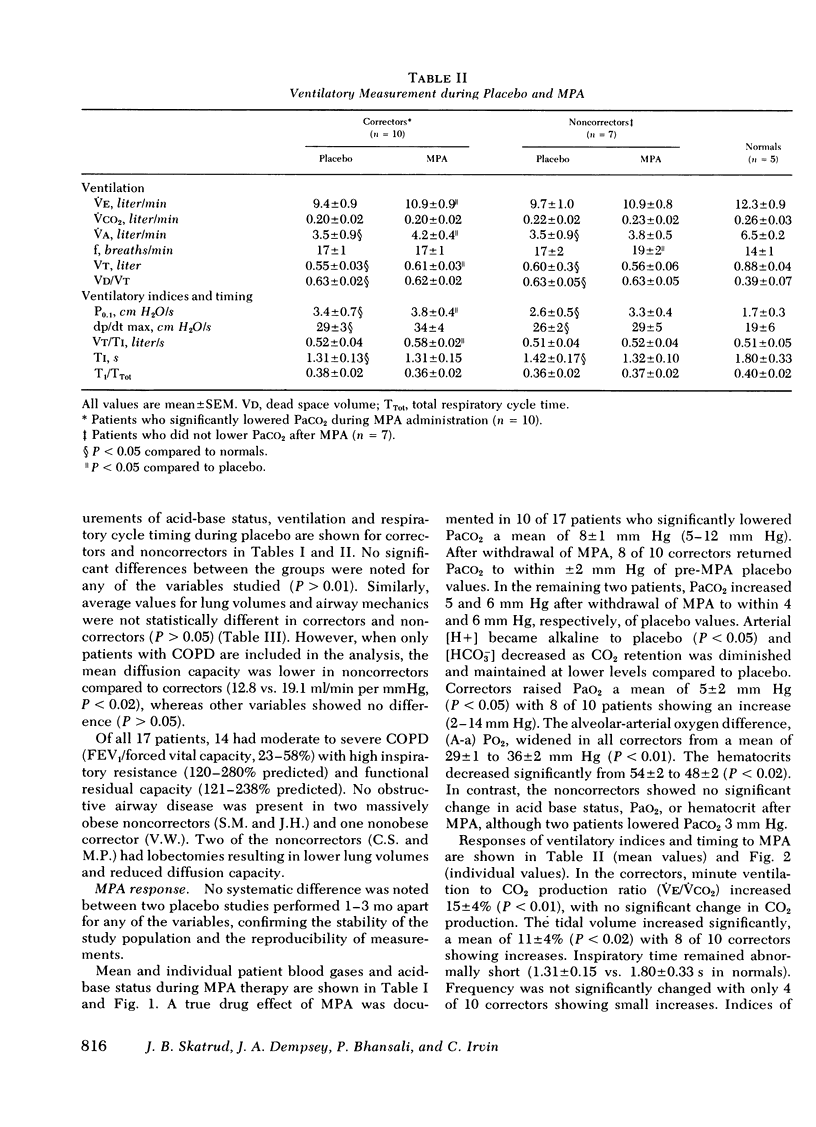
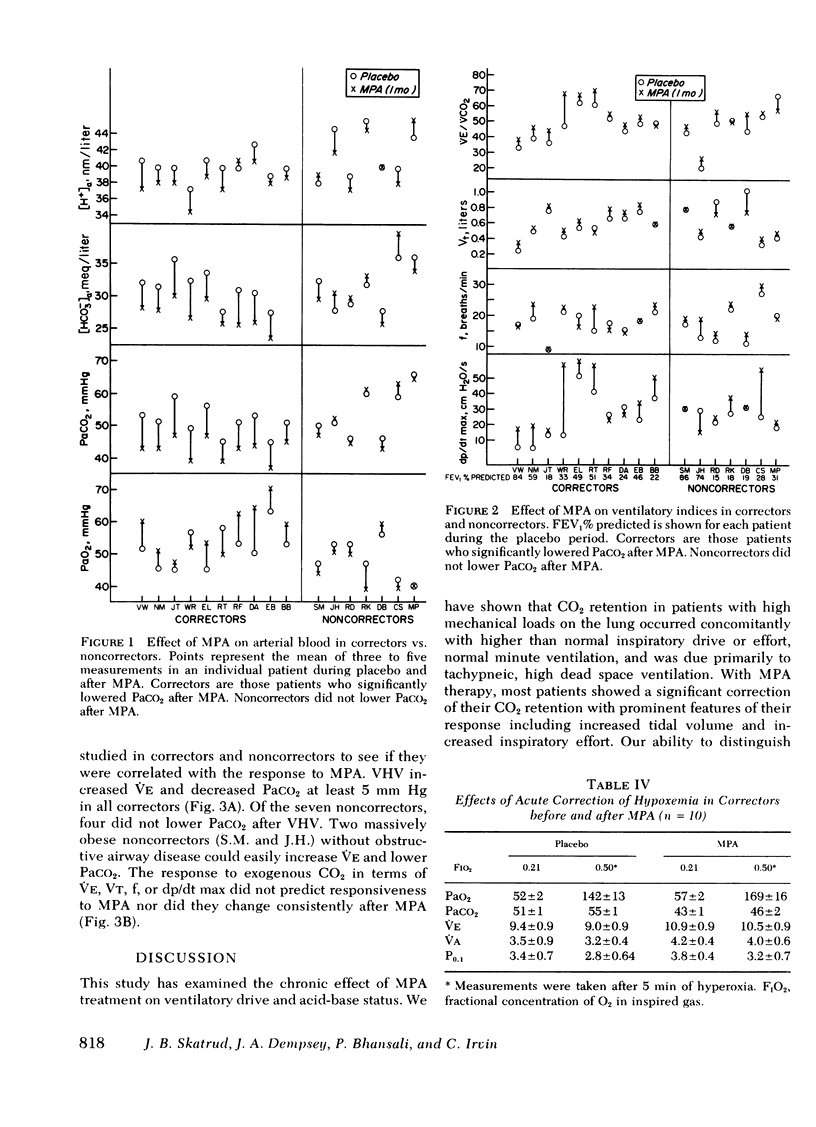
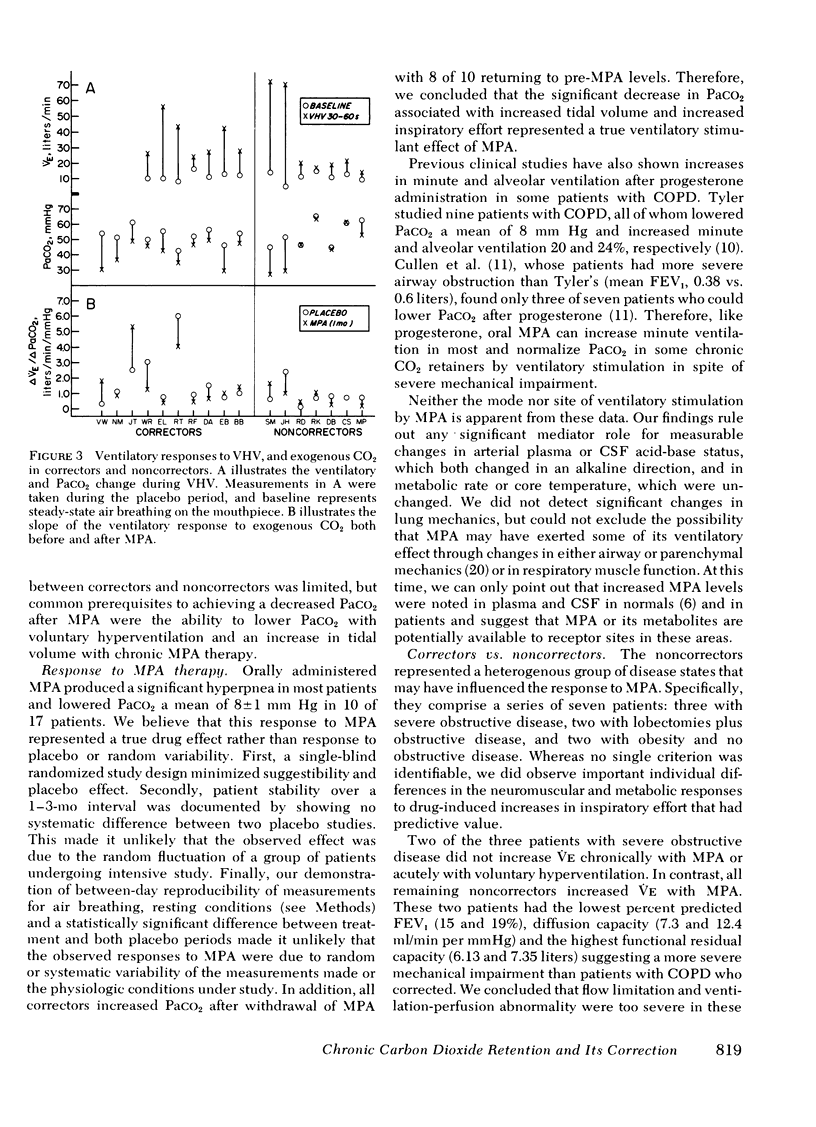
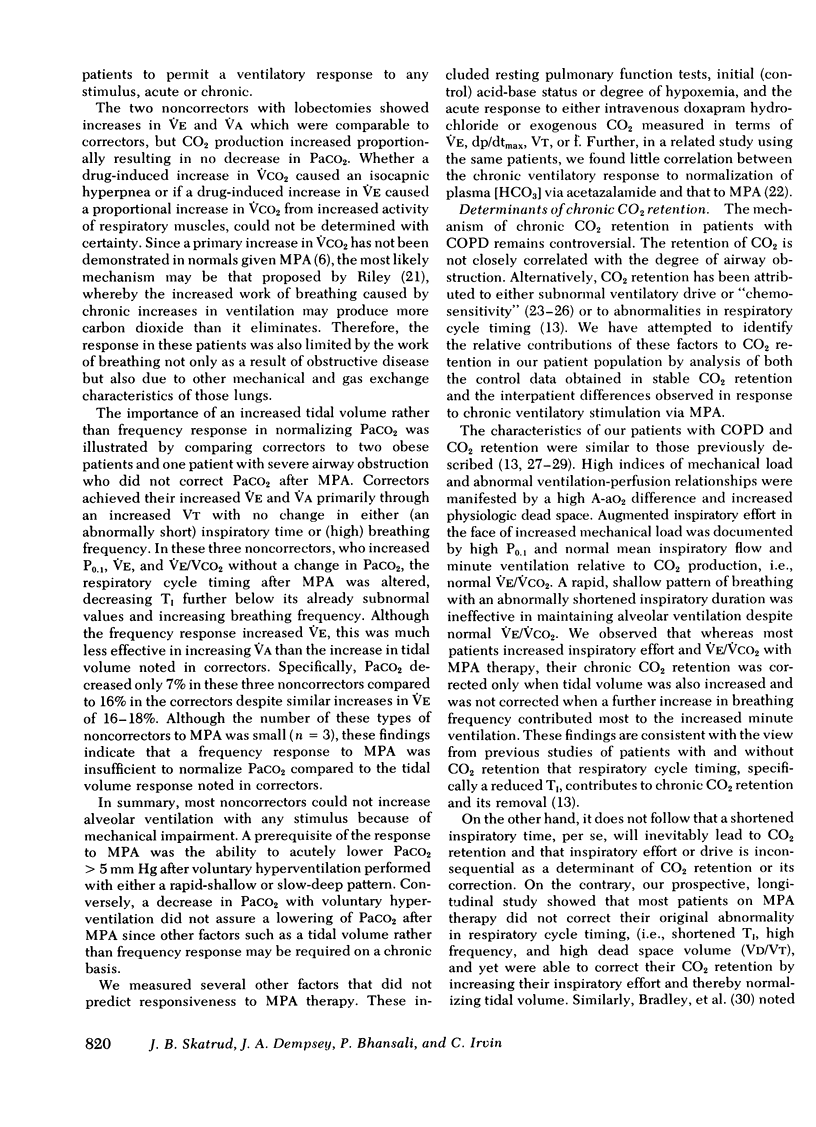
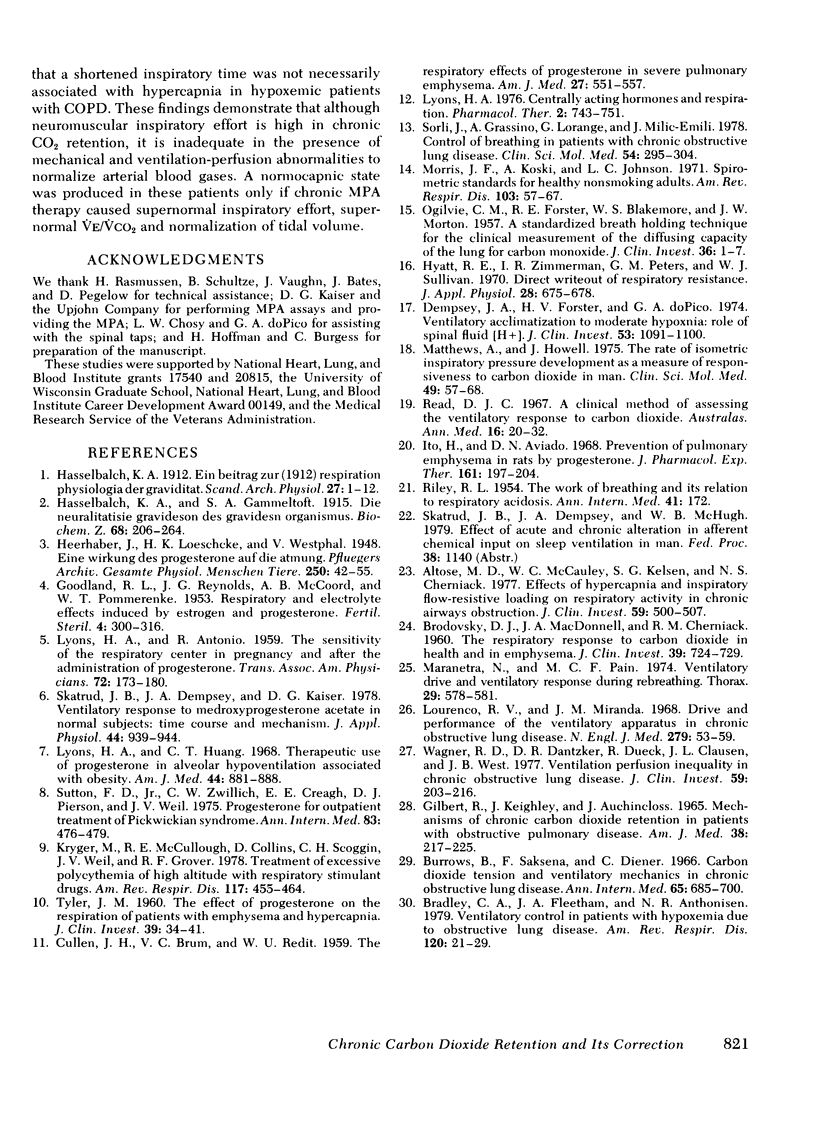
17 patients with chronic ventilatory failure (including 14 with chronic obstructive pulmonary disease) were studied to determine the causes of carbon dioxide retention and the chronic effect of medroxyprogesterone acetate on ventilatory drive and acid-base status. Carbon dioxide retention in patients with high mechanical loads occurred concomitantly with a higher than normal inspiratory effort (mouth occlusion pressure) and normal minute ventilation to carbon dioxide production ratio (V̇e/V̇co2); but with shortened inspiratory time (1.3±0.1 vs. 1.8±3 s), increased breathing frequency (17±1 vs. 14±1 breaths/min), low tidal volume (0.57±0.03 vs. 0.88±0.04 L), and high dead space to tidal volume ratio (0.63±0.02 vs. 0.39±0.07). Using a randomized application of treatment and placebo conditions, it was shown that 4 wk of medroxyprogesterone acetate caused significant reductions in Paco2 (from 51±1 to 42±1 mm Hg) in 10 of 17 patients. This “correction” of Paco2 in these patients was associated with increases in mouth occlusion pressure (14%), tidal volume (11%), and alveolar ventilation (15%) compared to placebo, although inspiratory time remained shortened. Arterial and lumbar cerebrospinal fluid pH was alkaline compared to placebo in patients who “corrected” Paco2. No change was noted in lung mechanics or core temperature. Common prerequisites for correction of Paco2 with medroxyprogesterone acetate treatment were the ability to significantly lower Paco2 upon acute voluntary hyperventilation and to increase tidal volume rather than breathing frequency in response to the drug. We attribute chronic CO2 retention in these patients to alterations in respiratory cycle timing and to a neuromuscular inspiratory effort which is adequate for the level of tissue CO2 production, but inadequate in the presence of mechanical and ventilation-perfusion abnormalities to normalize arterial blood gases.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Altose M. D., McCauley W. C., Kelsen S. G., Cherniack N. S. Effects of hypercapnia and inspiratory flow-resistive loading on respiratory activity in chronic airways obstruction. J Clin Invest. 1977 Mar;59(3):500–507. doi: 10.1172/JCI108665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- BLAKEMORE W. S., FORSTER R. E., MORTON J. W., OGILVIE C. M. A standardized breath holding technique for the clinical measurement of the diffusing capacity of the lung for carbon monoxide. J Clin Invest. 1957 Jan;36(1 Pt 1):1–17. doi: 10.1172/JCI103402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- BRODOVSKY D., MACDONELL J. A., CHERNIACK R. M. The respiratory response to carbon dioxide in health and in emphysema. J Clin Invest. 1960 May;39:724–729. doi: 10.1172/JCI104089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradley C. A., Fleetham J. A., Anthonisen N. R. Ventilatory control in patients with hypoxemia due to obstructive lung disease. Am Rev Respir Dis. 1979 Jul;120(1):21–30. doi: 10.1164/arrd.1979.120.1.21. [DOI] [PubMed] [Google Scholar]
- Burrows B., Saksena F. B., Diener C. F. Carbon dioxide tension and ventilatory mechanics in chronic obstructie lung disease. Ann Intern Med. 1966 Oct;65(4):685–700. doi: 10.7326/0003-4819-65-4-685. [DOI] [PubMed] [Google Scholar]
- CULLEN J. H., BRUM V. C., REIDT W. U. The respiratory effects of progesterone in severe pulmonary emphysema. Am J Med. 1959 Oct;27:551–557. doi: 10.1016/0002-9343(59)90040-3. [DOI] [PubMed] [Google Scholar]
- Dempsey J. A., Forster H. V., DoPico G. A. Ventilatory acclimatization to moderate hypoxemia in man. The role of spinal fluid (H+). J Clin Invest. 1974 Apr;53(4):1091–1100. doi: 10.1172/JCI107646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- GILBERT R., KEIGHLEY J., AUCHINCLOSS J. H., Jr MECHANISMS OF CHRONIC CARBON DIOXIDE RETENTION IN PATIENTS WITH OBSTRUCTIVE PULMONARY DISEASE. Am J Med. 1965 Feb;38:217–225. doi: 10.1016/0002-9343(65)90175-0. [DOI] [PubMed] [Google Scholar]
- GOODLAND R. L., REYNOLDS J. G., MCCOORD A. B., POMMERENKE W. T. Respiratory and electrolyte effects induced by estrogen and progesterone. Fertil Steril. 1953 Jul-Aug;4(4):300–317. doi: 10.1016/s0015-0282(16)31327-9. [DOI] [PubMed] [Google Scholar]
- Hyatt R. E., Zimmerman I. R., Peters G. M., Sullivan W. J. Direct writeout of total respiratory resistance. J Appl Physiol. 1970 May;28(5):675–678. doi: 10.1152/jappl.1970.28.5.675. [DOI] [PubMed] [Google Scholar]
- Ito H., Aviado D. M. Prevention of pulmonary emphysema in rats by progesterone. J Pharmacol Exp Ther. 1968 Jun;161(2):197–204. [PubMed] [Google Scholar]
- Kryger M., McCullough R. E., Collins D., Scoggin C. H., Weil J. V., Grover R. F. Treatment of excessive polycythemia of high altitude with respiratory stimulant drugs. Am Rev Respir Dis. 1978 Mar;117(3):455–464. doi: 10.1164/arrd.1978.117.3.455. [DOI] [PubMed] [Google Scholar]
- Lourenço R. V., Miranda J. M. Drive and performance of the ventilatory apparatus in chronic obstructive lung disease. N Engl J Med. 1968 Jul 11;279(2):53–59. doi: 10.1056/NEJM196807112790201. [DOI] [PubMed] [Google Scholar]
- Lyons H. A. Centrally acting hormones and respiration. Pharmacol Ther B. 1976;2(4):743–751. doi: 10.1016/0306-039x(76)90076-3. [DOI] [PubMed] [Google Scholar]
- Lyons H. A., Huang C. T. Therapeutic use of progesterone in alveolar hypoventilation associated with obesity. Am J Med. 1968 Jun;44(6):881–888. doi: 10.1016/0002-9343(68)90088-0. [DOI] [PubMed] [Google Scholar]
- Maranetra N., Pain M. C. Ventilatory drive and ventilatory response during rebreathing. Thorax. 1974 Sep;29(5):578–581. doi: 10.1136/thx.29.5.578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matthews A. W., Howell J. B. The rate of isometric inspiratory pressure development as a measure of responsiveness to carbon dioxide in man. Clin Sci Mol Med. 1975 Jul;49(1):57–68. doi: 10.1042/cs0490057. [DOI] [PubMed] [Google Scholar]
- Morris J. F., Koski A., Johnson L. C. Spirometric standards for healthy nonsmoking adults. Am Rev Respir Dis. 1971 Jan;103(1):57–67. doi: 10.1164/arrd.1971.103.1.57. [DOI] [PubMed] [Google Scholar]
- Read D. J. A clinical method for assessing the ventilatory response to carbon dioxide. Australas Ann Med. 1967 Feb;16(1):20–32. doi: 10.1111/imj.1967.16.1.20. [DOI] [PubMed] [Google Scholar]
- Sorli J., Grassino A., Lorange G., Milic-Emili J. Control of breathing in patients with chronic obstructive lung disease. Clin Sci Mol Med. 1978 Mar;54(3):295–304. doi: 10.1042/cs0540295. [DOI] [PubMed] [Google Scholar]
- Sutton F. D., Jr, Zwillich C. W., Creagh C. E., Pierson D. J., Weil J. V. Progesterone for outpatient treatment of Pickwickian syndrome. Ann Intern Med. 1975 Oct;83(4):476–479. doi: 10.7326/0003-4819-83-4-476. [DOI] [PubMed] [Google Scholar]
- TYLER J. M. The effect of progesterone on the respiration of patients with emphysema and hypercapnia. J Clin Invest. 1960 Jan;39:34–41. doi: 10.1172/JCI104024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wagner P. D., Dantzker D. R., Dueck R., Clausen J. L., West J. B. Ventilation-perfusion inequality in chronic obstructive pulmonary disease. J Clin Invest. 1977 Feb;59(2):203–216. doi: 10.1172/JCI108630. [DOI] [PMC free article] [PubMed] [Google Scholar]



