Abstract
Statement of the Problem
Orthodontists often find challenges in treating the anterior open bite and maintaining the results.
Purpose
This retrospective study was aimed to evaluate the stability of corrected open bite in the retention phase during permanent dentition.
Materials and Method
A total number of 37 patients, including 20 males and 17 females, with the mean age of 18±2.1 years at the beginning of the treatment were studied after correction of the anterior open bite. Overbites of the patients were measured from their lateral cephalograms before (T1), at the end (T2) and at least 3 years after the end of the treatment in the presence of their fixed retainers (T3).The mean overbite changes and the number of patients with open bite, due to treatment relapse, at T3 were calculated. The relationship between the pre-treatment factors and the treatment relapse was assessed at T1 and T2. Also the effects of treatment methods, extraction and adjunctive use of removable appliances on the post-treatment relapse were evaluated.
Results
The mean overbite change during the post-treatment period was -0.46±0.7 mm and six patients (16.2%) had relapse in the follow-up recall. Cephalometric Jaraback index showed statistically significant, but weak correlation with overbite changes after the treatment (p= 0.035; r= -0.353). No significant difference was found between the extraction and non-extraction groups (p= 0.117) the use and the type of the removable appliances (p= 0.801).
Conclusion
Fixed retainers alone are insufficient for stabilizing the results of corrected open bite. The change of overbite in the retention phase could not be predicted from cephalometric measurements. Extraction and use of adjunctive removable appliance did not have any effect on the treatment relapse.
Key Words: Open bite, Relapse, Stability, Retention
Introduction
Orthodontists often find challenges in treating the anterior open bite and maintaining the results. Race and age are the two variables which can affect the occurrence of anterior open bite. [1] For instance, the prevalence of open bite is more in African Americans than in Caucasians or Hispanics. [1] The prevalence of open bite in different Iranian populations and various age categories has been reported to be from 1.6% [2] to 7.8%. [3] Prevalence of open bite has been shown to be 3.8% among the students aged 9-11 in downtown Shiraz in 2000. [4]
Open bite is a multifactorial, i.e. it cannot be induced by only a single factor. [5] The underlying influential causes are oral habits, undesirable growth patterns, enlarged lymphatic tissue and mouth breathing, as well as the tongue size and position. [6]
Open bite diagnosis is based on clinical examination and cephalometric analysis. A large interlabial gap is considered to be the most significant soft tissue feature of a skeletal open bite. [7] The steepness of mandibular plane is concerned as the key skeletal finding in skeletal anterior open bite. [8]
For the treatment of growing patients with anterior open bite, various appliances have been suggested such as occipital headgear, posterior bite block, vertical chin cup, [9] palatal crib, open bite bionator [10] and functional appliances. [11]
Anterior open bite is one of the most challenging malocclusion type to be retained after treatment. [12] The difficulty of maintaining the occlusion arises from the lack of control over the tongue position and movements in open bite cases. [12] In addition to the overcorrection, different retainers have been recommended for the patients such as occipital headgears, functional appliances with posterior thick bite plane [13] or palatal cribs, [14] as well as fixed retainers.
The negative esthetic features including reverse smile line and interproximal anterior spacing are usually expected when the relapse occurs in open bite patients. Concerning the mechanical difficulty involved in retaining the vertical correction, especially in the case of incisor extrusion, dentists have found it a serious challenge to maintain the long-term stability of anterior open bite treatment. Due to the complex interaction of all possible etiologic factors, ambiguity still remains on the reasons behind instability. [15]
Continuation of vertical facial growth through adolescence, long duration of the treatment, necessity of long-term cooperation of open bite patients [16] and greater rate of the relapse in this malocclusion are the issues required for comprehensive studies on the stability of open bite treatments.
Remmors et al. [17] evaluated 52 patients with pre-treatment open bite and observed that 27% of successfully treated patients showed opening of the bite 5 years after treatment. The study of Jonson et al. [18] showed negative overlap in 25.8% of their sample group at the end of post-treatment period, Lopez Gavito et al. [19] found treatment relapse in more than 35% of their patients in the post-retention period. Zuroff et al. [20] divided 64 patients into three groups according to the amount of the pre-treatment overbite and reported that all patients had positive overbite at the post retention recall. The study of de Freitas et al. [21] showed no relation between the overbite at the beginning of the treatment or its change during treatment and the rate of treatment relapse. Beckman et al. [22] mentioned significant and positive correlation between pre-treatment SN-GoGn angle and the changes of overbite after the treatment.
Previous studies had some drawbacks such as small sample size, [23-24] relatively short follow-up periods, [25] and improper definitions of open-bite. [19] Some researchers did not mention the treatment duration and the type of retainers used at the end of treatment. [17, 20] Some other studies did not discriminate between post-retention and post-treatment periods. [18] Headgear and bite plane, as accessory appliances, have considerable effects on the treatment of anterior open bite; however, to the best of our knowledge, the stability of the treatment results has not been investigated in any study. Also, there were few studies on the amount and cause of relapse of open bite treatments in Iran. Besides, there have been considerable contradictions in the results of previous studies; the relapse rate of 38.1% in one research [21] to report of no relapse in two other studies. [20, 26]
The present study was carried out to evaluate the stability of open bite treatment results in the retention phase during permanent dentition. Also, the effect of predictive factors such as pretreatment cephalometric variables and their changes during treatment was evaluated. In addition, the influence of treatment methods (extraction versus non-extraction) and simultaneous use of removable appliances on the changes of overbite in retention phase was assessed.
Materials and Method
Eighty patients with anterior open bite who had received treatment in Orthodontic Department of Shiraz Dental School and a private orthodontic office during 2006 to 2010 were recruited in this study. The inclusion criteria for patient selection were based on:
Presence of all permanent teeth up to the first molars before treatment initiation
Presence of pre-treatment overbite of ≤ 0 up to -3 millimeter (mm) without obvious need for surgery (such as extreme tooth show at rest, excessive display of gingiva on smile or too much facial length)
Skeletal nature of open bite (30>FMA>25, 60 <Jaraback index<65%)
Having had a course of comprehensive orthodontic treatment with or without removable appliances
Use of fixed retainer (bonded flexible spiral wire 4-4) at the end of treatment for at least three years
No frequent fracture of fixed retainers in the retention phase
Availability of lateral cephalograms related to pre-treatment (T1), post-treatment (T2) and at least 3 years after the end of the treatment (T3)
Preparation of lateral cephalograms of each patient with the same X-ray machine
No prosthodontic treatment or replacement in the incisal regions
Thirty-seven patients (20 males, 17 females) fulfilled these criteria and were included in this study. All patients were treated with full fixed appliances (edgewise technique), while a number of patients additionally had high-pull headgear or bite plane or both. The range of pre-treatment overbites was 0 to -3 mm. Twenty Two patients were treated by extraction (upper premolars or upper and lower premolars) and 15 cases did not have extraction in their treatment. Since the amount of crowding was less than 3 mm which was not sufficient for extracting premolar teeth, the main reason for extraction in the first group was open bite correction. Fixed retainers (bonded flexible spiral wire 4-4; both upper and lower arches) were placed for all the subjects. Patients were re-evaluated at least 3 years after the end of treatment in the presence of these retainers.
The major sources for gaining information were lateral cephalograms of the patients at T1, T2 and T3,as well as clinical inspections. For each patient, analysis of lateral cephalograms at different stages was performed by the same investigator. Magnification scales were applied on each cephalogram to control the measurement errors of linear variables caused by different magnifications of ephalograms. Intra-examiner error was assessed by measuring 10 radiographs twice a week apart. The mean differences of variables between the two time periods and their standard deviation (SD), as well as the correlation coefficient between two measurements were calculated for measurement error expression.
The mean overbite of cases was obtained from the lateral cephalograms at T1, T2 and T3. The mean changes of overbite between T1 and T2 and between T2 and T3 were calculated. Likewise, the number of patients with open bite and their percentage was determined at T3.
The effects of pre-treatment factors on the post-treatment relapse were studied by considering the relationship between the overbite change (T3-T2) and some factors including pre-treatment overbite, horizontal relationship of the jaws (ANB), vertical relationship of facial structures (FMA, Bjork angle and Jaraback index) and alveolar heights of molar and incisal areas of both jaws. These variables are displayed in figure 1 and represented in Table 1.
Figure 1.
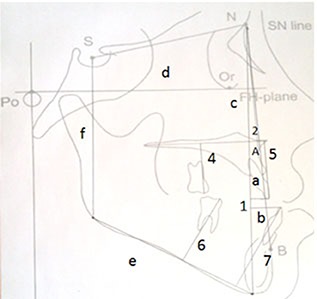
Cephalometric lines and angles used in this study
Table 1.
Definition of cephalometric lines and angles used in the present study
| Number (in figure) | Variable | Definition |
|---|---|---|
| 1 | Overbite | Vertical overlap of the incisal edges of maxillary (a) and mandibular incisors (b) relative to nasion-menton (N-Me) line (c) |
| 2 | ANB | The angle between the lines NA and NB |
| FMA | The angle between mandibular plane (Go-Me) (e) and Frankfort line (Po-Or) (d) | |
| Jaraback index | The posterior facial height (S-Go) (f) relative to anterior facial height (N-Me) (c) | |
| 4 | Maxillary Posterior Alveolar Height | The distance between mesiobuccal cusp of maxillary 1st molar and palatal plan (ANS-PNS) |
| 5 | Maxillary Anterior Alveolar Height | The distance between incisal edge of maxillary central incisor and palatal plane |
| 6 | Mandibular Posterior Alveolar Height | The distance between mesiobuccal cusp of mandibular 1st molar and mandibular plane (Go-Me) |
| 7 | Mandibular Anterior Alveolar Height | The distance between incisal edge of mandibular central incisor and mandibular plane |
During the treatment, some factors were also evaluated that were supposed to have influence on the post-treatment relapse such as extraction versus non-extraction therapy, using or not using the removable appliances and the type of these appliances (high-pull headgear, bite plane or both). The number of patients pertaining to either one of these treatment modalities was detected and the mean changes of overbite (T3-T2) in each group was measured and compared statistically.
To enroll descriptive statistics, independent sample t-test, one-way ANOVA and Pearson and Spearman correlation coefficients were employed for quantitative data. The significance level adopted was p= 0.05 and SPSS Software (Statistical Package for Social Sciences) was used for analyzing the variables.
Results
The Mean±SD age of samples at the beginning of the treatment was 18±2.1, the Mean±SD treatment duration was 20±3 months, and the mean follow-up period was 4 years and 2 months after treatment, with a range of 3 to 6 years.
Concerning the angles, the intra-examiner error varied from 0.23 for ANB to 0.65 for Bjork angle. While for the lines, the range of measurement errors was from 0.17 mm for mandibular posterior alveolar height to 0.76 mm for mandibular anterior alveolar height. Considering the standard deviation of measurements, the random error was small for all variables.
Table 2 displays the mean overbite of samples at T1, T2, T3, between T1 and T2 (T2-T1) and between T2 and T3 (T3-T2). Additionally, 16.6% (6 cases) had open bite (overbite≤0) at T3.
Table 2.
Mean overbite at various stages of treatment, follow-up and mean overbite changes between the phases
| T1 | T2 | T2-T1 | T3 | T3-T2 | |
|---|---|---|---|---|---|
| Mean overbite (mm) | -0.63±0.76 | 1.62±0.50 | 2.25±0.62 | 1.16±0.88 | -0.46±0.7 |
Pearson correlation was used to evaluate the relationship between overbite changes (T3-T2) and cephalometric variables at T1 (Table 3). Only Jaraback index showed statistically significant relation with post-treatment overbite changes (p= 0.035; r=0.353). The correlation of other variables was positive; however, not statistically significant (p> 0.05) (Table 3).
Table 3.
The correlation between cephalometric measurements and post-treatment overbite change
| Cephalometric variables | Correlation coefficient (r) | P-value |
|---|---|---|
| pre-treatment overbite | 0.035 | 0.815 |
| ANB | 0.290 | 0.082 |
| Bjork | 0.314 | 0.058 |
| FMA | 0.044 | 0.795 |
| Jaraback index | -0.353 | 0.035 |
| Maxillary posterior alveolar height t | 0.135 | 0.427 |
| Mandibular posterior alveolar height | 0.044 | 0.798 |
| Maxillary anterior alveolar height | 0.175 | 0.300 |
| Mandibular anterior alveolar height | 0.323 | 0.051 |
The relationship between Jaraback index and overbite change in the follow-up period is illustrated in figure 2. As it is shown, increase in Jaraback index lead to a decrease in the overbite changes; that is, there was a reverse correlation between Jaraback index and open bite tendency.
Figure 2.
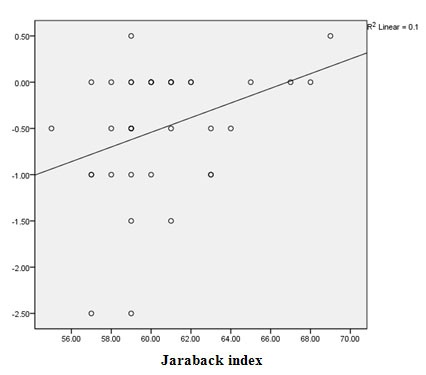
Relationship between Jaraback index and post-treatment overbite change
ANOVA test was applied for comparing the mean post-treatment overbite changes in the 3 groups with various removable appliances including (1) Headgear (HG), (2) Headgear and Bite Plane (BP) or Bite Plane and (3) No accessory appliance (Table 4). There was no significant difference among the three groups, although the mean overbite change was less in “no-appliance” group. Independent sample t-test was used to analyze and compare the means of overbite change (T3-T2) in extraction and non-extraction groups (Table 4). No significant difference was observed between the two groups; however, the mean overbite change was greater in the extraction group. Spearman correlation was used to assess the relationship between overbite changes at follow-up period (T3-T2) and changes of cephalometric measurements during the treatment (T2-T1) (Table 5). None of the radiographic variables revealed significant statistical correlation (p> 0.05).
Table 4.
The relationship between the treatment modalities and mean overbite change at follow-up period
| Variable | Group | Number | Mean ± SD | Statistical index( F ) | P-value |
|---|---|---|---|---|---|
| Removable appliance | HG | 18 | -0. 52±0.83 | 0.224 | 0.801 |
|
HG+BP Or BP |
7 | -0.57±0.73 | |||
| Type of treatment | No appliance | 12 | -0.37±0.48 | 0.224 | 0.801 |
| extraction | 22 | -0.63±0.77 | |||
| Non extraction | 15 | -0.26±0.63 |
Table 5.
The relationship between changes of cephalometric variables during the treatment and post-treatment overbite changes
| Change of Cephalometric variables ( T2-T1) | Correlation coefficient(r) | P-value |
|---|---|---|
| ANB | 0.108 | 0.523 |
| Bjork | 0.230 | 0.171 |
| FMA | 0.191 | 0.257 |
| Jaraback index | 0.105 | 0.543 |
| Maxillary posterior alveolar height | 0.158 | 0.351 |
| Mandibular posterior alveolar height | 0.296 | 0.075 |
| Maxillary anterior alveolar height | -0.069 | 0.687 |
| Mandibular anterior alveolar height | 0.062- | 0.717 |
Discussion
Based on the findings of this study, 6 patients (16/6%) experienced relapse of open bite in the presence of their fixed retainers. No relationship was found between the cephalometric variables or their changes during the treatment and the post-treatment bite opening in the studied sample. Moreover, various treatment strategies or simultaneous use of removable appliances did not show any significant difference regarding treatment stability.
Based on the results of this study, the mean overbite change during the follow-up period was found to be -0.46±0.7 mm. However, the number of patients with relapse (six open bite cases comprising 16.6%) during the post-treatment observations seems more important from clinical point of view. Remmors et al. [17] and Janson et al. [18] reported similar results in their studies. Remmors et al. evaluated 52 patients with pre-treatment open bite and observed that 27% of successfully treated patients showed opening of the bite 5 years after treatment. The study by Jonson et al. showed negative overlap in 25.8% of the samples at the end of post-treatment period; although they applied a different definition for overbite measurement. In a meta-analysis study, Greenlee et al. [27] reported the stability of nonsurgical treatments of anterior open bite to be greater than 75% at 12 or more months after the treatment. Lopez Gavito et al. [19] found treatment relapse in more than 35% of their patients in post-retention period. However, the limitation of their study was the inaccurate definition of open bite, which could likely not only be observed in deep bite patients, but also was affected by antero-posterior position of the incisors. Zuroff et al. [20] divided 64 patients into three groups based on the amounts of pre-treatment overbite and reported that all the patients had positive overbite at the post retention recall. However, as the authors expressed, their finding should be interpreted with caution since only 15 patients with pre-treatment open bite were present in that study.
In our study, neither the pre-treatment cephalometric measurements (primary overbite, horizontal jaw relationships, vertical relationships of facial structures and alveolar heights in the different parts of the jaws), nor the change of radiographic variables during the treatment had the capability to predict stability of the treatment. Only Jaraback index value in the pre-treatment phase showed significant- but weak- relationship with post-treatment overbite changes. As expected, a negative correlation was noticed because the increase in posterior facial height relative to the anterior part of face decreases the tendency for creating anterior open bite. Regarding this poor relationship and the possibility of chance in that, it could be possibly concluded that there was no reliable factor for predicting post-treatment changes of open bite therapies. Moreover, no significant correlation was found between the changes of Jaraback index during the treatment and the treatment stability. Considering the limitations of our study, such as retrospective design, sample size and lack of control on all variables, this conclusion should be interpreted with caution. Similarly, Lopez Gavito et al. [19] have not reported any relation between primary overbite, steepness of mandibular plane or any exclusive factor and post-treatment stability. The study of de Freitas et al. [21] also showed no relation between overbite at the beginning of the treatment or its changes during the treatment and the rate of treatment relapse. Among many factors investigated by Remmers et al. [17] only mandibular and palatal plane angles at the beginning of the treatment showed significant relationship with post-treatment overbite changes. Nonetheless, the researchers explained this was achieved only by chance, hence, open bite could not be predicted successfully from pre-treatment cephalometric variables. Beckman et al. [22] mentioned significant and positive correlation between pre-treatment SN-GoGn angle and the changes of overbite after treatment. However, inconsistent treatment techniques, broad range of participants’ age, various types of retainers and the limited number of cases at the follow-up recall influenced the results of the study.
Based on the results of our study, the extraction and non-extraction groups did not show any significant difference in terms of treatment stability. Remmers et al. [17] reported that extraction therapy (either in the upper or both arches) was not associated with the closure or stability of anterior open bite. Janson et al. [18] observed that the relapse rate of open bite treatment in extraction and non-extraction groups were 25.8% and 38.1%, respectively, with extraction therapy exhibiting greater stability. Nonetheless, neither group showed a statistically significant difference in the number of patients with open bite in the follow-up period.
The influence of using removable appliances in addition to comprehensive treatment of anterior open bite was not evaluated in the previous studies. Our investigation showed that simultaneous use of headgear or bite plane or their combination would not lead to a better stability of the treatment. It must be pointed out, however, that more accurate studies with greater control of other variables are required to assess the advantages or disadvantages of using removable appliances as adjunct to fixed appliance therapy.
Some adjunctive treatments like orofacial myofunctional therapy (OMT) [28] and non-surgical treatments with temporary anchorage devices [29] have presented promising results in recent studies; although their long-term effectiveness has not been evaluated thoroughly. [30]
Considering the relapse of treated open bite in six patients during the retention phase, it seems that fixed retainers alone were not absolutely sufficient for maintaining the results of open bite treatment. However, since this study, similar to the previous investigations, is a retrospective study, some attempts such as gaining strict control over the variables, making comparison with control groups, evaluating the impact of growth, and post-treatment factors like use of other types of retainers, patients cooperation and lengthening the follow-up period, as well as designing prospective studies are suggested to be considered for future investigations.
Conclusion
Fixed retainers were not thoroughly successful in maintaining the overlap of incisors achieved during treatment of open bite patients.
There was no possibility of predicting treatment stability due to the absence of correlation between pre-treatment overbite and cephalometric variables or the change of radiographic measurements during treatment.
No significant difference was observed between the extraction and non-extraction groups with regard to the post treatment overbite changes.
Simultaneous use of removable appliances and their type did not show significant differences in the rate of treatment relapse.
In addition to fixed retainers, other types of retainers for controlling interarch discrepancy and vertical dimension are suggested in the retention phase of open bite patients.
Acknowledgment
The authors thank the vice-chancellery of Shiraz University of Medical Science and Orthodontic Research Centre of Shiraz University of Medical Sciences for supporting the research (Grant#5034). This article is derived from the post graduate thesis by Dr. Alireza Hoseini. The authors also thank Dr.Sh.Hamedani and Dr. Amalsaleh from the Dental Research Development Center, at the School of Dentistry for improving the English edition of the manuscript and Dr. Sayadi for the statistical consultation.
Conflict of Interest: The authors of this manuscript certify that they have no financial or other competing interest concerning this article.
References
- 1.Nanda R, Urib F. Management of open bite malocclusions. In: Nanda R, editor. Biomechanical and esthetic strategies in clinical orthodontics. 2nd ed. Saunders: Elsevier; 2005. p. 156. [Google Scholar]
- 2.Shahri F. Prevalence of anterior of open bite in 12-15 years old. Tabib-e-Shargh. 2003; 5: 191–195. [Google Scholar]
- 3.Khanemasjedi M, Basiri L. A Study on prevalence of open bite in 11- 14 year old boy student in Ahwaz in 2001. J Mash Dent Sch. 2003; 27: 11–15. [Google Scholar]
- 4.Pakshir HR, Keramoddin Sh. Prevalence assessment of anterior open bite and evaluation of related skeletal and dental changes in 9-11 years old Shiraz primary school students. J Dent Shiraz Univ Med Sci. 2000; 2: 31–45. [Google Scholar]
- 5.Stojanović L. Etiological aspects of anterior open bite. Med Pregl. 2007; 60: 151–155. doi: 10.2298/mpns0704151s. [DOI] [PubMed] [Google Scholar]
- 6.Lentini Oliveira D, Carvalho FR, Qingsong Y, Junjie L, Saconato H, Machado MA, et al. Orthodontic and orthopaedic treatment for anterior open bite in children. Cochrane Database Syst Rev. 2007; 18: CD005515. doi: 10.1002/14651858.CD005515.pub2. [DOI] [PubMed] [Google Scholar]
- 7.Proffit WR, Sarver DM. Diagnosis: gathering and organizing the appropriate information. In: Proffit WR, White RP, Sarver DM, editors. Contemporary treatment of dentofacial deformity. 4th ed. St. Louis: Mosby; 2003. p. 157. [Google Scholar]
- 8.Nanda R, Urib F. Management of open bite malocclusions. In: Nanda R, editor. Biomechanical and esthetic strategies in clinical orthodontics. 2nd ed. Saunders: Elsevier; 2005. p. 156. [Google Scholar]
- 9.Torres F, Almeida RR, de Almeida MR, Almeida Pedrin RR, Pedrin F, Henriques JF. Anterior open bite treated with a palatal crib and high-pull chin cup therapy. A prospective randomized study. Eur J Orthod. 2006; 28: 610–617. doi: 10.1093/ejo/cjl053. [DOI] [PubMed] [Google Scholar]
- 10.Cozza P, Baccetti T, Franchi L, Mucedero M. Comparison of 2 early treatment protocols for open-bite malocclusions. Am J Orthod Dentofacial Orthop. 2007; 132: 743–747. doi: 10.1016/j.ajodo.2005.11.045. [DOI] [PubMed] [Google Scholar]
- 11.Ibitayo AO, Pangrazio Kulbersh V, Berger J, Bayirli B. Dentoskeletal effects of functional appliances vs bimaxillary surgery in hyperdivergent Class II patients. Angle Orthod. 2011; 81: 304–311. doi: 10.2319/060110-297.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Uzdil F, Kayalioglu M, Kendi E, Toroglu MS. A new type of modified Essix Retainer for anterior open bite retention. Prog Orthod. 2010; 11: 45–52. doi: 10.1016/j.pio.2010.04.009. [DOI] [PubMed] [Google Scholar]
- 13.Proffit WR. Retention. In: Proffit WR, Fields HW, Sarver DM, editors. Contemporary orthodontics. 5th ed. Mosby: Elsevier; 2013. pp. 610–611. [Google Scholar]
- 14.Vandersdall RL, Musich DR. Adult interdisciplinary therapy, diagnosis and treatment. In: Graber Lee, Vanarsdall RL, Katherine WL., editors. Orthodontics: current principles and techniques. 4th ed. Mosby: Elsevier; 2012. p. 884. [Google Scholar]
- 15.Nanda R, Urib F. Management of open bite malocclusions. In: Nanda R, editor. Biomechanical and esthetic strategies in clinical orthodontics. 2nd ed. Saunders: Elsevier; 2005. p. 174. [Google Scholar]
- 16.Proffit WR, Fields HW. Treatment of skeletal problems in children and preadolscents. In: Proffit WR, Fields HW, Sarver DM, editors. Contemporary orthodontics. 5th ed. Mosby: Elsevier; 2013. p. 518. [Google Scholar]
- 17.Remmers D, Van't Hullenaar RW, Bronkhorst EM, Bergé SJ, Katsaros C. Treatment results and long-term stability of anterior open bite malocclusion. Orthod Craniofac Res. 2008; 11: 32–42. doi: 10.1111/j.1601-6343.2008.00411.x. [DOI] [PubMed] [Google Scholar]
- 18.Janson G, Valarelli FP, Henriques JF, de Freitas MR, Cançado RH. Stability of anterior open bite nonextraction treatment in the permanent dentition. Am J Orthod Dentofacial Orthop. 2003; 124: 265–276. doi: 10.1016/s0889-5406(03)00449-9. [DOI] [PubMed] [Google Scholar]
- 19.Lopez Gavito G, Wallen TR, Little RM, Joondeph DR. Anterior open-bite malocclusion: a longitudinal 10-year postretention evaluation of orthodontically treated patients. Am J Orthod. 1985; 87: 175–186. doi: 10.1016/0002-9416(85)90038-7. [DOI] [PubMed] [Google Scholar]
- 20.Zuroff JP, Chen SH, Shapiro PA, Little RM, Joondeph DR, Huang GJ. Orthodontic treatment of anterior open-bite malocclusion: stability 10 years postretention. Am J Orthod Dentofacial Orthop. 2010; 137: 302. doi: 10.1016/j.ajodo.2009.06.020. e1-8. [DOI] [PubMed] [Google Scholar]
- 21.de Freitas MR, Beltrão RT, Janson G, Henriques JF, Cançado RH. Long-term stability of anterior open bite extraction treatment in the permanent dentition. Am J Orthod Dentofacial Orthop. 2004; 125: 78–87. doi: 10.1016/j.ajodo.2003.01.006. [DOI] [PubMed] [Google Scholar]
- 22.Beckmann SH, Segner D. Changes in alveolar morphology during open bite treatment and prediction of treatment result. Eur J Orthod. 2002; 24: 391–406. doi: 10.1093/ejo/24.4.391. [DOI] [PubMed] [Google Scholar]
- 23.Huang GJ, Justus R, Kennedy DB, Kokich VG. Stability of anterior openbite treated with crib therapy. Angle Orthod. 1990; 60: 17–24. doi: 10.1043/0003-3219(1990)060<0017:SOAOTW>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 24.Katsaros C, Berg R. Anterior open bite malocclusion: a follow-up study of orthodontic treatment effects. Eur J Orthod. 1993; 15: 273–280. doi: 10.1093/ejo/15.4.273. [DOI] [PubMed] [Google Scholar]
- 25.Denison TF, Kokich VG, Shapiro PA. Stability of maxillary surgery in openbite versus nonopenbite malocclusions. Angle Orthod. 1989; 59: 5–10. doi: 10.1043/0003-3219(1989)059<0005:SOMSIO>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 26.Kim YH, Han UK, Lim DD, Serraon ML. Stability of anterior openbite correction with multiloop edgewise archwire therapy: A cephalometric follow-up study. Am J Orthod Dentofacial Orthop. 2000; 118: 43–54. doi: 10.1067/mod.2000.104830. [DOI] [PubMed] [Google Scholar]
- 27.Greenlee GM, Huang GJ, Chen SS, Chen J, Koepsell T, Hujoel P. Stability of treatment for anterior open-bite malocclusion: a meta-analysis. Am J Orthod Dentofacial Orthop. 2011; 139: 154–169. doi: 10.1016/j.ajodo.2010.10.019. [DOI] [PubMed] [Google Scholar]
- 28.Smithpeter J, Covell D. Relapse of anterior open bites treated with orthodontic appliances with and without orofacial myofunctional therapy. Am J Orthod Dentofacial Orthop. 2010; 137: 605–614. doi: 10.1016/j.ajodo.2008.07.016. [DOI] [PubMed] [Google Scholar]
- 29.Razavi MR. Molar intrusion using miniscrew palatal anchorage. J Clin Orthod. 2012; 46: 493–498. [PubMed] [Google Scholar]
- 30.Huang GJ, Greenlee GM. Stability of anterior open bite correction- an assessment of the evidence. In: Huang GJ, Richmond S, Katherine WL, editors. Evidenced-based orthodontics. 1st ed. United States: Wiley-Blackwell; 2011. p. 112. [Google Scholar]


