Abstract
Objectives
Few studies outside United Kingdom have documented effects of mentalization-based treatment (MBT) for patients with borderline personality disorder (BPD). This study aimed to investigate outcomes for BPD patients treated in an MBT programme in a Norwegian specialist treatment unit and compare benefits of the implemented MBT with the unit's former psychodynamic treatment programme.
Design
A naturalistic, longitudinal, comparison of treatment effects for BPD patients before and after transition to MBT.
Methods
The sample consisted of 345 BPD patients treated in the period 1993–2013. Before 2008, patients were admitted to a psychodynamic treatment programme (n = 281), after 2008 patients received MBT (n = 64). Symptom distress, interpersonal problems, and global functioning were assessed repeatedly throughout the treatment. Suicidal/self-harming acts, hospital admissions, medication, and occupational status were assessed at the start and end of treatment. Therapists' competence and adherence to MBT was rated and found satisfactory. The statistical method for longitudinal analyses was mixed models.
Results
BPD patients in MBT and in the former psychodynamic treatment programme had comparable baseline severity and impairments of functioning. BPD patients in MBT had a remarkably low drop-out rate (2%), significantly lower than the former treatment. Improvements of symptom distress, interpersonal, global and occupational functioning were significantly greater for MBT patients. Large reductions in suicidal/self-harming acts, hospital admissions, and use of medication were evident in the course of both treatments.
Conclusions
The study confirms the effectiveness of MBT for BPD patients and indicates greater clinical benefits than in traditional psychodynamic treatment programmes.
Practitioner points
MBT is an effective treatment for patients with BPD.
MBT can successfully be implemented in therapeutic settings outside United Kingdom and may be more beneficial than psychodynamic treatment programmes for BPD patients.
Keywords: mentalization-based treatment, MBT, borderline personality disorder, step-down programme, psychodynamic psychotherapy, group psychotherapy
Background
Mentalization-based treatment (MBT) has been found effective for patients with borderline personality disorder (BPD) in two randomized trials for adults (Bateman & Fonagy, 2001, 2008, 2009) and in one for adolescents (Rossouw & Fonagy, 2012). Outside the United Kingdom, results have so far been more divergent. While positive outcomes were replicated in a Dutch naturalistic study (Bales et al., 2012), small benefits were reported in a Danish trial (Jorgensen et al., 2012). These studies have the limitation of lacking measurements of therapist adherence to MBT, and it is therefore uncertain to which extent treatments labelled MBT actually represent the same treatment approach. Accordingly, two research questions are highly relevant: (1) Can MBT be successfully implemented outside the milieu of origin, that is, London, UK, and (2) Is ‘therapist adherent MBT’ better than other high-quality treatments for BPD?
Mentalization-based treatment was implemented at the Department for Personality Psychiatry in August 2008. The department had previously offered patients treatment in a psychodynamic programme. Patients admitted to MBT and to the former psychodynamic treatment were recruited from the same catchment area, the city of Oslo, Norway. This study aims to compare outcomes for BPD patients who either received MBT or the former psychodynamic treatment programme.
Implementation of MBT involved retraining of clinical staff with respect to theoretical understanding and therapeutic techniques, through a series of courses and seminars in close collaboration with Anthony Bateman, one of the founders of MBT. A Nordic group for MBT was established which worked towards a consensus of what should count as MBT within a Nordic culture and language tradition. As a result three manuals were published: (1) Manual for individual MBT (Karterud & Bateman, 2010), (2) Manual for psychoeducational MBT (Karterud & Bateman, 2011), and (3) Manual for group MBT (Karterud, 2012). We also designed and tested an MBT Adherence and Competence Scale (MBT-ACS; Karterud et al., 2013). This study is thus able to include ratings of therapist MBT adherence and competence.
The comparison treatment, the former psychodynamic programme, represents a highly specialized, multifaceted, and structured long-term treatment on a specialist level, specially designed for personality disorders. Patients were first admitted to 18 weeks in a day hospital treatment programme and thereafter offered weekly long-term outpatient group psychotherapy. In previous MBT trials, the comparison groups were either non-specialist or less intensive treatments. In the first MBT trial (Bateman & Fonagy, 2001) and in the study of adolescents (Rossouw & Fonagy, 2012), comparison groups received community-based psychiatric treatment, defined as treatment as usual. The comparison group in the second MBT trial (Bateman & Fonagy, 2009) received a defined combination of individual and group therapy termed ‘Structured Clinical Management for BPD patients – best clinical practice’. This treatment was characterized as a supportive approach, had 18 months duration, and was delivered by non-specialist practitioners within United Kingdom psychiatric services. In the Danish study (Jorgensen et al., 2012), the comparison group received supportive group psychotherapy, every second week, for a maximum of 18 months. The psychodynamic treatment in this study is thus more comprehensive and specialized than the comparison groups in previous MBT studies.
Clinical effects of the former psychodynamic treatment programme have been described in naturalistic studies (Wilberg, Karterud, Urnes, Pedersen, & Friis, 1998; Wilberg et al., 2003) and in a trial comparing the psychodynamic programme with individual outpatient psychotherapy by experts (The Ullevål Personality Project, UPP: Gullestad et al., 2012; Kvarstein et al., 2013). Although the main treatment results for BPD patients were reasonably good, drop-out rates were high (Kvarstein, Karterud, & Pedersen, 2004), and long-term outcomes associated with early drop-out were poor (Kvarstein & Karterud, 2013).
The main research questions for this study are the following: (1) Is MBT as implemented in a Norwegian treatment unit, effective for BPD patients? (2) Is MBT associated with greater clinical benefits for BPD patients compared to a psychodynamic treatment programme?
Material and methods
Subjects
Patients with BPD were selected (n = 345) from a total of 907 patients with different personality disorders admitted to specialist treatment at the Department of Personality Psychiatry during 1993–2013. Patients treated before 2008 received the traditional psychodynamic treatment (n = 281, 83% females, mean age 30 years, standard deviation [SD] 7), and patients treated between 2008 and 2013 received MBT (n = 64, 84% females, mean age 26 years, SD 6). Patients treated in the transition period (n = 16) and patients included in a randomized controlled trial (the UPP) during 2004–2006 (n = 25) were excluded.
Mentalization-based treatment
The MBT followed guidelines (Bateman & Fonagy, 2006) and manuals for individual (Karterud & Bateman, 2010), psychoeducational (Karterud & Bateman, 2011), and group MBT (Karterud, 2012). When starting treatment, a mentalization-based case formulation (Simonsen, Nørgaard, Larsen, & Bjørnholm, 2011) was made for each patient and when indicated, a crisis plan. All patients were offered a maximum treatment duration of 3 years. The first year patients received weekly sessions of individual MBT, 12 sessions in an MBT psychoeducational group, and once weekly (1.5 hr) MBT dynamic group. Over the second and third year, the frequency of individual therapy sessions was gradually reduced. In the course of the second year, the majority received individual therapy sessions every second week. During the final year, frequencies of individual therapy sessions were reduced to every third week. Weekly MBT group sessions continued throughout treatment. Decisions of treatment termination before 3 years were based on clinical judgement in dialogue with the patient. Pharmacotherapy was monitored by a psychiatrist.
Therapist MBT training and supervision
The therapists of the former psychodynamic treatment programme and new therapists (two psychologists, one residential doctor) were trained for MBT through specialized courses and seminars arranged regularly throughout the study period. Therapists also met for weekly video-based supervision of individual and group therapies conducted in groups with approximately eight members. All supervisors were associated with the unit and were experienced clinicians with MBT training.
Therapist adherence to MBT
To measure MBT adherence and competence, the MBT-ACS was developed and tested for the individual psychotherapy component (Karterud et al., 2013). The results proved high reliability (intraclass correlation [ICC] 2.1) by seven raters on adherence (0.84) and competence (0.88). On a 1–7 scale, ‘good enough’ adherence and competence is defined as level 4. During 2013, 19 individual sessions conducted by eight therapists in the programme were rated by five raters. Mean adherence level was 4.7 (SD 1.2) and mean competence-level 4.4 (SD 1.2). The therapists received feedback on their scores.
The psychodynamic treatment programme
The initial day hospital treatment phase lasted 18 weeks and consisted of a combination of group psychotherapies in an 11-hr weekly treatment programme (small group psychotherapy, art group therapy, large group psychotherapy, problem-solving, and cognitive behavioural group therapy; Karterud & Urnes, 2004). After completing day hospital treatment, patients were offered long-term outpatient group psychotherapy with weekly 1.5-hr sessions, according to modified group analytic principles. Maximum treatment duration was 4 years. Psychotherapy groups (day hospital and outpatient) were conducted by experienced, highly qualified staff (three psychiatric nurses, two psychiatrists, one residential doctor, one art therapist, one physiotherapist, one social worker, and one psychologist). The majority were qualified group analysts (5 years training) with a mean age (year 2004) of 48 (SD 9) years, 80% females. Pharmacotherapy was monitored by a psychiatrist.
Diagnostic status at the start of treatment (baseline)
Clinical staff performed standardized, semi-structured diagnostic interviews, the Mini International Neuropsychiatric Interview version 4.4 for DSM Axis-I diagnosis (Sheehan et al., 1994), and the Structured Clinical Interview for DSM Disorders (SCID-II) for DSM Axis-II diagnoses (First, 1994) at baseline. From 1993 to 1995, guidelines from the DSM-III-R (Frances, 1994) were followed, while the DSM-IV was implemented from 1996. Table 1 demonstrates baseline diagnoses.
Table 1.
Baseline diagnostic status
| Psychodynamic programme (n = 281) | MBT (n = 64) | |
|---|---|---|
| M (SD) | M (SD) | |
| Number of BPD criteria | 6.1 (1.1) | 6.2 (1.3) |
| Number of PD criteria | 17 (6) | 15 (7)* |
| Number of PDs | 1.7 (0.8) | 1.6 (0.8) |
| Number of symptom disorders | 2.6 (1.3) | 2.7 (1.5) |
| Comorbid disorders | % | % |
| Schizotypal | 3 | 0 |
| Paranoid | 9 | 19* |
| Antisocial | 4 | 2 |
| Narcissistic | 4 | 5 |
| Histrionic | 3 | 0 |
| Avoidant | 24 | 17 |
| Obsessive–compulsive | 6 | 8 |
| Dependent | 13 | 5 |
| PTSD | 5 | 11 |
| Somatoform | 10 | 6 |
| Eating | 24 | 19 |
| Mood | 73 | 81 |
| Anxiety | 67 | 69 |
| Substance use | 30 | 22 |
| No symptom disorder | 3 | 5 |
Note. The table demonstrates the full evaluation of diagnoses for patients when admitted to treatment (MBT or the former psychodynamic treatment programme). All patients had the diagnoses of borderline (B) personality disorder (PD).
MBT = mentalization-based treatment; BPD = borderline personality disorder; M = mean; SD = standard deviation.
Statistically significant differences between treatment groups (p < .05).
Diagnostic skills and reliability
SCID-II interviews were performed by experienced clinical staff with 10–20 years practice; all trained through SCID-II courses and regular quality assurance procedures at the unit. Twenty-four SCID-II interviews performed by staff members were videotaped (during 2004–2006) and rated by an independent rater for reliability testing of personality disorder diagnoses. The kappa value for BPD was 0.66.
Outcome measures
1. The duration of treatment
We report treatment duration as a variable of outcome, defined as the number of months in treatment and treatment drop-out as less than 3 months in treatment.
2. The Brief Symptom Inventory 18
The Brief Symptom Inventory (BSI-18; Derogatis, 2000) is a self-report questionnaire where the intensity of symptoms (depression, somatization and anxiety) is rated on a 0–4 scale (score 0: ‘not at all’, score 4: ‘extremely’). BSI-18 includes an overall severity index, the mean sum-score (BSI). The BSI-18 is adapted from the 53-item BSI (Derogatis, 1993), itself a shortened form of the 90-item Symptom Checklist-90-Revised (SCL-90-R; Derogatis, 1977). The BSI-18 applies the same clinical case-rule originally developed for the SCL-90-R. For the latter, original, instrument a cut-off for clinical/non-clinical ranges of severity (sum-score, the global severity index [GSI] 0.8) has been reckoned on the basis of Norwegian sample norms and patient samples (Pedersen & Karterud, 2004). In this study, we therefore refer to a clinical/non-clinical cut-off score of BSI = 0.8. The BSI-18 was administered to all patients in MBT. BSI-scores were calculated from SCL-90-R for patients in the psychodynamic treatment.
3. Interpersonal problems
The Circumplex of Interpersonal Problems (CIP; Pedersen, 2002) is a short version (48 items) of the Inventory of Interpersonal Problems-Circumplex version (IIP-C) self-report questionnaire (Alden, Wiggins, & Pincus, 1990). Severity is rated on a 0–4 scale (score 0: ‘not at all’, score 4: ‘extremely’). The mean sum-score (CIP) correlates r = .99 with the original IIP-C sum-score (Pedersen, 2002). The reported validity of CIP is high (4-day test–retest coefficient [ICC, 2.1], r = .96, 95% CI; .93–.98; Pedersen, Hagtvet, & Karterud, 2011). In a non-clinical Norwegian sample mean CIP-scores were 0.5 (SD 0.3; Pedersen, 2001). Thus, including one standard deviation, we in this study operate with a clinical/non-clinical CIP cut-off score of 0.8. The nine subscales of CIP are dominating, self-centred, cold, socially inhibited, non-assertive, overly accommodating, self-sacrificing, intrusive and mistrust.
4. Global functioning
Global functioning was evaluated at all assessment times. The observer-rated global assessment of functioning (GAF) provides a composite score of psychosocial functioning on a 0–100 scale (Axis V, Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition [DSM-IV], American Psychiatric Association; Pedersen & Karterud, 2011). Higher GAF scores indicate better psychosocial functioning. A level of 60 is often used as a cut-off level between mild/no impairment and moderate/severe impairment.
Throughout the investigation period, GAF scores were rated by therapists at the treatment unit. All received courses on GAF assessment (arranged by the Norwegian Network of Personality-focused Treatment Programs), supplemented with an Internet-based interactive GAF training course, developed by Karterud and Pedersen (http://www.personlighetsprosjekt.com/gaf/) and sponsored by the Norwegian Health Authorities. In 1998, the reliability of GAF assessments, based on clinical vignettes scored by staff consensus in 8 day units (including the studied treatment unit), was high (ICC 2.1, single measure, absolute agreement definition was 0.94, 95% CI .85–.98). In 2001, 58 staff members from the same units independently assessed GAF from clinical vignettes and high consistency of GAF scores across units and raters was demonstrated with estimated generalizability coefficients of absolute decision (the score) ranging from .86 to .95 (Pedersen, Hagtvet, & Karterud, 2007).
Repeated outcome assessments
Outcome measures 2, 3, and 4 were repeatedly assessed during the study period. Patients in the former psychodynamic treatment had a mean number of 3.4 assessments (SD, 0.8, median 3, range 1–5) over maximum 6 years, 91% were assessed at least three times, and 10% had the maximum of five assessments. MBT patients had a mean number of 3.6 assessments (SD 1.5, median 3, range 1–7) over maximum 4 years, 74% had at least three assessments, and 27% had five or more.
5–9. Sociodemographic questionnaire
Based on a self-report questionnaire administered within the Network at the start and end of treatment, patients and therapists reported: (5) incidents of self-harming and suicide attempts previous year, (6) hospital admissions previous year, (7) use and type of medication previous year, (8) number of months in work or study previous year and present employment/disability status and (9) present close relationship. At the start of treatment, patients were also asked about previous treatments and their age the first time.
Statistical procedures
Mixed models (Singer & Willett, 2003) were used for statistical analysis of longitudinal data (Mixed Models, SPSS, version 19). Time, months from baseline (0 years) up to 6 years, was modelled as a continuous variable. The time-points of each individual's outcome scores (GAF, BSI, CIP, and all CIP subscales) were approximated within the periods 1–3 months, 4–6 months, 7–12 months, and the following 6-month periods. Linear trajectories captured significant longitudinal trends in the data for all three outcome measures (GAF, GSI, and CIP: p < .001). The log likelihood estimations of model fit indicated significant improvements from an unconditional model to a linear random coefficients model (critical values for chi-square statistic: p < .01). Calculated effect sizes (Cohen's d) were based on mixed model predicted values.
The influence of a predictor is judged by the associated deviation of the trajectory of the outcome variable, the change in estimated residual variation, and log likelihood statistics, reductions of both indicating better model fit. Treatment (MBT/former psychodynamic programme) was the main predictor. All predictor analyses were based on models controlling for baseline variation.
Chi-square tests were used for statistical comparison of categorical variables at baseline and end of treatment. Data on work/study functioning were not normally distributed, and the non-parametric test, Related-Samples Sign Test was used to compare differences from baseline to end of treatment.
Patient consent
All patients gave written consent allowing research on anonymous data. This procedure was approved by the Norwegian Data Inspectorate and The Regional Committee for Medical Research Ethics.
Results
Treatment duration and drop-out
Patients in the former psychodynamic treatment had a significantly higher early drop-out rate and shorter average treatment duration than patients in MBT (p < .05, Table 2). MBT had not only remarkably low early drop-out rates (2%), but also considerably fewer patients with less than 6 months of treatment (MBT 5% vs. former treatment 42%, p < .05).
Table 2.
Treatment duration
| Psychodynamic programme (n = 281), % | MBT (n = 64), % | |
|---|---|---|
| Duration <3 months (drop-out) | 15 | 2 |
| Duration 3–5 months | 27 | 3 |
| Duration 6–17 months | 20 | 37 |
| Duration 18–29 months | 15 | 27 |
| Duration >30 months | 22 | 32 |
| M (SD) | M (SD) | |
| Months in treatment | 17 (19) | 23 (12) |
Note. The table demonstrates significant differences (p < .01) in treatment duration for patients in MBT and in the former psychodynamic treatment programme.
MBT = mentalization-based treatment; M = mean; SD = standard deviation.
Symptom distress
The severity of distress (BSI) reported at the start of treatment was substantial in both groups, and symptom levels were comparable (no significant difference, p > .05). Long-term improvements of BSI were significantly better for patients in MBT than patients in the psychodynamic treatment (p < .001), and 3-year effect sizes were large (Table 3). The trajectories of BSI-change are demonstrated in Figure1. From baseline to the end of treatment observed BSI-scores for MBT patients changed from mean 2.0 (SD 0.8) to 0.8 (SD 0.8), the latter score indicating no clinically significant distress. Corresponding mean BSI-scores for patients in the psychodynamic programme changed more moderately from 2.1 (SD 0.8) to 1.4 (SD 0.9) at the end of treatment.
Table 3.
Longitudinal outcomes: Psychodynamic programme versus MBT
| Linear mixed model estimates | |||
|---|---|---|---|
| Baseline (0 months) | Monthly change-rate | Three-year effect size | |
| M (SE) | M (SE) | ||
| Symptom distress: BSI | |||
| Psychodynamic program | 1.9 (0.04) | −0.01 (0.002) | 0.88 |
| MBT | 2.1 (0.1) | −0.03 (0.005) | 1.79 |
| Difference (psychodynamic program – MBT) | ns | 0.015 (0.004)** | |
| Interpersonal problems: CIP | |||
| Psychodynamic program | 1.8 (0.03) | −0.01 (0.001) | 0.91 |
| MBT | 1.7 (0.08) | −0.02 (0.002) | 1.41 |
| Difference (psychodynamic program – MBT) | ns | 0.07 (0.003)** | |
| CIP subscale: Mistrust | |||
| Psychodynamic program | 2.42 (0.06) | −0.016 (0.002) | 0.67 |
| MBT | 2.55 (0.15) | −0.03 (0.006) | 1.46 |
| Difference (psychodynamic program – MBT) | ns | 0.01 (0.004)* | |
| Psychosocial functioning: GAF | |||
| Psychodynamic program | 46 (0.3) | 0.24 (0.02) | 2.97 |
| MBT | 48 (0.7) | 0.49 (0.09) | 4.60 |
| Difference (psychodynamic program – MBT) | ns | −0.21 (0.05)** | |
Note.The table demonstrates mixed model estimations of longitudinal (linear) change and corresponding estimated effect sizes for patients in MBT and in the former psychodynamic treatment program.
MBT = mentalization-based treatment; M = mean; SE = standard error; BSI = Brief Symptom Inventory; CIP = Circumplex of Interpersonal Problems; GAF = global assessment of functioning.
** and *indicates statistically significant at p < .01 and p < .05, respectively. Not significant differences (p > .05) are indicated by ns.
Figure 1.
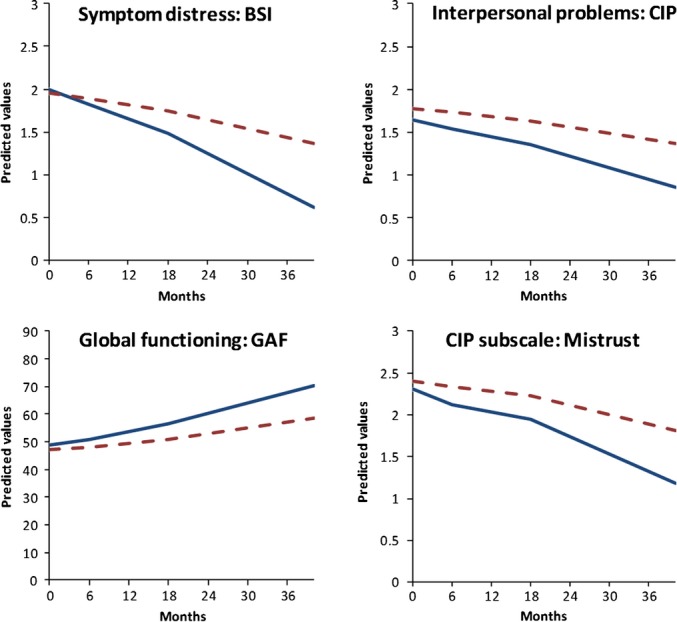
The figure demonstrates longitudinal trajectories of change based on linear mixed models statistical estimations of symptom distress, interpersonal problems, and global functioning with significant differences (p < .05) for patients in mentalization-based treatment (solid line) and the former psychodynamic treatment (dashed line).
Interpersonal functioning
At baseline, patients reported comparable (p > .05) and severe problems of interpersonal functioning (CIP). The overall decline in CIP-severity was significantly greater for patients in MBT (p < .001), and effect sizes were large (Table 3, Figure1). From the start to end of treatment, mean observed CIP-scores for MBT patients changed from 1.7 (SD 0.6) to 0.9 (SD 0.7), the latter indicating only mild interpersonal problems. Correspondingly, in the psychodynamic programme observed mean CIP scores changed more moderately from 1.8 (SD 0.5) to 1.4 (SD 0.7). Among specific CIP subscales, the subscale mistrust was initially rated the most problematic of all among patients in both groups (baseline mean score 2.6, SD 1.1, group difference: p > .05). This specific subscale improved significantly more for patients in MBT (Table 3, Figure1). Improvement-rates for the CIP subscales intrusive, dominating, and self-centred were also significantly higher for patients in MBT (p < .05). Over time the subscale non-assertive improved the least, and differences between treatment groups were insignificant (p > .05).
Global assessment of functioning
Patient's baseline levels of global functioning (GAF) indicated extensive psychosocial problems, and differences between treatment groups were insignificant (p > .05). GAF improvements over time were greater for MBT patients (p < .001), and effect sizes were large (Table 3, Figure1). From the start to end of treatment, the observed GAF-scores for MBT patients changed from mean 48 (SD 6) to mean 63 (SD 12), the latter score above the clinical/non-clinical cut-off level, indicating mild impairments of psychosocial functioning. For patients in the psychodynamic programme, the observed mean GAF-level changed from 46 (SD 5) to 56 (SD 10) at the end of treatment.
Self-harming and suicide attempts
Frequencies of self-harming behaviour and suicide attempts decreased in both groups during treatment, and differences between the treatment groups were insignificant (p > .05). In MBT, baseline frequencies of self-harming were higher than in the psychodynamic programme (p < .05) and dropped from 89% to 27%. For patients in the psychodynamic programme reports of self-harming decreased from 47% to 12%. Frequencies of suicide attempts previous year decreased from 35% to 6% in MBT and from 25% to 4% in the psychodynamic programme (group differences p > .05).
Previous use of mental health services and hospital admissions
Patients in both groups had previous treatment experience before being referred to the department. MBT patients were on average younger (p < .05) at baseline, but had nevertheless greater treatment experience. Experience included several psychiatric outpatient treatments (MBT: mean number 8, SD 17, median 3, Psychodynamic programme: mean number 1, SD 0.5, median 1) and started in adolescence/young adulthood (MBT: mean age first treatment 16 years, SD 7, Psychodynamic programme: mean age first treatment 20 years, SD 9). Baseline reports of previous psychiatric hospital admissions were more frequent in the former treatment (MBT: 38%, Psychodynamic programme: 53%, p < .05). During the last year of treatment, patients in both groups reported considerably fewer hospital admissions than before treatment (MBT: 6%, Psychodynamic programme: 9%, p > .05).
Medication
Antidepressants were the most frequently used medication at baseline (MBT: 46%, Psychodynamic programme: 44%, p > .05). During the course of treatment, their use was approximately halved. Among patients originally on antidepressants, 44% in the psychodynamic programme and 54% in MBT no longer used this medication at the end of treatment (group difference: p > .05). Neuroleptics were more frequent at baseline among patients in the psychodynamic programme (MBT: 8%, Psychodynamic programme: 22%, p < .05), but at the end of treatment use of neuroleptics was quite infrequent in both groups (MBT: 8%, Psychodynamic programme: 13%, p > .05). Use of anxiolytics and mood stabilizers was infrequent at both baseline and the end of treatment in both groups (group differences at the end of treatment: p > .05).
Work functioning
Occupational problems were considerable at baseline with 46% in the psychodynamic programme and 56% in MBT reporting unemployment or work disability of at least 50% (group difference p > .05). During treatment, unemployment frequencies were reduced in both groups. At baseline a higher proportion of patients in psychodynamic treatment reported unemployment (31% vs. 16% in MBT, p < .05), but by the end of treatment, a status of unemployment was infrequent in both groups (8% and 2%, p > .05). From the start to the end of treatment the reported number of months in work/study (previous year) increased moderately. In the psychodynamic programme the mean number of months in work/study was at baseline 4.5 (SD 4, median 4) and at the end of treatment 5.9 (SD 5, median 6). Patients in MBT had a significantly greater increase (p < .05) from baseline mean 4.8 (SD 4, median 4) to mean 7.1 (SD 5, median 8) at the end of treatment.
Close relationships
The frequency of patients living alone decreased during treatment in both groups, and the percentage of patients married/cohabiting correspondingly, increased (MBT: start: 30% – end: 45%, Psychodynamic programme: start: 22% – end: 44%, group difference p > .05).
Discussion
Main findings
(1) BPD patients who received MBT as implemented in Oslo, Norway, had a remarkably low rate of drop-out and achieved clinically relevant reductions in symptom distress, self-harming/suicidal incidents, psychiatric hospital admissions, and improvements of psychosocial, occupational, and interpersonal functioning. Effect sizes were large. (2) Clinical benefits associated with MBT were greater than the benefits of the former psychodynamic treatment programme, although important and considerable reductions in self-harm/suicidal incidents and hospital admissions were evident in both treatments.
Drop-out rates were lower in MBT
Low treatment adherence and early drop-out are known to be major obstacles to treatment of BPD, contributing to the typical treatment histories often seen – multiple outpatient treatments, frequent emergency service use, hospital admissions, high consumption of all kinds of health services, polypharmacy, and not least, negative treatment experiences (Horz, Zanarini, Frankenburg, Reich, & Fitzmaurice, 2010; Zanarini, Frankenburg, Khera, & Bleichmar, 2001). Poor long-term outcomes of BPD have been associated with treatment drop-out, and on the other hand, good long-term outcomes with high adherence to psychotherapy (Kvarstein & Karterud, 2013; Perry, Banon, & Ianni, 1999). The initial establishment of a treatment alliance is therefore crucial. In this study, the treatment adherence of the 64 BPD patients who received MBT was remarkably high and clearly contrasted the comparison treatment. The low drop-out rates also contrast other previous treatment studies. In a meta-analysis including 41 studies of BPD psychotherapy the average reported drop-out rate was 29% (Barnicot, Katsakou, Marougka, & Priebe, 2011).
The high treatment adherence among MBT patients in our study is in line with other MBT studies, all presenting drop-out rates far below previous reports. In Bateman and Fonagy (2009) study of outpatient MBT, the authors report that six of the 71 patients in the MBT group (8%) had less than 6 months treatment duration, while Bales et al. (2012) report no drop-out at all before 11 months. Jorgensen et al. (2012) on the other hand report that eight BPD patients of 56 in the MBT group (14%) terminated treatment at an early stage. The low drop-out rates indicated by these results is a considerable asset of MBT.
Mentalization-based treatment is advocated to be specifically tailored for patients with BPD, and has several features which are likely to contribute to enhance early motivation for therapy. We would suggest that the specific, dynamic, and mutually understood case formulation, the initial psychoeducational component focusing explicitly on central BPD problems and especially on mentalization (Liotti & Gilbert, 2011), and the combination of individual and group therapy, may all be important factors. However, at present no studies have investigated the importance of the specific ingredients of an MBT programme.
The higher rate of drop-out in the former psychodynamic programme may partly be due to its step-down format. As previously described, it is characterized by a transition from an initial phase of day-hospital treatment to long-term outpatient group psychotherapy. The format was originally designed for the treatment of poorly functioning patients with personality disorder, based on the idea that the intensive day hospital programme would provide initial containment, support, and initiate a treatment alliance, while the protracted outpatient group psychotherapy would facilitate further personality development. However, despite observed benefits of the day-hospital phase (Karterud et al., 2003; Wilberg et al., 1999), additional effects of the outpatient treatment were less than expected (Wilberg et al., 2003). Moreover, a qualitative study of drop-out patients with BPD identified the transition to outpatient group psychotherapy as a major disturbance of the treatment process (Hummelen, Wilberg, & Karterud, 2007). It is likely that BPD patients with poor reflective functioning would be especially vulnerable to an interruption of therapeutic alliances and attachment processes.
Better clinical outcomes in MBT
Patients in this study reported severe symptom distress, interpersonal problems, and frequent incidents of self-harming at the time of admission. Their severity of condition corresponded to baseline symptom levels and functioning reported in the Danish study (Jorgensen et al., 2012), and was slightly less severe than patients in the other two outpatient MBT studies (Bales et al., 2012; Bateman & Fonagy, 2009). At the end of treatment, the MBT patients in our study were considerably improved on measures of symptom distress, interpersonal and global functioning, and use of emergency health services. Our study clearly indicates that the clinical effects of MBT were greater than the comparison psychodynamic programme and held a high standard also when compared to other mentioned MBT reports.
Borderline personality disorder patients in the comparison group reported improvements, but benefits were poorer, and symptoms and functioning were still within a clinical range. A recent study concluded that outcomes of step-down treatment were mixed, best for patients with fairly good capacity for mentalization, while low treatment response was associated with poor mentalizing capacity (Gullestad, Johansen, Hoglend, Karterud, & Wilberg, 2013). It thus seems that the idea of treating poorly functioning BPD patients in step-down treatment programs should be reconsidered.
Effective emergency and suicide prevention evident in both treatments
In both the specialized treatments of this study, we demonstrate considerable reductions in self-destructive crises and hospitalizations, and in both treatments frequencies were reduced to low levels. These results are comparable to other MBT studies and to studies of other specialized BPD treatments (McMain et al., 2009; Pasieczny & Connor, 2011). Moreover, the results are considerably better than the reported treatment utilization in a longitudinal follow-up study of BPD patients in non-specific treatments (Zanarini, Frankenburg, Hennen, & Silk, 2004). Such emergency prevention is an important benefit and in itself a quality indicator of treatment.
Occupational functioning improved more in MBT
Although we report superior improvements of occupational functioning for patients in MBT, we must emphasize that the presence of occupational problems at the end of treatment was notable in both groups. In a large longitudinal study, Zanarini et al. also report that stable occupational activity seems hard to attain for BPD patients despite other clinical improvements (Zanarini, Frankenburg, Reich, & Fitzmaurice, 2010; Zanarini, Jacoby, Frankenburg, Reich, & Fitzmaurice, 2009). Several other studies have more generally highlighted the problem of gaining adequate psychosocial functioning for patients with BPD (Bateman & Fonagy, 2001; Gunderson et al., 2011). Despite the obvious and important challenges, few studies have specifically focused on occupational rehabilitation for patients with BPD. This is an important future research issue. Interestingly, a recent study reports that even small improvements of mentalizing after attending a psychoeducational programme were associated with observable occupational improvements (Bly, Wright, & Tuber, 2012).
Strengths and limitations
This study is the first to include ratings of therapist adherence to MBT (Karterud et al., 2013). Their scores indicated that the psychotherapeutic work performed by the therapists fulfilled good enough standards for MBT with respect to the individual psychotherapy. It is a considerable strength that we can report that therapists in the investigated MBT-team followed the specified model of treatment to an acceptable extent and with acceptable quality.
The study does not have randomized, controlled conditions and conclusions are thus limited. Nevertheless, the study presents a retrospective, naturalistic comparison of two clinically representative and highly specialized, sophisticated treatments conducted within the same unit, but during different time periods. Patients were recruited from the same geographical area, and we document that they represented comparable cohorts with respect to sociodemography and personality pathology.
The sample size of the MBT group in our study is equivalent to other previously published MBT studies. It further strengthens our results that we present a comparison group which is larger and received more competent treatment than in any previous MBT trial.
This study has a longitudinal design with repeated measurements over a long span of time. We use recommended, advanced, statistical methods able to incorporate unbalanced data (Singer & Willett, 2003). This is a considerable asset as it minimizes loss of patient data due to incomplete series. The validity of the chosen linear change model is confirmed by the high correlations (r) between model-based predicted values and observed values (GSI: r = .85, CIP: r = .86, GAF: r = .89).
Differences between patients' number of assessments is a possible bias. For all dependent variables we investigated the deviance of linear change associated with different assessment numbers using mixed model statistics (Hedeker & Gibbons, 1997). We found no significant linear deviation (p > .05). All significant results were also cross-checked in linear change models including only patients with at least three assessments. We conclude that the bias of missing assessments is likely to be small.
The MBT programme recruited younger patients compared to the psychodynamic programme, and it has been suggested that younger BPD patients are more susceptible to change (Johnson et al., 2000). We therefore cross-checked all significant longitudinal analyses in models controlling for age. We conclude that younger age in MBT did not significantly bias results.
Conclusions
1. MBT as implemented in Oslo, Norway, is an effective treatment for patients with BPD. 2. In treatment of BPD, MBT is associated with greater clinical benefits than a psychodynamic treatment programme.
References
- Alden LE, Wiggins JS. Pincus AL. Construction of circumplex scales for the Inventory of Interpersonal Problems. Journal of Personality Assessment. 1990;55:521–536. doi: 10.1080/00223891.1990.9674088. [DOI] [PubMed] [Google Scholar]
- Bales D, van Beek N, Smits M, Willemsen S, Busschbach JJ, Verheul R. Andrea H. Treatment outcome of 18-month, day hospital mentalization-based treatment (MBT) in patients with severe borderline personality disorder in the Netherlands. Journal of Personality Disorders. 2012;26:568–582. doi: 10.1521/pedi.2012.26.4.568. doi: 10.1521/pedi.2012.26.4.568. [DOI] [PubMed] [Google Scholar]
- Barnicot K, Katsakou C, Marougka S. Priebe S. Treatment completion in psychotherapy for borderline personality disorder: A systematic review and meta-analysis. Acta Psychiatrica Scandinavica. 2011;123:327–338. doi: 10.1111/j.1600-0447.2010.01652.x. doi: 10.1111/j.1600-0447.2010.01652.x. [DOI] [PubMed] [Google Scholar]
- Bateman A. Fonagy P. Treatment of borderline personality disorder with psychoanalytically oriented partial hospitalization: An 18-month follow-up. American Journal of Psychiatry. 2001;158:36–42. doi: 10.1176/appi.ajp.158.1.36. [DOI] [PubMed] [Google Scholar]
- Bateman A. Fonagy P. Mentalization based treatment for borderline personality disorder. A practical guide. Oxford, UK: Oxford University Press; 2006. [Google Scholar]
- Bateman A. Fonagy P. 8-year follow-up of patients treated for borderline personality disorder: Mentalization-based treatment versus treatment as usual. American Journal of Psychiatry. 2008;165:631–638. doi: 10.1176/appi.ajp.2007.07040636. doi: 10.1176/appi.ajp.2007.07040636. [DOI] [PubMed] [Google Scholar]
- Bateman A. Fonagy P. Randomized controlled trial of outpatient mentalization-based treatment versus structured clinical management for borderline personality disorder. American Journal of Psychiatry. 2009;166:1355–1364. doi: 10.1176/appi.ajp.2009.09040539. [DOI] [PubMed] [Google Scholar]
- Bly EM, Wright AJ. Tuber SB. Unemployed and poor in New York: The impact of mentalization and Axis II psychopathology on job outcome. Bulletin of the Menninger Clinic. 2012;76:101–129. doi: 10.1521/bumc.2012.76.2.101. doi: 10.1521/bumc.2012.76.2.101. [DOI] [PubMed] [Google Scholar]
- Derogatis LR. The SCL-90-R: Administration, scoring and procedures manual. Baltimore, MD: Clinical Psychometric Research Unit, John Hopkins University School of Medicine; 1977. [Google Scholar]
- Derogatis LR. The Brief Symptom Inventory (BSI): Administration, scoring, and procedures manual. Minneapolis, MN: National Computer Services; 1993. [Google Scholar]
- Derogatis LR. The Brief-Symptom-Inventory-18 (BSI-18): Administration, scoring, and procedures manual. Minneapolis, MN: National Computer Services; 2000. [Google Scholar]
- First M. Structured Clinical Interview for DSM-IV (version 2.0) New York, NY: New York State Psychiatric Institute; 1994. [Google Scholar]
- Frances A. Diagnostic and statistical manual of mental disorders (DSM IV) 4th ed. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- Gullestad FS, Johansen MS, Hoglend P, Karterud S. Wilberg T. Mentalization as a moderator of treatment effects: Findings from a randomized clinical trial for personality disorders. Psychotherapy Research: Journal of the Society for Psychotherapy Research. 2013;23:674–689. doi: 10.1080/10503307.2012.684103. doi: 10.1080/10503307.2012.684103. [DOI] [PubMed] [Google Scholar]
- Gullestad FS, Wilberg T, Klungsoyr O, Johansen MS, Urnes O. Karterud S. Is treatment in a day hospital step-down program superior to outpatient individual psychotherapy for patients with personality disorders? 36 months follow-up of a randomized clinical trial comparing different treatment modalities. Psychotherapy Research: Journal of the Society for Psychotherapy Research. 2012;22:426–441. doi: 10.1080/10503307.2012.662608. doi: 10.1080/10503307.2012.662608. [DOI] [PubMed] [Google Scholar]
- Gunderson JG, Stout RL, McGlashan TH, Shea MT, Morey LC, Grilo CM. Skodol AE. Ten-year course of borderline personality disorder: Psychopathology and function from the Collaborative Longitudinal Personality Disorders study. Archives of General Psychiatry. 2011;68:827–837. doi: 10.1001/archgenpsychiatry.2011.37. doi: 10.1001/archgenpsychiatry.2011.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hedeker D. Gibbons RD. Application of random-effects pattern-mixture models for missing data in longitudinal studies. Psychological Methods. 1997;2:64–78. [Google Scholar]
- Horz S, Zanarini MC, Frankenburg FR, Reich DB. Fitzmaurice G. Ten-year use of mental health services by patients with borderline personality disorder and with other axis II disorders. Psychiatric Services (Washington, D.C.) 2010;61:612–616. doi: 10.1176/appi.ps.61.6.612. doi: 10.1176/appi.ps.61.6.612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hummelen B, Wilberg T. Karterud S. Interviews of female patients with borderline personality disorder who dropped out of group psychotherapy. International Journal of Group Psychotherapy. 2007;57:67–91. doi: 10.1521/ijgp.2007.57.1.67. [DOI] [PubMed] [Google Scholar]
- Johnson JG, Cohen P, Kasen S, Skodol AE, Hamagami F. Brook JS. Age-related change in personality disorder trait levels between early adolescence and adulthood: A community-based longitudinal investigation. Acta Psychiatrica Scandinavica. 2000;102:265–275. doi: 10.1034/j.1600-0447.2000.102004265.x. [DOI] [PubMed] [Google Scholar]
- Jorgensen CR, Freund C, Boye R, Jordet H, Andersen D. Kjolbye M. Outcome of mentalization-based and supportive psychotherapy in patients with borderline personality disorder: A randomized trial. Acta Psychiatrica Scandinavica. 2012;127:305–317. doi: 10.1111/j.1600-0447.2012.01923.x. doi: 10.1111/j.1600-0447.2012.01923.x. [DOI] [PubMed] [Google Scholar]
- Karterud S. Manual for mentaliseringsbasert gruppeterapi (MBT-G) Oslo, Norway: Gyldendal Akademisk; 2012. [Google Scholar]
- Karterud S. Bateman A. Manual for mentaliseringsbasert terapi (MBT) og MBT vurderingsskala. Versjon individualterapi. Oslo, Norway: Gyldendal Akademisk; 2010. [Google Scholar]
- Karterud S. Bateman A. Manual for mentaliseringsbasert psykoedukativ gruppeterapi (MBT-I) Oslo, Norway: Gyldendal Akademisk; 2011. [Google Scholar]
- Karterud S, Pedersen G, Bjordal E, Brabrand J, Friis S, Haaseth O. Urnes O. Day treatment of patients with personality disorders: Experiences from a Norwegian treatment research network. Journal of Personality Disorders. 2003;17:243–262. doi: 10.1521/pedi.17.3.243.22151. [DOI] [PubMed] [Google Scholar]
- Karterud S, Pedersen G, Engen M, Johansen MS, Johansson PN, Schluter C. Bateman AW. The MBT Adherence and Competence Scale (MBT-ACS): Development, structure and reliability. Psychotherapy Research: Journal of the Society for Psychotherapy Research. 2013;23:705–717. doi: 10.1080/10503307.2012.708795. doi: 10.1080/10503307.2012.708795. [DOI] [PubMed] [Google Scholar]
- Karterud S. Urnes O. Short-term day treatment programmes for patients with personality disorders. What is the optimal composition? Nordic Journal of Psychiatry. 2004;58:243–249. doi: 10.1080/08039480410006304. [DOI] [PubMed] [Google Scholar]
- Kvarstein EH, Arnevik E, Halsteinli V, Ro FG, Karterud S. Wilberg T. Health service costs and clinical gains of psychotherapy for personality disorders: A randomized controlled trial of day-hospital-based step-down treatment versus outpatient treatment at a specialist practice. BMC Psychiatry. 2013;13:315. doi: 10.1186/1471-244X-13-315. doi: 10.1186/1471-244X-13-315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kvarstein EH. Karterud S. Large variation of severity and longitudinal change of symptom distress among patients with personality disorders. Personality and Mental Health. 2013;7:265–276. doi: 10.1002/pmh.1226. doi: 10.1002/pmh.1226. [DOI] [PubMed] [Google Scholar]
- Kvarstein E, Karterud S. Pedersen G. Severely disturbed borderline patients need more than short-term day hospital treatment. Therapeutic Communities. 2004;25:120–130. [Google Scholar]
- Liotti G. Gilbert P. Mentalizing, motivation, and social mentalities: Theoretical considerations and implications for psychotherapy. Psychology and Psychotherapy. 2011;84:9–25. doi: 10.1348/147608310X520094. doi: 10.1348/147608310X520094. [DOI] [PubMed] [Google Scholar]
- McMain SF, Links PS, Gnam WH, Guimond T, Cardish RJ, Korman L. Streiner DL. A randomized trial of dialectical behavior therapy versus general psychiatric management for borderline personality disorder. American Journal of Psychiatry. 2009;166:1365–1374. doi: 10.1176/appi.ajp.2009.09010039. doi: 10.1176/appi.ajp.2009.09010039. [DOI] [PubMed] [Google Scholar]
- Pasieczny N. Connor J. The effectiveness of dialectical behaviour therapy in routine public mental health settings: An Australian controlled trial. Behaviour Research and Therapy. 2011;49:4–10. doi: 10.1016/j.brat.2010.09.006. doi: 10.1016/j.brat.2010.09.006. [DOI] [PubMed] [Google Scholar]
- Pedersen G. Assessment of self-reported symptoms and interpersonal problems: Psychometric considerations and validity of clinical use. London, UK: Warnborough University; 2001. [Google Scholar]
- Pedersen G. Revised Norwegian version of Inventory of Interpersonal Problems - Circumplex (IIP-C) Tidsskrift for Norsk Psykologforening. 2002;39:25–34. [Google Scholar]
- Pedersen G, Hagtvet KA. Karterud S. Generalizability studies of the Global Assessment of Functioning-Split version. Comprehensive Psychiatry. 2007;48:88–94. doi: 10.1016/j.comppsych.2006.03.008. [DOI] [PubMed] [Google Scholar]
- Pedersen G, Hagtvet KA. Karterud S. Interpersonal problems: Self-therapist agreement and therapist consensus. Journal of Clinical Psychology. 2011;67:308–317. doi: 10.1002/jclp.20762. doi: 10.1002/jclp.20762. [DOI] [PubMed] [Google Scholar]
- Pedersen G. Karterud S. Is SCL-90R helpful for the clinician in assessing DSM-IV symptom disorders? Acta Psychiatrica Scandinavica. 2004;110:215–224. doi: 10.1111/j.1600-0447.2004.00321.x. [DOI] [PubMed] [Google Scholar]
- Pedersen G. Karterud S. The symptom and function dimensions of the Global Assessment of Functioning (GAF) scale. Comprehensive Psychiatry. 2011;48:88–94. doi: 10.1016/j.comppsych.2011.04.007. [DOI] [PubMed] [Google Scholar]
- Perry JC, Banon E. Ianni F. Effectiveness of psychotherapy for personality disorders. American Journal of Psychiatry. 1999;156:1312–1321. doi: 10.1176/ajp.156.9.1312. [DOI] [PubMed] [Google Scholar]
- Rossouw TI. Fonagy P. Mentalization-based treatment for self-harm in adolescents: A randomized controlled trial. Journal of the American Academy of Child and Adolescent Psychiatry. 2012;51:1304–1313. doi: 10.1016/j.jaac.2012.09.018. [DOI] [PubMed] [Google Scholar]
- Sheehan DV, Lecrubier Y, Janavs J, Weiller E, Baker R. Hergueta P. Mini International Neuropsychiatric Interview (M.I.N.I.) Tampa, FL and Paris, France: University of South Florida Institute for Research in Psychiatry and INSERM-Hôpital de la Salpétrière; 1994. [Google Scholar]
- Simonsen S, Nørgaard NL, Larsen KA. Bjørnholm KI. Mentalization-inspired case formulation: Minding the difficult patient. Personality and Mental Health. 2011;5:73–79. [Google Scholar]
- Singer JD. Willett JB. Applied longitudinal data analysis. New York, NY: Oxford University Press; 2003. [Google Scholar]
- Wilberg T, Karterud S, Pedersen G, Urnes O, Irion T, Brabrand J. Stubbhaug B. Outpatient group psychotherapy following day treatment for patients with personality disorders. Journal of Personality Disorders. 2003;17:510–521. doi: 10.1521/pedi.17.6.510.25357. [DOI] [PubMed] [Google Scholar]
- Wilberg T, Karterud S, Urnes O, Pedersen G. Friis S. Outcomes of poorly functioning patients with personality disorders in a day treatment program. Psychiatric Services (Washington, D.C.) 1998;49:1462–1467. doi: 10.1176/ps.49.11.1462. [DOI] [PubMed] [Google Scholar]
- Wilberg T, Urnes O, Friis S, Irion T, Pedersen G. Karterud S. One-year follow-up of day treatment for poorly functioning patients with personality disorders. Psychiatric Services (Washington, D.C.) 1999;50:1326–1330. doi: 10.1176/ps.50.10.1326. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Frankenburg FR, Hennen J. Silk KR. Mental health service utilization by borderline personality disorder patients and Axis II comparison subjects followed prospectively for 6 years. Journal of Clinical Psychiatry. 2004;65:28–36. doi: 10.4088/jcp.v65n0105. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Frankenburg FR, Khera GS. Bleichmar J. Treatment histories of borderline inpatients. Comprehensive Psychiatry. 2001;42:144–150. doi: 10.1053/comp.2001.19749. [DOI] [PubMed] [Google Scholar]
- Zanarini MC, Frankenburg FR, Reich DB. Fitzmaurice G. The 10-year course of psychosocial functioning among patients with borderline personality disorder and axis II comparison subjects. Acta Psychiatrica Scandinavica. 2010;122:103–109. doi: 10.1111/j.1600-0447.2010.01543.x. doi: 10.1111/j.1600-0447.2010.01543.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zanarini MC, Jacoby RJ, Frankenburg FR, Reich DB. Fitzmaurice G. The 10-year course of social security disability income reported by patients with borderline personality disorder and axis II comparison subjects. Journal of Personality Disorders. 2009;23:346–356. doi: 10.1521/pedi.2009.23.4.346. doi: 10.1521/pedi.2009.23.4.346. [DOI] [PMC free article] [PubMed] [Google Scholar]


