Abstract
Access to healthy foods among secondary school students is patterned by individual-level socioeconomic status, but few studies have examined how school nutrition policies and practices are patterned by school-level characteristics. The objective of this study was to examine school nutrition policies and practices by school characteristics (location, racial/ethnic composition and free/reduced priced lunch eligibility [FRPL]) in Minnesota secondary schools between 2008 and 2012. Data from the 2008 to 2012 Minnesota School Health Profiles survey were used to assess school nutrition policies and practices, and National Center for Educational Statistics (NCES) data were used for school characteristics (n = 505 secondary schools). Nutrition policies and practices included: 1) the availability of low-nutrient, energy dense (LNED) items, 2) strategies to engage students in healthy eating, and 3) restrictions on advertisements of LNED products in areas around the school. Among school-level characteristics, school location was most strongly related to school nutrition policies. Across all years, city schools were less likely than town/rural schools to have vending machines/school stores [prevalence difference (PD)=13.7, 95% confidence interval (CI) -25.0,-2.3], and less likely to sell sports drinks (PD= -36.3, 95% CI: -51.8, -20.7). City schools were also more likely to prohibit advertisements for LNED products in school buildings (PD=17.7, 95% CI: 5.5, 29.9) and on school grounds (PD=15.6, 95% CI: 1.7, 29.5). Between 2008 and 2012 the prevalence of some healthy eating policies/practices (limiting salty snacks, offering taste testing, banning unhealthy food advertisements in school publications) declined in city schools only, where these policies/practices had previously been more common. Monitoring of these trends is needed to understand the impact of these policies on student outcomes across school settings.
Keywords: Nutritional policies, secondary schools, health disparities, adolescent obesity, rural health
INTRODUCTION
Rates of obesity for all U.S. adolescents have been rising for more than three decades1 and are disproportionately higher among some populations. Racial/ethnic minority youth are more likely to be overweight or obese compared to non-Hispanic white youth,1–5 and youth from low-income households are more like likely to be overweight or obese compared to those from higher income households.2–4,6 Disparities in obesity extend to geography as well, with children in rural areas more likely to be obese or overweight than urban children.7,8
Obesity also clusters according to school characteristics. Secondary schools with high minority enrollment or low mean parental education have students with disproportionately higher body mass index (BMI), and schools located in non-metropolitan areas have a high proportion of students who are obese.9 More research is needed to examine how youth obesity may be patterned by school characteristics,10 beyond family, peer and neighborhood influences.11,12
School nutrition and physical activity policies may contribute to patterns in adolescent obesity rates.9,13 Specific policy solutions for reducing obesity include regulating the food environment by restricting competitive food and fundraiser sales,14–16 using price incentives and other strategies to engage students in healthy eating,13,17,18 and eliminating advertisements for unhealthy products in schools.13,19 School policies related to the availability of healthy food are a plausible mechanism by which disparities in obesity and related health behaviors might arise. However, little is known about how policies and practices vary at the school level by geography, socioeconomic status, and racial and economic composition of students at the school.13
To fill this gap, this paper examined policies and practices that may improve the school food environment and promote healthy eating by school characteristics. Our aim was to explore differences in the prevalence of nutritional policies and practices in Minnesota secondary schools by racial/ethnic composition of the student body, free/reduced price lunch eligibility, and school location between 2008 and 2012.
METHODS
The study was part of the School Obesity-related Policy Evaluation (ScOPE) study, which aims to evaluate nutrition and physical activity policies and practices in Minnesota secondary schools; it was approved by the Institutional Review Board at the University of Minnesota. Data on school nutrition policies and practices were obtained from the 2008 to 2012 Minnesota School Health Profiles principal survey20 administered by the Minnesota Department of Education with funding and technical assistance from the Centers for Disease Control and Prevention. This survey is a random, biennial, self-administered assessment, mailed to school principals or designees. Between 2008 and 2012, the response rate for principals ranged from 70% to 84%.20 For this study, three policy and practice questions were assessed: 1) the availability of low-nutrient, energy-dense (LNED) snacks, 2) implementation of strategies to promote healthy eating at school, and 3) banning advertisements for LNED foods.21 Profiles questions were the same in all study years.
Availability of LNED foods
Principals were asked: “Can students purchase any snack foods or beverages from one or more vending machines at the school or at a school store, canteen, or snack bar?” If yes, they were asked whether students could purchase each of the following items: a) soda pop or fruit drinks that are not 100% juice; b) sports drinks (e.g., Gatorade); c) chocolate candy or other kinds of candy; and d) salty snacks that are not low in fat. Response options were “Yes/No.”
Strategies to engage students in healthy eating
Principals were asked: “During this school year, has your school done any of the following? a) Priced nutritious foods and beverages at a lower cost while increasing the price of less nutritious foods and beverages; b) Collected suggestions from students, families, and school staff on nutritious food preferences and strategies to promote healthy eating; c) Provided information to students or families on the nutrition and caloric content of foods available; d) Conducted taste tests to determine food preferences for nutritious items; and e) Provided opportunities for students to visit the cafeteria to learn about food safety, food preparation, or other nutrition-related topics.” Response options were “Yes/No.”
Banning advertisements for LNED foods
Principals were asked: “Does your school prohibit advertisements for candy, fast food restaurants, or soft drinks in the following locations? a) In the school building; b) On school grounds, including on the outside of the school building, on playing fields, or other areas of the campus; c) On school buses or other vehicles used to transport children; d) In school publications (e.g., newsletters, newspapers, web sites, or other school publications).” Response options were “Yes/No.”
National Center for Educational Statistics (NCES) Common Core Data 22 were used to characterize schools. High schools were defined as those with a low grade of 9 or higher and a high grade of 10 or higher. Junior/ senior high schools had a low grade of 8 or lower and a high grade of 10 or higher. Schools with no grade below 5th grade and no grade above 9th were classified as middle schools. Other school characteristics included the percent of minority (non-white and/or Hispanic) enrollment in three categories (<5%, 5-<50%, ≥50%), percent student free/reduced price lunch (FRPL) eligibility in three categories (<20%, 20-<60%, ≥60%), and school location in three categories (city, suburban, and town/rural). School location was determined using a combination of NCES and Rural-Urban Commuting Areas classification schemes.22,23 School-level data for 2012 are based on the 2011 NCES data.
The association between school characteristics and nutrition policies and practices were estimated across years (2008, 2010, 2012) between school locations (with town/rural as the reference group), FRPL eligibility categories (with <20% FRPL as the reference group), and minority enrollment categories (with <5% minority enrollment as the reference group) using generalized estimating equation models with a robust unstructured correlation structure, binomial distribution and logit link, adjusted policy prevalence differences (PD) and 95% confidence intervals (CI). All models included school level (middle, junior/senior high, high school) to account for the Profiles stratified sampling scheme. A Taylor series expansion was used to obtain the standard error (and 95% CI) for adjusted prevalences and adjusted PD from the logistic regression models. All models included location, FRPL eligibility, and minority enrollment, also adjusted for school level and year. Interactions were tested between year and school location, FRPL eligibility, and minority enrollment and estimated adjusted PD (95% CI) stratified by year where significant interactions were found. This modeling strategy allowed us to identify trends over time and differences by school characteristics across years. Analyses were conducted in Stata Statistical Software (version 12.1, 2011, StataCorp).
RESULTS AND DISCUSSION
School characteristics
Table 1 presents school characteristics from 2008 to 2012 for schools included in the analysis. The analysis included 505 unique schools (some schools were part of the sample in more than one year). The sample was equally divided between high schools, junior/senior high schools, and middle schools. In all years, at least two-thirds were rural or small town schools. Few schools (less than 10%) had more than half minority enrollment and all of these schools were located in a city. FRPL eligibility was more variable; in most of the schools, 20-60% of students were eligible. Online Supplemental Materials present the unadjusted prevalence of each school policy or practice from 2008 to 2012 according to each school characteristic, including the availability of LNED items (Online Supplement A), healthy eating strategies (Online Supplement B) and banned ads for LNED items (Online Supplement C).
Table 1.
Demographic Characteristics of Schools Participating in the Minnesota School Health Profiles Survey in 2008, 2010, and 2012
| 2008 N= 203 N (%) | 2010 N=226 N (%) | 2012a N = 275 N (%) | |
|---|---|---|---|
| Grade Levelb | |||
| Middle School | 68 (33.5%) | 82 (30.4%) | 95 (33.8%) |
| Junior/Senior High School | 68 (33.5%) | 98 (36.8%) | 101 (36.7%) |
| High School | 67 (33%) | 87 (32.7%) | 83 (30.2%) |
| School Locationc | |||
| City | 28 (13.8%) | 38 (14.3%) | 26 (9.5%) |
| Suburb | 39 (19.2%) | 49 (18.4%) | 47 (17.1%) |
| Town/Rural | 136 (67%) | 179 (67.3%) | 202 (73.5%) |
| Free/Reduced Price Lunch (FRPL) Eligibilityd | |||
| < 20% | 57 (28.1%) | 51 (19.2%) | 50 (18.2%) |
| 20- <60% | 130 (64%) | 195 (73.3%) | 207 (75.3%) |
| ≥ 60% | 16 (7.9%) | 20 (7.5%) | 18 (6.5%) |
| Minority Enrollmente | |||
| < 5% | 70 (34.5%) | 79 (29.7%) | 67 (24.4%) |
| 5- <50% | 113 (55.7%) | 167 (62.8%) | 191 (69.5%) |
| ≥ 50% | 20 (9.9%) | 20 (7.5%) | 17 (6.2%) |
Data for school location, minority enrollment and FRPL school level data from 2011
Middle School defined as having a low grade of ≥ 5 and a high grade of ≤ 9; Junior/ Senior High School defined as having a low grade of ≤ 8 and a high grade of ≥10; High School defined as having a low grade of ≥9 and a high grade of ≥10
Classified according to NCES and Rural-Urban Commuting Areas schemes
Percent of students eligible to receive free/reduced price lunch
Percent of non-white and/or Hispanic students enrolled at school
Average prevalence differences in policies by school characteristics
Differences in the adjusted prevalence of school policies and practices by school location and FRPL eligibility are presented in Table 2. Differences are averaged across all years (2008, 2010, and 2012) unless there was a statistically significant interaction between year and either school location or FRPL eligibility, in which case differences are presented in each year. Across all years, on average, city schools were less likely than town/rural schools to have vending machines or school stores (PD= -13.7, 95% CI: -25.0, -2.3), and less likely to sell sports drinks (PD= -36.3, 95% CI: -51.8, -20.7). City schools were also more likely to ban advertisements for LNED products in school buildings (PD=17.7, 95% CI: 5.5, 29.9) and on school grounds (PD=15.6, 95% CI: 1.7, 29.5).
Table 2.
Nutrition Policies and Practices by School Location, Free-Reduced Price Lunch (FRPL) Status: Average Adjusted Prevalence Differences (PD),a and 95% Confidence Intervals (CI) from 2008-2012
| City PD (95% CI) compared town/rural | Suburb PD (95% CI) compared to town/rural | High % FRPL PD (95% CI) compared to low % FRPL | Medium % FRPL PD (95% CI) compared to low % FRPL | |
|---|---|---|---|---|
| Availability of LNEDb items | ||||
| Vending machine/ school store | −13.7 (−25.0, −2.3) | −3.1 (−10.7, 4.4) | −10.0 (−26.3, 6.3) | −0.1 (−6.9, 6.6) |
| Soda available | −8.1 (−24.2, 8.0) | 12.3 (0.6, 24.0) | −2.4 (−30.9, 26.0) | 1.1 (−9.1, 11.4) |
| Sports drinks available | −36.3 (−51.8, −20.7) | −9.2 (−17.3, −0.9) | 3.7 (−15.6, 22.9) | −2.6 (−9.9, 4.6) |
| Candy available | −5.6 (−22.3, 11.0) | 0.3 (−12.6, 13.2) | −9.4 (−33.1, 14.3) | 9.1 (−19.7, 1.5) |
| Salty snacks available | −31.6c (−53.1, −10.0) | −17.1c (−35.7, 1.5) | 4.9 (−20.3, 30.0) | −6.1 (−16.8, 4.6) |
| −11.8d (−28.2, 4.6) | −8.3d (−20.6, 4.0) | |||
| Healthy eating strategies | 8.9e (−12.9, 30.7) | 0.7e (−15.8, 17.2) | ||
| Pricing incentives | 6.2 (−7.4, 19.7) | 3.2 (−6.3, 12.7) | 10.7c (−22.8, 44.1) | 1.9c (−9.4, 13.3) |
| −6.7d (−27.4, 13.9) | −8.5d (−16.7, −0.2) | |||
| −21.9e (−41.5, −2.3) | −19.5e (−32.7, −6.2) | |||
| Food preferences of students | 0.9 (−12.2, 14.0) | −3.7 (−14.9, 7.4) | −11.4 (−34.9, 12.1) | −7.6 (−17.1, 1.9) |
| Info on nutrition content | 6.9 (−6.6, 20.5) | 6.2 (−4.6, 16.9) | −17.4 (−40.1, 5.2) | −5.9 (−15.2, 3.3) |
| Taste testing | 23.5c (2.5, 44.4) | 0.3c (−14.3, 14.8) | −5.8 (−22.9, 11.3) | −0.1 (−8.5, 8.4) |
| 12.2d (−1.5, 25.9) | 9.7d (−1.1, 20.5) | |||
| 0.9e (−15.7, 17.5) | 21.1e (5.9, 36.3) | |||
| Learning opportunities in cafeteria | 5.0 (−6.9, 16.8) | −0.8 (−10.0, 8.5) | −13.2 (−27.2, 0.8) | −3.7 (−12.2, 4.7) |
| Banned ads for LNED items | ||||
| In building | 17.7 (5.5, 29.9) | 6.3 (−4.8, 17.4) | −12.0 (−33.3, 9.5) | −7.7 (−16.4, 1.0) |
| On grounds | 15.6 (1.7, 29.5) | 16.1 (5.6, 26.7) | −0.5 (−23.1, 22.1) | −6.9 (−16.4, 2.6) |
| On bus | 7.9 (−5.0, 20.8) | 9.3 (−0.4, 19.0) | −4.2 (−24.2, 15.8) | −5.6 (−14.6, 3.5) |
| In school publications | 22.7c (6.9, 38.6) | 13.6c (−2.3, 29.5) | −2.7 (−24.1, 18.7) | −6.3 (−15.0, 2.4) |
| 6.4d (−8.3, 21.1) | 5.9d (−4.8, 16.7) | |||
| −15.1e (−34.1, 4.0) | −2.5e (−17.8, 12.8) |
All models adjusted for location (city, suburb, town/rural), FRPL eligibility (the percent students eligible to receive free/reduced price lunch), minority enrollment (the percent of non-white and/or Hispanic students enrolled at school) and school grade level (middle school, junior/senior high school, or high school). Bolded PDs are statistically significant at alpha = 0.05
Low-nutrient, energy-dense
2008
2010
2012
Study findings suggest that there are a number of policies and practices in Minnesota city schools that support a healthier food environment for their students compared with schools in rural areas and towns. At least two other (cross-sectional) studies of secondary schools – one in Utah and one in a multistate sample of secondary schools – found that rural schools trailed behind city schools in a number of policies and practices to promote healthy eating.24,25 Rural schools may be particularly understaffed, overwhelmed by academic achievement tests, or lack wellness coordinators to implement policy.14 Although these challenges may not be unique to rural schools, they may contribute to the lack of prioritizing initiatives aimed at improving nutrition.
Across all years, suburban schools were more likely to sell soda than town/rural schools (PD=12.3, 95% CI: 0.6, 24.0). It could be that, in more affluent areas where fewer students participate in subsidized meal programs, competitive food sales provide revenue to cover operational costs of food services.26 However, suburban schools had other policies, including being less likely to sell sports drinks (PD= -9.2, 95% CI: -17.3, -0.9) and more likely to ban advertisements of LNED products on school grounds (PD=16.1, 95% CI: 5.6, 26.7) compared with rural schools.
Unlike previous studies, 24,25 the current study found, on average, no policy differences by FRPL eligibility or minority enrollment. In our sample of schools, it was difficult to separate the influence of race/ethnicity, socioeconomic status, and location in shaping policy environments, given that few Minnesota town or rural schools have a high minority enrollment, and few schools with high FRPL eligibility have low minority enrollment. Our results suggested that policy differences were more strongly associated with school location or socioeconomic factors than the racial/ethnic makeup of the school. Future research in more diverse settings is needed to adequately assess the relationship between racial/ethnic school composition and school policies and practices.
Overall trends over time
Overall trends over time indicated a number of changes from 2008 to 2012. The proportion of schools selling sports drinks declined from 2008 to 2012 (p = 0.04), consistent with another study of Minnesota secondary schools based on the same data source that found a decline in the sale of candy, salty snack, and sugary drinks among middle schools between 2002 and 2010.27 This finding could reflect increased attention to the nutritional quality of food and beverages sold in vending machines and school stores, particularly in schools with younger students. Schools became less likely to ban advertisements for LNED items on school grounds (p = 0.01), suggesting an increased use of advertising for revenue28,29 that may be used to cover basic costs and programming when financial resources are limited.30 This shift toward increased advertising should be examined in future research, and linked to changes in school budgets and student health outcomes.
Trends over time by school characteristics
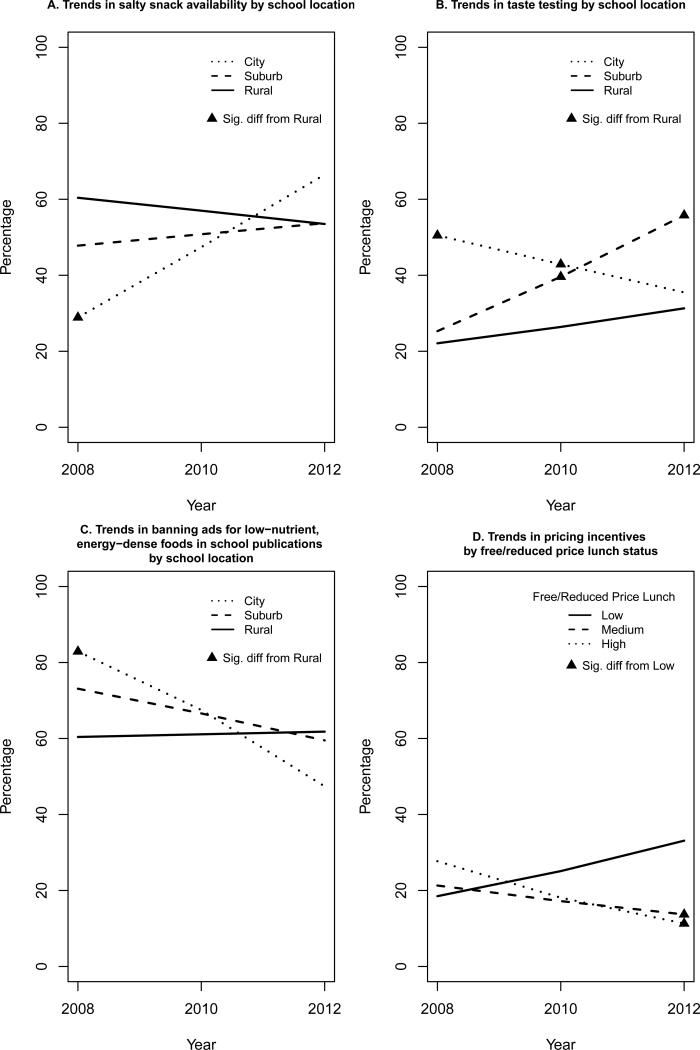
Trends over time in policies and practices with a statistically significant difference by school location or FRPL eligibility are presented in Figure 1. In 2008, city schools were less likely to sell salty snacks than rural schools, but this was no longer the case in 2012 (Figure 1a). City schools were also more likely to offer taste testing (Figure 1b) and ban advertisements in school publications (Figure 1c) than town/rural schools in 2008, but this was no longer the case in 2012. Additionally, by 2012, schools with high and moderate FRPL eligibility were less likely to offer pricing incentives for healthy food items than schools with low FRPL eligibility, whereas this was not the case in 2008 (Figure 1d).
Figure 1.
Adjusted prevalence of policies with different trends over time, Minnesota, 2008−2012.
Study findings suggest that maintaining policy environments consistent with healthy eating over time may be challenging for some schools. City schools may have initially played a leadership role in health promotion, compared with schools elsewhere, for political or other reasons.31 However, it appears that such policies were not sustained in city schools in recent years, perhaps because policies related to sales or advertising can garner much-needed financing for school programs.29 While the shifts observed in the current study represent a reduction in urban/rural disparities by some measures, they also indicate an overall worsening of conditions in city schools.
Strengths
This study has several strengths. The study used a large sample of schools to examine the current state of policies in Minnesota. Unlike previous studies,24,25 the current study captured multiple years and documented changes over time. The nutritional policies examined included those recommended for schools by the Institute of Medicine32 and policies that promote Healthy People 2020 goals.33 This study is also one of the first to examine differences in policy implementation across school-level characteristics including the racial/ethnic and socioeconomic composition of students, location, and grades enrolled.
Limitations
This study also has limitations. Findings from Minnesota schools may not be generalizable to other states. Previous work by the authors examined obesity-related school policies and found that Minnesota falls roughly in the middle,34 suggesting that these findings may be applicable to other areas. In addition, Minnesota has a mix of urban, suburban and rural areas similar to many other states.
Nutrition policies and practices at the school level were self-reported by school principals or designees, and it is possible that respondents were not aware of the current policy environment or did not accurately report answers. Although survey response rates were adequate, it is also possible that schools that did not participate were different from those that did participate. Only select nutritional policies that have been measured over time are reported, rather than reporting on all possible obesity-related indicators or policies.
CONCLUSIONS
In Minnesota, schools located in cities generally provide a healthier food environment for their students compared with schools in rural areas and towns. Despite these initial advantages, some policies and practices in city schools are eroding over time, while town and rural school policies have largely remained unchanged. Meanwhile, across all schools, advertising of LNED items appears to be increasing over time. These results indicate a need for further research to monitor future changes in these trends, and to understand the impact of these policies on diet, weight and academic outcomes across school settings.
Supplementary Material
Acknowledgements
This research was supported by a grant from National Institute for Health (5R01HD070738). Additional support for statistical analysis was provided by the National Center for Advancing Translational Sciences of the National Institutes of Health (UL1TR000114). The authors also thank Peter Rode and Susan Lowry for their contributions to the manuscript. Funding support for the lead author (CC) was also provided through the National Cancer Institute by the Cancer Related Health Disparities Education and Career Development Program (5R25CA163184). Funding agencies played no role in this study and the contents of this manuscript are solely the responsibility of the authors.
Funding disclosure
This research received funding from the National Institute for Health (grants 5R01HD070738, UL1TR000114, and 5R25CA163184). Funding agencies played no role contents of this manuscript. Manuscript contents are solely the responsibility of the authors.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of interest
The authors declare no conflict of interest.
REFERENCES
- 1.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999-2010. Jama-J Am Med Assoc. 2012;307(5):483–490. doi: 10.1001/jama.2012.40. doi:10.1001/jama.2012.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kumanyika S, Grier S. Targeting interventions for ethnic minority and low-income populations. Future Child. 2006;16(1):187–207. doi: 10.1353/foc.2006.0005. doi:10.1353/foc.2006.0005. [DOI] [PubMed] [Google Scholar]
- 3.Rossen LM, Schoendorf KC. Measuring health disparities: trends in racial-ethnic and socioeconomic disparities in obesity among 2- to 18-year old youth in the United States, 2001-2010. Ann Epidemiol. 2012;22(10):698–704. doi: 10.1016/j.annepidem.2012.07.005. doi:10.1016/j.annepidem.2012.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Singh GK, Siahpush M, Kogan MD. Rising social inequalities in US childhood obesity, 2003-2007. Ann Epidemiol. 2010;20(1):40–52. doi: 10.1016/j.annepidem.2009.09.008. doi:10.1016/j.annepidem.2009.09.008. [DOI] [PubMed] [Google Scholar]
- 5.Data/Statistics [April 12, 2013];U.S. Department of Health and Human Services Office of Minority Health. Available at: http://minorityhealth.hhs.gov/templates/browse.aspx?lvl=3&lvlid=537.
- 6.Vieweg VR, Johnston CH, Lanier JO, Fernandez A, Pandurangi AK. Correlation between high risk obesity groups and low socioeconomic status in school children. South Med J. 2007;100(1):8–13. doi: 10.1097/01.smj.0000253479.03665.6f. [DOI] [PubMed] [Google Scholar]
- 7.Tae-Seale T, Chandler C. Rural Healthy People 2010: A Companion Document to Healthy People 2010. The Texas A&M University System Health Science Center, School of Rural Public Health, Southwest Rural Health Center; College Station, TX: 2003. Nutrition and overweight concerns in rural areas: A literature review. pp. 115–130. [Google Scholar]
- 8.Liu J, Jones SJ, Sun H, Probst J, Merchant A, Cavicchia P. Diet, physical activity, and sedentary behaviors as risk factors for childhood obesity: an urban and rural comparison. Obesity. 2010;18:S178–S178. doi: 10.1089/chi.2012.0090. [DOI] [PubMed] [Google Scholar]
- 9.O'Malley PM, Johnston LD, Delva J, Bachman JG, Schulenberg JE. Variation in obesity among American secondary school students by school and school characteristics. Am J Prev Med. 2007;33(4):S187–S194. doi: 10.1016/j.amepre.2007.07.001. doi:10.1016/j.amepre.2007.07.001. [DOI] [PubMed] [Google Scholar]
- 10.Richmond TK, Subramanian SV. School level contextual factors are associated with the weight status of adolescent males and females. Obesity. 2008;16(6):1324–1330. doi: 10.1038/oby.2008.48. doi:10.1038/oby.2008.48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lee H, Harris KM, Lee J. Multiple levels of social disadvantage and links to obesity in adolescence and young adulthood. J Sch Health. 2013;83(3):139–149. doi: 10.1111/josh.12009. doi:10.1111/josh.12009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Martin MA, Frisco ML, Nau C, Burnett K. Social stratification and adolescent overweight in the United States: How income and educational resources matter across families and schools. Soc Sci Med. 2012;74(4):597–606. doi: 10.1016/j.socscimed.2011.11.006. doi:10.1016/j.socscimed.2011.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nanney MS, Davey C. Evaluating the distribution of school wellness policies and practices: A framework to capture equity among schools serving the most weight-vulnerable children. J Am Diet Assoc. 2008;108(9):1436–1439. doi: 10.1016/j.jada.2008.06.440. doi:10.1016/j.jada.2008.06.440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Belansky ES, Cutforth N, Chavez R, Crane LA, Waters E, Marshall JA. Adapted Intervention Mapping: A strategic planning process for increasing physical activity and healthy eating opportunities in schools =via environment and policy change. J Sch Health. 2013;83(3):194–205. doi: 10.1111/josh.12015. doi:10.1111/josh.12015. [DOI] [PubMed] [Google Scholar]
- 15.Larson N, Story M. Are “competitive foods” sold at school making our children fat? Health Aff Proj Hope. 2010;29(3):430–435. doi: 10.1377/hlthaff.2009.0716. doi:10.1377/hlthaff.2009.0716. [DOI] [PubMed] [Google Scholar]
- 16.Story M. The third School Nutrition Dietary Assessment Study: findings and policy implications for improving the health of US children. J Am Diet Assoc. 2009;109(2 Suppl):S7–13. doi: 10.1016/j.jada.2008.11.005. doi:10.1016/j.jada.2008.11.005. [DOI] [PubMed] [Google Scholar]
- 17.Belansky ES, Romaniello C, Morin C, et al. Adapting and implementing a long-term nutrition and physical activity curriculum to a rural, low-income, biethnic community. J Nutr Educ Behav. 2006;38(2):106–113. doi: 10.1016/j.jneb.2005.11.011. doi:10.1016/j.jneb.2005.11.011. [DOI] [PubMed] [Google Scholar]
- 18.Wechsler H, Devereaux RS, Davis M, Collins J. Using the school environment to promote physical activity and healthy eating. Prev Med. 2000;31(2):S121–S137. doi:10.1006/pmed.2000.0649. [Google Scholar]
- 19.Dority BL, McGarvey MG, Kennedy PF. Marketing foods and beverages in schools: the effect of school food policy on students’ overweight measures. J Public Policy Mark. 2010;29(2):204–218. [Google Scholar]
- 20. [July 26, 2013];CDC - School Health Profiles - Adolescent and School Health. Available at: http://www.cdc.gov/healthyyouth/profiles/.
- 21.Brener ND, Demissie Z, Foti K, et al. School Health Profiles: Characteristics of Health Programs Among Secondary Schools (Profiles 2010) Centers for Disease Control and Prevention; Atlanta, GA: 2010. [Google Scholar]
- 22.National Center for Educational Statistics Common Core of Data. 2013 Available at: http://nces.ed.gov/ccd.
- 23.USDA Economic Research Service [April 12, 2013];Rural-Urban Commuting Area Codes. Available at: http://www.ers.usda.gov/data-products/rural-urban-commuting-area-codes.aspx#.UWhl5TedXW8.
- 24.Nanney MS, Bohner C, Friedrichs M. Poverty-related factors associated with obesity prevention policies in Utah secondary schools. J Am Diet Assoc. 2008;108(7):1210–1215. doi: 10.1016/j.jada.2008.04.019. doi:10.1016/j.jada.2008.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nanney MS, Davey CS, Kubik MY. Rural disparities in the distribution of policies that support healthy eating in US secondary schools. J Acad Nutr Diet. 2013;113(8):1062–1068. doi: 10.1016/j.jand.2013.04.021. doi:10.1016/j.jand.2013.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Guthrie JF, Newman C, Ralston K, Prell M, Ollinger M. Understanding school food service characteristics associated with higher competitive food revenues can help focus efforts to improve school food environments. Child Obes Print. 2012;8(4) doi: 10.1089/chi.2012.0062. doi:10.1089/chi.2012.0062. [DOI] [PubMed] [Google Scholar]
- 27.Kubik MY, Davey C, Nanney MS, MacLehose RF, Nelson TF, Coombes B. Vending and school store snack and beverage trends: Minnesota secondary schools, 2002-2010. Am J Prev Med. 2013;44(6):583–588. doi: 10.1016/j.amepre.2013.02.009. doi:10.1016/j.amepre.2013.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Delva J, O'Malley PM, Johnston LD. Availability of more-healthy and less-healthy food choices in American schools - A national study of grade, Racial/Ethnic, and socioeconomic differences. Am J Prev Med. 2007;33(4):S226–S239. doi: 10.1016/j.amepre.2007.07.018. doi:10.1016/j.amepre.2007.07.018. [DOI] [PubMed] [Google Scholar]
- 29.Polacsek M, O'Rourke K, O'Brien L, Whatley J, Donahue S. Examining compliance with a statewide law banning junk food and beverage marketing in Maine schools. Public Health Rep. 2012;127(2):216–223. doi: 10.1177/003335491212700211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Crooks DL. Trading nutrition for education: Nutritional status and the sale of snack foods in an eastern Kentucky school. Med Anthropol Q. 2003;17(2):182–199. doi: 10.1525/maq.2003.17.2.182. doi:10.1525/maq.2003.17.2.182. [DOI] [PubMed] [Google Scholar]
- 31.Schwartz MB, Henderson KE, Falbe J, et al. Strength and comprehensiveness of district school wellness policies predict policy implementation at the school level. J Sch Health. 2012;82(6):262–267. doi: 10.1111/j.1746-1561.2012.00696.x. doi:10.1111/j.1746-1561.2012.00696.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. [August 30, 2013];Nutrition Standards for Foods in Schools: Leading the Way Toward Healthier Youth. Available at: http://www.nap.edu/openbook.php?record_id=11899.
- 33.Healthy People 2020 [April 15, 2013]; Available at: http://www.healthypeople.gov/2020/topicsobjectives2020/objectiveslist.aspx?topicId=29.
- 34.Nanney MS, Nelson T, Wall M, et al. State school nutrition and physical activity policy environments and youth obesity. Am J Prev Med. 2010;38(1):9–16. doi: 10.1016/j.amepre.2009.08.031. doi:10.1016/j.amepre.2009.08.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.