Abstract
Objectives
To describe the characteristics of head and neck leiomyosarcoma and to identify factors associated with survival.
Design
Retrospective population-based study.
Patients
The 17-registry Surveillance, Epidemiology, and End Results database was used to identify 578 patients with leiomyosarcoma of the head and neck.
Interventions
Surgery and primary and adjuvant radiotherapy.
Main Outcome Measures
Patient demographics and tumor characteristics were examined. Treatment modalities were compared, and survival was assessed using the log-rank test.
Results
The mean age at diagnosis was 64 years. Most tumors were smaller than 5 cm in greatest dimension (87%) and high grade (44% were moderately differentiated and 39% were poorly differentiated). The primary tumor demonstrated deep extension in 39% of cases, and 2% had lymph node metastases. The most common primary site was the skin and soft tissue of the head and neck (83%). Surgical treatment was provided to 89% of patients, 14% received adjuvant radiotherapy, and 4% received radiotherapy alone. The median observed survival was 84.7 months. The 5-year disease-specific survival rate was 87.6% in patients with well-differentiated tumors, 85.7% in patients with moderately differentiated tumors, and 52.7% in patients with poorly differentiated tumors (P<.001). Survival was better for patients who received surgery alone (median survival, 100.1 months [n=413]) than for those who received radiotherapy alone (median survival, 16 months [n=16]) or adjuvant radiotherapy (median survival, 64.2 months [n=80]) (P<.001). The latter group was more likely to have poorly differentiated, large, locally invasive tumors.
Conclusions
Leiomyosarcoma typically presents in older patients; it is often poorly differentiated; and improved survival is associated with surgical treatment.
Soft-tissue sarcomas are rare in the head and neck, accounting for 1% of malignant neoplasms in this area.1 Leiomyosarcoma (LMS), a sarcoma derived from smooth muscle that can be either cutaneous (derived from arrector pili muscles of hair follicles) or subcutaneous (derived from vascular smooth muscle), represents 1% to 4% of such tumors.2-4 As such, LMS of the head and neck is an extremely rare entity that because of its infrequency has been associated with both delayed diagnosis and misdiagnosis.5,6
LeVay et al7 reviewed a single institution’s experience with head and neck soft-tissue sarcoma. The patients were treated with primary surgery, with or without adjuvant radiotherapy. The authors found tumor size greater than 5 cm, high-grade histologic type, and surgical margin status to be predictors of poor survival. However, of 52 cases treated curatively, only 3 were LMS. Farhood et al8 reported similar prognostic factors in another series of soft-tissue sarcomas of the head and neck. We performed a population-based analysis to better clarify the disease characteristics, survival rates, and practice patterns of this rare tumor. Furthermore, we examined whether there were survival differences between cutaneous and noncutaneous LMS.
METHODS
We reviewed the Surveillance, Epidemiology, and End Results (SEER) database, which includes 17 registries that together cover 26% of the US population, to identify patients who were diagnosed as having International Classification of Diseases for Oncology, Third Edition, histology codes 8890, 8891, 8895, and 8896 (LMS not otherwise specified , epithelioid LMS, myosarcoma, and myxoid LMS) between 1973 and 2007. We included all head and neck subsites (oral cavity, pharynx, major salivary gland, nasal cavity, larynx, skull, mandible, orbit, thyroid, parathyroid, and carotid body) as well as adjacent skin, nerve, lymphatic tissue, and connective tissue.
We also examined patient demographic characteristics (sex, race, and age), tumor characteristics (histologic differentiation, size and extent of tumor, and primary site), and treatment, which included both surgery and radiotherapy, with survival being the main outcome measure, and compared survival for cutaneous and noncutaneous LMS. We analyzed data using SAS version 9.2 (SAS Institute, Cary, North Carolina) and calculated relative frequencies for all demographic and tumor characteristics as well as treatment modalities. The Kaplan-Meier method was used to estimate survival, and the log-rank test was used to examine differences between groups. Statistical significance was defined as P≤.05. Institutional review board approval was not required.
RESULTS
PATIENT AND TUMOR CHARACTERISTICS
A total of 578 patients with LMS were identified, most of whom were male (68%) (95% confidence interval, 63.8%-71.4%) and white (89%); only 9% of the patients were of minority descent (Table 1). The frequency of LMS increased with age: more than 50% of the patients were older than 70 years, and 75% were older than 50 years at the time of diagnosis (mean age at diagnosis, 64 years). The primary site of 83% of the tumors was the skin and soft tissue of the head and neck, with a minority found in mucosal sites and salivary glands. The histologic type of most tumors was LMS not otherwise specified (95%), with epithelioid, myxoid, and myosarcoma variants making up the remainder. Few tumors were well differentiated (16.4%), as most were either moderately (44.4%) or poorly (39.2%) differentiated. Most tumors were smaller than 5 cm in greatest dimension (87%) and localized (61%), with a substantial minority demonstrating deep extension (39%) and only 2% demonstrating lymphatic spread (Table 2).
Table 1.
Demographics of 578 Patients With Leiomyosarcoma of the Head and Neck
| Variable | No. (%) |
|---|---|
| Sex | |
| Female | 187 (32.3) |
| Male | 391 (67.6) |
| Race | |
| Black | 25 (4.3) |
| Other | 27 (4.7) |
| Unknown | 11 (1.9) |
| White | 515 (89.1) |
| Age, y | |
| <50 | 144 (24.9) |
| 50-59 | 64 (11.1) |
| 60-69 | 81 (14.0) |
| 70-79 | 133 (23.0) |
| ≥80 | 156 (27.0) |
Table 2.
Tumor Characteristics in 578 Cases of Leiomyosarcoma (LMS) of the Head and Neck
| Variable | No. (%) |
|---|---|
| Histologic tumor type | |
| LMS NOS | 552 (95.5) |
| Epithelioid LMS | 16 (2.8) |
| Myosarcoma | 7 (1.2) |
| Myxoid LMS | 3 (0.5) |
| Grade | |
| Well differentiated | 41 (16.4) |
| Moderately differentiated | 111 (44.4) |
| Poorly differentiated | 98 (39.2) |
| Extent | |
| Localized | 307 (61.3) |
| Deep extension | 186 (37.1) |
| Distant spread | 8 (1.6) |
| Size, cm | |
| ≤5 | 257 (86.8) |
| >5 | 39 (13.2) |
| Head and neck subsite | |
| Oral cavity/pharynx | 33 (5.7) |
| Salivary gland | 8 (1.4) |
| Nasal cavity | 31 (5.4) |
| Larynx | 13 (2.2) |
| Skull/mandible | 4 (0.7) |
| Soft tissue | 302 (52.2) |
| Skin | 175 (30.3) |
| Orbit | 6 (1.0) |
| Other | 6 (1.0) |
Abbreviation: NOS, not otherwise specified.
TREATMENT AND SURVIVAL
Leiomyosarcoma of the head and neck was most commonly treated with surgery (89%). In 14% of patients, treatment comprised primary surgery with adjuvant radiotherapy. An additional 4% of cases were treated with primary radiotherapy. Of the few cases in which surgery was not performed, it was not recommended in 6% and recommended but not pursued because of patient refusal or other reason in 4%.
The median observed survival for our cohort was 84.7 months, with 56.4% of the patients surviving 5 years. The 5-year disease-specific survival for well-differentiated tumors was 87.6% compared with 85.7% for moderately differentiated tumors and 52.7% for poorly differentiated tumors (P<.001)(Figure 1). A similar trend was noted for 5-year disease-specific observed survival (data not shown). Improved survival was noted for patients who received surgery alone (median survival, 100.1 months [n = 413]) compared with those who received radiotherapy alone (median survival, 16 months, n=16) or adjuvant radiotherapy (median survival, 64.2 months, [n=80]) (P<.001). Patients who were treated with adjuvant radiotherapy were more likely to have poorly differentiated, large, locally invasive tumors.
Figure 1.
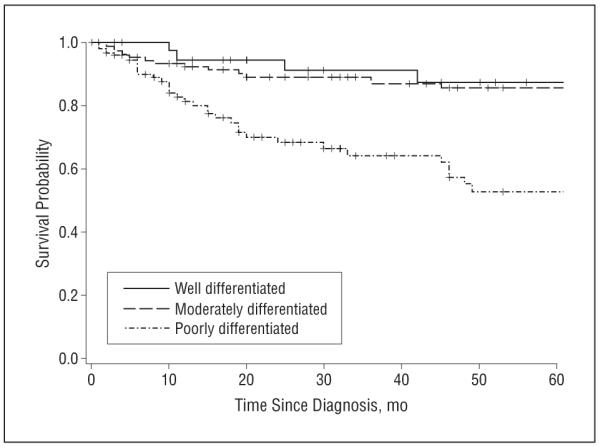
Survival curve of tumor differentiation and disease-specific survival.
Tumors were also divided into cutaneous (n=175) and noncutaneous (n=403) groups to compare survival differences. Although 5-year disease-specific survival was improved for cutaneous LMS (96.3% vs 70.5%; P<.001), observed survival only approached significance (66.9% vs 52.1; P=.08) (Figure 2). However, patients with cutaneous LMS were older (Table 3). When cutaneous tumors were excluded, the trend of improved survival for patients with well-differentiated tumors was maintained (data not shown).
Figure 2.
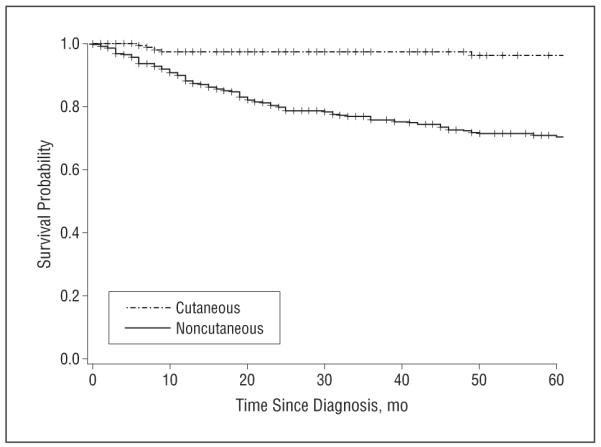
Survival curve of cutaneous vs noncutaneous disease-specific survival.
Table 3.
Distribution of Cutaneous vs Noncutaneous Leiomyosarcoma (LMS) by Patient Agea
| Age, y |
|||||
|---|---|---|---|---|---|
| Type of LMS | <50 | 50-59 | 60-69 | 70-79 | ≥80 |
| Cutaneous | 24 | 15 | 19 | 48 | 69 |
| Noncutaneous | 120 | 49 | 62 | 85 | 87 |
(P<.001).
COMMENT
Leiomyosarcoma is a rare entity in the head and neck. The data presented herein describe its basic clinical characteristics. Importantly, 13% of head and neck LMS tumors were larger than 5 cm at the time of diagnosis, and 39% were described as deeply invasive. Almost 40% of tumors were poorly differentiated. This number is clinically relevant because poorly differentiated tumors were associated with worse observed and disease-specific survival. As expected for sarcomas, there were few patients with lymph node metastasis at presentation.
Surgery is generally described as the mainstay of treatment for LMS of the head and neck, with adjuvant radiotherapy in selected cases, and radiotherapy alone reserved for cases in which surgery was not recommended or refused.9 Our series of patients shows that these recommendations were generally followed. In our cohort, patients who received surgery alone had improved survival compared with those who received primary or adjuvant radiotherapy, implying that adjuvant radiotherapy was reserved for patients who had poor prognostic factors such as large, invasive tumors with poorly differentiated histologic features.
Our results suggest that LMS is more common in males. The sarcoma series described by LeVay et al7 reported a similar ratio; however, that by Farhood et al8 showed an equal distribution between sexes. The reason for the possible male predilection is not clear. Our cohort demonstrated a median survival of approximately 7 years after diagnosis; however, patients with high-grade tumors had worse survival. The series reported by LeVay and colleagues, who noted a 5-year disease-specific survival of 63%, did not stratify tumors based on grade in their survival calculations. Farhood and colleagues argue that not stratifying patients with sarcoma by grade leads to falsely elevated survival statistics. In their series, patients with high-grade sarcomas had a 5-year observed survival of 32%, whereas those with lowgrade tumors had a 90% 5-year survival. Our results corroborate this trend (87.6% 5-year disease-specific survival for well-differentiated tumors compared with 52.7% for poorly differentiated tumors).
There are several drawbacks to our analysis. Although the SEER database is compiled from records at many centers around the country, the patients in the database may not be reflective of the US population. The current 17-registry SEER database, covering 26% of the US population, has been in place since 2000. Before that time, there were fewer registries, so a smaller portion of the population was represented. However, this population-based database does not have a bias toward larger or more complicated tumors, as might occur in series identified at tertiary care referral centers.
A prior review of LMS showed that the most common location of the primary lesion was the oral cavity followed by the paranasal sinuses, findings that do not agree with our results.10 The site of the primary lesion for more than 50% of the tumors in our cohort was classified as soft tissue. This discrepancy could arise from limitations of the SEER database and poor classification of primary tumor sites, or it could be attributable to the comparably larger number of patients in our cohort. The SEER database does not capture detailed information about chemotherapy, so we cannot describe its role in our population. Surgical margin status, a well-described prognostic factor, was also not available. Furthermore, although the SEER database describes patients’ initial presentation in detail, it does not provide data on patients’ clinical course. Therefore, we cannot draw conclusions about common patterns of recurrence.
An important question related to soft-tissue sarcomas involves their relationship to prior cancer radiotherapy. The SEER database does not allow a detailed analysis of this patient history. Analysis of the relationship between prior head and neck radiotherapy and the clinical course of subsequent LMS would require a true cohort study.
In conclusion, because of the scarcity of LMS cases, most studies are underpowered to characterize LMS. Use of the SEER database has allowed us to complete a population-based analysis of a large cohort. Despite the limitations of retrospective analysis, several trends have emerged. Leiomyosarcoma typically presents in older patients; it is often poorly differentiated; and improved survival is associated with surgical treatment. Because of the rarity of LMS, more studies are needed to characterize this disease.
Footnotes
Author Contributions: Dr Pagedar had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: Eppsteiner, Milhem, and Pagedar. Acquisition of data: DeYoung and Pagedar. Analysis and interpretation of data: Eppsteiner, DeYoung, Milhem, and Pagedar. Drafting of the manuscript: Eppsteiner. Critical revision of the manuscript for important intellectual content: Eppsteiner, DeYoung, Milhem, and Pagedar. Statistical analysis: Pagedar. Study supervision: DeYoung and Pagedar.
Financial Disclosure: None reported.
Previous Presentation: This study was presented in part at the American Head and Neck Society Annual Meeting; April 28, 2011; Chicago, Illinois.
REFERENCES
- 1.Weber RS, Benjamin RS, Peters LJ, Ro JY, Achon O, Goepfert H. Soft tissue sarcomas of the head and neck in adolescents and adults. Am J Surg. 1986;152(4):386–392. doi: 10.1016/0002-9610(86)90309-0. [DOI] [PubMed] [Google Scholar]
- 2.De Giorgi V, Sestini S, Massi D, Papi F, Alfaioli B, Lotti T. Superficial cutaneous leiomyosarcoma: a rare, misleading tumor. Am J Clin Dermatol. 2008;9(3):185–187. doi: 10.2165/00128071-200809030-00008. [DOI] [PubMed] [Google Scholar]
- 3.Freedman AM, Reiman HM, Woods JE. Soft-tissue sarcomas of the head and neck. Am J Surg. 1989;158(4):367–372. doi: 10.1016/0002-9610(89)90135-9. [DOI] [PubMed] [Google Scholar]
- 4.Singh RP, Grimer RJ, Bhujel N, Carter SR, Tillman RM, Abudu A. Adult head and neck soft tissue sarcomas: treatment and outcome. Sarcoma. 2008;2008:654987. doi: 10.1155/2008/654987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schadendorf D, Haas N, Ostmeier H, Czarnetzki BM. Primary leiomyosarcoma of the skin: a histological and immunohistochemical analysis. Acta Derm Venereol. 1993;73(2):143–145. doi: 10.2340/0001555573143145. [DOI] [PubMed] [Google Scholar]
- 6.Snowden RT, Osborn FD, Wong FS, Sebelik ME. Superficial leiomyosarcoma of the head and neck: case report and review of the literature. Ear Nose Throat J. 2001;80(7):449–453. [PubMed] [Google Scholar]
- 7.LeVay J, O’Sullivan B, Catton C, et al. Outcome and prognostic factors in soft tissue sarcoma in the adult. Int J Radiat Oncol Biol Phys. 1993;27(5):1091–1099. doi: 10.1016/0360-3016(93)90529-5. [DOI] [PubMed] [Google Scholar]
- 8.Farhood AI, Hajdu SI, Shiu MH, Strong EW. Soft tissue sarcomas of the head and neck in adults. Am J Surg. 1990;160(4):365–369. doi: 10.1016/s0002-9610(05)80544-6. [DOI] [PubMed] [Google Scholar]
- 9.Shellenberger TD, Sturgis EM. Sarcomas of the head and neck region. Curr Oncol Rep. 2009;11(2):135–142. doi: 10.1007/s11912-009-0020-8. [DOI] [PubMed] [Google Scholar]
- 10.Suen J, Vural E, Waner M. Unusual tumors. In: Myers E, Suen J, Myers J, Hanna E, editors. Cancer of the Head and Neck. WB Saunders Co; Philadelphia, PA: 2003. pp. 611–629. [Google Scholar]


