Abstract
Background
The aim of this study was to detect the seroprevalence of human fascioliasis in Isfahan County, central Iran in 2013.
Methods
Overall, 471 sera samples were collected from people recalled randomly to 20 health centers in the city of Isfahan and 10 related villages in 2014. Sera were examined using ELISA test. A questionnaire was filled out for each participant.
Results
Altogether eight cases (1.7%) were seropositive which had the OD absorbance in ELISA test more than the calculated cutoff of 0.36. All of them were female. One positive subject had a history of consuming Delar (Local dish) and three seropositive cases with history of eating Zeitoon-Parvadeh (Proceeded olive).
Conclusion
Isfahan County might be considered as one area apt for fascioliasis. More studies in terms of veterinary investigation and verifying the risk factors are necessary.
Keywords: Fascioliasis, Prevalence, ELISA, Iran
Introduction
Fascioliasis is a zoonotic disease caused by liver parasites, Fasciola hepatica and F. gigantica(1). It is one of the important neglected tropical diseases disseminated in most parts of the world and especially in the Middle East and parts of the Africa (2). About 56.2 million people were infected with food-borne trematodes, 7.9 million had severe sequelae, and the global burden was 665,352 DALYs, of which a most important contribution was attributed to fasciolosis (3).
An infective metacercaria, produced after spending the evolution cycle in the presence of an intermediate snail, is deposited on the water plant or suspended in the water. It is ingested by people through different by either cyst-contaminated vegetation or water, and excysts in the duodenum, releasing the juvenile stage, which burrows through the gut mucosa and migrates to the liver parenchyma. After 3-4 months, the parasite mature and reside in the bile ducts (4).
The highest rate of illness relates to Bolivia, Peru, Cuba, Portugal, Spain, Nile delta in Egypt, central areas of Vietnam and Northern Iran (5). Up to 1989, human fasciolosis was reported only sporadically in Iran. In 1989, the world’s biggest outbreak occurred in Gilan Province, northern Iran, affecting more than 10,000 people (6, 7). Ten years later this region again encountered with the 2nd outbreak of 10-15,000 infected people (8). Several hundred additional human cases reported before and after the second outbreak, caused this province to be called an endemic region for human fasciolosis, particularly in Bandar-Anzali City.
Due to the specific situation of Iran and occurrence of new foci for fasciolosis (9, 10), and receiving some reports on noticing Fasciola parasite during surgery operation in Isfahan, we decided to clarify the seroprevalence of human fascioliasis using indirect ELISA in Isfahan District, central Iran.
Materials and Methods
Serum collection
Isfahan district is located in central Iran. The city has a population of 2174172 people (Fig. 1). Overall, 470 serum samples were collected from Isfahan City, and suburb area in 2014. According to the statistician consultant, because population of the city is higher than in rural areas, 320 samples were collected from the city and 150 from rural areas. Based on a random sampling, people were asked to present in health centers for collecting sera.
Fig. 1.
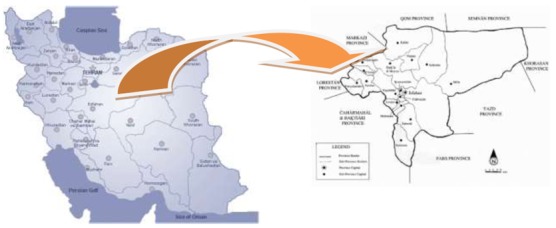
Location of Isfahan Province in Iran
A questionnaire including information on food diet, vegetable consumption, travelling to northern Iran, clinical symptoms etc. was filled out for each patient. Bedsides, informed consent was taken from each of them and in case of inability of the participant to fill it out for any reason, his/her guardians were asked to do so.
The study was approved already by the Ethics Committee of Tehran University of Medical Sciences, Tehran, Iran.
Antigen preparation
For antigen preparation, Fasciola infected livers were prepared from Tehran slaughterhouses and transferred to the laboratory of Helminthic Diseases, School of Public Health, Tehran University of Medical Sciences, Iran. After isolation of parasites from liver, and washing for 6 times with normal saline, they were homogenized in 0.045 mM PBS with electrical homogenizer. After homogenization, sonication was carried out and centrifuged in 10000 g at 4 °C for 15 min. The supernatant was kept in refrigerator for later usage.
ELISA test
ELISA test was conducted based on previously reported study with some modifications (11). Briefly, 100 microliters of somatic antigen (10 mg/ml) was added to wells of plates and incubated overnight at 37 °C and then 200 microliters of BSA 2% was dispensed to microtiter plates. Wells of plates were washed with PBS/Tween 20 for three times. One hundred microliters of a serum samples (diluted 1:500) was added to wells coated with antigen and incubated at 37 °C for 30 min. Plates were washed 5 times with PBS/Tween 20. Peroxidase-conjugated goat anti-human IgG (diluted 1:10000) was added to wells and incubated at 37 °C for 30 min. After final washing step with PBS/Tween 20, 100 microliters of OPD (O-phenylendiaminedihydrochloride) was added to wells and reaction was stopped with adding 50 microliters of stopper solution (12.5% H2S04). OD was measured at 490 nm with ELISA reader.
Statistical analysis
Statistical analysis was done using SPSS version 16 (Chicago, IL, USA). Chi square test was used for analyzing of data. Cut-off was calculated as Mean± 3 SD.
Results
Cut-off was calculated as 0.36. Of 470 examined cases, 197 (41.8%) were male and 274 (58.2%) were female. Altogether eight persons (1.7%) were serologically positive for fasciolosis. Figure 1 demonstrates the distribution of OD absorbance in subjects and healthy control cases. Of these four people were resident in urban areas of the city. The highest positive rate was in age group of more than 60 yr old. Table 1 shows the seropositivity in different age groups.
Fig. 1.
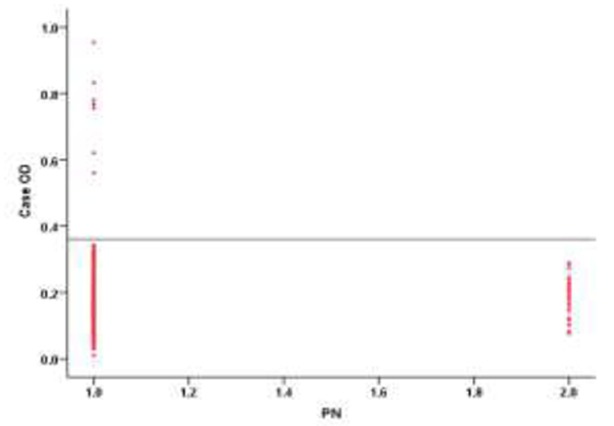
Analysis of sera from subjects and normal controls from Isfahan City and rural areas, Isfahan Province, Iran by IgG-ELISA. Serum samples obtained from subjects (470 cases, Lanes 1), and normal controls (30, Lanes 2)
Table 1.
Seropositivity rate of fascioliasis in different age groups from Isfahan City, and suburb area in 2014
| Age groups(yr) | Total No. | Seropositivity Cases No. (%) |
|---|---|---|
| ≤9 | 5 | 0 (0.0) |
| 10-19 | 14 | 1 (7.1) |
| 20-29 | 115 | 1 (0.9) |
| 30-39 | 91 | 2 (2.2) |
| 40-49 | 94 | 0 (0.0) |
| 50-59 | 69 | 1 (1.4) |
| ≥60 | 83 | 3 (3.6) |
| Total | 471 | 8 |
All eight positive cases were female which showed significant difference with male cases (P<0.05). Of them four cases were illiterate followed by three cases of preliminary educations and one case of secondary education. Seven positive cases were housekeepers and one case was self-employment. In terms of eating Delar (local dish), only one of seropositive case had the history.
Discussion
In this study using ELISA, we could detect the 1.7% seropositivity for human fasciolosis in Isfahan City and rural areas. Following up filling the gap of determining the rate of fasciolosis in apt regions of Iran, this study is of importance. According to the literature, it might be considered as a mesoendemic case of human fasciolosis (12).
Generally, Iran is one of the most important countries that are known for human fasciolosis (2). North parts of Iran with a history of two great outbreaks are the most involved regions in the country (13, 14). In north parts of Iran, Ashrafi et al. have reported the prevalence of 0.4% and 1.2% using coprological and serological methods, respectively, confirming a hypoendemic situation (15).The disease in Iran is considered as emerging and reemerging case. Sarkari et al., reported for the first time 1.8% of seropositivity in people of Yasuj District, Kohkiloyeh and Boyerahmad Province, southeast Iran (9). Besides another case of small outbreak as emerging cases, was reported in Kermanshah City, western Iran (10).
In our study, the highest rate of seropositivity was seen in age group of >60 yr old. Normally Iran is considered of a pattern of fasciolosis mostly in adults than children (5). During the outbreaks in Gilan and Kermanshah, the highest number of infected individuals was seen in the 10-29 year and in 10-19 year age groups, respectively. In non-epidemic situations, the numbers of infected cases were higher in older (> 20 year) age groups (15, 16).
All of positive cases in our study were female. In Iran, Asmar et al., reported that prevalence of disease in females as 1.16% higher than males (7). In Ilam Province, western Iran that seroprevalence rate in women was higher than men (17). In Peru, the rate of infection in men has been higher than women in most of regions (18). In Egypt, seroprevalence of fascioliasis in males was higher than in females (19).
In terms of eating Delar (local dish), made using local water plants, only one of seropositive case had the history of its eating.Two very important sources in the endemic regions of northern Iran are green salt (Local name: Dalar) and elaborated olive (Local name: Zeitoon parvardeh) (20).
Conclusion
The rate of seropositivity for human fasciolosis in Isfahan shows an apt region for this disease. This is for the first time that a seroprevalence study is conducted. No doubt to determine the exact rate of infection in the area we need to examine more cases and use coprological tests in addition to ELISA to be sure of the result as much as possible.
Acknowledgments
The study was financially supported by Deputy of Research, Tehran University of Medical Sciences through grant No. 23081-27-01-93. The study was conducted as an MSPH thesis of the first author. The authors declare that there is no conflict of interest.
Reference
- 1.Mas-Coma S, Bargues MD, Valero MA. Fascioliasis and other plant-borne trematode zoonoses. Int J Parasitol. 2005;35:1255–1278. doi: 10.1016/j.ijpara.2005.07.010. [DOI] [PubMed] [Google Scholar]
- 2.Rokni MB, Lotfy WM, Ashrafi K, Murrell KD. Fasciolosis in the mena region. In: McDowell MA, Rafati S, editors. Neglected tropical diseases - Middle east and north Africa. Springer; Vienna: 2014. [Google Scholar]
- 3.Fürst T, Keiser J, Utzinger J. Global burden of human food-borne trematodiasis: A systematic review and meta-analysis. The Lancet Infectious Diseases. 2012;12:210–221. doi: 10.1016/S1473-3099(11)70294-8. [DOI] [PubMed] [Google Scholar]
- 4.Mas-Coma S, Bargues M. Human liver flukes: A review. Res Rev Parasitol. 1997;57:145–218. [Google Scholar]
- 5.Mas-Coma S. Epidemiology of fascioliasis in human endemic areas. J Helminthol. 2005;79:207–216. doi: 10.1079/joh2005296. [DOI] [PubMed] [Google Scholar]
- 6.Massoud J. Fasciolosis outbreak in man and drug test (triclabandazole) in caspian littoral, northern part of iran. Bull Soc France Parasitol. 1989;8:438. [Google Scholar]
- 7.Assmar M, Milaninia A, Amir-Khani A, Yadegari D, Forghan-Parast K, Nahravanian H, Piazak N, Esmayli A, Hovanesian A, Valadkhani Z. Seroepidemiological investigation of fascioliasis in northern iran. Medical Journal of the Islamic Republic of Iran. 1991;5:23–27. [Google Scholar]
- 8.Forghan-parast K, Yadegari D, Asmar M. Clinical epidemiology of human fascioliasis in gilan. Journal of Gilan University of Medical Sciences. 1993;6:4–11. [Google Scholar]
- 9.Sarkari B, Ghobakhloo N, Moshfea A, Eilami O. Seroprevalence of human fasciolosis in a new-emerging focus of fasciolosis in Yasuj district, southwest of Iran. Iran J Parasitol. 2012;7:15–20. [PMC free article] [PubMed] [Google Scholar]
- 10.Hatami H, Asmar M, Masoud J, Mansouri F, Namdaritabar H, Ramazankhani A. The first epidemic and new-emerging human fascioliasis in Kermanshah (western Iran) and a ten-year follow up, 1998-2008. Int J Prev Med. 2012;3:266–272. [PMC free article] [PubMed] [Google Scholar]
- 11.Rokni MB, Massoud J, O’Neill SM, Parkinson M, Dalton JP. Diagnosis of human fasciolosis in the Gilan province of northern Iran: Application of cathepsin L-ELISA. Diagn Microbiol Infect Dis. 2002;44:175–179. doi: 10.1016/s0732-8893(02)00431-5. [DOI] [PubMed] [Google Scholar]
- 12.Mas-Coma M, Esteban J, Bargues M. Epidemiology of human fascioliasis: A review and proposed new classification. Bull World Health Organ. 1999;77:340–346. [PMC free article] [PubMed] [Google Scholar]
- 13.Ashrafi K, Valero MA, Massoud J, Sobhani A, Solaymani-Mohammadi S, Conde P, Khoubbane M, Bargues MD, Mas-Coma S. Plant-borne human contamination by fascioliasis. Am J Trop Med Hyg. 2006;75:295–302. [PubMed] [Google Scholar]
- 14.Rokni MB. The present status of human helminthic diseases in Iran. Ann Trop Med Parasitol. 2008;102:283–295. doi: 10.1179/136485908X300805. [DOI] [PubMed] [Google Scholar]
- 15.Ashrafi K, Saadat F, Rahmati B. Evaluating the level of endemicity of human fascioliasis in rural communities of bandar-e-anzali district; an important step for implementation of disease control programs. First International and 8th National Congress of Parasitology and Parasitic Diseases in Iran; Kerman, Iran. 17-19; Oct, 2012. p. 121. [Google Scholar]
- 16.Moghaddam AS, Massoud J, Mahmoodi M, Mahvi AH, Periago MV, Artigas P, Fuentes MV, Bargues MD, Mas-Coma S. Human and animal fascioliasis in mazandaran province, northern Iran. Parasitol Res. 2004;94:61–69. doi: 10.1007/s00436-004-1169-6. [DOI] [PubMed] [Google Scholar]
- 17.Abdi J, Naserifar R, Rostami Nejad M, Mansouri V. New features of fascioliasis in human and animal infections in Ilam province, western Iran. Gastroenterol Hepatol Bed Bench. 2013;6:152–155. [PMC free article] [PubMed] [Google Scholar]
- 18.González L, Esteban JG, Bargues MD, Valero MA, Ortiz P, Náquira C, Mas-Coma S. Hyperendemic human fascioliasis in andean valleys: An altitudinal transect analysis in children of Cajamarca province, Peru. Acta Tro. 2011;120:119–129. doi: 10.1016/j.actatropica.2011.07.002. [DOI] [PubMed] [Google Scholar]
- 19.Periago M, Valero M, El Sayed M, Ashrafi K, El Wakeel A, Mohamed M, Desquesnes M, Curtale F, Mas-Coma S. First phenotypic description of Fasciola hepatica, Fasciola gigantica and intermediate forms from the human endemic area of the Nile delta, Egypt. Infect Genet Evol. 2008;8:51–58. doi: 10.1016/j.meegid.2007.10.001. [DOI] [PubMed] [Google Scholar]
- 20.Ashrafi K, MA Valero K, Forghan-Parast M, Rezaeian SJ, Shahtaheri MR, Hadiani MD, Bargues S, Mas-Coma S. Potential transmission of human fascioliasis through traditional local foods, in northern Iran. Iran J Publ Health. 2006;35:57–63. [Google Scholar]


